Mon, May 6, 2024
[Archive]
Volume 17, Issue 11 (November 2019)
IJRM 2019, 17(11): 841-850 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Momeni Z, Dehghani A, Fallahzadeh H, Koohgardi M, Dafei M, Mohammadi M. Effects of low-dose contraceptive pills on the risk factors of cardiovascular diseases among 15-35-year-old women: A retrospective cohort. IJRM 2019; 17 (11) :841-850
URL: http://ijrm.ir/article-1-1724-en.html
URL: http://ijrm.ir/article-1-1724-en.html
Zahra Momeni * 

 1, Ali Dehghani2
1, Ali Dehghani2 

 , Hossein Fallahzadeh2
, Hossein Fallahzadeh2 

 , Moslem Koohgardi3
, Moslem Koohgardi3 

 , Maryam Dafei4
, Maryam Dafei4 

 , Masoud Mohammadi5
, Masoud Mohammadi5 




 1, Ali Dehghani2
1, Ali Dehghani2 

 , Hossein Fallahzadeh2
, Hossein Fallahzadeh2 

 , Moslem Koohgardi3
, Moslem Koohgardi3 

 , Maryam Dafei4
, Maryam Dafei4 

 , Masoud Mohammadi5
, Masoud Mohammadi5 


1- Deputy of Health, Bushehr University of Medical Sciences, Bushehr, Iran., Department of Biostatistics and Epidemiology, Faculty of Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran. , zmomeni547@gmail.com
2- Department of Biostatistics and Epidemiology, Faculty of Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
3- Department of Health Education and Health Promotion, Faculty of Health, Rafsanjan University of Medical Sciences and Health Services, Kerman, Iran.
4- Department of Midwifery, School of Nursing and Midwifery, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
5- Department of Nursing, Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
2- Department of Biostatistics and Epidemiology, Faculty of Health, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
3- Department of Health Education and Health Promotion, Faculty of Health, Rafsanjan University of Medical Sciences and Health Services, Kerman, Iran.
4- Department of Midwifery, School of Nursing and Midwifery, Shahid Sadoughi University of Medical Sciences and Health Services, Yazd, Iran.
5- Department of Nursing, Faculty of Nursing and Midwifery, Kermanshah University of Medical Sciences, Kermanshah, Iran.
Full-Text [PDF 291 kb]
(912 Downloads)
| Abstract (HTML) (3948 Views)
HCY is a sulfur-contained amino acid and as a by-product of methionine breakdown (10) prevents the normal function of nitric oxide (NO) resulting from the autoxidation process. It can, therefore, cause endothelial dysfunction (11). NO is produced in the endothelium by L-arginine synthesis (11) and can cause vasodilatation, -preventing platelet accumulation- and migration (12, 13). In a study it was shown that a decrease in NO may lead to diseases like atherosclerosis, cardiac disease, and hypertension (14).
Various studies have demonstrated that female gonadal steroids may affect NO and HCY (12, 13). However, because of the contradictory results, it is still unclear whether an oral contraceptive pill (OCP) is related to changes in plasma HCY levels (15, 16) or not. Nowadays, low-dose pills containing 0.15 mg of levonorgestrel and 0.03 mg of ethinylestradiol (16) are considered as the usage contraindication of the pills after the age of 35 yr. Nevertheless, the pills were widely administered on women who are nonsmoker and without hypertension and migraine, which predisposes them to cardiovascular disease risk (17, 18).
Furthermore, it has been reported that OCPs can change some plasma lipids concentration including total cholesterol, high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), and triglyceride (15-18). Consuming OCPs can have a negative effect on the lipid profiles in healthy women, that is, it can increase the triglyceride level and also decrease the high-density lipoproteins (HDL) level (18).
Although consuming OCPs can increase cardiovascular risk factors, there are limited reports in this regard in the literature. Therefore, this research is designed and conducted to investigate the relationship between cardiovascular disease risk factors and the consumption of low-dose OCPs amongst healthy women in Yazd, Iran.
The sample population was followed-up in 2014 for a minimum duration of three months and a maximum of six months and the OCP users’ blood samples were examined for two years.
2.1.Subjects
Participants were classified into OCP and non-OCP groups. The OCP group consisted of women with menstrual cycles of at least three days and a maximum of 36 days, who used OCP (Aburaihan Pharmaceutical Co., Iran) for 0-3, 4-23, and 36- 24 months. After taking 21 pills, they stopped taking the pills for 7 days, then they took the next box of pills. The non-OCP group included women referred to the health care centers for any other reasons and did not take any birth birth-control hormonal preparations.
2.2.Sample size and sampling method
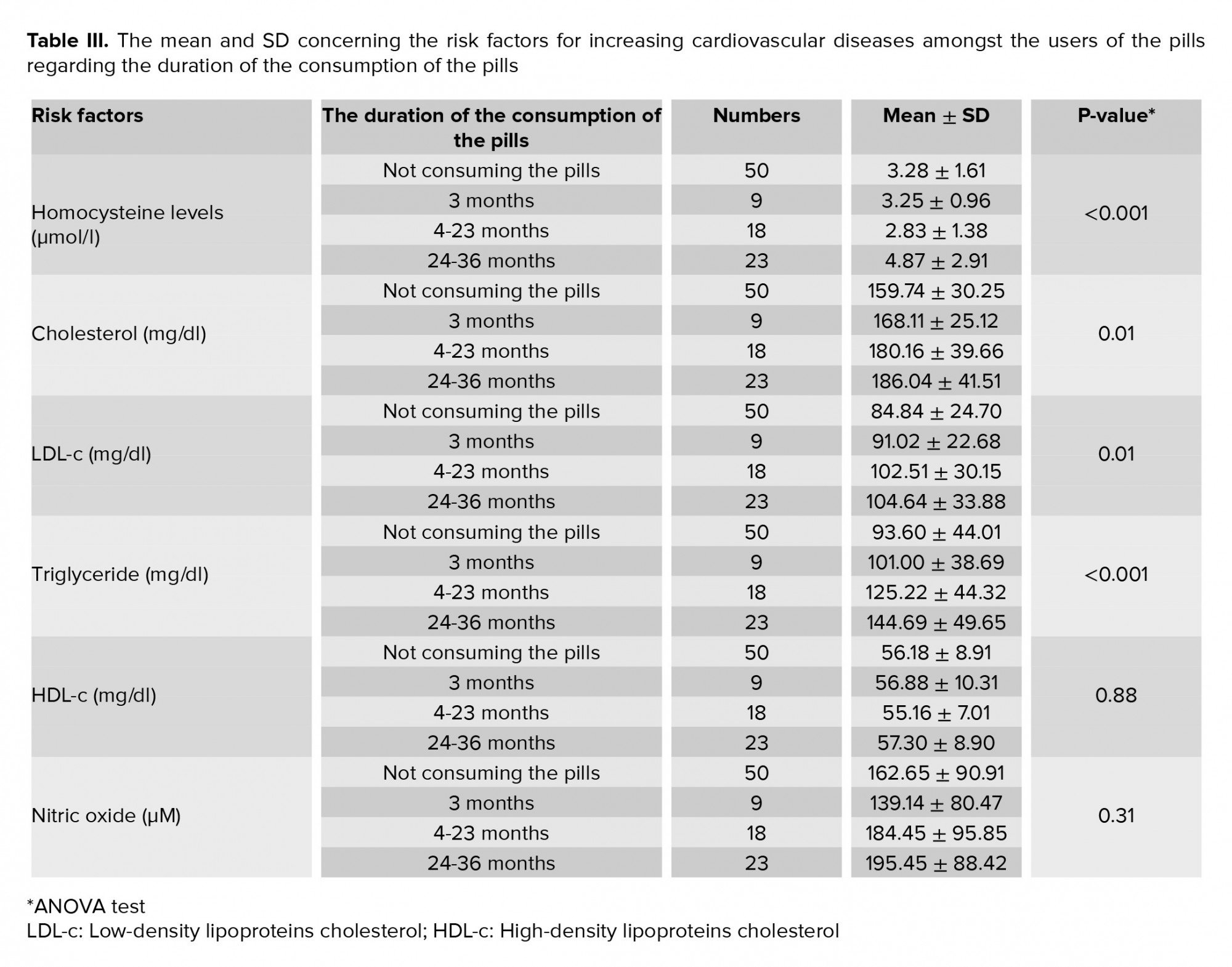
The significance level of 5% and the test power of 90% were used for this study. Considering the standard deviation of HCY level in the previous study (SD = 3.5) (19), for achieving a minimum difference of more than 3 units between the mean HCY levels after a maximum of six months follow-up in both groups, according to the following formula, 50 samples per group were required:
2.3.Data collection
The demographic data including the age, occupation, educational level, family income level, as well as data regarding the history of pregnancy, delivery type, number of children, smoking and alcohol habits, history of taking medication (e.g., OCPs), menstrual cycle, duration of OCP usage, and physical exercise were obtained through a face-to-face interview. The exclusion criteria included repeated abortion history (≥ 2 times), thyroid dysfunction, history of heart diseases in family before the age of 40 yr, personal history of heart disease, diabetes, hepatic disease, renal dysfunction, and dyslipidemia. Other exclusion criteria encompassed those working with pesticides, smoking themselves or having a partner who smokes, drinking alcohol, history of anemia, taking vitamin supplements such as folic acid, vitamins B6 and B12 during the last year, receiving a blood transfusion, and being pregnant since the last year. The essential information was gathered through face-to-face interviews and recorded on a checklist.
Also, a literature survey was done to determine the factors influencing lipid profiles, HCY, and NO levels (9-18).
2.4.Procedures
After consulting specialists, some factors influencing blood biochemical parameters were determined and recorded and ultimately prepared as a checklist validated by authorities. Based on this checklist, the candidates who were not meeting the exclusion criteria were included in the study. The participants were categorized into four groups. The first group had not consumed those pills or using any other hormonal method to prevent pregnancy. Groups 2, 3, and 4, on the other hand, had consumed LD tablets for a time period of 3, 4-23, and 24-36 months, respectively.
The participants were followed-up for a minimum duration of three months and a maximum of six months. After that, their weight, blood pressure, body mass index (BMI) (manufactured by OMRON health care BF511, China), and waist-hip ratio (WHR) were measured. In the end, the venous blood samples were taken from the groups (OCP and non-OCP groups) and were sent to the central laboratory in Yazd to analyze the biochemical parameters using the standard techniques (2, 17, 20-23).
2.5.The conditions and methods of blood biochemical parameter measurements
"10cc blood sample was taken from each participants between 9 and 11 am to minimize the chemical changes. 4 ml was put into EDTA tubes, and 6 ml in the sodium citrate tubes being kept in the ice throughout the preparation process, during the time of the sampling phase until the samples were sent to the central laboratory for analyzing the parameters. Total cholesterol, triglyceride, HDL-c, and LDL-c levels were measured. The following parameters were calculated using auto Analyzer (Hitachi, Japan) and commercial kits, manufactured by Bionic corporation (confirmed by the Iran Health Reference Laboratory): triglyceride levels in serum by using the enzymatic method (lipase for converting triglyceride to glycerol), cholesterol levels by using the enzymatic cholesterol esterase (lipase for converting triglyceride to glycerol), and HDL-c by using the enzymatic precipitation method. LDL-c was also calculated using the Friedwald formula (24).
HCY levels were determined (coefficient of variation ≤ 5%) via the enzymatic and photometric method using the HCY kit manufactured by Diazyme (Roche subsidiary company, USA) and Auto Analyzer BT3000 (Biotechnics, Italy). The NO levels were determined using a photometric method and also Greiss reaction. A micropipette reader (having CV < 5%), a kit manufactured by Iran Sib Bio, and an ELISA microplate reader 3200 FaxStat (Awareness Technologies, USA) were used in this work.
2.6.Ethical consideration
This study was approved by Shahid Sadoughi University of Medical Sciences Ethics Committee, Yazd, Iran (Code: IR.SSU.SPH.REC.1394.69). Written informed consent was obtained from all participants in this study.
2.7.Data analysis
The collected data were analyzed using the Statistical Package for the Social Sciences software (SPSS, version 16, SPSS Inc, Chicago, Illinois, USA), the descriptive tests, Chi-square test, independent t-test, Tukey’s test, and ANOVA test with a significance level of 0.05. In conclusion, the results were attained by comparing the participants consuming the pills with those using non-hormonal birth control methods.
According to the results, a majority of participants in the OCP group were housewives that is 88.8%, 94.4%, and 91.3% of those exposed to the pills for 3, 4-23, and 24-36 months, respectively. Moreover, regarding the education level of the participants, in the groups exposed to the pills for 3 and 24-36 months, a majority of the participants had primary school education degree or were illiterate. On the contrary, in the non-OCP group, most of the participants were housewives with a university degree (Table I).
Based on our findings, there were no comprehensible statistical differences regarding job (p = 0.525), educational level (p = 0.636), and hourly physical exercises in a week (p = 0.830). Although there was no significant difference statistically between the two groups, there was a comprehensible statistical association between the groups concerning the monthly family income level (p = 0.011).
Anthropometric features and the participants’ blood pressure measurements are shown in Table II. Using ANOVA test, no statistically significant differences were found in the mean values of BMI, WHR, and diastolic blood pressure amongst the groups regarding the duration of the consumption of the pills (p ≥ 0.05), while there were comprehensible differences in the systolic blood pressure amongst the groups regarding the pills-usage duration. Tukey’s test proved that the maximum mean systolic blood pressure was seen amongst the women consuming the pills for 4-23 and 24-36 months (p = 0.05).
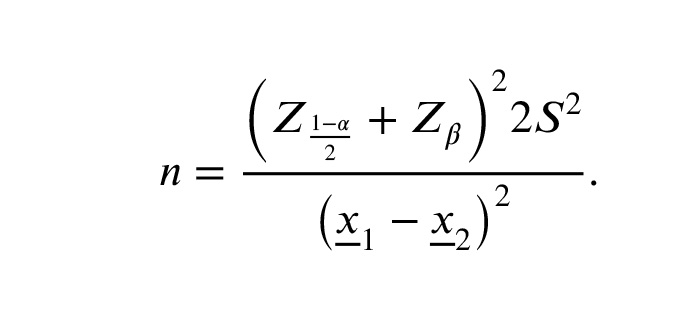
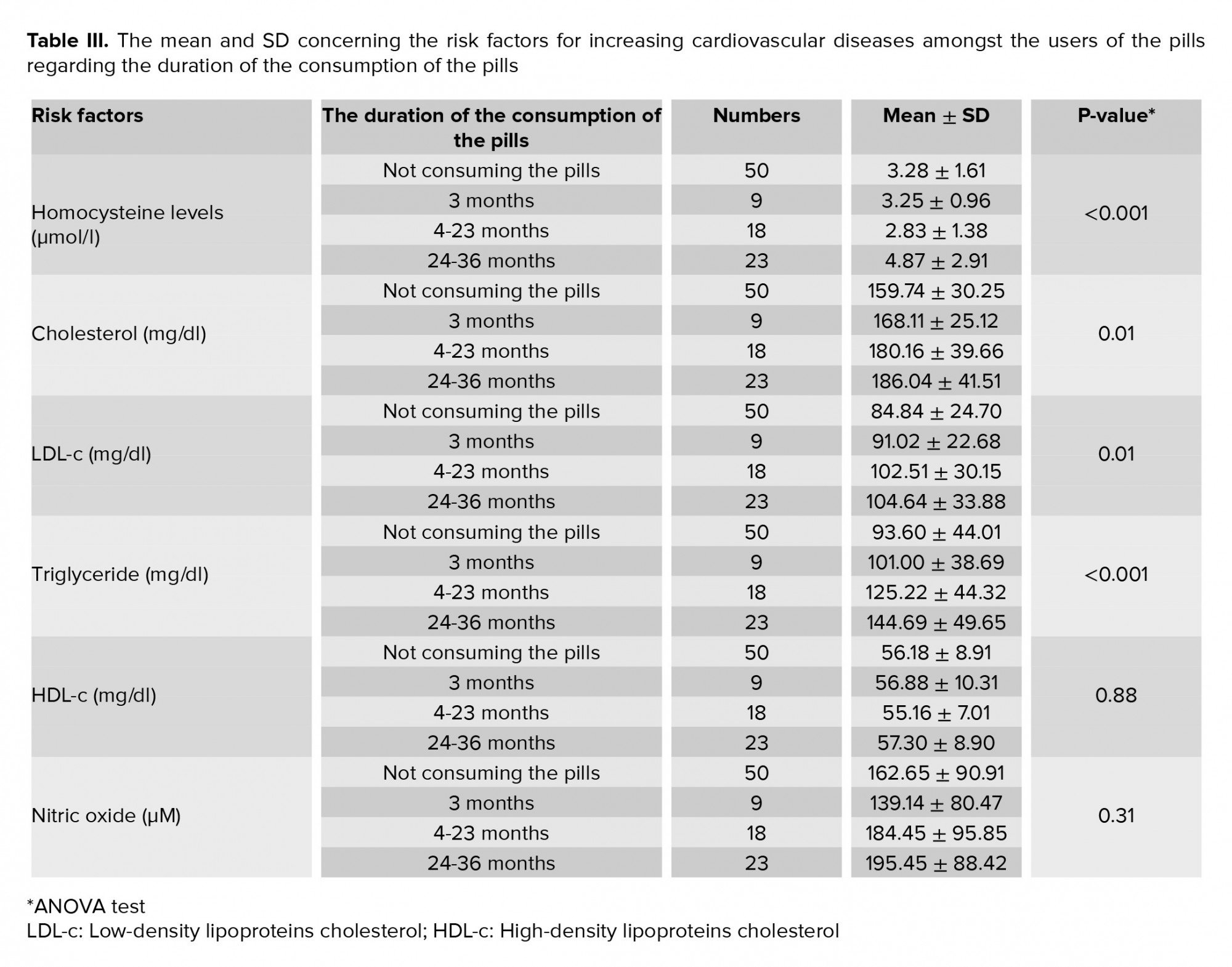
The average incidence rates of risk factors for increasing cardiovascular diseases amongst the participants are displayed in Table III. There were no remarkable differences in the mean values of the NO and HDL levels amongst the groups regarding the duration of the consumption of LD contraceptive pills according to the ANOVA test. However, there were comprehensible differences in the mean values of LDL, HCY, cholesterol, and triglyceride levels between the groups due to the difference in the duration of the consumption of LD contraceptive pills statistically. Tukey’s test proved that the mean values of LDL (p = 0.02), cholesterol (p = 0.01), and triglyceride (p < 0.001) levels amongst the users of the pills for 24-36 months and the mean value of HCY level among the users for 4-23 and 24-36 months were higher than the mean values of those levels amongst the other corresponding person (p < 0.001).


The present study indicated that there was a comprehensible difference in the mean value of the plasma level of HCY due to the difference in the duration of the pill consumption. A study carried out by Fallah and colleagues on 100 women with/without a history of consuming the pills in Tehran, Iran, showed a result compatible with ours (12).
The results proved that although the mean values of NO and HDL-c levels among the women using the pills for the longest period were high, there were no significant differences in comparison with the other groups in this regard. According to other findings, the mean values of triglyceride, cholesterol, and LDL-c levels among the women consuming the pills for the longest time were high, which in this finding was comprehensible amongst the users of the pills statistically. Moreover, the study accomplished by Emokpae and colleagues to investigate the influence of long-term usage of the pills on lipid profiles showed results compatible with our results (25). Contrasting to this study, a study by Guazzelli to investigate lipid profiles revealed that the duration of the pill consumption made no statistically significant changes in this regard (30). Dissimilar to the conducted studies, examining the influence of OCPs for a short period of time, investigating the effects on women attending only one public health clinic, and also considering no difference between the prescribed pills, the current study has some strengths as follows: only LD contraceptive pills were used for a long time and they were given to the women who attended several public health clinics.
There were also some limitations in this study. First, the limitation of costs for this project due to which the study was conducted on a relatively small population. Therefore, some relationships were not detected due to the low sample size. Second, the study was performed in a limited time so that only one blood sample was taken from each participant regardless of the follicular and luteal phase of the menstrual cycle.
Acknowledgments
The authors thank the faculty members of the Faculty of Health, Shahid Sadoughy University of Medical Sciences. This study was funded by the Vice Chancellor for Research and Technology of Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Conflict of interests
The authors declare that there is no conflicts of interests.
Full-Text: (347 Views)
- Introduction
HCY is a sulfur-contained amino acid and as a by-product of methionine breakdown (10) prevents the normal function of nitric oxide (NO) resulting from the autoxidation process. It can, therefore, cause endothelial dysfunction (11). NO is produced in the endothelium by L-arginine synthesis (11) and can cause vasodilatation, -preventing platelet accumulation- and migration (12, 13). In a study it was shown that a decrease in NO may lead to diseases like atherosclerosis, cardiac disease, and hypertension (14).
Various studies have demonstrated that female gonadal steroids may affect NO and HCY (12, 13). However, because of the contradictory results, it is still unclear whether an oral contraceptive pill (OCP) is related to changes in plasma HCY levels (15, 16) or not. Nowadays, low-dose pills containing 0.15 mg of levonorgestrel and 0.03 mg of ethinylestradiol (16) are considered as the usage contraindication of the pills after the age of 35 yr. Nevertheless, the pills were widely administered on women who are nonsmoker and without hypertension and migraine, which predisposes them to cardiovascular disease risk (17, 18).
Furthermore, it has been reported that OCPs can change some plasma lipids concentration including total cholesterol, high-density lipoprotein cholesterol (HDL-c), low-density lipoprotein cholesterol (LDL-c), and triglyceride (15-18). Consuming OCPs can have a negative effect on the lipid profiles in healthy women, that is, it can increase the triglyceride level and also decrease the high-density lipoproteins (HDL) level (18).
Although consuming OCPs can increase cardiovascular risk factors, there are limited reports in this regard in the literature. Therefore, this research is designed and conducted to investigate the relationship between cardiovascular disease risk factors and the consumption of low-dose OCPs amongst healthy women in Yazd, Iran.
- Materials and Methods
The sample population was followed-up in 2014 for a minimum duration of three months and a maximum of six months and the OCP users’ blood samples were examined for two years.
2.1.Subjects
Participants were classified into OCP and non-OCP groups. The OCP group consisted of women with menstrual cycles of at least three days and a maximum of 36 days, who used OCP (Aburaihan Pharmaceutical Co., Iran) for 0-3, 4-23, and 36- 24 months. After taking 21 pills, they stopped taking the pills for 7 days, then they took the next box of pills. The non-OCP group included women referred to the health care centers for any other reasons and did not take any birth birth-control hormonal preparations.
2.2.Sample size and sampling method
The significance level of 5% and the test power of 90% were used for this study. Considering the standard deviation of HCY level in the previous study (SD = 3.5) (19), for achieving a minimum difference of more than 3 units between the mean HCY levels after a maximum of six months follow-up in both groups, according to the following formula, 50 samples per group were required:
2.3.Data collection
The demographic data including the age, occupation, educational level, family income level, as well as data regarding the history of pregnancy, delivery type, number of children, smoking and alcohol habits, history of taking medication (e.g., OCPs), menstrual cycle, duration of OCP usage, and physical exercise were obtained through a face-to-face interview. The exclusion criteria included repeated abortion history (≥ 2 times), thyroid dysfunction, history of heart diseases in family before the age of 40 yr, personal history of heart disease, diabetes, hepatic disease, renal dysfunction, and dyslipidemia. Other exclusion criteria encompassed those working with pesticides, smoking themselves or having a partner who smokes, drinking alcohol, history of anemia, taking vitamin supplements such as folic acid, vitamins B6 and B12 during the last year, receiving a blood transfusion, and being pregnant since the last year. The essential information was gathered through face-to-face interviews and recorded on a checklist.
Also, a literature survey was done to determine the factors influencing lipid profiles, HCY, and NO levels (9-18).
2.4.Procedures
After consulting specialists, some factors influencing blood biochemical parameters were determined and recorded and ultimately prepared as a checklist validated by authorities. Based on this checklist, the candidates who were not meeting the exclusion criteria were included in the study. The participants were categorized into four groups. The first group had not consumed those pills or using any other hormonal method to prevent pregnancy. Groups 2, 3, and 4, on the other hand, had consumed LD tablets for a time period of 3, 4-23, and 24-36 months, respectively.
The participants were followed-up for a minimum duration of three months and a maximum of six months. After that, their weight, blood pressure, body mass index (BMI) (manufactured by OMRON health care BF511, China), and waist-hip ratio (WHR) were measured. In the end, the venous blood samples were taken from the groups (OCP and non-OCP groups) and were sent to the central laboratory in Yazd to analyze the biochemical parameters using the standard techniques (2, 17, 20-23).
2.5.The conditions and methods of blood biochemical parameter measurements
"10cc blood sample was taken from each participants between 9 and 11 am to minimize the chemical changes. 4 ml was put into EDTA tubes, and 6 ml in the sodium citrate tubes being kept in the ice throughout the preparation process, during the time of the sampling phase until the samples were sent to the central laboratory for analyzing the parameters. Total cholesterol, triglyceride, HDL-c, and LDL-c levels were measured. The following parameters were calculated using auto Analyzer (Hitachi, Japan) and commercial kits, manufactured by Bionic corporation (confirmed by the Iran Health Reference Laboratory): triglyceride levels in serum by using the enzymatic method (lipase for converting triglyceride to glycerol), cholesterol levels by using the enzymatic cholesterol esterase (lipase for converting triglyceride to glycerol), and HDL-c by using the enzymatic precipitation method. LDL-c was also calculated using the Friedwald formula (24).
HCY levels were determined (coefficient of variation ≤ 5%) via the enzymatic and photometric method using the HCY kit manufactured by Diazyme (Roche subsidiary company, USA) and Auto Analyzer BT3000 (Biotechnics, Italy). The NO levels were determined using a photometric method and also Greiss reaction. A micropipette reader (having CV < 5%), a kit manufactured by Iran Sib Bio, and an ELISA microplate reader 3200 FaxStat (Awareness Technologies, USA) were used in this work.
2.6.Ethical consideration
This study was approved by Shahid Sadoughi University of Medical Sciences Ethics Committee, Yazd, Iran (Code: IR.SSU.SPH.REC.1394.69). Written informed consent was obtained from all participants in this study.
2.7.Data analysis
The collected data were analyzed using the Statistical Package for the Social Sciences software (SPSS, version 16, SPSS Inc, Chicago, Illinois, USA), the descriptive tests, Chi-square test, independent t-test, Tukey’s test, and ANOVA test with a significance level of 0.05. In conclusion, the results were attained by comparing the participants consuming the pills with those using non-hormonal birth control methods.
- Results
According to the results, a majority of participants in the OCP group were housewives that is 88.8%, 94.4%, and 91.3% of those exposed to the pills for 3, 4-23, and 24-36 months, respectively. Moreover, regarding the education level of the participants, in the groups exposed to the pills for 3 and 24-36 months, a majority of the participants had primary school education degree or were illiterate. On the contrary, in the non-OCP group, most of the participants were housewives with a university degree (Table I).
Based on our findings, there were no comprehensible statistical differences regarding job (p = 0.525), educational level (p = 0.636), and hourly physical exercises in a week (p = 0.830). Although there was no significant difference statistically between the two groups, there was a comprehensible statistical association between the groups concerning the monthly family income level (p = 0.011).
Anthropometric features and the participants’ blood pressure measurements are shown in Table II. Using ANOVA test, no statistically significant differences were found in the mean values of BMI, WHR, and diastolic blood pressure amongst the groups regarding the duration of the consumption of the pills (p ≥ 0.05), while there were comprehensible differences in the systolic blood pressure amongst the groups regarding the pills-usage duration. Tukey’s test proved that the maximum mean systolic blood pressure was seen amongst the women consuming the pills for 4-23 and 24-36 months (p = 0.05).
The average incidence rates of risk factors for increasing cardiovascular diseases amongst the participants are displayed in Table III. There were no remarkable differences in the mean values of the NO and HDL levels amongst the groups regarding the duration of the consumption of LD contraceptive pills according to the ANOVA test. However, there were comprehensible differences in the mean values of LDL, HCY, cholesterol, and triglyceride levels between the groups due to the difference in the duration of the consumption of LD contraceptive pills statistically. Tukey’s test proved that the mean values of LDL (p = 0.02), cholesterol (p = 0.01), and triglyceride (p < 0.001) levels amongst the users of the pills for 24-36 months and the mean value of HCY level among the users for 4-23 and 24-36 months were higher than the mean values of those levels amongst the other corresponding person (p < 0.001).


- Discussion
The present study indicated that there was a comprehensible difference in the mean value of the plasma level of HCY due to the difference in the duration of the pill consumption. A study carried out by Fallah and colleagues on 100 women with/without a history of consuming the pills in Tehran, Iran, showed a result compatible with ours (12).
The results proved that although the mean values of NO and HDL-c levels among the women using the pills for the longest period were high, there were no significant differences in comparison with the other groups in this regard. According to other findings, the mean values of triglyceride, cholesterol, and LDL-c levels among the women consuming the pills for the longest time were high, which in this finding was comprehensible amongst the users of the pills statistically. Moreover, the study accomplished by Emokpae and colleagues to investigate the influence of long-term usage of the pills on lipid profiles showed results compatible with our results (25). Contrasting to this study, a study by Guazzelli to investigate lipid profiles revealed that the duration of the pill consumption made no statistically significant changes in this regard (30). Dissimilar to the conducted studies, examining the influence of OCPs for a short period of time, investigating the effects on women attending only one public health clinic, and also considering no difference between the prescribed pills, the current study has some strengths as follows: only LD contraceptive pills were used for a long time and they were given to the women who attended several public health clinics.
There were also some limitations in this study. First, the limitation of costs for this project due to which the study was conducted on a relatively small population. Therefore, some relationships were not detected due to the low sample size. Second, the study was performed in a limited time so that only one blood sample was taken from each participant regardless of the follicular and luteal phase of the menstrual cycle.
- Conclusion
Acknowledgments
The authors thank the faculty members of the Faculty of Health, Shahid Sadoughy University of Medical Sciences. This study was funded by the Vice Chancellor for Research and Technology of Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Conflict of interests
The authors declare that there is no conflicts of interests.
Type of Study: Original Article |
References
1. Kazemy T, Sharifzadeh Gh. Ten-year changes in mortality and risk factors in acute myocardial infarction in Birjand (1994-2003). Horizon Med Sci 2004; 10: 38-42. (in Persian)
2. Robbins CL, Farr SL, Zapata LB, D'Angelo DV, Callaghan WM. Postpartum contraceptive use among women with a recent preterm birth. Am J Obstet Gynecol 2015; 213: 508. e1-e9. [DOI:10.1016/j.ajog.2015.05.033] [PMID] [PMCID]
3. Alonso de Lecinana M, Egido J. Estrogens as neuroprotectants against ischemic stroke. Cerebrovasc Dis 2006; 21 (Suppl.2): 48-53. [DOI:10.1159/000091703] [PMID]
4. Ribeiro CCM, Shimo AKK, Lopes MHBM, Lamas JLT. Effects of different hormonal contraceptives in women's blood pressure values. Rev Bras Enferm 2018; 71 (suppl.3): 1453-1459. [DOI:10.1590/0034-7167-2017-0317] [PMID]
5. Sbarouni E, Kyriakides ZS, Kremastinos DT. The effect of hormone replacement therapy and simvastatin on plasma homocysteine. J Womens Health (Larchmt) 2005; 14: 154-158. [DOI:10.1089/jwh.2005.14.154] [PMID]
6. Gupta M, Sharma P, Garg G, Kaur K, Bedi GK, Vij A. Plasma homocysteine: an independent or an interactive risk factor for coronary artery disease. Clin Chim Acta 2005; 352: 121-125. [DOI:10.1016/j.cccn.2004.08.005] [PMID]
7. Vasan RS, Beiser A, D'Agostino RB, Levy D, Selhub J, Jacques PF, et al. Plasma homocysteine and risk for congestive heart failure in adults without prior myocardial infarction. JAMA 2003; 289: 1251-1257. [DOI:10.1001/jama.289.10.1251] [PMID]
8. Kannel WB. Overview of hemostatic factors involved in atherosclerotic cardiovascular disease. Lipids 2005; 40: 1215-1220. [DOI:10.1007/s11745-005-1488-8] [PMID]
9. Serapinas D, Boreikaite E, Bartkeviciute A, Bandzeviciene R, Silkunas M, Bartkeviciene D. The importance of folate, vitamins B6 and B12 for the lowering of homocysteine concentrations for patients with recurrent pregnancy loss and MTHFR mutations. Reprod Toxicol 2017; 72: 159-163. [DOI:10.1016/j.reprotox.2017.07.001] [PMID]
10. Ardawi MS, Rouzi AA, Qari MH, Dahlawi FM, Al-Raddadi RM. Influence of age, sex, folate and vitamin B12 status on plasma homocysteine in Saudis. Saudi Med J 2002; 23: 959-968.
11. Mirzaei N, Dehpour AR. Investigation of homocystein plasma level in cholestatic rat and its effect on nitric oxide secretion in liver. Sci J Hamadan Univ Med Sci 2005; 12: 25-34.
12. Merki-Feld GS, Imthurn B, Keller PJ. Effects of two oral contraceptives on plasma levels of nitric oxide, homocysteine, and lipid metabolism. Metabolism 2002; 51: 1216-1221. [DOI:10.1053/meta.2002.34038] [PMID]
13. Merki-Feld GS, Imthurn B, Keller PJ. Effects of two oral contraceptives on plasma levels of nitric oxide, homocysteine, and lipid metabolism. Metabolism 2002; 51: 1216-1221. [DOI:10.1053/meta.2002.34038] [PMID]
14. Mirershadi F, Faghihi M, Dehpour AR. Effect of endogenous nitric oxide on cardiac ischemic preconditioning in rat. Repository of Research and Investigative Information Hormozgan University of Medical Sciences 2009; 14: 13-21. (in Persian)
15. Lussana F, Zighetti M, Bucciarelli P, Cugno M, Cattaneo M. Blood levels of homocysteine, folate, vitamin B6 and B12 in women using oral contraceptives compared to non-users. Thromb Res 2003; 112: 37-41. [DOI:10.1016/j.thromres.2003.11.007] [PMID]
16. Rosendaal FR, Helmerhorst FM, Vandenbroucke JP. Female hormones and thrombosis. Arterioscler Thromb Vasc Biol 2002; 22: 201-210. [DOI:10.1161/hq0202.102318] [PMID]
17. Akbarzadeh M, SHarifi N. Comparison of cardiovascular disease in women with OCP use and without OCP use in hospitals of Shiraz University of Medical Sciences. Iranian Journal of Nursing Research 2013; 8: 19-28.
18. Tuchman E. Women's injection drug practices in their own words: a qualitative study. Harm Reduct J 2015; 12: 6. [DOI:10.1186/s12954-015-0041-6] [PMID] [PMCID]
19. Fallah S, Nouroozi V, Seifi M, Samadikuchaksaraei A, Aghdashi EM. Influence of oral contraceptive pills on homocysteine and nitric oxide levels: As risk factors for cardiovascular disease. J Clin Lab Anal 2012; 26: 120-123. [DOI:10.1002/jcla.21492] [PMID] [PMCID]
20. Kumar A, Palfrey HA, Pathak R, Kadowitz PJ, Gettys TW, Murthy SN. The metabolism and significance of homocysteine in nutrition and health. Nutr Metab (Lond) 2017; 14: 78. [DOI:10.1186/s12986-017-0233-z] [PMID] [PMCID]
21. Eslami A, Lotfaliany M, Akbarpour S, Azizi F, Hadaegh F. Trend of cardiovascular risk factors in the older Iranian population: 2002-2014. Geriatr Gerontol Int 2018; 18: 130-137. [DOI:10.1111/ggi.13154] [PMID]
22. Esmaillzadeh A, Mirmiran P, Azizi F. Waist-to-hip ratio is a better screening measure for cardiovascular risk factors than other anthropometric indicators in Tehranian adult men. Int J Obes Relat Metab Disord 2004; 28: 1325-1332. [DOI:10.1038/sj.ijo.0802757] [PMID]
23. Tohidi M, Assadi M, Dehghani Z, Vahdat K, Emami SR, Nabipour I. High sensitive C-reactive protein and ischemic heart disease, a population- based study. Iran South Med J 2012; 15: 253-262.
24. Saw SM, Yuan JM, Ong CN, Arakawa K, Lee HP, Coetzee GA, et al. Genetic, dietary, and other lifestyle determinants of plasma homocysteine concentrations in middle-aged and older Chinese men and women in Singapore. Am J Clin Nutr 2001; 73: 232-239. [DOI:10.1093/ajcn/73.2.232] [PMID]
25. Emokpae MA, Uadia PO, Osadolor HB. Effect of duration of use of hormonal contraceptive pills on total lipid and lipoproteins in Nigerian women. Int J Pharm Biol Sci 2010; 1: 1-5.
26. Grossman D, Fuentes L. Over-the-counter access to oral contraceptives as a reproductive healthcare strategy. Curr Opin Obstet Gynecol 2013; 25: 500-505. [DOI:10.1097/GCO.0000000000000019] [PMID]
27. Azizi F, Ainy E, Mirmiran P, Habibian S. Contraceptive methods and risk factors of cardiovascular diseases in Tehranian women: Tehran Lipid and Glucose Study. Eur J Contracept Reprod Health Care 2002; 7: 1-6. [DOI:10.1080/ejc.7.1.1.6] [PMID]
28. Lech MM, Ostrowska L. Effects of low-dose OCs on weight in women with central European nutritional habits and lifestyle. Contraception 2002; 66: 159-162. [DOI:10.1016/S0010-7824(02)00352-9]
29. Pelkman CL, Chow M, Heinbach RA, Rolls BJ. Short - term effects of a progestational contraceptive drug on food intake, resting energy expenditure, and body weight in young women. Am J Clin Nutr 2001; 73: 19-26. [DOI:10.1093/ajcn/73.1.19] [PMID]
30. Guazzelli CA, Lindsey PC, de Araújo FF, Barbieri M, Petta CA, Aldrighi JM. Evaluation of lipid profile in adolescents during long-term use of combined oral hormonal contraceptives. Contraception 2005; 71: 118-121. [DOI:10.1016/j.contraception.2004.08.002] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |