Wed, Apr 24, 2024
[Archive]
Volume 20, Issue 4 (April 2022)
IJRM 2022, 20(4): 255-272 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Samami E, Shahhosseini Z, Elyasi F. The effects of psychological interventions on menopausal hot flashes: A systematic review. IJRM 2022; 20 (4) :255-272
URL: http://ijrm.ir/article-1-1830-en.html
URL: http://ijrm.ir/article-1-1830-en.html
1- Student Research Committee, Mazandaran University of Medical Sciences, Sari, Iran.
2- Sexual and Reproductive Health Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
3- Psychiatry and Behavioral Sciences Research Center, Sexual and Reproductive Health Research Center, Addiction Institute, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran. , Forouzan.elyasi@gmail.com
2- Sexual and Reproductive Health Research Center, Mazandaran University of Medical Sciences, Sari, Iran.
3- Psychiatry and Behavioral Sciences Research Center, Sexual and Reproductive Health Research Center, Addiction Institute, School of Medicine, Mazandaran University of Medical Sciences, Sari, Iran. , Forouzan.elyasi@gmail.com
Full-Text [PDF 829 kb]
(769 Downloads)
| Abstract (HTML) (1141 Views)
1. Introduction
Menopause is a normal physiological phenomenon in women aged 47-55 yr (1, 2). It is often closely identified with common symptoms such as anxiety, depression, stress, mood disorders, sexual concerns, night sweats, and in particular hot flashes (HFs) (1, 3-6). HFs represents the most common complication of menopause, with a prevalence rate of 20-80% (7-9). HFs are a sudden feeling of warmth in the upper body, including the face, neck, and chest, which may spread to the legs (5). This symptom of menopausal transition often results in a high resting heart rate, fatigue, nausea, increased metabolism, and anxiety (8). Studies show that some women might experience HFs for more than 20 yr. Therefore, it is of paramount importance to focus attention on this issue in women’s health (8, 10).
According to the literature, various methods can improve HFs in postmenopausal women, including hormone therapy (9, 11, 12) along with the use of non-hormonal medications (e.g., clonidine and gabapentin) (8, 13), medicinal herbs (e.g., black cohosh) (14), complementary medicine (15) and psychological interventions such as cognitive behavioral therapy (CBT) (16-22), mindfulness-based stress reduction (MBSR) (23, 24), and hypnotherapy (5, 8, 25). Studies in this line have demonstrated that hormone therapy is the principal treatment for HFs in postmenopausal women. However, its continuous use might increase the risk of breast cancer, cardiovascular diseases, stroke, venous complications, and thromboembolism (4, 5). Non-hormonal treatments might lead to potential side effects and incur considerable costs in the long term (8). Concerning these complications and risks, women tend to benefit from non-pharmacological treatments such as complementary medicine and psychological interventions (7, 26).
Studies have shown that the use of psychological interventions such as CBT, MBSR, and hypnotherapies lessen the frequency and severity of HFs, enhance sleep quality, and reduce night sweats, depression, and anxiety in postmenopausal women (4, 8, 24, 27). However, some surveys have suggested that psychological interventions might fail to lessen HFs or improve menopause symptoms even though their results have been non-significant (20, 22, 28). The lack of significant findings can be attributed to different measurement tools and small sample sizes.
As the results of these studies regarding the effects of psychological interventions on menopausal HFs are contradictory, a structured, systematic review was conceived as one way to overcome these inconsistencies since it brings together a series of related investigations and allows readers to consider the results of multiple studies on the same topic simultaneously (29, 30). A comprehensive overview of the available literature in this field indicated that previous systematic reviews had solely evaluated the effects of non-pharmacological treatments (31), medicinal plants (14), and relaxation techniques (32) on HFs and other symptoms of menopause. Accordingly, no specific assessment has been performed on the effects of psychological interventions, to the best of the authors’ knowledge. With this background in mind, this systematic review aimed to investigate the effects of psychological interventions on menopausal HFs.
2. Materials and Methods
2.1. Research question
This study was a systematic review carried out based on the performed reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (33, 34). In addition, this systematic review addressed the following question: are psychological interventions effective in reducing menopausal HFs?
2.2. Search strategy
To find all the electronic articles published from January 2000 to June 2019, the databases of Google Scholar, Scopus, PubMed, Web of Science, Science Direct, the Cochrane Library, and Scientific Information Database were searched. The list of the studies retrieved was manually searched to extract the ones with related topics. The last search was done on June 22, 2019. The researchers also used the following English keywords or their Persian equivalents regarding the Boolean searching operators: (‘Menopause’ OR ‘Premenopausal’ OR ‘Post Menopause’ OR ‘Climacteric’) AND (‘Hot Flashes’ OR ‘Vasomotor Symptoms’ OR ‘Menopause Symptoms’) AND (‘Intervention’ OR ‘Psychological Intervention’ OR ‘Supportive Intervention’ OR ‘Cognitive Behavioral Therapy’ OR ‘Mindfulness’ OR ‘Psychotherapy’ OR ‘Behavior Therapy’ OR ‘Relaxation’ OR ‘Hypnosis’).
2.3. Study selection
At this stage, all the articles related to the research question were extracted through a systematic and advanced search. The irrelevant articles were recognized based on their titles, abstracts, and full texts upon eliminating the duplicates. Article selection was done by 2 independent researchers (F.E and E.S) and in the case of a disagreement, the third researcher made the final decision (Z. Sh). All the studies considered for this systematic review met the following inclusion criteria: clinical or quasi-experimental clinical trials published, which focused on the effects of psychological interventions on menopausal HFs (naturally or surgically induced), reported sample size, and reported results of interventions. Articles about HFs in women with cancer and chemotherapy-induced menopause, those in languages other than English and Persian, and the studies whose abstracts had been presented at conferences without their full texts were excluded from this review.
2.4. Data extraction and quality assessment
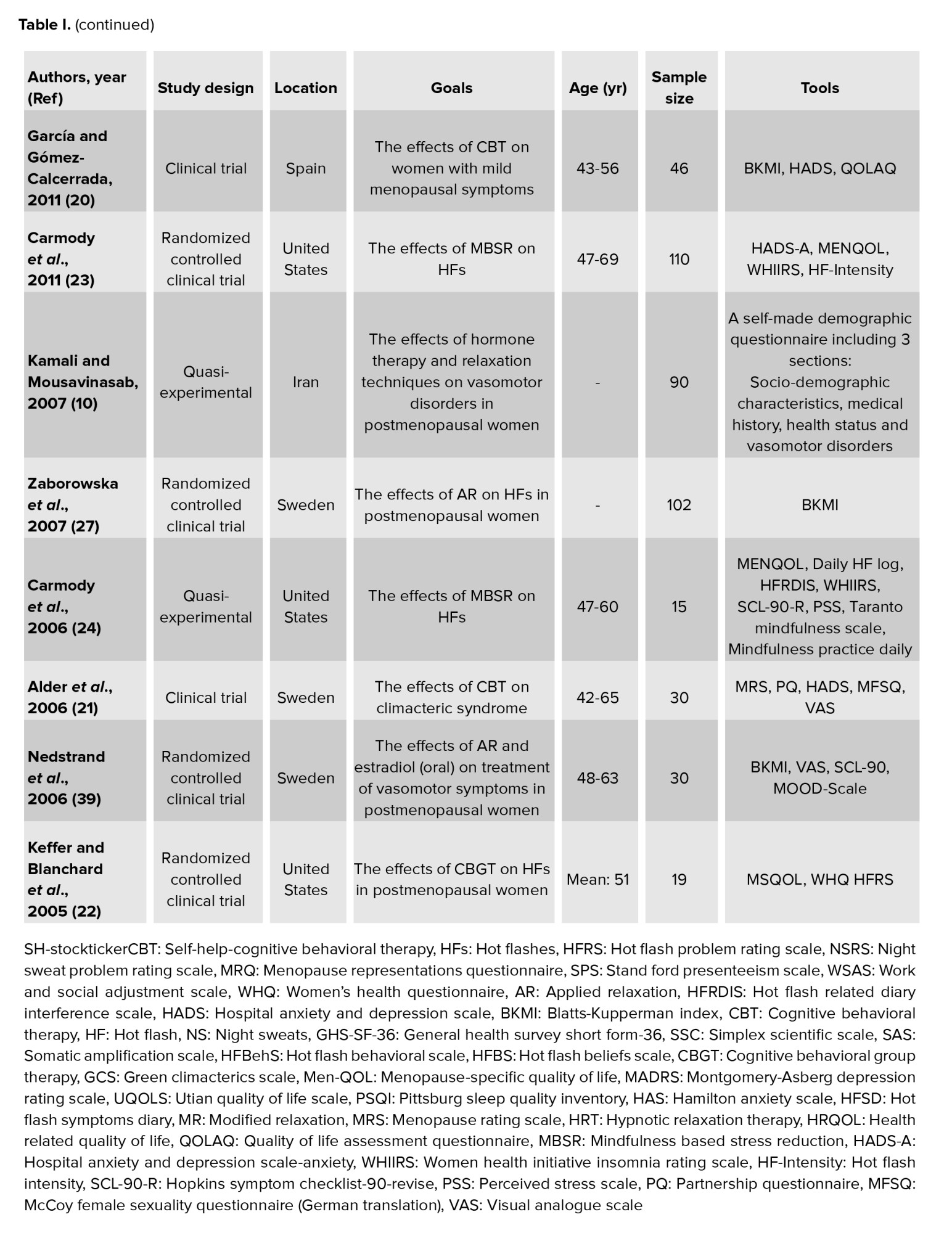
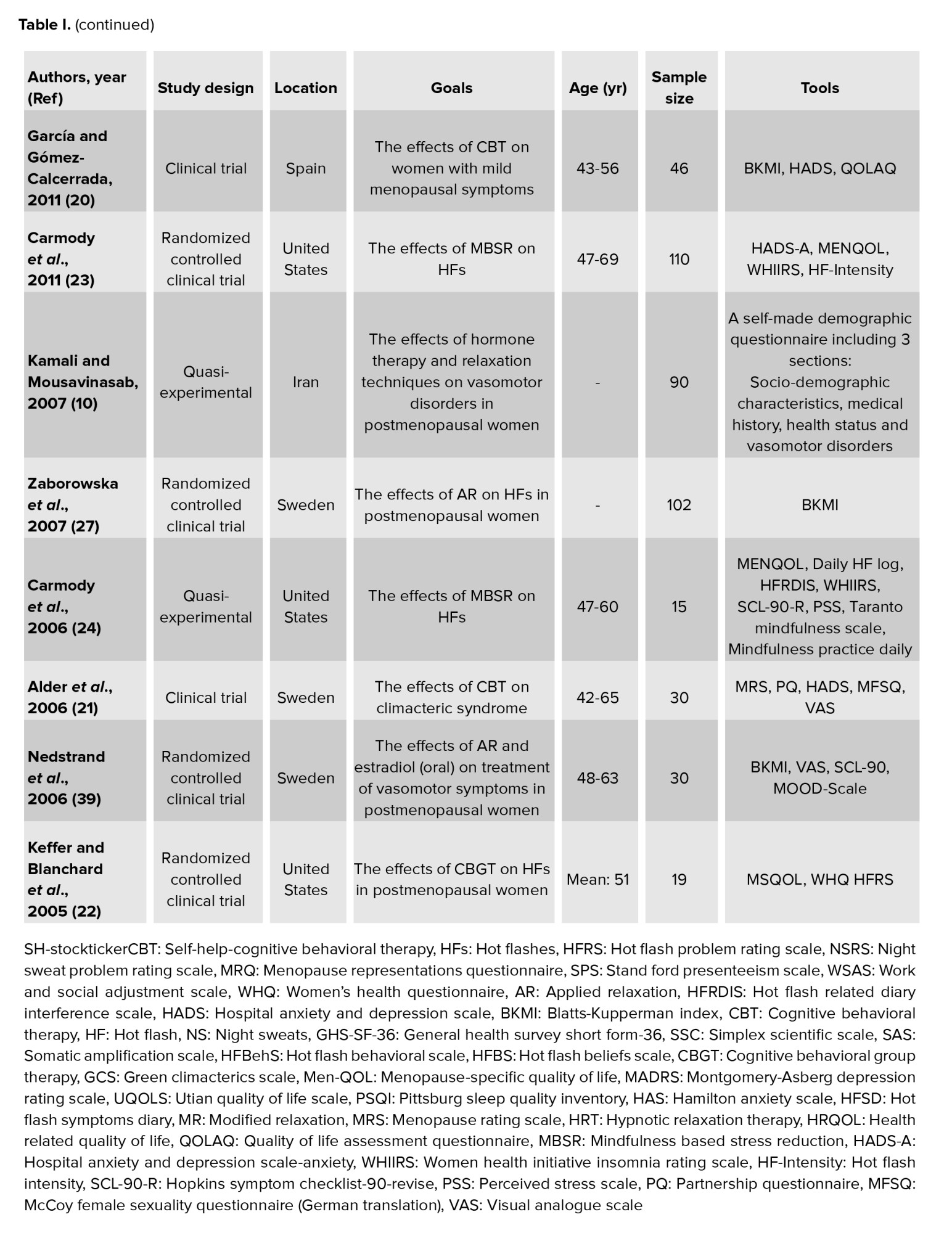
The data including authors’ names, year, study design, location, goals, age, sample size, tools, type of interventions, duration of intervention, follow-up, outcomes, and results were extracted following the abstracts’ assessment and review, and full texts of the eligible articles. Finally, the extracted data were classified and reported as a systematic review and illustrated in tables I and II.
The risk of bias of the included articles was assessed with the Cochrane collaboration tool (35, 36). The risk of bias was assessed for each study using the following 7 items: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and anything else ideally prespecified (other bias). Each item was classified as low risk, high risk, and unclear. Finally, overall rating of risk of bias is as follows: the study has low risk of bias for all items (low risk); the study has high risk of bias in at least one items for this result (high risk); and the study has to raise some concerns in at least one items for this result, but not to be at high risk of bias for any items (unclear) (35-38).

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
2.5. Ethical considerations
This is a systematic review registered in Mazandaran University of Medical Sciences (Grant number: 5824) and the Iran National Committee for Ethics in Biomedical Research, Sari, Iran (Code: IR.MAZUMS.REC.1398.1080).
3. Results
3.1. Search results and descriptions of articles
At the first stage, 20,843 articles were obtained by searching the databases, and 4 articles were found manually. However, 197 articles remained once the duplicate and unrelated studies were eliminated. In the end, 134 and 44 articles were respectively excluded after reviewing their abstracts and reading their full texts, which led to the remaining 19 articles (Figure 1).
3.2. Article review and study participants
The subjects recruited in the selected articles were women who presented with the symptoms of HFs, at premenopausal, menopausal, and postmenopausal stages. Moreover, the participants’ age range was 18-77 yr. (age was not been mentioned in 2 studies (10, 27)).
3.3. Interventions
3.3.1. CBT
CBT is a structured, short-term, and skills-focused psychotherapy and it is a combination of cognitive and behavioral therapies. The main approach in this treatment gives priority to the role of thoughts, beliefs, maladaptive perceptions, and cognitions to attain compatible thoughts and behaviors (4, 39). 4 studies with high quality (low risk) in this systematic review evaluated the effects of CBT on menopausal HFs (4, 7, 16-22), which involved 4-10 intervention sessions held for 1.5-2 hr. The intervention sessions also provided psychoeducation about menopause and HFs, stress management, problem-solving, cognitive and behavioral strategies to help manage HFs, relaxation techniques, breathing techniques, Kegel exercises, as well as identification and control of excessive worries and irrational beliefs.
3.3.2. MBSR
Mindfulness represents a meditation style that underlines the importance of awareness at the present moment (40). MBSR is a structured group program that uses mindfulness meditation to understand, evaluate, and deal with chronic diseases and their symptoms (24). In this review, one study with high quality (low risk) reflected on the effects of MBSR on HFs in postmenopausal women. 7 weekly sessions (one session per wk) were held for 2.5 hr, and one session (morning and evening) was organized at the end of the 6th wk (24). During the intervention sessions, the actions included body scan meditation, intention-setting meditation, and mindfulness-stretching exercises to develop awareness (mindfulness) during movements. Besides, all of participants in the study received CDs as guided instructions for practiced mindfulness at home for 45 min, 6 days a wk.
3.3.3. Hypnotherapy
Hypnotherapy refers to one of the psychological interventions and transient states caused by changes in accuracy and focus. This notion includes changes in consciousness and memory, increased sensitivity, inclusiveness, and imaginations that would not normally be possible (8, 40). One study with high quality (low risk) in this systematic review assessed the impacts of hypnotherapy on HFs in postmenopausal women (5, 8, 25). In this study, 5 weekly intervention sessions (one session per wk) were held for 45 min. Hypnotic interventions also included induction and instruction in self-hypnosis practices towards the therapeutic goals of reduction of HFs. The participants were provided with a hypnotic suggestion for mental imagery involving coolness, safe-place imagery, hypnotic relaxation, and symptom reduction. Moreover, they were given a CD containing information about HFs for use as a home guide.
3.3.4. Relaxation techniques
Relaxation is a simple, beneficial, and executable technique in behavior therapy that can be easily performed with simple training (40). Accordingly, applied relaxation (AR) is one type of relaxation practiced in different uncomfortable situations with quick relaxation and proper breathing (28). In this review, 3 studies with high quality (low risk) evaluated the effects of relaxation techniques on menopause-induced HFs (10, 26-28, 41). In 3 articles, 12 weekly intervention sessions (one session per wk) were held for 60 min (26, 27, 41). Another study included 5 group sessions (every other day) and one month of daily relaxation practices at home (10). The intervention sessions further provided information about menopause, theories about HFs, progressive relaxation, differential relaxation, fast relaxation, release-only relaxation, application development training, and conservation programs aimed at coping with vasomotor symptoms such as HFs.
3.4. Tools
The outcome of HFs in postmenopausal women was measured in all of the studies. Only one study implemented a researcher-made questionnaire to assess this condition (10), and the rest utilized various standard tools. In this context, 6 studies used the Hot Flash Related Daily Interference Scale (4, 5, 8, 24, 25, 28), and 5 studies applied the Hot Flash Rating Scale (7, 17-19, 22). On the other hand, 4 studies implemented the Blatt and Kupperman Menopausal Index (16, 20, 27, 41), whereas 2 articles administered the Menopause Rating Scale (21, 26). Furthermore, 2 studies employed the Hot Flash Symptom Diary (8, 25) while one study applied the Hot Flash-Intensity scores (23).
3.5. Article quality assessment
The results of the quality assessment of the 19 articles conducted from 2005-2018 (18 in English and one in Persian) based on the Cochrane collaboration tool for assessing the risk of bias are presented in figures 2 and 3. The 2 reviewers (F.E, E.S) had good agreement, and any discrepancies were resolved following discussion. 6 studies had a high risk of bias in random sequence generation and allocation concealment (selection bias) (5, 16, 18, 20, 21, 39). The category of blinding participants and personnel (performance bias) was rated as at a high risk of bias in 3 studies (5, 21, 39) and low risk of bias in eleven studies (4, 7, 8, 10, 17, 19, 22- 24, 26, 27). Eleven studies had a low risk of bias in the blinding outcome assessment (detection bias) (4, 7, 8, 10, 17, 19, 22- 24, 26, 27). The category of incomplete outcome data (attrition bias) was rated as at a high risk of bias in 4 studies (7, 23, 28, 39). Only one study was unclear in incomplete outcome data (attrition bias) and selective reporting (reporting bias) (25). Finally, from the 19 articles, 9 studies were assessed as low risk (4, 8, 10, 17, 19, 22, 24, 26, 27), 9 studies had high risk (5, 7, 16, 18, 20, 21, 23, 28, 39), and one study had an unclear risk of bias (25).



4. Discussion
This systematic review was performed on 19 studies to evaluate the effects of psychological interventions on menopausal HFs. This was a review of studies related to various psychological interventions conducted with menopausal women. From the 19 studies, 9 studies were of a high quality and low risk of bias.
In this review and according to previous studies (7, 18, 19), CBT improved and decreased the frequency of HFs in postmenopausal women by altering thoughts and behaviors, and through a particular focus on vasomotor symptoms and HFs (4, 17).
In the present review, MBSR was also recognized as an efficient intervention targeting HFs in postmenopausal women. According to this study, MBSR decreased the frequency of daily HFs by focusing on body scan meditation and mindfulness-stretching exercises to develop awareness (24).
In this review, hypnotherapy was documented as another useful method to mitigate menopausal HFs. Hypnotherapy reduced the symptoms of vasomotor disorders and HFs through making changes in physiological responses to mental distress (25).
Relaxation was also one of the cognitive interventions affecting HFs in this review. The results of the studies showed that AR led to subsided HFs in postmenopausal women. As mentioned earlier, the findings of the studies demonstrated that relaxation, especially AR (as one the most common techniques), could moderate the frequency of HFs in postmenopausal women by moderating the sympathetic nervous system (10, 27).
The results of the included studies were fairly consistent and there was a statistically significant improvement in HF symptoms in almost all of them (4, 8, 10, 17, 19, 24, 26, 27). However, some studies were underpowered considering their small sample sizes (4, 5, 8, 22). In addition, the studies had a high risk of bias because the effects of psychological interventions are relatively influenced by the patient-therapist relationship.
The assessment of outcomes performed in some of the studies involved the comparison of a baseline assessment with a post-intervention assessment; changes found in these studies may have been due to the placebo effect (8, 27). Loprinzi et al. found that placebo administration for 4 wk alleviated HFs by approximately 30% (42). Another question was related to the control group: was it enough to provide them with the usual care, or should the control group have had equal contact time as the experimental group? The answer to this question is unclear. Another potential confounding factor in this review was the time effect, because HFs decrease in frequency and intensity over time (43). To reduce the effect of this potential confounding factor, instead of using a control group, the researcher could measure the outcome at 2 different pre-intervention time points to obtain 2 baseline assessments (44).
One of the main and important problems with evaluating the effectiveness of psychological interventions for HFs is the methodological quality of the published articles, which was of impartial or poor quality and therefore precluded corrects conclusions. In order to increase internal validity, it is useful to report accurate and precise information in the study (such as the number and causes of loss to follow-up and treatment equivalence beside the trial intervention) based on the Consolidated Standards of Reporting Trial recommendations (45). Differences in outcome assessment tools used in the different studies also made it difficult to compare the results. The use of valid outcome assessment tools in all studies is crucial to ensure good external validity. Blinding of outcome assessments is another essential design feature that was often not achieved or not reported in the articles. Therefore, effective analysis was not possible due to some degree of potential bias.
According to the studies’ results and the consistency of the results in the follow-ups, the CBT (4, 17, 19) and relaxation techniques (10, 26, 27) were recommended as effective low-risk treatments to reduce and improve menopausal HFs and their related symptoms. Although the results of the studies showed that MBSR (24) and hypnosis (8) therapies improved and decreased HFs in postmenopausal women as well, only one study assessed their effectiveness, which shows the need for more interventional studies on the impact of these interventions on HFs in postmenopausal women. It is necessary to mention, psychological therapies have been shown to be effective in treating other psychiatric disorders such as fibromyalgia and tocophobia (46, 47).
4.1. Suggestions
There is limited evidence for the impact of effective psychological therapies on symptoms of post-menopausal women. Previous studies have however shown that HF symptoms in breast cancer survivors are more common, severe and distressing than in women who have not had cancer (48, 49). Therefore, one of our suggestions is to compile a review article evaluating the effects of psychological interventions on HFs in breast cancer survivors. Further assessment on the effects of these interventions on HFs and other symptoms of menopause with high quality studies, such as randomized controlled trials, is another suggestion of this study. In addition, there is insufficient evidence to guide clinical practice for physicians, and conducting high-quality studies can be a step towards developing these guidelines.
4.2. Clinical implications
These interventions, performed by trained health professionals, provide additional treatment options for menopausal symptoms. CBT and relaxation techniques are a low-risk treatment for HFs.
4.3. Strengths and limitations
The major strength of this study was that it was a systematic review performed based on the reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. Another strength was the use of a comprehensive search strategy in electronic databases. One of the main limitations of this study was the low number of high-quality studies available for this review. In addition, many of these studies had a high risk of bias due to the absence of adequate blinding. This bias is often an integral part of psychological studies, although evaluators may be blinded for treatment. Also, conducting a meta-analysis was impossible due to differences in and heterogeneity of the studies.
5. Conclusion
Based on the findings of this systematic review, psychological interventions, especially CBT and relaxation techniques are potentially effective for reducing vasomotor symptoms and HFs in healthy postmenopausal women, although the quality of published research on this topic is sometimes questionable.
Acknowledgments
This project was supported by Mazandaran University of Medical Sciences, Sari, Iran (Grant number: 5824). The authors are grateful to the Student Research Committee of Mazandaran University of Medical Sciences for financially supporting the protocol of this systematic review.
Conflicts of Interest
The authors declare that there is no conflict of interest.
Full-Text: (184 Views)
1. Introduction
Menopause is a normal physiological phenomenon in women aged 47-55 yr (1, 2). It is often closely identified with common symptoms such as anxiety, depression, stress, mood disorders, sexual concerns, night sweats, and in particular hot flashes (HFs) (1, 3-6). HFs represents the most common complication of menopause, with a prevalence rate of 20-80% (7-9). HFs are a sudden feeling of warmth in the upper body, including the face, neck, and chest, which may spread to the legs (5). This symptom of menopausal transition often results in a high resting heart rate, fatigue, nausea, increased metabolism, and anxiety (8). Studies show that some women might experience HFs for more than 20 yr. Therefore, it is of paramount importance to focus attention on this issue in women’s health (8, 10).
According to the literature, various methods can improve HFs in postmenopausal women, including hormone therapy (9, 11, 12) along with the use of non-hormonal medications (e.g., clonidine and gabapentin) (8, 13), medicinal herbs (e.g., black cohosh) (14), complementary medicine (15) and psychological interventions such as cognitive behavioral therapy (CBT) (16-22), mindfulness-based stress reduction (MBSR) (23, 24), and hypnotherapy (5, 8, 25). Studies in this line have demonstrated that hormone therapy is the principal treatment for HFs in postmenopausal women. However, its continuous use might increase the risk of breast cancer, cardiovascular diseases, stroke, venous complications, and thromboembolism (4, 5). Non-hormonal treatments might lead to potential side effects and incur considerable costs in the long term (8). Concerning these complications and risks, women tend to benefit from non-pharmacological treatments such as complementary medicine and psychological interventions (7, 26).
Studies have shown that the use of psychological interventions such as CBT, MBSR, and hypnotherapies lessen the frequency and severity of HFs, enhance sleep quality, and reduce night sweats, depression, and anxiety in postmenopausal women (4, 8, 24, 27). However, some surveys have suggested that psychological interventions might fail to lessen HFs or improve menopause symptoms even though their results have been non-significant (20, 22, 28). The lack of significant findings can be attributed to different measurement tools and small sample sizes.
As the results of these studies regarding the effects of psychological interventions on menopausal HFs are contradictory, a structured, systematic review was conceived as one way to overcome these inconsistencies since it brings together a series of related investigations and allows readers to consider the results of multiple studies on the same topic simultaneously (29, 30). A comprehensive overview of the available literature in this field indicated that previous systematic reviews had solely evaluated the effects of non-pharmacological treatments (31), medicinal plants (14), and relaxation techniques (32) on HFs and other symptoms of menopause. Accordingly, no specific assessment has been performed on the effects of psychological interventions, to the best of the authors’ knowledge. With this background in mind, this systematic review aimed to investigate the effects of psychological interventions on menopausal HFs.
2. Materials and Methods
2.1. Research question
This study was a systematic review carried out based on the performed reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (33, 34). In addition, this systematic review addressed the following question: are psychological interventions effective in reducing menopausal HFs?
2.2. Search strategy
To find all the electronic articles published from January 2000 to June 2019, the databases of Google Scholar, Scopus, PubMed, Web of Science, Science Direct, the Cochrane Library, and Scientific Information Database were searched. The list of the studies retrieved was manually searched to extract the ones with related topics. The last search was done on June 22, 2019. The researchers also used the following English keywords or their Persian equivalents regarding the Boolean searching operators: (‘Menopause’ OR ‘Premenopausal’ OR ‘Post Menopause’ OR ‘Climacteric’) AND (‘Hot Flashes’ OR ‘Vasomotor Symptoms’ OR ‘Menopause Symptoms’) AND (‘Intervention’ OR ‘Psychological Intervention’ OR ‘Supportive Intervention’ OR ‘Cognitive Behavioral Therapy’ OR ‘Mindfulness’ OR ‘Psychotherapy’ OR ‘Behavior Therapy’ OR ‘Relaxation’ OR ‘Hypnosis’).
2.3. Study selection
At this stage, all the articles related to the research question were extracted through a systematic and advanced search. The irrelevant articles were recognized based on their titles, abstracts, and full texts upon eliminating the duplicates. Article selection was done by 2 independent researchers (F.E and E.S) and in the case of a disagreement, the third researcher made the final decision (Z. Sh). All the studies considered for this systematic review met the following inclusion criteria: clinical or quasi-experimental clinical trials published, which focused on the effects of psychological interventions on menopausal HFs (naturally or surgically induced), reported sample size, and reported results of interventions. Articles about HFs in women with cancer and chemotherapy-induced menopause, those in languages other than English and Persian, and the studies whose abstracts had been presented at conferences without their full texts were excluded from this review.
2.4. Data extraction and quality assessment
The data including authors’ names, year, study design, location, goals, age, sample size, tools, type of interventions, duration of intervention, follow-up, outcomes, and results were extracted following the abstracts’ assessment and review, and full texts of the eligible articles. Finally, the extracted data were classified and reported as a systematic review and illustrated in tables I and II.
The risk of bias of the included articles was assessed with the Cochrane collaboration tool (35, 36). The risk of bias was assessed for each study using the following 7 items: random sequence generation and allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and anything else ideally prespecified (other bias). Each item was classified as low risk, high risk, and unclear. Finally, overall rating of risk of bias is as follows: the study has low risk of bias for all items (low risk); the study has high risk of bias in at least one items for this result (high risk); and the study has to raise some concerns in at least one items for this result, but not to be at high risk of bias for any items (unclear) (35-38).

.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
2.5. Ethical considerations
This is a systematic review registered in Mazandaran University of Medical Sciences (Grant number: 5824) and the Iran National Committee for Ethics in Biomedical Research, Sari, Iran (Code: IR.MAZUMS.REC.1398.1080).
3. Results
3.1. Search results and descriptions of articles
At the first stage, 20,843 articles were obtained by searching the databases, and 4 articles were found manually. However, 197 articles remained once the duplicate and unrelated studies were eliminated. In the end, 134 and 44 articles were respectively excluded after reviewing their abstracts and reading their full texts, which led to the remaining 19 articles (Figure 1).
3.2. Article review and study participants
The subjects recruited in the selected articles were women who presented with the symptoms of HFs, at premenopausal, menopausal, and postmenopausal stages. Moreover, the participants’ age range was 18-77 yr. (age was not been mentioned in 2 studies (10, 27)).
3.3. Interventions
3.3.1. CBT
CBT is a structured, short-term, and skills-focused psychotherapy and it is a combination of cognitive and behavioral therapies. The main approach in this treatment gives priority to the role of thoughts, beliefs, maladaptive perceptions, and cognitions to attain compatible thoughts and behaviors (4, 39). 4 studies with high quality (low risk) in this systematic review evaluated the effects of CBT on menopausal HFs (4, 7, 16-22), which involved 4-10 intervention sessions held for 1.5-2 hr. The intervention sessions also provided psychoeducation about menopause and HFs, stress management, problem-solving, cognitive and behavioral strategies to help manage HFs, relaxation techniques, breathing techniques, Kegel exercises, as well as identification and control of excessive worries and irrational beliefs.
3.3.2. MBSR
Mindfulness represents a meditation style that underlines the importance of awareness at the present moment (40). MBSR is a structured group program that uses mindfulness meditation to understand, evaluate, and deal with chronic diseases and their symptoms (24). In this review, one study with high quality (low risk) reflected on the effects of MBSR on HFs in postmenopausal women. 7 weekly sessions (one session per wk) were held for 2.5 hr, and one session (morning and evening) was organized at the end of the 6th wk (24). During the intervention sessions, the actions included body scan meditation, intention-setting meditation, and mindfulness-stretching exercises to develop awareness (mindfulness) during movements. Besides, all of participants in the study received CDs as guided instructions for practiced mindfulness at home for 45 min, 6 days a wk.
3.3.3. Hypnotherapy
Hypnotherapy refers to one of the psychological interventions and transient states caused by changes in accuracy and focus. This notion includes changes in consciousness and memory, increased sensitivity, inclusiveness, and imaginations that would not normally be possible (8, 40). One study with high quality (low risk) in this systematic review assessed the impacts of hypnotherapy on HFs in postmenopausal women (5, 8, 25). In this study, 5 weekly intervention sessions (one session per wk) were held for 45 min. Hypnotic interventions also included induction and instruction in self-hypnosis practices towards the therapeutic goals of reduction of HFs. The participants were provided with a hypnotic suggestion for mental imagery involving coolness, safe-place imagery, hypnotic relaxation, and symptom reduction. Moreover, they were given a CD containing information about HFs for use as a home guide.
3.3.4. Relaxation techniques
Relaxation is a simple, beneficial, and executable technique in behavior therapy that can be easily performed with simple training (40). Accordingly, applied relaxation (AR) is one type of relaxation practiced in different uncomfortable situations with quick relaxation and proper breathing (28). In this review, 3 studies with high quality (low risk) evaluated the effects of relaxation techniques on menopause-induced HFs (10, 26-28, 41). In 3 articles, 12 weekly intervention sessions (one session per wk) were held for 60 min (26, 27, 41). Another study included 5 group sessions (every other day) and one month of daily relaxation practices at home (10). The intervention sessions further provided information about menopause, theories about HFs, progressive relaxation, differential relaxation, fast relaxation, release-only relaxation, application development training, and conservation programs aimed at coping with vasomotor symptoms such as HFs.
3.4. Tools
The outcome of HFs in postmenopausal women was measured in all of the studies. Only one study implemented a researcher-made questionnaire to assess this condition (10), and the rest utilized various standard tools. In this context, 6 studies used the Hot Flash Related Daily Interference Scale (4, 5, 8, 24, 25, 28), and 5 studies applied the Hot Flash Rating Scale (7, 17-19, 22). On the other hand, 4 studies implemented the Blatt and Kupperman Menopausal Index (16, 20, 27, 41), whereas 2 articles administered the Menopause Rating Scale (21, 26). Furthermore, 2 studies employed the Hot Flash Symptom Diary (8, 25) while one study applied the Hot Flash-Intensity scores (23).
3.5. Article quality assessment
The results of the quality assessment of the 19 articles conducted from 2005-2018 (18 in English and one in Persian) based on the Cochrane collaboration tool for assessing the risk of bias are presented in figures 2 and 3. The 2 reviewers (F.E, E.S) had good agreement, and any discrepancies were resolved following discussion. 6 studies had a high risk of bias in random sequence generation and allocation concealment (selection bias) (5, 16, 18, 20, 21, 39). The category of blinding participants and personnel (performance bias) was rated as at a high risk of bias in 3 studies (5, 21, 39) and low risk of bias in eleven studies (4, 7, 8, 10, 17, 19, 22- 24, 26, 27). Eleven studies had a low risk of bias in the blinding outcome assessment (detection bias) (4, 7, 8, 10, 17, 19, 22- 24, 26, 27). The category of incomplete outcome data (attrition bias) was rated as at a high risk of bias in 4 studies (7, 23, 28, 39). Only one study was unclear in incomplete outcome data (attrition bias) and selective reporting (reporting bias) (25). Finally, from the 19 articles, 9 studies were assessed as low risk (4, 8, 10, 17, 19, 22, 24, 26, 27), 9 studies had high risk (5, 7, 16, 18, 20, 21, 23, 28, 39), and one study had an unclear risk of bias (25).



4. Discussion
This systematic review was performed on 19 studies to evaluate the effects of psychological interventions on menopausal HFs. This was a review of studies related to various psychological interventions conducted with menopausal women. From the 19 studies, 9 studies were of a high quality and low risk of bias.
In this review and according to previous studies (7, 18, 19), CBT improved and decreased the frequency of HFs in postmenopausal women by altering thoughts and behaviors, and through a particular focus on vasomotor symptoms and HFs (4, 17).
In the present review, MBSR was also recognized as an efficient intervention targeting HFs in postmenopausal women. According to this study, MBSR decreased the frequency of daily HFs by focusing on body scan meditation and mindfulness-stretching exercises to develop awareness (24).
In this review, hypnotherapy was documented as another useful method to mitigate menopausal HFs. Hypnotherapy reduced the symptoms of vasomotor disorders and HFs through making changes in physiological responses to mental distress (25).
Relaxation was also one of the cognitive interventions affecting HFs in this review. The results of the studies showed that AR led to subsided HFs in postmenopausal women. As mentioned earlier, the findings of the studies demonstrated that relaxation, especially AR (as one the most common techniques), could moderate the frequency of HFs in postmenopausal women by moderating the sympathetic nervous system (10, 27).
The results of the included studies were fairly consistent and there was a statistically significant improvement in HF symptoms in almost all of them (4, 8, 10, 17, 19, 24, 26, 27). However, some studies were underpowered considering their small sample sizes (4, 5, 8, 22). In addition, the studies had a high risk of bias because the effects of psychological interventions are relatively influenced by the patient-therapist relationship.
The assessment of outcomes performed in some of the studies involved the comparison of a baseline assessment with a post-intervention assessment; changes found in these studies may have been due to the placebo effect (8, 27). Loprinzi et al. found that placebo administration for 4 wk alleviated HFs by approximately 30% (42). Another question was related to the control group: was it enough to provide them with the usual care, or should the control group have had equal contact time as the experimental group? The answer to this question is unclear. Another potential confounding factor in this review was the time effect, because HFs decrease in frequency and intensity over time (43). To reduce the effect of this potential confounding factor, instead of using a control group, the researcher could measure the outcome at 2 different pre-intervention time points to obtain 2 baseline assessments (44).
One of the main and important problems with evaluating the effectiveness of psychological interventions for HFs is the methodological quality of the published articles, which was of impartial or poor quality and therefore precluded corrects conclusions. In order to increase internal validity, it is useful to report accurate and precise information in the study (such as the number and causes of loss to follow-up and treatment equivalence beside the trial intervention) based on the Consolidated Standards of Reporting Trial recommendations (45). Differences in outcome assessment tools used in the different studies also made it difficult to compare the results. The use of valid outcome assessment tools in all studies is crucial to ensure good external validity. Blinding of outcome assessments is another essential design feature that was often not achieved or not reported in the articles. Therefore, effective analysis was not possible due to some degree of potential bias.
According to the studies’ results and the consistency of the results in the follow-ups, the CBT (4, 17, 19) and relaxation techniques (10, 26, 27) were recommended as effective low-risk treatments to reduce and improve menopausal HFs and their related symptoms. Although the results of the studies showed that MBSR (24) and hypnosis (8) therapies improved and decreased HFs in postmenopausal women as well, only one study assessed their effectiveness, which shows the need for more interventional studies on the impact of these interventions on HFs in postmenopausal women. It is necessary to mention, psychological therapies have been shown to be effective in treating other psychiatric disorders such as fibromyalgia and tocophobia (46, 47).
4.1. Suggestions
There is limited evidence for the impact of effective psychological therapies on symptoms of post-menopausal women. Previous studies have however shown that HF symptoms in breast cancer survivors are more common, severe and distressing than in women who have not had cancer (48, 49). Therefore, one of our suggestions is to compile a review article evaluating the effects of psychological interventions on HFs in breast cancer survivors. Further assessment on the effects of these interventions on HFs and other symptoms of menopause with high quality studies, such as randomized controlled trials, is another suggestion of this study. In addition, there is insufficient evidence to guide clinical practice for physicians, and conducting high-quality studies can be a step towards developing these guidelines.
4.2. Clinical implications
These interventions, performed by trained health professionals, provide additional treatment options for menopausal symptoms. CBT and relaxation techniques are a low-risk treatment for HFs.
4.3. Strengths and limitations
The major strength of this study was that it was a systematic review performed based on the reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. Another strength was the use of a comprehensive search strategy in electronic databases. One of the main limitations of this study was the low number of high-quality studies available for this review. In addition, many of these studies had a high risk of bias due to the absence of adequate blinding. This bias is often an integral part of psychological studies, although evaluators may be blinded for treatment. Also, conducting a meta-analysis was impossible due to differences in and heterogeneity of the studies.
5. Conclusion
Based on the findings of this systematic review, psychological interventions, especially CBT and relaxation techniques are potentially effective for reducing vasomotor symptoms and HFs in healthy postmenopausal women, although the quality of published research on this topic is sometimes questionable.
Acknowledgments
This project was supported by Mazandaran University of Medical Sciences, Sari, Iran (Grant number: 5824). The authors are grateful to the Student Research Committee of Mazandaran University of Medical Sciences for financially supporting the protocol of this systematic review.
Conflicts of Interest
The authors declare that there is no conflict of interest.
Type of Study: Review Article |
Subject:
Reproductive Psycology
References
1. Najaf Najafi M, Dadgar S, Ghazanfarpour M. The effect of aromatherapy on quality of sleep in pre-post-menopausal women: A systematic review and meta-analysis. Iran J Obstet Gynecol Infertil 2018; 21 (Suppl.): 1-9. [DOI:10.1080/13697137.2018.1472566] [PMID]
2. Azizi M, Fooladi E, Abdollahi F, Elyasi F. Biopsychosocial risk factors of depression in the menopausal transition: A narrative review. Iran J Psychiatry Behav Sci 2018; 12: e12928. [DOI:10.5812/ijpbs.12928]
3. Weidner K, Croy I, Siepmann T, Brähler E, Beutel M, Bittner A. Menopausal syndrome limited to hot flushes and sweating a representative survey study. J Psychosom Obstet Gynecol 2017; 38: 170-179. [DOI:10.1080/0167482X.2017.1291624] [PMID]
4. Green SM, Haber E, McCabe RE, Soares CN. Cognitive-behavioral group treatment for menopausal symptoms: A pilot study. Arch Womens Ment Health 2013; 16: 325-332. [DOI:10.1007/s00737-013-0339-x] [PMID]
5. Elkins G, Johnson A, Fisher W, Sliwinski J, Keith T. A pilot investigation of guided self-hypnosis in the treatment of hot flashes among postmenopausal women. Int J Clin Exp Hypn 2013; 61: 342-350. [DOI:10.1080/00207144.2013.784112] [PMID]
6. Khani S, Azizi M, Elyasi F, Kamali M, Moosazadeh M. The prevalence of sexual dysfunction in the different menopausal stages: A systematic review and meta-analysis. Int J Sex Health 2021; 33: 439-472. [DOI:10.1080/19317611.2021.1926039]
7. Hardy C, Griffiths A, Norton S, Hunter MS. Self-help cognitive behavior therapy for working women with problematic hot flushes and night sweats (MENOS@ Work): A multicenter randomized controlled trial. Menopause 2018; 25: 508-519. [DOI:10.1097/GME.0000000000001048] [PMID]
8. Elkins GR, Fisher WI, Johnson AK, Carpenter JS, Keith TZ. Clinical hypnosis in the treatment of post-menopausal hot flashes: A randomized controlled trial. Menopause 2013; 20: 291-298. [DOI:10.1097/gme.0b013e31826ce3ed] [PMID] [PMCID]
9. Chiang C, Gallicchio L, Zacur H, Miller S, Flaws JA, Smith RL. Hormone variability and hot flash experience: Results from the midlife women's health study. Maturitas 2019; 119: 1-7. [DOI:10.1016/j.maturitas.2018.10.007] [PMID] [PMCID]
10. Kamali S, Mosavinasab SNAD. Differential effectiveness of hormone replacement therapy and relaxation techniques on consequences of menopause vasomotor symptoms. J Inflamamt Dis 2007; 11: 34-40.
11. Arizanović Z, Vujović S, Ivović M, Tančić-Gajić M, Marina L, Stojanović M, et al. Hot flash values of gonadotropins and estradiol in menopause. Srp Arh Celok Lek 2018; 146: 403-406. [DOI:10.2298/SARH160303012A]
12. Brockie J. Managing menopausal symptoms: Hot flushes and night sweats. Nurs Stand 2013; 28: 48-53. [DOI:10.7748/ns2013.11.28.12.48.e8067] [PMID]
13. McGarry K, Geary M, Gopinath V. Beyond estrogen: Treatment options for hot flashes. Clin Ther 2018; 40: 1778-1786. [DOI:10.1016/j.clinthera.2018.08.010] [PMID]
14. Kashani L, Khajuei Kermani F, Akhondzadeh S. [The efficacy of herbal medicines for treatment of hot flash: A systematic review]. J Med Plants 2017; 4: 1-20. (in Persian)
15. Buchanan DT, Landis CA, Hohensee Ch, Guthrie KA, Otte JL, Paudel M, et al. Effects of yoga and aerobic exercise on actigraphic sleep parameters in menopausal women with hot flashes. J Clin Sleep Med 2017; 13: 11-18. [DOI:10.5664/jcsm.6376] [PMID] [PMCID]
16. Larroy C, Marin C, Gutiérrez S. The effects of cognitive-behavioral techniques on hot flushes, depression and anxiety related to menopause in Spanish women. Wulfenia 2015; 22: 31-43.
17. Norton S, Chilcot J, Hunter MS. Cognitive-behavior therapy for menopausal symptoms (hot flushes and night sweats): Moderators and mediators of treatment effects. Menopause 2014; 21: 574-578. [DOI:10.1097/GME.0000000000000095] [PMID]
18. Stefanopoulou E, Hunter M. Telephone-guided self-help cognitive behavioural therapy for menopausal symptoms. Maturitas 2014; 77: 73-77. [DOI:10.1016/j.maturitas.2013.09.013] [PMID]
19. Ayers B, Smith M, Hellier J, Mann E, Hunter MS. Effectiveness of group and self-help cognitive behavior therapy in reducing problematic menopausal hot flushes and night sweats (MENOS 2): A randomized controlled trial. Menopause 2012; 19: 749-759. [DOI:10.1097/gme.0b013e31823fe835] [PMID]
20. García CL, Gómez-Calcerrada SG. Cognitive-behavioral intervention among women with slight menopausal symptoms: A pilot study. Span J Psychol 2011; 14: 344-355. [DOI:10.5209/rev_SJOP.2011.v14.n1.31] [PMID]
21. Alder J, Besken KE, Armbruster U, Decio R, Gairing A, Kang A, et al. Cognitive-behavioural group intervention for climacteric syndrome. Psychother Psychosom 2006; 75: 298-303. [DOI:10.1159/000093951] [PMID]
22. Keefer L, Blanchard EB. A behavioral group treatment program for menopausal hot flashes: Results of a pilot study. Appl Psychophysiol Biofeedback 2005; 30: 21-30. [DOI:10.1007/s10484-005-2171-1] [PMID]
23. Carmody JF, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: Results of a randomized trial. Menopause 2011; 18: 611-620. [DOI:10.1097/gme.0b013e318204a05c] [PMID] [PMCID]
24. Carmody J, Crawford S, Churchill L. A pilot study of mindfulness-based stress reduction for hot flashes. Menopause 2006; 13: 760-769. [DOI:10.1097/01.gme.0000227402.98933.d0] [PMID]
25. Kendrick C, Johnson AK, Sliwinski J, Patterson V, Fisher WI, Elkins GR, et al. Hypnotic relaxation therapy for reduction of hot flashes in postmenopausal women: Examination of cortisol as a potential mediator. Int J Clin Exp Hypn 2015; 63: 76-91. [DOI:10.1080/00207144.2014.931169] [PMID]
26. Saensak S, Vutyavanich T, Somboonporn W, Srisurapanont M. Effectiveness of a modified version of the applied relaxation technique in treatment of perimenopausal and postmenopausal symptoms. Int J Womens Health 2013; 5: 765-771. [DOI:10.2147/IJWH.S53652] [PMID] [PMCID]
27. Zaborowska E, Brynhildsen J, Damberg S, Fredriksson M, Lindh-Åstrand L, Nedstrand E, et al. Effects of acupuncture, applied relaxation, estrogens and placebo on hot flushes in postmenopausal women: An analysis of two prospective, parallel, randomized studies. Climacteric 2007; 10: 38-45. [DOI:10.1080/13697130601165059] [PMID]
28. Lindh-Åstrand L, Holm ACS, Sydsjö G, Andersson G, Carlbring P, Nedstrand E. Internet-delivered applied relaxation for vasomotor symptoms in postmenopausal women: Lessons from a failed trial. Maturitas 2015; 80: 432-434. [DOI:10.1016/j.maturitas.2015.01.010] [PMID]
29. Samami E, Elyasi F, Mousavinasab SN, Shojaee L, Zaboli E, Shahhosseini Z. Effect of non-pharmacological interventions on stress of women with breast cancer undergoing chemotherapy: A systematic review. J Mazandaran Univ Med Sci 2019; 29: 167-180.
30. Samami E, Elyasi F, Mousavi Nasab N, Shojaee L, Zaboli E, Shahhosseini Z. Coping strategies-oriented interventions in breast cancer women: A systematic scoping review of the quantitative evidence. Iran J Psychiatry Behav Sci 2020; 14: e99884. [DOI:10.5812/ijpbs.99884]
31. Tong IL. Nonpharmacological treatment of postmenopausal symptoms. Obstet Gynaecol 2013; 15: 19-25. [DOI:10.1111/j.1744-4667.2012.00143.x]
32. Saensak S, Vutyavanich T, Somboonporn W, Srisurapanont M. Relaxation for perimenopausal and postmenopausal symptoms. Cochrane Database Syst Rev 2014; 7: 1-15. [DOI:10.1002/14651858.CD008582.pub2] [PMID]
33. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. BMJ 2009; 339: b2700. [DOI:10.1136/bmj.b2700] [PMID] [PMCID]
34. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2016; 354: i4086. [DOI:10.1136/bmj.i4086] [PMID]
35. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; 343: 592-598. [DOI:10.1136/bmj.d5928] [PMID] [PMCID]
36. Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Assessing risk of bias in a randomized trial. In: Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. 2nd Ed. Chichester (UK): John Wiley & Sons; 2019: 205-228. [DOI:10.1002/9781119536604.ch8]
37. Ghaffari SF, Elyasi F, Mousavinasab SN, Shahhosseini Z. A systematic review of clinical trials affecting anxiety, stress and fear of childbirth in expectant fathers. Nurs Open 2021; 8: 1527-1537. [DOI:10.1002/nop2.681] [PMID] [PMCID]
38. Au K, Lam D, Garg N, Chau A, Dzwonek A, Walker B, et al. Improving skills retention after advanced structured resuscitation training: A systematic review of randomized controlled trials. Resuscitation 2019; 138: 284-296. [DOI:10.1016/j.resuscitation.2019.03.031] [PMID]
39. Nedstrand E, Wijma K, Wyon Y, Hammar M. Applied relaxation and oral estradiol treatment of vasomotor symptoms in postmenopausal women. Maturitas 2005; 51: 154-162. [DOI:10.1016/j.maturitas.2004.05.017] [PMID]
40. Behzadipoor S, Sepahmansour M, Keshavarzi F, Farzad V, Naziri Gh, Zamanian S. Effectiveness of stress management based on cognitive-behavioral intervention on guality of life and coping styles for female with breast cancer. J Psych Models Methods 2013; 3: 29-46.
41. Emami-Sahebi A, Elyasi F, Yazdani-Charati J, Shahhosseini Z. Psychological interventions for nausea and vomiting of pregnancy: A systematic review. Taiwan J Obstet Gynecol 2018; 57: 644-649. [DOI:10.1016/j.tjog.2018.08.005] [PMID]
42. Loprinzi CL, Kugler JW, Sloan JA, Mailliard JA, LaVasseur BI, Barton DL, et al. Venlafaxine in management of hot flashes in survivors of breast cancer: A randomised controlled trial. Lancet 2000; 356: 2059-2063. [DOI:10.1016/S0140-6736(00)03403-6]
43. Tremblay A, Sheeran L, Aranda SK. Psychoeducational interventions to alleviate hot flashes: A systematic review. Menopause 2008; 15: 193-202. [DOI:10.1097/gme.0b013e31805c08dc] [PMID]
44. Germaine LM, Freedman RR. Behavioral treatment of menopausal hot flashes: Evaluation by objective methods. J Consult Clin Psychol 1984; 52: 1072-1079. [DOI:10.1037/0022-006X.52.6.1072]
45. Moher D, Schulz KF, Altman DG. The CONSORT statement: Revised recommendations for improving the quality of reports of parallel-group randomised trials. BMC Med Res Methodol 2001; 1: 2. [DOI:10.1186/1471-2288-1-2] [PMID] [PMCID]
46. Azizi M, Kamali M, Elyasi F, Shirzad M. Fear of childbirth in Iran: A systematic review of psychological intervention research. Int J Reprod Biomed 2021; 19: 401-420. [DOI:10.18502/ijrm.v19i5.9250] [PMID] [PMCID]
47. Samami E, Shahhosseini Z, Elyasi F. The effect of psychological interventions on the quality of life in women with fibromyalgia: A systematic review. J Clin Psycho Med Settings 2021; 28: 503-517. [DOI:10.1007/s10880-021-09794-0] [PMID]
48. Tran S, Hickey M, Saunders Ch, Ramage L, Cohen PA. Nonpharmacological therapies for the management of menopausal vasomotor symptoms in breast cancer survivors. Support Care Cancer 2020; 29: 1183-1193. [DOI:10.1007/s00520-020-05754-w] [PMID]
49. Khanipour Sh, Hakimi S, Nourizade R, Eghdamzamiri R, Salimi Namin M. Comparison of the effects of aerobic exercise and acupressure in reducing hot flashes in breast cancer survivors. Crescent J Med Biol Sci 2020; 7: 539-544.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







