BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijrm.ir/article-1-5-en.html

 , Nadia Nobakhti
, Nadia Nobakhti 
 , Zahra Atrkar Roushan
, Zahra Atrkar Roushan 
 , Havva Dashtdar
, Havva Dashtdar 
 , Mane Oudi
, Mane Oudi 
 , Ahmad Hosseini
, Ahmad Hosseini 

Introduction
Approximately 15% of couples experience difficulty in conceiving and a proportion of them may require assisted conception treatment to alleviate infertility (Trummer, et al., 2000). IUI is an effective first line treatment in properly selected cases and is less invasive than IVF or ICSI. IUI is a procedure in which spermatozoa are placed directly into the uterine cavity through a catheter near the time of ovulation (Chaffkin, et al., 1991). This procedure is most commonly performed as a therapeutic method for couples with a wide variety of subfertility etiologies, such as low count or low motility of sperm, or an incompatibility between the sperm and the cervical mucus (Francavilla et al., 1990; Guzick et al., 1998). It also can be performed to overcome problems associated with husband’s inability to ejaculate inside the woman's vagina due to impotence, premature ejaculation or other medical conditions (Westerlaken et al., 1998). IUI increases the chances of pregnancy because the spermatozoa are placed directly in recommended, because studies have shown that pregnancy will more the uterus, (Berg et al., 1997) bypassing the cervix which improves the delivery of sperm to egg, also providing sperm with higher rates of motility and morphology than those found in untreated ejaculates. IUI is often likely occur if timing of exposure to sperm is controlled, and if high quality spermatozoa are placed into uterine cavity (Sahakyan et al., 1999). The pregnancy rate for IUI is about 3-6% per treatment cycle, but this success rate is dependent on the type and severity of the infertility problem. However, stimulating the ovaries to develop multiple eggs increases the pregnancy rates to 9-20%; however the utility of controlled ovarian hyperstimulation and IUI still remains controversial (Dodson and Haney, 1991; Guzick et al., 1998). Furthermore, most studies are based on small patient population and a low IUI treatment cycles which lead in difficulty in interpretation considering the relatively low pregnancy rate (PR) per cycle Therefor, the objective of the present study was to evaluate the factors such as postwash sperm quality, etiology and duration of infertility that might influence the success of IUI procedure.

Materials and Methods
336 therapeutic IUI were done for 336 women with ages of 20-42 years with infertility problems due to male factor, female factor, or unexplained infertility. This study was limited to first cycle that performed for every couple. All patients were stimulated with a combination of clomiphene citrate (cc) (100 mg from 3rd to 7th days of the menstrual cycle) and HMG (75 IU IM) beginning at 8th day of menstruation, which was adjusted with follicular development monitoring by vaginal ultrasound. When at least one follicular diameter was 18 mm, 10000 IU IM HCG was administered. Approximately 38 hours after HCG injection, IUI procedure was performed. The luteal phase was supported by 1500 IU IM HCG 3 days after insemination and repeated every 3days for a two additional injections.Semen processing
Semen samples were obtained preferably at the Institute. Specimens were left to liquefy at 37 0c for 15 to 60 minutes, and then were subjected to routine semen analysis. Samples were diluted in Ham’s F-10 medium with 5% human serum albumin (HAS) and centrifuged for 3 minutes (300 ´ g). The pellets were resuspended in 1 ml of medium and centrifuged for 3 minutes at 300 ´ g and then were left at 37 0c for 30 to 60 minutes in humidified incubator (5% Co2) to allow motile sperm to rise. The postwash sperm characteristics (number of motile sperm; at least one million/ml, grading of motile sperm;I-IV and normal morphology sperm above 10%) were evaluated and then used for insemination.After sperm processing, it was placed into a Wallace IUI catheter. It was passed through the cervix and into the uterine cavity under sterile conditions. After insemination, the patient was allowed to rest for about one hour before being discharged.
Statistical Analysis
The pregnancy rates were evaluated with sperm parameters, cause and duration of infertility with use of c2 test. Statistical significant differences were determined at p<0.05 levels.

Results
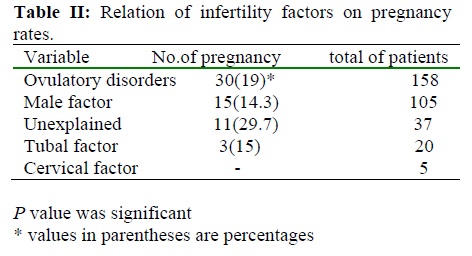
Overall clinical pregnancy rate was 18.2%. The mean age of female was 29.3 (range 20-42 years) and the meanage of male was 33.3 (range 24-54 years). The majority of the pregnancies were achieved in 25-29 years old (20.6%); Table I. Data showed that although the differences between pregnancy rate (PR) and kind of infertility were statistically insignificant, the highest rate of pregnancy was observed in patients with unexplained infertility (29.7% Table II). Duration of infertility didn’t influence PR, but the pregnancy rate according to infertility duration <5 years, 5-10 years and 10-15 years were observed 39(17.8%), 17(20.5%), 5(17.9%), respectively. However, in patients with >15 years infertility no pregnancy took place. The PR was significantly increased with high number of inseminated motile sperm of over 10 million/ml (Table III). Our results demonstrated that the percentage of normal forms post washed sperms ³ 50 was related with pregnancy in 61cases (22.5%) and pregnancy wasn’t observed with sperm motility less than 50% in postwashed sperm analysis (P<0.001). Pregnancy was observed with normal morphology of sperm =10-30%, 30%-
50%, and over/or=50%, 1 (3.6%), 17 (19.3%) and 43(19.8%) respectively (p>0.05).
Discussion
IUI with husband’s sperm has been used empirically for a wide variety of indications. It seems reasonable to consider simpler and inexpensive therapies such as controlled ovarian hyperstimulation (COH) combined with IUI for first-line treatment in subfertility. Overall, ovarian stimulation combined with IUI procedure is more simple than IVF, making COH/IUI treatment convenient for patients. Furthermore, in several studies, COH/IUI treatment has been considered to be cost-effective for subfertile couples before undergoing invasive ART (Dawood, 1996; Van Voorish, 2001). The stimulation protocol used for COH and the insemination technique may affect the outcome of COH/IUI treatment. Zeynelgu et al (1998) study confirmed that addition of IUI to superovulation alone increase the pregnancy chance anywhere from 30% to 160. In addition, patient characteristics such as female age, duration of infertility and diagnostic category may have an effect on the likelihood of pregnancy. All these factors should be taken into account when treatment success is estimated for individual couples and the results of different studies are compared with each other. Pregnancy rate following IUI performed in women over the age of 40 are less than 9.4% per treatment cycle. This is probably due to the adverse effect of age on egg and embryo quality. This is apparent even when the woman produces a number of large follicles on ultrasound. Furthermore, the age-related decrease in fertility has been found in IUI treatment with partner’s sperm, although there has been variability in the results. Many investigators have confirmed a significantly lower PR per cycle in women over the age of 35 years (7 to 10%) compared with younger ones (15 to 23%) ( Brzechffa et al., 1998; Dickey et al., 1991; Pasqualotto et al., 1999; Dickey et al., 1999). Some studies, like Campana et al ( Campana et al., 1996) showed the outcome of IUI treatment was adversely affected if the female’s age was > 39 years. Also Sahakyan et al (1999) represented clear age-related decline in fecundity associated with gonadotropin- induced controlled ovarian hyperstimulation/IUI in patients <40 years old and those with male factor infertility or tubal factor have a particularly poor prognosis. However, van der Westerlaken et al (1998) showed that although there were no pregnancies observed in women 40 years or older, but age did not have a significant effect either. In our study, an advanced female age has not been found to affect the PR in COH/IUI treatment .
The duration of infertility has been shown to be a prognostic factor for live births among untreated subfertile couples in several studies. For example, Snick et al (1997) presented that after 2 to 4 years of infertility the likelihood of a live birth begins to decrease. In COH/IUI therapy, some authors have found that the treatment outcome will be significantly impaire after 3 to 8 years of infertility ( Dickey et al., 1991); but, there are also studies in which the duration of infertility has not been shown to affect the PR ( Dodson and Haney, 1991). Our findings approved similar results as well. Controlled ovarian hyperstimulation together with IUI is widely used for the treatment of subfertility, particularly for couples with unexplained infertility, male factor infertility or mild endometriosis ( Chaffkin et al., 1991; Dodson and Haney, 1991; Brzechffa et al., 1998). However, randomized trials which compare COH/IUI with a non-treated control group in different categories of subfertility are rare .The PR per cycle is achieved in cases of unexplained infertility, using different stimulation protocols (CC, CC/HMG or HMG) and standard IUI are mainly good, varying between 11% to 20% (Brzechffa et al., 1998; Van et al., 2001). In our study, although the difference of pregnancy rate in categories of subfertility wasn’t statistically significant, the most pregnancy rates observed in patients with unexplained infertility (29.7%).
Several semen parameters have been shown to correlate with IUI outcome and maybe useful to consider them. Cut-off values of sperm parameters would be predictive for COH/IUI success. In several studies, treatment outcome has been shown to be more successful if the number of inseminated motile sperm is over 0.25 to 1 × 106 ( Campana et al., 1996; Berg et al., 1997; Sahakyan et al., 1999;). Sahakyan et al (Sahakyan et al., 1999) found the number of inseminated spermatozoa significantly affected the pregnancy rate: <2 million, 4.6%;³2 to< 10 million, 3.9%; and ³10 million, 11.3%. Also, Van der Westerlaken et al (1998) noted when number of sperm were above 10 × 106, pregnancy occurred. Berg et al (1997) showed that PR after IUI in correlation to motile sperm after swim up increased. Francavilla et al (1990) reported no pregnancy when the total motile sperm count was <5 ×106 after swim up. However, there are other reports of a satisfactory PRs when as few as 1 ×106 total motile sperm are available after swim up. This study showed that the pregnancy rate was significantly lower for couples with £10 million (6.7%), there is controversy about the predictive role of sperm count in pregnancy rate. In addition, normal morphology of sperm under 10% has been found to be predictive of poor treatment outcome (Burr et al., 1996); however, this has not been confirmed in all studies. Shulman et al (1998) demonstrated the degree of sperm motility, after appropriate preparation for IUI, is the only parameter to be correlated with treatment outcome. In our study, this parameter was one of the effective factor to increase pregnancy rate. Dickey et al (1999) showed that there is no relation between sperm morphology and IUI outcome. In present study, similar findings has been approved, higher and lower pregnancy rate was observed with morphologically normal sperm ³50% and £30%, respectively. Also it was (Dickey et al., 1999) demonstrated the sperm quality that is necessary for successful IUI is lower than WHO threshold values for normal sperm IUI is effective therapy for male factor infertility when initial sperm motility is > or= 30% and the total motile sperm count is > or=5 ×10 6. When initial values are lower, IUI has little chance of success. These figures are similar to our results. Superovulation with IUI is less invasive and less expensive methods that should be used for subfertile couples before undergoing invasive ART. In conclusion, post wash semen quality was the most important factor for predication of successful pregnancy in this study.
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


