Sat, Feb 21, 2026
[Archive]
Volume 6, Issue 3 (7-2008)
IJRM 2008, 6(3): 89-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sohrabvand F, Abedinia N, Pirjani R, Jafarabadi M. Effect of anxiety and depression on ART outcome. IJRM 2008; 6 (3) :89-0
URL: http://ijrm.ir/article-1-107-en.html
URL: http://ijrm.ir/article-1-107-en.html
1- Department of Obstetrics, Gynecology and Infertility, Tehran University of Medical Sciences, Tehran, Iran , fsohrabvand@yahoo.com
2- Vali-e-Asr Reproductive Health Research Center, Tehran, Iran
2- Vali-e-Asr Reproductive Health Research Center, Tehran, Iran
Full-Text [PDF 95 kb]
(772 Downloads)
| Abstract (HTML) (3415 Views)
Full-Text: (424 Views)
Introduction
Although it is widely accepted that infertility causes significant levels of psychological distress (1), the possibility that distress could cause or contribute to infertility remains a topic for debate (2-10). Several statistical models have been published using combinations of biomedical factors in relation with IVF outcome (11, 12).
The model of Templeton is well known. It is based on a large database and includes the factors age, duration of infertility, number of previous unsuccessful IVF attempts, indication for fertility treatment and number of previous pregnancies as independent predictors (13). A possible reason for the limited validity of the available models is that they are based only on stable variables. Some studies, however, indicate that the success of assisted reproductive treatment may also be dependent on variable factors, such as a woman's distress level at the time of treatment (7, 10, 14). There is increasing evidence that psychological factors, for instance anxiety and depression, are related to IVF/ICSI treatment outcome (7, 15).
There are also studies in which no relationship between the psychosocial status of women and treatment outcome has been found (10, 16). This discrepancy may be explained by differences in population characteristics, study design and differences in the assessment of psychosocial factors. In general, a distinction is made between direct and indirect effects of stress. The direct effects refer to the effects mediated by the autonomic nervous system, the (neuro) endocrine system and the immune system, whereas the indirect effects imply those health changes resulting from changes in health behavior, for instance smoking. Modulation results in an integrated adaptive psychobiological reaction pattern to environmental challenges (17). The main objective of the current study, conducted at two Iranian hospitals, was to clarify the additional role of pre-existing anxiety and depression on ICSI outcome.
Materials and methods
All patients referred to the infertility clinic of Reproductive Health Research Center, Tehran University of Medical Sciences and Alvand Hospital, for the first cycle of an ICSI treatment between January 2006 and 2007 were asked to participate in this prospective cohort pilot study. Of the 195 invited patients 89 declined or were excluded. The main reasons indicated by patients was lack of time (n=33), and it was unknown in 16 cases. Twenty two patients were excluded because of missing data, and 18 because of communication difficulties. Thus, the remaining group consisted of 106 patients. After being examined by a gynecologist the patients were visited by a psychologist and informed of the study purpose.
The study was approved by the Ethical Committee of the deputy of research in Tehran University of Medical Sciences before starting any medications. All women were asked to complete a questionnaire on psychological factors. All participants were guaranteed anonymity, and separation of questionnaire information from their clinical management. Signed informed consent was obtained from all participants. Data regarding the state of anxiety and depression of each volunteer were collected using the translated and validated Iranian Cattle Anxiety and Beck Depression Inventories (BDI) by a single psychologist during interview.
The Cattle inventory is a 40-item self-report measure of anxiety. Scores can range from 0 to 80, with scores of 28 or more demonstrating anxiety. Classification of anxiety scores involves: 0-27 (without anxiety), 28-40 (neurotic anxiety), 41-49 (moderate anxiety) and 50-80 (severe anxiety) (18).
The Beck Depression Inventory (BDI) is a 21 item test. It is one of the most widely used scales for assessing intensity of depression and each of its items describes a specific behavioral manifestation of depression.
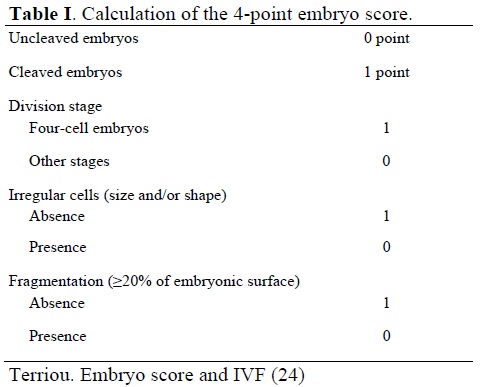
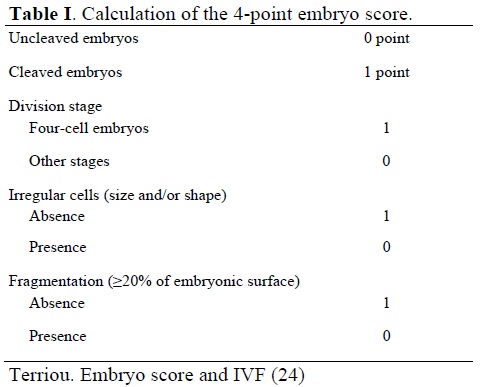
Scores on each item can range from 0 indicating no depression, to 3 indicating a severe level of symptomatology. Scores of 17 or above indicate clinically significant depression. The classification of depression scores involves: 0-16 (without depression), 17-27 (mild depression), 28-34 (moderate depression) and 35-64 (severe depression) (19, 20). The ICSI treatment cycle included pituitary desensitization by Buserelin® (Hoechst Marion Roussel, Germany) 0.5 mg subcutaneous injection per day and then administration of HMG (Pergonal®, Serono, Canada ) 150 IU per day, followed by HCG (Pregnyl®, Organon, The Netherlands), oocyte retrieval after 36 hours and microinjection thereafter. After 3 days the embryos were transferred after scoring. Patients were not informed of the number and scores of transferred embryos in order to avoid inadvertent distress. The CES and MSTE were based on a 4-point score (21- 24) (Table I).
The CES was obtained by adding the individual embryo scores of all transferred embryos, and the MSTE was obtained by dividing the CES by the number of transferred embryos (24). The demographic and gynaecological variables affecting ICSI outcomes consisting of age, duration of infertility, cause of infertility, number and CES and MSTE of transferred embryos were recorded for each patient.
Statistical analysis
All statistical analyses were performed by means of the SPSS-10 software. The outcome measure was clinical pregnancy rate. The first step was to find biomedical variables related to treatment outcome in the current sample. The second step was to add psychological variables to this block of variables. T-student and Chi-square tests were used to compare groups regarding baseline parameters. Multiple logistic regression analysis was used to compare outcome variables between groups omitting the confounding parameters.
Results
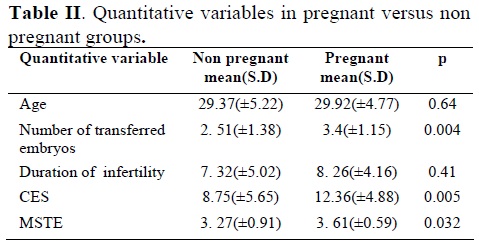
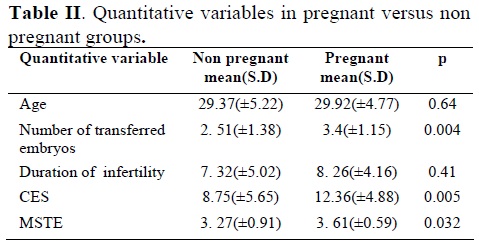
Among 106 women studied, 25 cases of clinical pregnancy occurred after the ICSI procedure. Demographic and basic infertility characteristics of studied groups are summarized in Table II.
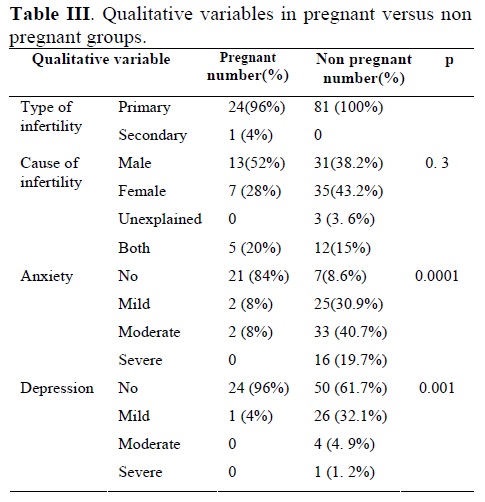
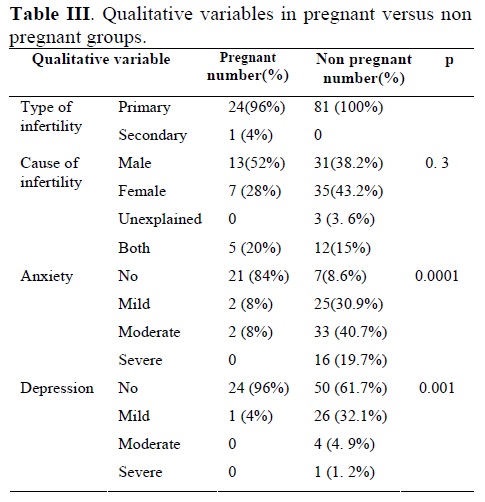
In univariate analysis using t-student and χ2 tests, age of women and duration and cause of infertility were not significantly different between pregnant and nonpregnant groups (Tables II, III). As there was only one case of secondary infertility, p-value was not calculated for the type of infertility (Table III). Number of transferred embryos which was 3.4±1.15 in pregnant group and 2.5±1.38 in nonpregnant group was significantly associated with pregnancy rate (p=0.004) (Table II). Cumulative embryonic score (CES) which was 12.36±4.88 in pregnant and 8.75±5.65 in nonpregnant women and mean score of total embryo (MSTE) being 3.61±0.59 in pregnant and 3.27±0.91 in nonpregnant women were significantly associated with pregnancy rate (p=0.005 and p=0.032 respectively) (Table II). Among 106 women who participated in the study 73.58% of patients had anxiety (mild 25.4%, moderate 33% and severe 15.18%) and 30.18% had depression (mild 25.4%, moderate 3.8% and severe 0.9%). Out of 28 patients with no anxiety, 21(75%) and out of 74 patients with no depression, 24(32%) became pregnant. There was significant association between mean score of depression and anxiety with pregnancy rate (p=0.034 and p=0.000 respectively) (Table III).
Logistic regression analysis was used to adjust the effect of anxiety and depression on ART outcome after ruling out the confounding factors. The results showed anxiety and depression to be independent variables significantly affecting the pregnancy rate (Table IV).

Discussion
Infertility and the shortcomings of the treatment modalities especially impose patients to deal with different degrees of psychological distress. Epidemiologic data suggest a relationship between psychological factors and infertility (2, 3). Nevertheless the role of psychological factors in IVF/ICSI outcome has still to be established.
Though IVF is regarded as the great breakthrough in infertility treatment, it is still considered by the patients to be a stressful experience and its outcome may be influenced by many known and yet unknown factors.
This study shows that there is a significant relationship between depression and anxiety with pregnancy outcome in ICSI cycles. Our study is in accordance with Smeenk’s study (23) that showed a significant relationship between baseline psychological factors and the probability to become pregnant after IVF/ICSI treatments controlling for other factors. They showed that state anxiety had a slightly stronger correlation (p=0.01) with treatment outcomes than depression (p=0.03) (23). Correlation test in our study also showed a more significant negative relation between mean score of anxiety and pregnancy rate in comparison to depression and pregnancy rate. (p=0.000 and p=0.034 respectively).
In a more recent study Smeenk et al have shown that dropout, being a well-known phenomenon in IVF-ICSI, is related to preexisting psychological factors in IVF-ICSI. (25). Peddie et al (26) have shown that psychological factors even play a role in dropouts in IVF treatment which in turn lead to the development of depressive and anxiety symptoms in 10- 50% of women. We did not deal with dropouts because we studied only the first cycles of ART. Among twenty two patients who were excluded because of missing data, there were 8 patients postponing the treatment because of increased anxiety in themselves or their husbands.
In our study anxiety was noted in 73.58 % and depression in 30.18% of the patients. In a study by Jedrzejczak et al, depression was found in 25% of women being treated with IVF and in 25.8% of women attending an infertility clinic compared to 13.2% of control patients awaiting a routine gynecological examination (27). The severity of the depressive symptomatology was assessed in another study (28) with the Beck depression inventory, which indicated that 36.7% of the women attending the infertility clinic were depressed, compared to 18.4% of the control patients. Thus in these studies the prevalence of depression in patients with infertility was high and usually twice that of control patients. The somewhat inconsistent findings in these studies may be due to population characteristics, the design of the study, uni-centeredness, or small sample sizes. Moreover, multi-center studies are preferable because predictions have the tendency to be centre-specific, whereas this study was carried out in two different IVF centers; one belonging to the university and the other a private one. Our results showed anxiety and depression to be independent variables significantly affecting the pregnancy rate, although according to the wide length of confidence interval for relative ratio (RR) of pregnancy, we should be conservative in interpretation (Table IV). It seems that adding the composite score of anxiety and depression to the previous models of stable predictive factors of ART outcome may lead to a better prognostic model with respect to pregnancy rate. The analysis in Smeenk’s study (29) showed that state anxiety only is a better predictor of pregnancy than depression. Our data are also in agreement with those of some previous studies (6, 14). Several other authors however have found no relationship between the emotional status of women and the outcome of ART (10, 24, 30, 31).
Some studies have indicated that the most anxiety provoking time for couples is during their first and final attempts to become pregnant, the first because of the fear of the unknown and the last because of its finality in determining their chances of producing biologic offspring (25, 32, 33). Since all our patients were having their first ART cycle, the number of previous ART cycles was not a confounding factor.
The mechanism of the distress effect on pregnancy rates is still unknown. Subtle disturbances of the cycle may play a role, these being caused by minor endocrinological alterations (34-36). Recent research support the theory that psychological distress can have effects on multiple systems, including inhibition of hypothalamic GnRH, activation of the hypothalamic- adrenal axis and alteration of the immune system (37, 38). In a prospective study in women undergoing IVF, an increase in state anxiety treatment was established, parallel to increase in serum prolactin and cortisol concentrations (28).
To date, several reviews on stress and female reproduction have been published (39-42), but little is known about the relationship between psychosocial stress and the release of adrenal hormones in relation to IVF/ICSI treatment outcome. As the treatment itself most probably influences psychosocial factors, it is extremely difficult to separate cause and effect of psychosocial factors on the outcome in IVF (10). The complex relationship is mediated by interplay of various systems; the underlying mechanisms of the relationship remain obscure so far and aspects of the treatment could influence the hormonal response. For instance Luppa et al. found an increased urinary excretion of cortisol metabolites after stimulation with a GnRH agonist (43).
Although the effects of psychosocial stressors on the activity of the sympathetic medullar system and on the hypothalamic–pituitary–adrenal axis have been studied intensively (44-46), no clear picture emerges on the exact relationship between the different types of stressors and release of stress hormones. Moreover, several authors have reported low correlation coefficients between questionnaire based and hormonal indicators of stress (44).
Stress was previously found to be associated with high amounts of activated T cells and reduced implantation rates in IVF-women (39). Demyttenaere et al indicated that women with high anticipatory state anxiety levels and high anticipatory cortisol concentrations have lower pregnancy rates in IVF (6). Facchinetti et al. demonstrated a negative correlation between stress susceptibility and outcome of IVF (14). Furthermore, Demyttenaere et al suggested that personality dependent stress responses are important for conception rates in stimulated cycles (47). On the other hand, women undergoing IVF were found to respond biophysically different to psychosocial stressors than controls (48). By any mechanism that anxiety and depression affect infertile women, the current and previous studies show that it is mandatory to include counseling and supportive psychotherapy in the general therapeutic framework of infertility.
Conclusion
Since psychological problems of infertile women can significantly affect the outcome of ART cycles, it is crucial to identify patients at greater demand for psychological support and offer them appropriate treatment.
Although it is widely accepted that infertility causes significant levels of psychological distress (1), the possibility that distress could cause or contribute to infertility remains a topic for debate (2-10). Several statistical models have been published using combinations of biomedical factors in relation with IVF outcome (11, 12).
The model of Templeton is well known. It is based on a large database and includes the factors age, duration of infertility, number of previous unsuccessful IVF attempts, indication for fertility treatment and number of previous pregnancies as independent predictors (13). A possible reason for the limited validity of the available models is that they are based only on stable variables. Some studies, however, indicate that the success of assisted reproductive treatment may also be dependent on variable factors, such as a woman's distress level at the time of treatment (7, 10, 14). There is increasing evidence that psychological factors, for instance anxiety and depression, are related to IVF/ICSI treatment outcome (7, 15).
There are also studies in which no relationship between the psychosocial status of women and treatment outcome has been found (10, 16). This discrepancy may be explained by differences in population characteristics, study design and differences in the assessment of psychosocial factors. In general, a distinction is made between direct and indirect effects of stress. The direct effects refer to the effects mediated by the autonomic nervous system, the (neuro) endocrine system and the immune system, whereas the indirect effects imply those health changes resulting from changes in health behavior, for instance smoking. Modulation results in an integrated adaptive psychobiological reaction pattern to environmental challenges (17). The main objective of the current study, conducted at two Iranian hospitals, was to clarify the additional role of pre-existing anxiety and depression on ICSI outcome.
Materials and methods
All patients referred to the infertility clinic of Reproductive Health Research Center, Tehran University of Medical Sciences and Alvand Hospital, for the first cycle of an ICSI treatment between January 2006 and 2007 were asked to participate in this prospective cohort pilot study. Of the 195 invited patients 89 declined or were excluded. The main reasons indicated by patients was lack of time (n=33), and it was unknown in 16 cases. Twenty two patients were excluded because of missing data, and 18 because of communication difficulties. Thus, the remaining group consisted of 106 patients. After being examined by a gynecologist the patients were visited by a psychologist and informed of the study purpose.
The study was approved by the Ethical Committee of the deputy of research in Tehran University of Medical Sciences before starting any medications. All women were asked to complete a questionnaire on psychological factors. All participants were guaranteed anonymity, and separation of questionnaire information from their clinical management. Signed informed consent was obtained from all participants. Data regarding the state of anxiety and depression of each volunteer were collected using the translated and validated Iranian Cattle Anxiety and Beck Depression Inventories (BDI) by a single psychologist during interview.
The Cattle inventory is a 40-item self-report measure of anxiety. Scores can range from 0 to 80, with scores of 28 or more demonstrating anxiety. Classification of anxiety scores involves: 0-27 (without anxiety), 28-40 (neurotic anxiety), 41-49 (moderate anxiety) and 50-80 (severe anxiety) (18).
The Beck Depression Inventory (BDI) is a 21 item test. It is one of the most widely used scales for assessing intensity of depression and each of its items describes a specific behavioral manifestation of depression.
Scores on each item can range from 0 indicating no depression, to 3 indicating a severe level of symptomatology. Scores of 17 or above indicate clinically significant depression. The classification of depression scores involves: 0-16 (without depression), 17-27 (mild depression), 28-34 (moderate depression) and 35-64 (severe depression) (19, 20). The ICSI treatment cycle included pituitary desensitization by Buserelin® (Hoechst Marion Roussel, Germany) 0.5 mg subcutaneous injection per day and then administration of HMG (Pergonal®, Serono, Canada ) 150 IU per day, followed by HCG (Pregnyl®, Organon, The Netherlands), oocyte retrieval after 36 hours and microinjection thereafter. After 3 days the embryos were transferred after scoring. Patients were not informed of the number and scores of transferred embryos in order to avoid inadvertent distress. The CES and MSTE were based on a 4-point score (21- 24) (Table I).
The CES was obtained by adding the individual embryo scores of all transferred embryos, and the MSTE was obtained by dividing the CES by the number of transferred embryos (24). The demographic and gynaecological variables affecting ICSI outcomes consisting of age, duration of infertility, cause of infertility, number and CES and MSTE of transferred embryos were recorded for each patient.
Statistical analysis
All statistical analyses were performed by means of the SPSS-10 software. The outcome measure was clinical pregnancy rate. The first step was to find biomedical variables related to treatment outcome in the current sample. The second step was to add psychological variables to this block of variables. T-student and Chi-square tests were used to compare groups regarding baseline parameters. Multiple logistic regression analysis was used to compare outcome variables between groups omitting the confounding parameters.
Results
Among 106 women studied, 25 cases of clinical pregnancy occurred after the ICSI procedure. Demographic and basic infertility characteristics of studied groups are summarized in Table II.
In univariate analysis using t-student and χ2 tests, age of women and duration and cause of infertility were not significantly different between pregnant and nonpregnant groups (Tables II, III). As there was only one case of secondary infertility, p-value was not calculated for the type of infertility (Table III). Number of transferred embryos which was 3.4±1.15 in pregnant group and 2.5±1.38 in nonpregnant group was significantly associated with pregnancy rate (p=0.004) (Table II). Cumulative embryonic score (CES) which was 12.36±4.88 in pregnant and 8.75±5.65 in nonpregnant women and mean score of total embryo (MSTE) being 3.61±0.59 in pregnant and 3.27±0.91 in nonpregnant women were significantly associated with pregnancy rate (p=0.005 and p=0.032 respectively) (Table II). Among 106 women who participated in the study 73.58% of patients had anxiety (mild 25.4%, moderate 33% and severe 15.18%) and 30.18% had depression (mild 25.4%, moderate 3.8% and severe 0.9%). Out of 28 patients with no anxiety, 21(75%) and out of 74 patients with no depression, 24(32%) became pregnant. There was significant association between mean score of depression and anxiety with pregnancy rate (p=0.034 and p=0.000 respectively) (Table III).
Logistic regression analysis was used to adjust the effect of anxiety and depression on ART outcome after ruling out the confounding factors. The results showed anxiety and depression to be independent variables significantly affecting the pregnancy rate (Table IV).

Discussion
Infertility and the shortcomings of the treatment modalities especially impose patients to deal with different degrees of psychological distress. Epidemiologic data suggest a relationship between psychological factors and infertility (2, 3). Nevertheless the role of psychological factors in IVF/ICSI outcome has still to be established.
Though IVF is regarded as the great breakthrough in infertility treatment, it is still considered by the patients to be a stressful experience and its outcome may be influenced by many known and yet unknown factors.
This study shows that there is a significant relationship between depression and anxiety with pregnancy outcome in ICSI cycles. Our study is in accordance with Smeenk’s study (23) that showed a significant relationship between baseline psychological factors and the probability to become pregnant after IVF/ICSI treatments controlling for other factors. They showed that state anxiety had a slightly stronger correlation (p=0.01) with treatment outcomes than depression (p=0.03) (23). Correlation test in our study also showed a more significant negative relation between mean score of anxiety and pregnancy rate in comparison to depression and pregnancy rate. (p=0.000 and p=0.034 respectively).
In a more recent study Smeenk et al have shown that dropout, being a well-known phenomenon in IVF-ICSI, is related to preexisting psychological factors in IVF-ICSI. (25). Peddie et al (26) have shown that psychological factors even play a role in dropouts in IVF treatment which in turn lead to the development of depressive and anxiety symptoms in 10- 50% of women. We did not deal with dropouts because we studied only the first cycles of ART. Among twenty two patients who were excluded because of missing data, there were 8 patients postponing the treatment because of increased anxiety in themselves or their husbands.
In our study anxiety was noted in 73.58 % and depression in 30.18% of the patients. In a study by Jedrzejczak et al, depression was found in 25% of women being treated with IVF and in 25.8% of women attending an infertility clinic compared to 13.2% of control patients awaiting a routine gynecological examination (27). The severity of the depressive symptomatology was assessed in another study (28) with the Beck depression inventory, which indicated that 36.7% of the women attending the infertility clinic were depressed, compared to 18.4% of the control patients. Thus in these studies the prevalence of depression in patients with infertility was high and usually twice that of control patients. The somewhat inconsistent findings in these studies may be due to population characteristics, the design of the study, uni-centeredness, or small sample sizes. Moreover, multi-center studies are preferable because predictions have the tendency to be centre-specific, whereas this study was carried out in two different IVF centers; one belonging to the university and the other a private one. Our results showed anxiety and depression to be independent variables significantly affecting the pregnancy rate, although according to the wide length of confidence interval for relative ratio (RR) of pregnancy, we should be conservative in interpretation (Table IV). It seems that adding the composite score of anxiety and depression to the previous models of stable predictive factors of ART outcome may lead to a better prognostic model with respect to pregnancy rate. The analysis in Smeenk’s study (29) showed that state anxiety only is a better predictor of pregnancy than depression. Our data are also in agreement with those of some previous studies (6, 14). Several other authors however have found no relationship between the emotional status of women and the outcome of ART (10, 24, 30, 31).
Some studies have indicated that the most anxiety provoking time for couples is during their first and final attempts to become pregnant, the first because of the fear of the unknown and the last because of its finality in determining their chances of producing biologic offspring (25, 32, 33). Since all our patients were having their first ART cycle, the number of previous ART cycles was not a confounding factor.
The mechanism of the distress effect on pregnancy rates is still unknown. Subtle disturbances of the cycle may play a role, these being caused by minor endocrinological alterations (34-36). Recent research support the theory that psychological distress can have effects on multiple systems, including inhibition of hypothalamic GnRH, activation of the hypothalamic- adrenal axis and alteration of the immune system (37, 38). In a prospective study in women undergoing IVF, an increase in state anxiety treatment was established, parallel to increase in serum prolactin and cortisol concentrations (28).
To date, several reviews on stress and female reproduction have been published (39-42), but little is known about the relationship between psychosocial stress and the release of adrenal hormones in relation to IVF/ICSI treatment outcome. As the treatment itself most probably influences psychosocial factors, it is extremely difficult to separate cause and effect of psychosocial factors on the outcome in IVF (10). The complex relationship is mediated by interplay of various systems; the underlying mechanisms of the relationship remain obscure so far and aspects of the treatment could influence the hormonal response. For instance Luppa et al. found an increased urinary excretion of cortisol metabolites after stimulation with a GnRH agonist (43).
Although the effects of psychosocial stressors on the activity of the sympathetic medullar system and on the hypothalamic–pituitary–adrenal axis have been studied intensively (44-46), no clear picture emerges on the exact relationship between the different types of stressors and release of stress hormones. Moreover, several authors have reported low correlation coefficients between questionnaire based and hormonal indicators of stress (44).
Stress was previously found to be associated with high amounts of activated T cells and reduced implantation rates in IVF-women (39). Demyttenaere et al indicated that women with high anticipatory state anxiety levels and high anticipatory cortisol concentrations have lower pregnancy rates in IVF (6). Facchinetti et al. demonstrated a negative correlation between stress susceptibility and outcome of IVF (14). Furthermore, Demyttenaere et al suggested that personality dependent stress responses are important for conception rates in stimulated cycles (47). On the other hand, women undergoing IVF were found to respond biophysically different to psychosocial stressors than controls (48). By any mechanism that anxiety and depression affect infertile women, the current and previous studies show that it is mandatory to include counseling and supportive psychotherapy in the general therapeutic framework of infertility.
Conclusion
Since psychological problems of infertile women can significantly affect the outcome of ART cycles, it is crucial to identify patients at greater demand for psychological support and offer them appropriate treatment.
Type of Study: Original Article |
References
1. Mahlstedt PP. The psychological component of infertility. Fertil Steril 1985; 43: 335- 336. [DOI:10.1016/S0015-0282(16)48428-1]
2. Freeman EW, Boxer AS, Rickels K. Psychological evaluation and support in a program of in vitro fertilization and embryo transfer. Fertil Steril 1985; 43: 48-53. [DOI:10.1016/S0015-0282(16)48316-0]
3. Lapane KL, Zierler S, Lasater TM. Is a history of depressive symptoms associated with an increased risk of infertility in women? Psychosom Med 1995; 57: 509- 513. [DOI:10.1097/00006842-199511000-00001]
4. Wright J, Allard M, Lecours A, Sabourin S. Psychosocial distress and infertility: a review of controlled research. Int J Fertil 1989; 34: 126-142.
5. Eugster A, Vingerhoets AJ. Psychological aspects of in vitro fertilization: a review. Soc Sci Med 1999; 5: 575- 589. [DOI:10.1016/S0277-9536(98)00386-4]
6. Demyttenaere K, Nijs P, Evers Kiebooms G, Koninckx PR. Coping and the ineffectiveness of coping influence the outcome of in vitro fertilization through stress responses. Psychoneuroendocrinology 1992; 17: 655- 665. [DOI:10.1016/0306-4530(92)90024-2]
7. Demyttenaere K, Bonte L, Gheldof M. Coping style and depression level influence outcome in in vitro fertilization. Fertil Steril 1998; 69: 1026- 1033. [DOI:10.1016/S0015-0282(98)00089-2]
8. Merari D, Feldberg D, Elizur A. Psychological and hormonal changes in the course of in vitro fertilization. J Assist Reprod Genet 1992; 9: 161- 169. [DOI:10.1007/BF01203757]
9. Thiering P, Beaurepaire J, Jones M. Mood state as a predictor of treatment outcome after in vitro fertilization/embryo transfer technology (IVF/ET). J Psychosom Res 1993; 37:481- 491. [DOI:10.1016/0022-3999(93)90004-Y]
10. Boivin J, Takefman J. Stress level across stages of in vitro fertilization in subsequently pregnant and nonpregnant women. Fertil Steril 1995; 64: 802-810. [DOI:10.1016/S0015-0282(16)57858-3]
11. Stolwijk AM, Zielhuis GA, Hamilton CJCM. Prognostic models for the probability of achieving an ongoing pregnancy after in vitro fertilization and the importance of testing their predictive value. Hum Reprod 1996; 11: 2298- 2303. [DOI:10.1093/oxfordjournals.humrep.a019092]
12. Smeenk JMJ, Stolwijk AM, Kremer JAM, Braat DDM. External validation of the Templeton model for predicting success after IVF. Hum Reprod 2000; 15: 1065- 1068. [DOI:10.1093/humrep/15.5.1065]
13. Templeton A, Morris JK, Parslow W. Factors that affect outcome of in vitro fertilization treatment. Lancet 1996; 348:1402-1406. [DOI:10.1016/S0140-6736(96)05291-9]
14. Facchinetti F, Matteo ML, Artini GP. An increased vulnerability to stress is associated with a poor outcome of in vitro fertilization-embryo transfer treatment. Fertil Steril 1997; 67: 309- 314. [DOI:10.1016/S0015-0282(97)81916-4]
15. Smeenk J, Verhaak C, Eugster A, Minnen A, Zielhuis G, Braat D. The effect of anxiety and depression on the outcome of in vitro fertilization. Hum Reprod 2001; 16: 7, 1420-1423. [DOI:10.1093/humrep/16.7.1420]
16. Slade P, Emery J, Lieberman BA. A prospective, longitudinal study of emotions and relationship in in-vitro fertilization treatment. Hum Reprod 1997; 12: 183-190. [DOI:10.1093/humrep/12.1.183]
17. Stroobant N, Vingerhoets G. Transcranial Doppler ultrasonography monitoring of cerebral hemodynamics during performance of cognitive tasks: a review. Neuropsychol Rev 2000; 10:213-231. [DOI:10.1023/A:1026412811036]
18. Alvandi A. Validity and reliability of Cattle inventory for Iranians. Tehran University; 1988; Graduation thesis.
19. Okhovat V. Validity and reliability of Beck depression for Iranian society. Tehran University 1974; Graduation thesis.
20. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression Arch Gen Psychiatry 1961; 4:561-571. [DOI:10.1001/archpsyc.1961.01710120031004]
21. Cummins JM, Breen TM, Harrison KL, Shaw JM, Wilson LM, Hennesey JF. A formula for scoring human embryo growth rates in in vitro fertilization: its value in predicting pregnancy and in comparison with visual estimates of embryo quality. J In Vitro Fert Embryo Trans 1986; 5: 284 -295. [DOI:10.1007/BF01133388]
22. Claman P, Armant DR, Seibel MM, Wang TA, Oskowitz SP, Taymor ML. The impact of embryo quality on implantation and the establishment of viable pregnancies. J In Vitro Fert Embryo Trans 1987; 4:218-222. [DOI:10.1007/BF01533759]
23. Puissant F, Van Rysselberge M, Barlow P, Deweze J, Leroy F. Embryo scoring as a prognostic tool in IVF treatment. Hum Reprod 1987; 8: 705-708. [DOI:10.1093/oxfordjournals.humrep.a136618]
24. Terriou P, Sapin C, Giorgetti C, Hans E, Spach JL, Roulier R. Embryo score is a better predictor of pregnancy than the number of transferred embryos or female age. Fertil Steril 2001; 75:525-531. [DOI:10.1016/S0015-0282(00)01741-6]
25. Smeenk JM, Verhaak CM, Stolwijk AM, Kremer JA, Braat DD. Reasons for dropout in an in vitro fertilization/intracytoplasmic sperm injection program. Fertil Steril 2004; 81:262-268. [DOI:10.1016/j.fertnstert.2003.09.027]
26. Peddie VL, van Teijlingen E, Bhattacharya S. A qualitative study of women's decision-making at the end of IVF treatment. Hum Reprod 2005; 20:1944-1951. [DOI:10.1093/humrep/deh857]
27. Jedrzejczak P, Luczak-Wawrzyniak J, Szyfter J, Przewozna J, Taszarek-Hauke G, Pawelczyk L. Feelings and emotions in women treated for infertility. Przegl Lek 2004; 61: 1334-1337.
28. Kee BS, Jung BJ, Lee SH. A study on psychological strain in IVF patients. J Assist Reprod Genet 2000; 17:445-448. [DOI:10.1023/A:1009417302758]
29. Smeenk JMJ , Verhaak CM , Vingerhoets AJJM , Sweep CGJ , Merkus JMWM , Willemsen SJ ,et al. Stress and outcome success in IVF: the role of self-reports and endocrine variables. Hum Reprod 2005; 20: 991 - 996. [DOI:10.1093/humrep/deh739]
30. Harlow CR, Fahy UM, Talbot WM. Stress and stress-related hormones during in-vitro fertilization treatment. Hum Reprod 1996; 11: 274-279. [DOI:10.1093/HUMREP/11.2.274]
31. Ardenti R, Campari C, Agazzi L. Anxiety and perceptive functioning of infertile women during in-vitro fertilization: exploratory survey of an Italian sample. Hum Reprod 1999; 14: 3126-3132. [DOI:10.1093/humrep/14.12.3126]
32. Rajkhowa M, Mcconnell A, Thomas GE. Reasons for discontinuation of IVF treatment: a questionnaire study. Hum Reprod 2006; 21: 358 - 363. [DOI:10.1093/humrep/dei355]
33. Klerk C, Hunfeld JAM, Duivenvoorden HJ, Outer MA, Fauser BCJM, Passchier J, et al. Effectiveness of a psychosocial counseling intervention for first-time IVF couples: a randomized controlled trial. Hum Reprod 2005; 20: 1333 - 1338. [DOI:10.1093/humrep/deh748]
34. Demyttenaere K, Nijs P, Evers-Kiebooms G, Koninckx PR. The effect of a specific emotional stressor on prolactin, cortisol, and testosterone concentrations in women varies with their trait anxiety. Fertil Steril 1989; 52: 942-948. [DOI:10.1016/S0015-0282(16)53156-2]
35. Demyttenaere K, Nijs P, Evers-Kiebooms G, Koninckx PR. Personality characteristics, psychoendocrinological stress and outcome of IVF depend upon the etiology of infertility. Gynecol Endocrinol 1994; 8: 233-240. [DOI:10.3109/09513599409023626]
36. Psech U, Weyer G, Taubert HD. Coping mechanisms in infertile women with luteal phase deficiency. J Psychosom Obstet Gynaecol 1989; 10: 15-19. [DOI:10.3109/01674828909016675]
37. Tilbrook AJ, Turner AI, Clarke IJ. Stress and reproduction: central mechanisms and sex differences in non-rodent species. Stress 2002; 5:83-100. [DOI:10.1080/10253890290027912]
38. Gallinelli A, Roncaglia R, Matteo ML, Ciaccio I, Volpe A, Facchinetti F. Immunological changes and stress are associated with different implantation rates in patients undergoing in vitro fertilization-embryo transfer. Fertil Steril 2001; 76: 85-91. [DOI:10.1016/S0015-0282(01)01826-X]
39. Greil AL. Infertility and psychological distress: a critical review of the literature. Soc Sci Med 1997; 45:1679-1704. [DOI:10.1016/S0277-9536(97)00102-0]
40. Magiakou MA, Mastorakos G, Webster E, Chrousos GP. The hypothalamic-pituitary-adrenal axis and the female reproductive system. Ann N Y Acad Sci 1997: 17; 816: 42-56. [DOI:10.1111/j.1749-6632.1997.tb52128.x]
41. Ferin M. Clinical review 105: Stress and the reproductive cycle. J Clin Endocrinol Metab 1999; 84: 1768-1774. [DOI:10.1210/jcem.84.6.5367]
42. Sheldon IM, Dobson H. Reproductive challenges facing the cattle industry at the beginning of the 21st century. Reprod Suppl 2003; 61: 1-13.
43. Luppa P, Muller B, Jacob K, Kimmig R, Strowitzki T, Hoss C, et al. Variations of steroid hormone metabolites in serum and urine in polycystic ovary syndrome after nafarelin stimulation: evidence for an altered corticoid excretion. J Clin Endocrinol Metab 1995; 80: 280-288. [DOI:10.1210/jcem.80.1.7829627]
44. Garippa PA, Sanders N. Resolution of erectile dysfunction and inhibited male orgasm in a single homosexual male and transfer of inhibited male orgasm cure to his partner: a case report. J Sex Marital Ther 1997; 23: 126-130. [DOI:10.1080/00926239708405313]
45. Buijs RM, la Fleur SE, Wortel J, Van Heyningen C, Zuiddam L, Mettenleiter TC, et al. The suprachiasmatic nucleus balances sympathetic and parasympathetic output to peripheral organs through separate preautonomic neurons. J Comp Neurol 2003; 464: 36-48. [DOI:10.1002/cne.10765]
46. Schommer NC, Hellhammer DH, Kirschbaum C. Dissociation between reactivity of the hypothalamus-pituitary-adrenal axis and the sympathetic-adrenal-medullary system to repeated psychosocial stress. Psychosom Med 2003; 65: 450-460. [DOI:10.1097/01.PSY.0000035721.12441.17]
47. Demyttenaere K, Nijs P, Evers-Kiebooms G, Koninckx PR. Coping, ineffectiveness of coping and the psychoendocrinological stress responses during in-vitro fertilization. J Psychosom Res 1991; 35: 231-243. [DOI:10.1016/0022-3999(91)90077-2]
48. Lindheim SR, Legro RS, Morris RS, Vijod MA, Lobo RA, Paulson RJ, et al. Altered responses to stress in women undergoing in-vitro fertilization and recipients of oocyte donation. Hum Reprod 1995; 10: 320-323. [DOI:10.1093/oxfordjournals.humrep.a135935]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




