Sun, Feb 1, 2026
[Archive]
Volume 17, Issue 11 (November 2019)
IJRM 2019, 17(11): 799-806 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gholampour F, Malekpour Mansourkhani S, Owji S M. Amelioration of testicular damages in renal ischemia/reperfusion by berberine: An experimental study. IJRM 2019; 17 (11) :799-806
URL: http://ijrm.ir/article-1-1720-en.html
URL: http://ijrm.ir/article-1-1720-en.html
Amelioration of testicular damages in renal ischemia/reperfusion by berberine: An experimental study
1- Department of Biology, School of Sciences, Shiraz University, Shiraz, Iran. , gholampour@shirazu.ac.ir
2- Department of Biology, School of Sciences, Shiraz University, Shiraz, Iran.
3- Department of Pathology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
2- Department of Biology, School of Sciences, Shiraz University, Shiraz, Iran.
3- Department of Pathology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
Full-Text [PDF 3590 kb]
(1245 Downloads)
| Abstract (HTML) (3489 Views)
Considering the potential therapeutic properties of berberine, the goals of this experiment were to determine the effects of AKI on the testicular function and to assess the effect of berberine on testicular damages induced by renal I/R injury.

2.4.Ethical consideration
All interventions in rats were provided according to the protocol provided by the ethics committee of Shiraz University (code: 900794).
2.5.Statistical analysis
Experimental data (mean ± SD) were analyzed using the SPSS statistics software package (SPSS for Windows version 16, Chicago, IL, USA). The normal distribution was tested by Shapiro-Wilk. Comparison between groups was calculated by one-way ANOVA and Tukey’s post-hoc test. The histopathological scores were statistically compared between groups by Kruskal-Wallis multiple comparison tests, and binary comparisons were done by Mann-Whitney U test. P < 0.05 was considered significant.
3.Results
3.1.Berberine ameliorates the I/R-induced changes in biochemical parameters
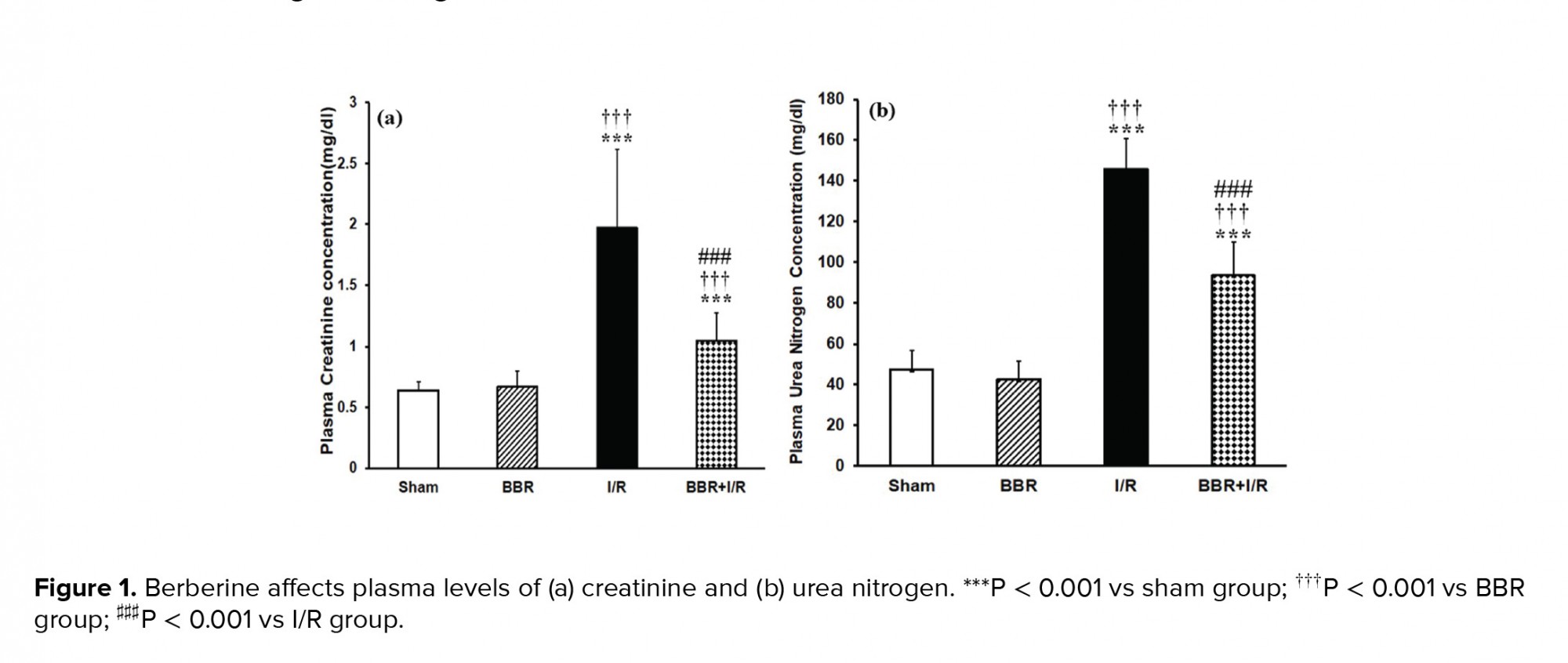
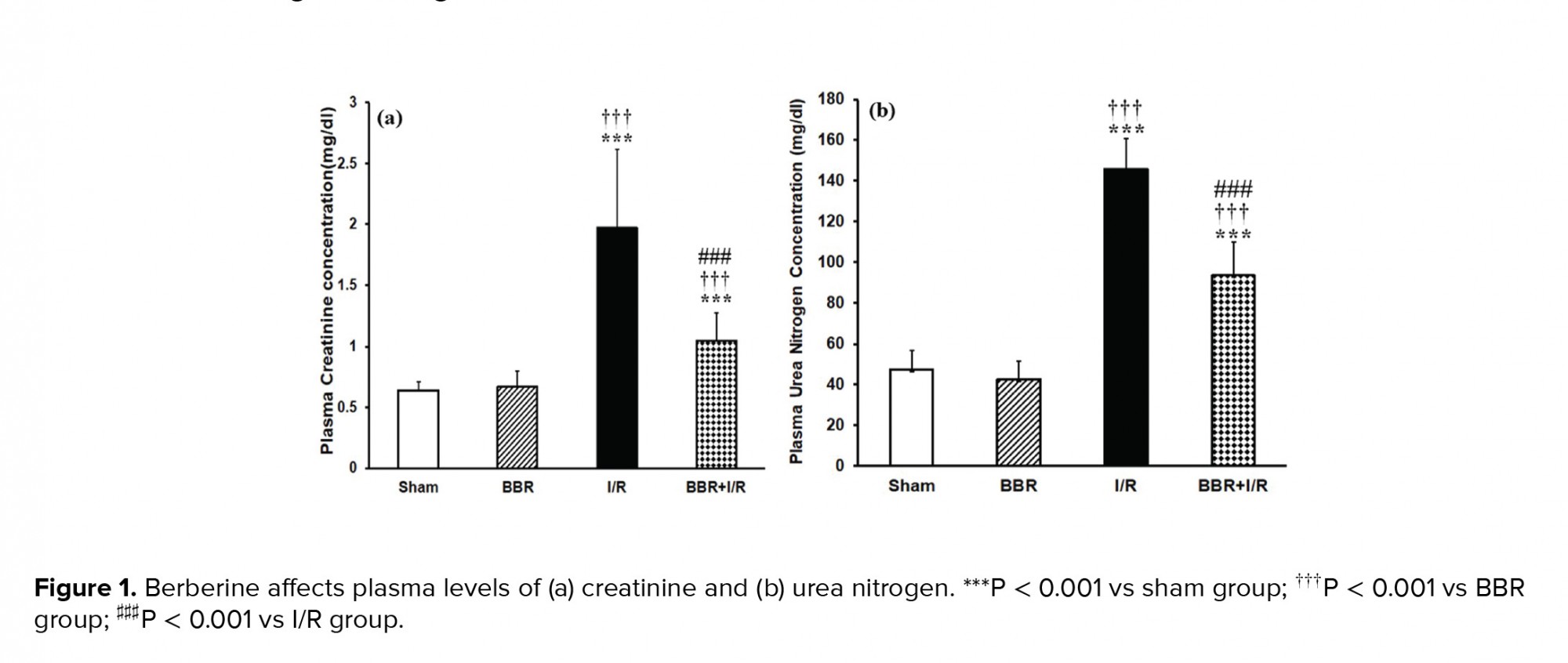
As shown in figure 1, at the end of 24 hr reperfusion period, the plasma levels of creatinine and urea nitrogen were statistically higher in I/R group in comparison with those of sham and BBR groups (p < 0.001). However, in the BBR + I/R group, there was a significant decrease in creatinine (Figure 1a) and BUN (Figure 1b) levels compared to the I/R group (p < 0.001). Figure 2a shows that in the I/R group, the plasma testosterone level was significantly decreased with respect to its level in the sham and BBR groups (p < 0.001). The testosterone level was increased in the BBR + I/R group in comparison to the I/R group (p < 0.001), while it was lower than the level in the sham and BBR groups (Figure 2a). Besides, plasma levels of LH and FSH observed were significantly increased in the I/R group compared to the sham and BBR groups (p < 0.001). But berberine pretreatment diminished the plasma levels of LH (Figure 2b) and FSH (Figure 2c) in the BBR + I/R group in comparison with the I/R group (p < 0.001).
3.2. Berberine protects the I/R-induced histological changes in testicular tissue
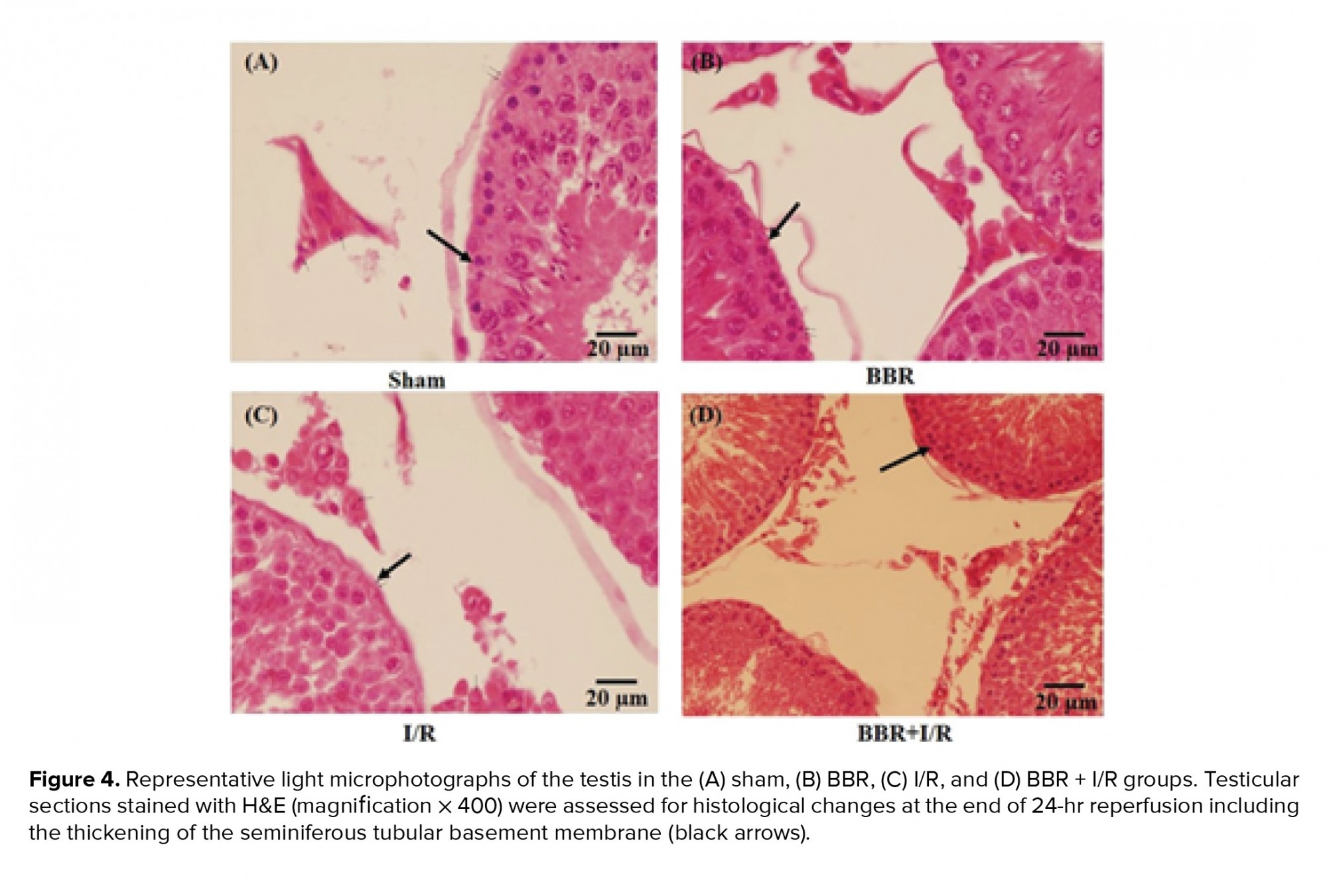
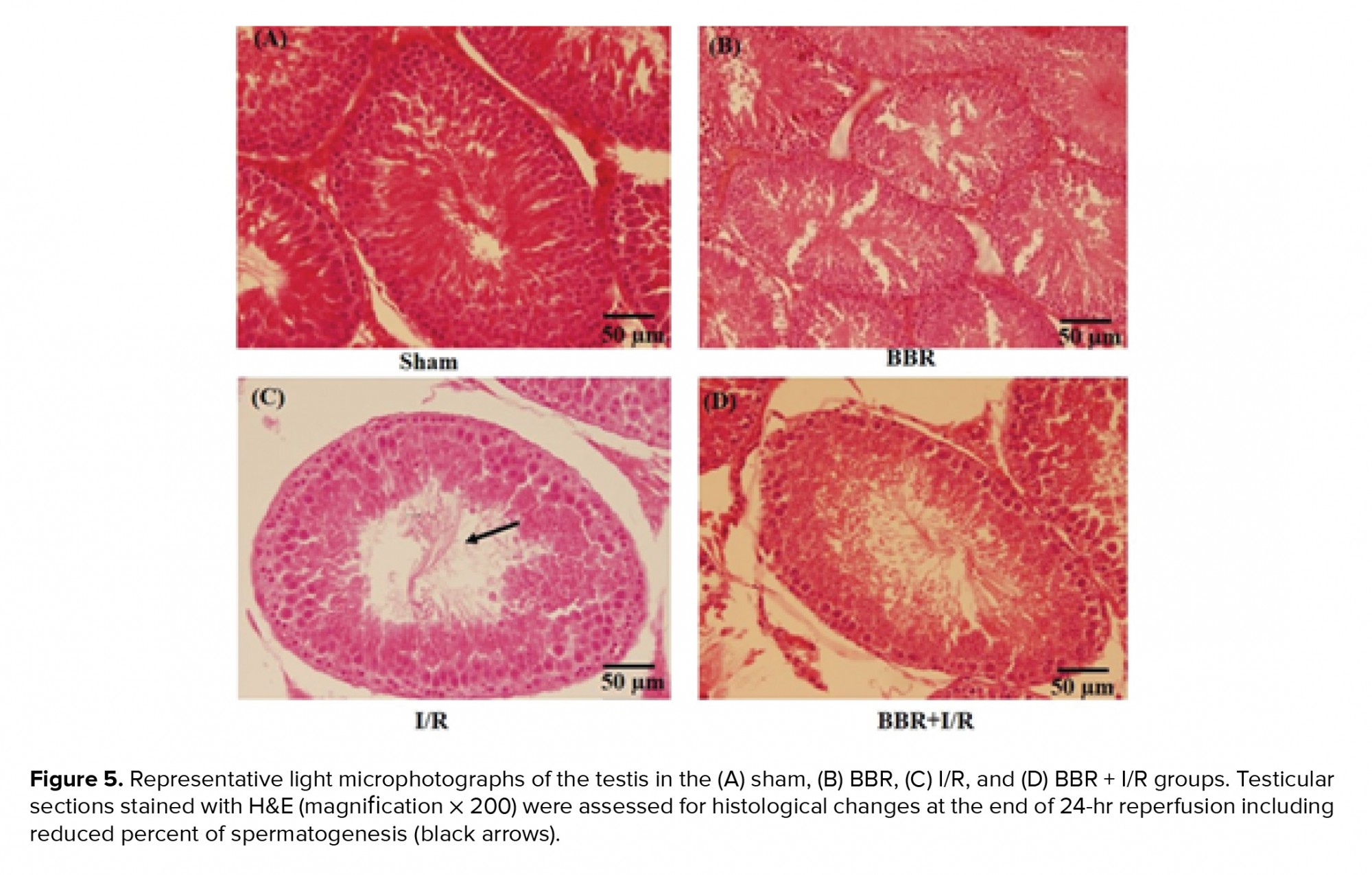
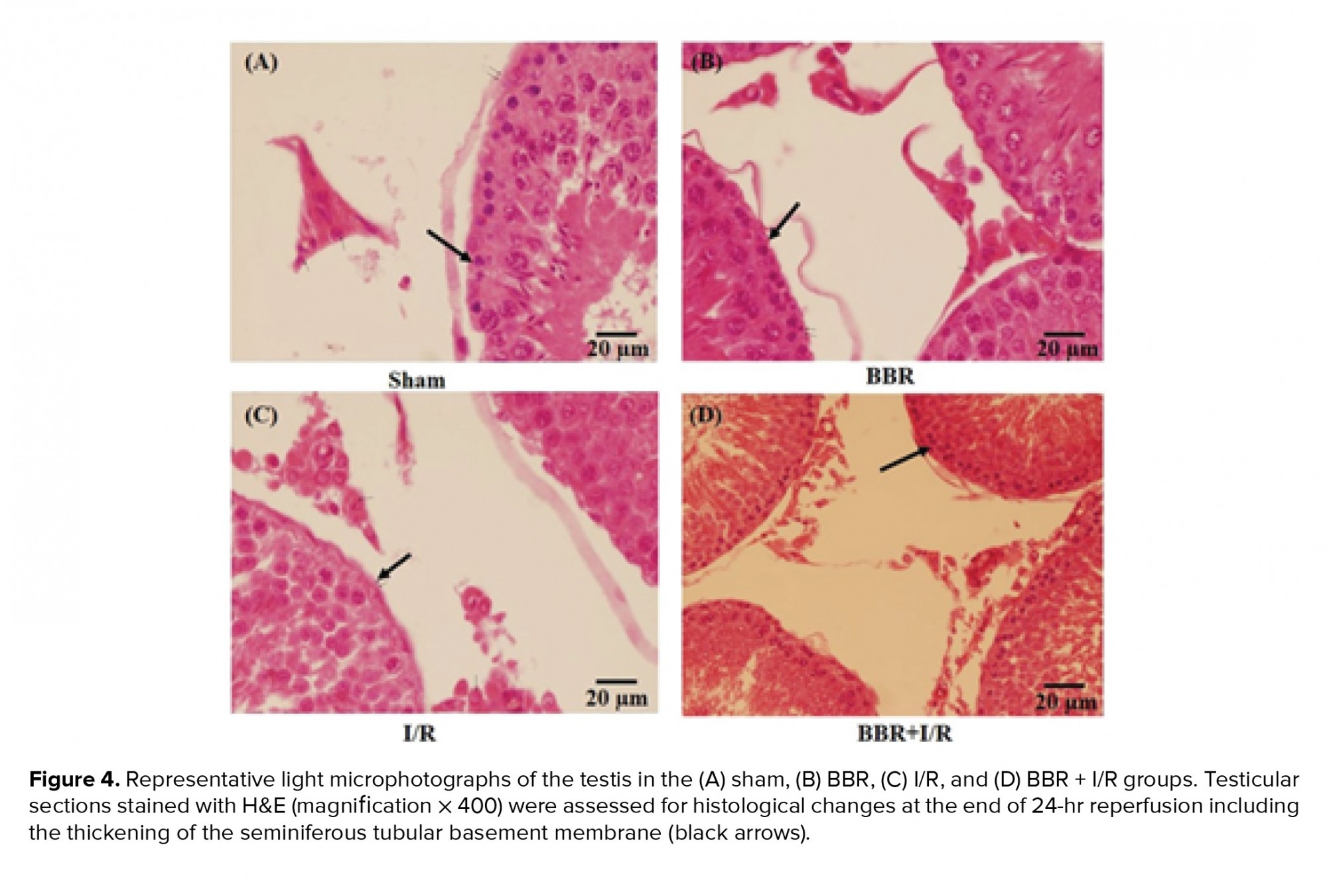
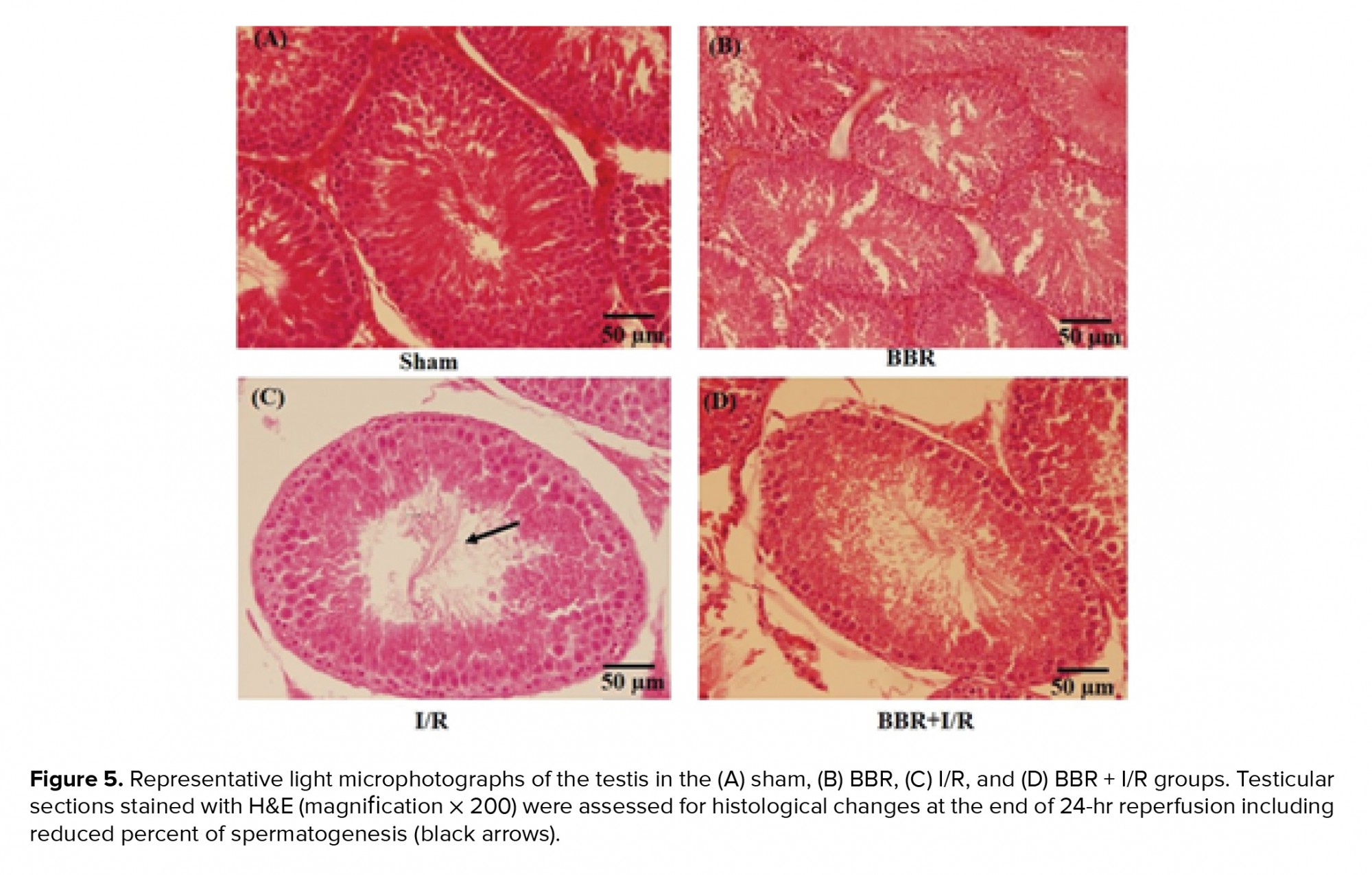
Figures 3, 4, and 5 shows that there were no detectable histological changes to the testes of the sham and BBR groups. However, the most prominent lesions in the I/R group (Figure 3, 4, 5) were increased number of interstitial Leydig cells (hyperplasia), increase in the volume percent of interstitial space and internal space of seminiferous tubules, decrease in the number of spermatogenic cells, and thickening of the tubular basement membrane. In the BBR + I/R group, less intense damages were noticed in comparison with the I/R group (Figures 3, 4, 5).


4.Discussion
The AKI is assumed as a pan-organ problem with negative consequences on many other organs in the body (11). The main goal of this study was to evaluate the effect of 45 min ischemia/24 hr reperfusion on functional-morphological characteristics of the testis in rats. The reason for considering 45-min ischemia/24 hr reperfusion as a timing of ischemia and reperfusion was that a minimum of 30 min ischemia is needed to induce AKI. Besides, mitochondrial function is restored by reperfusion when ischemic interval is 45 min or less. However, ischemic intervals longer than 45 min produce non-reversible impairment of ATP synthesis, and the marked reduction following 90 min of ischemia signifies possible transition to a non-viable state (12). Also, the maximum renal dysfunction following 30-45 min of renal ischemia happens at the end of 24 hr reperfusion period (13). The renal IRI resulted in testicular histological damages accompanied with increased plasma levels of creatinine, urea nitrogen, LH, and FSH, as well decrease of plasma testosterone concentration. Berberine diminished histological damage to the testis and attenuated the increase in plasma creatinine, urea nitrogen, LH, FSH, and decrease in plasma testosterone concentration in the BBR + I/R group.
In sham rats, the seminiferous tubules had normal size and were full of spermatogenic cells, with minimal interstitial connective tissue and a small number of Leydig cells. Morphological study of the testicular sections in the I/R group revealed a decreased number of spermatogenic cells, thickening of basement membrane, and Leydig cell hyperplasia. As very high quantities of testosterone are essential for the survival of the reproductive tract, it is concluded that this atrophy of seminiferous tubules is probably developed due to the reduction in the testosterone levels. Besides, Leydig cell hyperplasia might be created to offset the reduced testosterone level.
Our results showed elevated plasma LH concentration after the induction of I/R injury (Figure 2b). This can be due to the diminished testosterone feedback. The significant reduction in plasma testosterone level in the I/R group has been observed in the other investigations too (14). Another reason for the elevation in the LH levels is probably insufficient renal excretion. In agreement with our results, a decrease in the testosterone serum level concomitant to the elevated LH levels in patients who suffer from chronic renal failure has been reported previously (15, 16). An interpretation for the significant reduction in plasma testosterone level in the I/R group, despite the elevated LH levels, is that the response of testis to the LH tends to be reduced. In this regard, there is evidence of the existence of a factor in uremic serum which can block the LH receptor and is inversely correlated with the GFR (17). The reduced circulating LH bioactivity had been reported in chronic kidney failure (18). Moreover, the elevation in the FSH levels is probably due to decreased inhibin, which is produced by the Sertoli cells (16). Recently, a dysfunction of Sertoli cell was reported in the men suffering from an end-stage renal disease (19). FSH stimulates spermatogenesis. Histopathological study of the testis in the I/R group showed some disturbances in the seminiferous tubules, including the thickening of the basement membrane of the tubules, increased interstitial space, and decreased number of spermatogenic cells, particularly the number of spermatogonia. Testosterone, as a steroid hormone, is needed for spermatogenesis (20). Antioxidants can protect the cells and tissues against the detrimental effects of free radicals (21). The administration of berberine to the I/R group significantly augmented the level of testosterone. The spermatogenic inhibition observed in the I/R group in the current work cannot merely be caused due to the reduction in the plasma testosterone level. In addition to the hormonal change, the spermatogenic inhibition may also be created consequently to the establishment of free radicals in the testis due to their harmful effect on spermatogenesis. The improvement in the spermatogenesis observed in the BBR + I/R group may be associated with the antioxidant property of the berberine. Berberine is described by a variety of pharmacological effects including antioxidant and anti-inflammatory properties (22). In agreement with our results, berberine improved the testosterone level in the conditions of testicular inflammation and oxidative stress induced by gossypol (23). In the current research, the administration of berberine (15 mg/kg) for seven serial days significantly diminished the I/R-induced increase in the plasma levels of LH and FSH hormones. This decrease of LH and FSH levels could be due to the ameliorative effect of berberine on the function of both kidney and testis. The improvement in the renal function, as indicated by a reduction in I/R-induced increment in plasma levels of Cr and BUN, led to sufficient excretion of LH. Besides, the decrease of renal I/R-induced testicular damages by berberine resulted in improved function of sertoli cells. Consequently, plasma FSH level returned to normalcy due to sufficient inhibition by inhibin.
5.Conclusion
In summary, 45-min renal ischemia/24-hr reperfusion caused renal and testicular dysfunction. It also induced disturbances in the pituitary-gonadal axis. Gavage administration of berberine prior to the induction of renal I/R injury blunted functional disorders of kidney and testis and consequently diminished the increases in plasma levels of creatinine, urea nitrogen, LH and FSH, as well as a decrease in plasma level of testosterone. Our findings propose that berberine has the potential therapeutic property for the amelioration of testicular damages induced by renal I/R injury due to its antioxidant and anti-inflammatory properties.
Acknowledgments
The authors wish to acknowledge the Research Council of Shiraz University, Shiraz, Iran, for providing the financial support of this study (grant no. 88-GR-SCST-117).
Conflict of interest
The authors of this article declare that they have no conflict of interest.
Full-Text: (620 Views)
- Introduction
Considering the potential therapeutic properties of berberine, the goals of this experiment were to determine the effects of AKI on the testicular function and to assess the effect of berberine on testicular damages induced by renal I/R injury.
- Materials and methods
- Experimental procedure
- Biochemical tests
- Histopathological evaluation

2.4.Ethical consideration
All interventions in rats were provided according to the protocol provided by the ethics committee of Shiraz University (code: 900794).
2.5.Statistical analysis
Experimental data (mean ± SD) were analyzed using the SPSS statistics software package (SPSS for Windows version 16, Chicago, IL, USA). The normal distribution was tested by Shapiro-Wilk. Comparison between groups was calculated by one-way ANOVA and Tukey’s post-hoc test. The histopathological scores were statistically compared between groups by Kruskal-Wallis multiple comparison tests, and binary comparisons were done by Mann-Whitney U test. P < 0.05 was considered significant.
3.Results
3.1.Berberine ameliorates the I/R-induced changes in biochemical parameters
As shown in figure 1, at the end of 24 hr reperfusion period, the plasma levels of creatinine and urea nitrogen were statistically higher in I/R group in comparison with those of sham and BBR groups (p < 0.001). However, in the BBR + I/R group, there was a significant decrease in creatinine (Figure 1a) and BUN (Figure 1b) levels compared to the I/R group (p < 0.001). Figure 2a shows that in the I/R group, the plasma testosterone level was significantly decreased with respect to its level in the sham and BBR groups (p < 0.001). The testosterone level was increased in the BBR + I/R group in comparison to the I/R group (p < 0.001), while it was lower than the level in the sham and BBR groups (Figure 2a). Besides, plasma levels of LH and FSH observed were significantly increased in the I/R group compared to the sham and BBR groups (p < 0.001). But berberine pretreatment diminished the plasma levels of LH (Figure 2b) and FSH (Figure 2c) in the BBR + I/R group in comparison with the I/R group (p < 0.001).
3.2. Berberine protects the I/R-induced histological changes in testicular tissue
Figures 3, 4, and 5 shows that there were no detectable histological changes to the testes of the sham and BBR groups. However, the most prominent lesions in the I/R group (Figure 3, 4, 5) were increased number of interstitial Leydig cells (hyperplasia), increase in the volume percent of interstitial space and internal space of seminiferous tubules, decrease in the number of spermatogenic cells, and thickening of the tubular basement membrane. In the BBR + I/R group, less intense damages were noticed in comparison with the I/R group (Figures 3, 4, 5).


4.Discussion
The AKI is assumed as a pan-organ problem with negative consequences on many other organs in the body (11). The main goal of this study was to evaluate the effect of 45 min ischemia/24 hr reperfusion on functional-morphological characteristics of the testis in rats. The reason for considering 45-min ischemia/24 hr reperfusion as a timing of ischemia and reperfusion was that a minimum of 30 min ischemia is needed to induce AKI. Besides, mitochondrial function is restored by reperfusion when ischemic interval is 45 min or less. However, ischemic intervals longer than 45 min produce non-reversible impairment of ATP synthesis, and the marked reduction following 90 min of ischemia signifies possible transition to a non-viable state (12). Also, the maximum renal dysfunction following 30-45 min of renal ischemia happens at the end of 24 hr reperfusion period (13). The renal IRI resulted in testicular histological damages accompanied with increased plasma levels of creatinine, urea nitrogen, LH, and FSH, as well decrease of plasma testosterone concentration. Berberine diminished histological damage to the testis and attenuated the increase in plasma creatinine, urea nitrogen, LH, FSH, and decrease in plasma testosterone concentration in the BBR + I/R group.
In sham rats, the seminiferous tubules had normal size and were full of spermatogenic cells, with minimal interstitial connective tissue and a small number of Leydig cells. Morphological study of the testicular sections in the I/R group revealed a decreased number of spermatogenic cells, thickening of basement membrane, and Leydig cell hyperplasia. As very high quantities of testosterone are essential for the survival of the reproductive tract, it is concluded that this atrophy of seminiferous tubules is probably developed due to the reduction in the testosterone levels. Besides, Leydig cell hyperplasia might be created to offset the reduced testosterone level.
Our results showed elevated plasma LH concentration after the induction of I/R injury (Figure 2b). This can be due to the diminished testosterone feedback. The significant reduction in plasma testosterone level in the I/R group has been observed in the other investigations too (14). Another reason for the elevation in the LH levels is probably insufficient renal excretion. In agreement with our results, a decrease in the testosterone serum level concomitant to the elevated LH levels in patients who suffer from chronic renal failure has been reported previously (15, 16). An interpretation for the significant reduction in plasma testosterone level in the I/R group, despite the elevated LH levels, is that the response of testis to the LH tends to be reduced. In this regard, there is evidence of the existence of a factor in uremic serum which can block the LH receptor and is inversely correlated with the GFR (17). The reduced circulating LH bioactivity had been reported in chronic kidney failure (18). Moreover, the elevation in the FSH levels is probably due to decreased inhibin, which is produced by the Sertoli cells (16). Recently, a dysfunction of Sertoli cell was reported in the men suffering from an end-stage renal disease (19). FSH stimulates spermatogenesis. Histopathological study of the testis in the I/R group showed some disturbances in the seminiferous tubules, including the thickening of the basement membrane of the tubules, increased interstitial space, and decreased number of spermatogenic cells, particularly the number of spermatogonia. Testosterone, as a steroid hormone, is needed for spermatogenesis (20). Antioxidants can protect the cells and tissues against the detrimental effects of free radicals (21). The administration of berberine to the I/R group significantly augmented the level of testosterone. The spermatogenic inhibition observed in the I/R group in the current work cannot merely be caused due to the reduction in the plasma testosterone level. In addition to the hormonal change, the spermatogenic inhibition may also be created consequently to the establishment of free radicals in the testis due to their harmful effect on spermatogenesis. The improvement in the spermatogenesis observed in the BBR + I/R group may be associated with the antioxidant property of the berberine. Berberine is described by a variety of pharmacological effects including antioxidant and anti-inflammatory properties (22). In agreement with our results, berberine improved the testosterone level in the conditions of testicular inflammation and oxidative stress induced by gossypol (23). In the current research, the administration of berberine (15 mg/kg) for seven serial days significantly diminished the I/R-induced increase in the plasma levels of LH and FSH hormones. This decrease of LH and FSH levels could be due to the ameliorative effect of berberine on the function of both kidney and testis. The improvement in the renal function, as indicated by a reduction in I/R-induced increment in plasma levels of Cr and BUN, led to sufficient excretion of LH. Besides, the decrease of renal I/R-induced testicular damages by berberine resulted in improved function of sertoli cells. Consequently, plasma FSH level returned to normalcy due to sufficient inhibition by inhibin.
5.Conclusion
In summary, 45-min renal ischemia/24-hr reperfusion caused renal and testicular dysfunction. It also induced disturbances in the pituitary-gonadal axis. Gavage administration of berberine prior to the induction of renal I/R injury blunted functional disorders of kidney and testis and consequently diminished the increases in plasma levels of creatinine, urea nitrogen, LH and FSH, as well as a decrease in plasma level of testosterone. Our findings propose that berberine has the potential therapeutic property for the amelioration of testicular damages induced by renal I/R injury due to its antioxidant and anti-inflammatory properties.
Acknowledgments
The authors wish to acknowledge the Research Council of Shiraz University, Shiraz, Iran, for providing the financial support of this study (grant no. 88-GR-SCST-117).
Conflict of interest
The authors of this article declare that they have no conflict of interest.
Type of Study: Original Article |
References
1. Bonventre JV, Zuk A. Ischemic acute renal failure: an inflammatory disease? Kidney Int 2004; 66: 480-485. [DOI:10.1111/j.1523-1755.2004.761_2.x] [PMID]
2. Rouschop KM, Roelofs JJ, Claessen N, da Costa Martins P, Zwaginga JJ, Pals ST, et al. Protection against renal ischemia reperfusion injury by CD44 disruption. J Am Soc Nephrol 2005; 16: 2034-2043. [DOI:10.1681/ASN.2005010054] [PMID]
3. Shiao CC, Wu PC, Huang TM, Lai TS, Yang WS, Wu CH, et al. Long-term remote organ consequences following acute kidney injury. Crit Care 2015; 19: 438. [DOI:10.1186/s13054-015-1149-5] [PMID] [PMCID]
4. Karagiannis A, Harsoulis F. Gonadal dysfunction in systemic diseases. Eur J Endocrinol 2005; 152: 501-513. [DOI:10.1530/eje.1.01886] [PMID]
5. Adachi Y, Nakada T. Effect of experimentally induced renal failure on testicular testosterone synthesis in rats. Arch Androl 1999; 43: 37-45. [DOI:10.1080/014850199262715] [PMID]
6. El-Assaly NM, El-Ashry NI, Waked E, El-Damarawy M. Gonadal dysfunction in chronic renal failure. Aust J Basic & Appl Sci 2008; 2: 481-487.
7. Kuo CL, Chi CW, Liu TY. The anti-inflammatory potential of berberine in vitro and in vivo. Cancer Lett 2004; 203: 127-137. [DOI:10.1016/j.canlet.2003.09.002] [PMID]
8. Li Z, Geng YN, Jiang JD, Kong WJ. Antioxidant and anti-inflammatory activities of berberine in the treatment of diabetes mellitus. Evid Based Complement Alternat Med 2014; 2014: 289264. [DOI:10.1155/2014/289264] [PMID] [PMCID]
9. Peng L, Kang S, Yin Z, Jia R, Song X, Li L, et al. Antibacterial activity and mechanism of berberine against Streptococcus agalactiae. Int J Clin Exp Pathol 2015; 8: 5217-5223.
10. Strenberg SS. Diagnostic surgical pathology. Third Ed. Philadelphia: Lippincott Williams & Wilkins; 1996.
11. Kelly KJ. Acute renal failure: much more than a kidney disease. Semin Nephrol 2006; 26: 105-113. [DOI:10.1016/j.semnephrol.2005.09.003] [PMID]
12. Irazu CE, Ruidera E, Singh I, Orak JK, Fitts CT, Rajagopalan PR. Effect of ischemia and 24 hour reperfusion on ATP synthesis in the rat kidney. J Exp Pathol 1989; 4: 29-36.
13. Williams P, Lopez H, Britt D, Chan C, Ezrin A, Hottendorf R. Characterization of renal ischemia-reperfusion injury in rats. J Pharmacol Toxicol Methods 1997; 37: 1-7. [DOI:10.1016/S1056-8719(96)00141-4]
14. Levitan D, Moser SA, Goldstein DA, Kletzky OA, Lobo RA, Massry SG. Disturbances in the hypothalamic-pituitary-gonadal axis in male patients with acute renal failure. Am J Nephrol 1984; 4: 99-106. [DOI:10.1159/000166785] [PMID]
15. Handelsman DJ, Dong Q. Hypothalamo-pituitary gonadal axis in chronic renal failure. Endocrinol Metab Clin North Am 1993; 22: 145-161. [DOI:10.1016/S0889-8529(18)30184-1]
16. Palmer BF. Sexual dysfunction in uremia. J Am Soc Nephrol 1999; 10: 1381-1388.
17. Dunkel L, Raivio T, Laine J, Holmberg C. Circulating luteinizing hormone receptor inhibitor(s) in boys with chronic renal failure. Kidney Int 1997; 51: 777-784. [DOI:10.1038/ki.1997.109] [PMID]
18. Stewart-Bentley M, Gans D, Horton R. Regulation of gonadal function in uremia. Metabolism 1974; 23: 1065-1072. [DOI:10.1016/0026-0495(74)90073-0]
19. Eckersten D, Giwercman A, Christensson A. Male patients with terminal renal failure exhibit low serum levels of antimüllerian hormone. Asian J Androl 2015; 17: 149-153. [DOI:10.4103/1008-682X.135124] [PMID] [PMCID]
20. Smith LB, Walker WH. The regulation of spermatogenesis by androgens. Semin Cell Dev Biol 2014; 30: 2-13. [DOI:10.1016/j.semcdb.2014.02.012] [PMID] [PMCID]
21. Kurutas EB. The importance of antioxidants which play the role in cellular response against oxidative/nitrosative stress: current state. Nutr J 2016; 15: 71. [DOI:10.1186/s12937-016-0186-5] [PMID] [PMCID]
22. Imenshahidi M, Hosseinzadeh H. Berberis vulgaris and berberine: an update review. Phytother Res 2016; 30: 1745-1764. [DOI:10.1002/ptr.5693] [PMID]
23. Saleh SR, Attia R, Ghareeb DA. The ameliorating effect of berberine-rich fraction against gossypol-induced testicular inflammation and oxidative stress. Oxid Med Cell Longev 2018; 2018: 1056173. [DOI:10.1155/2018/1056173] [PMID] [PMCID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








