Sun, Feb 1, 2026
[Archive]
Volume 17, Issue 11 (November 2019)
IJRM 2019, 17(11): 851-856 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghasemi M, Esmailzadeh A. An unusual appearance of the post-pubertal Herlyn-Werner-Wunderlich syndrome with acute abdominal pain: A case report. IJRM 2019; 17 (11) :851-856
URL: http://ijrm.ir/article-1-1725-en.html
URL: http://ijrm.ir/article-1-1725-en.html
1- Department of Obstetrics and Gynecology, Pregnancy Health Research Center, Zahedan University of Medical Sciences, Zahedan, Iran. , drghasemim@yahoo.com, drghasemi@zaums.ac.ir
2- Department of Obstetrics and Gynecology, Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran.
2- Department of Obstetrics and Gynecology, Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran.
Keywords: Herlyn-Werner-Wunderlich syndrome, Uterus didelphys, Kidney agenesis, Mullerian duct anomaly
Full-Text [PDF 321 kb]
(1228 Downloads)
| Abstract (HTML) (4045 Views)
In this report, we described an unusual case of a young girl with HWW syndrome with pyocolpus, peritonitis, and endometriosis that was successfully treated by resectioning vaginal septum, salpingectomy, and pus drainage.
We decided to do abdominal and pelvic computed tomography scan to evaluate the cystic mass which was reported in abdominal ultrasound imaging. We had planned to do the surgery in an appropriate condition. This meant with patient’s intestinal preparation after evaluating computed tomography results, and in the presence of an expert general surgeon. However, a few hours after the admission, we had to do an emergency surgery on the same night because she had a high fever, increased ESR and CRP, and a possible risk of septic shock. We administered many antibiotics before the emergency surgery because of the acute abdominal pain.
During the first surgery, we did a physical examination while she was under anesthesia. The hymen was normal and intact. But a buldge was found in the right side of her vagina during the rectoabdominal examination. This was confirmed by vaginal examination with a speculum. The right longitudinal septum was revealed with a closed end. At first, we cut the closed end of the hemilateral obstruction of the vagina and then the vaginal septum was resected with an electrocautery device. Afterward, a 200-cc pus was drained out, and this sample was sent to a laboratory for culture and antibiogram.
The patient’s abdomen was opened with a midline incision. There was a severe adhesion of the intestine and omentum to the abdominal wall. Since no intestinal preparation had been done and there was a high risk of intestinal rupture, the general surgeon decided that it would be better to end this surgery and prepare the patient for another abdominal surgery in better conditions.
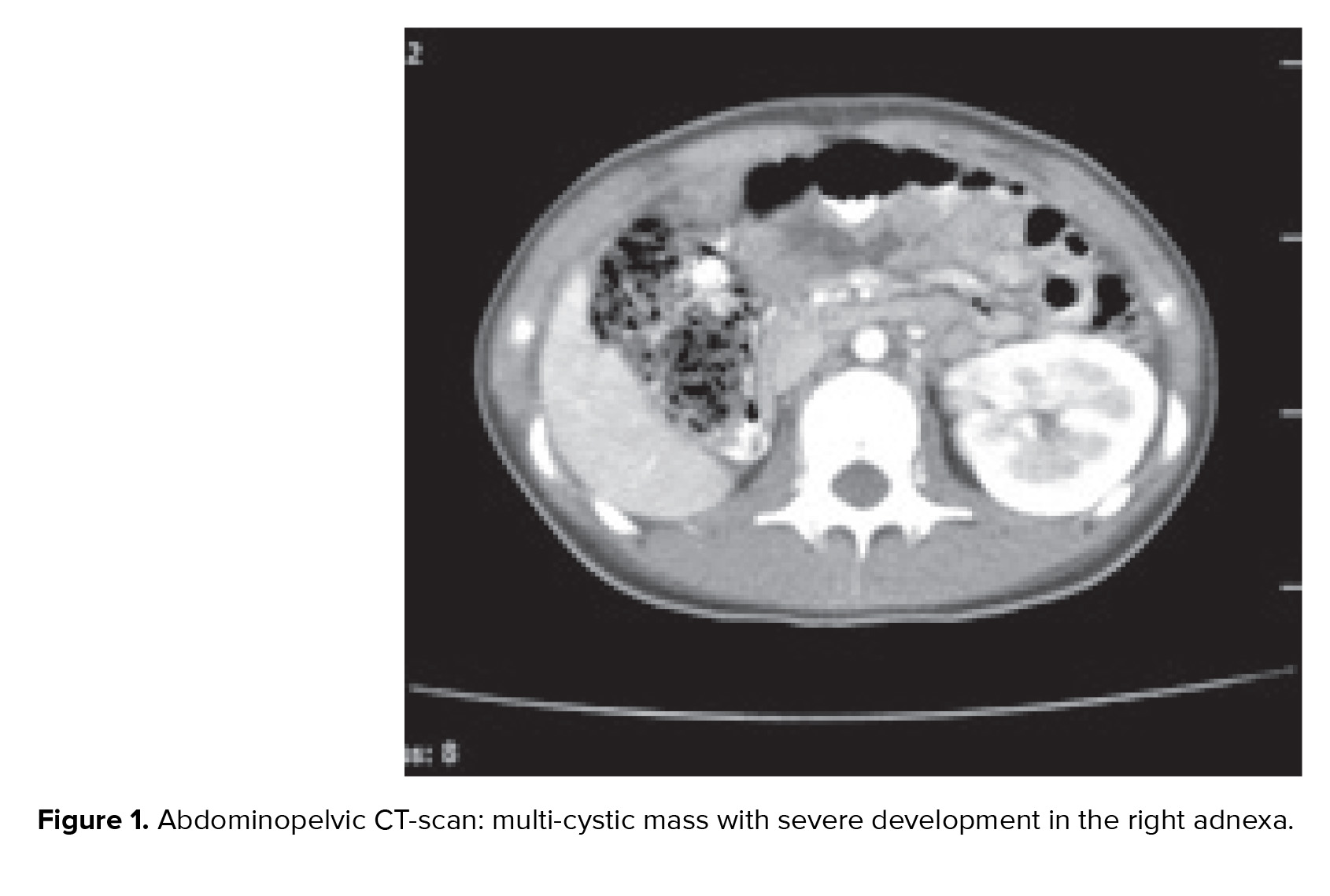
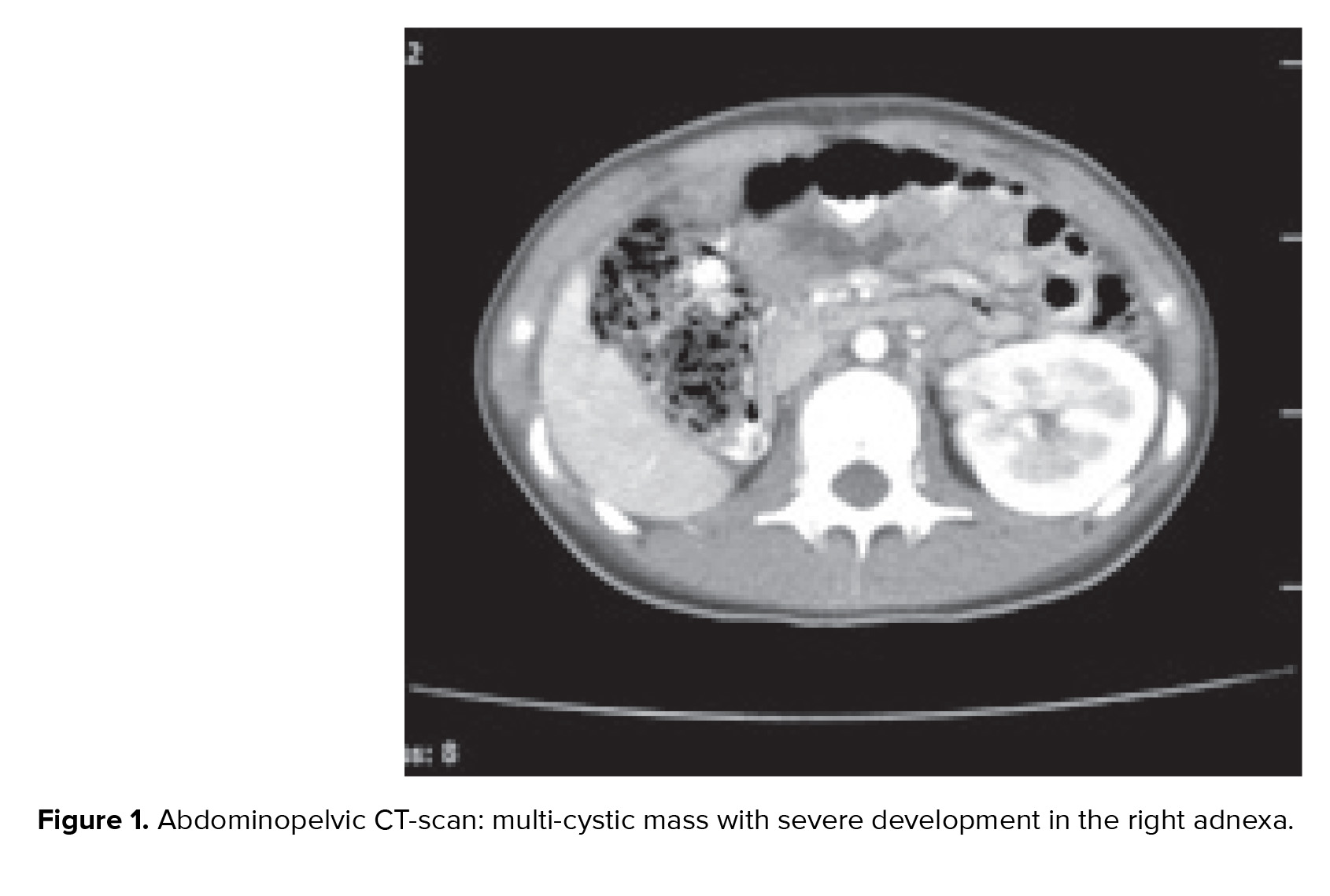
Abdominopelvic-computed tomography scan (with and without contrast which was done after the first surgery) confirmed the ultrasound imaging findings of uterus didelphys with multi-cystic mass with severe development in the right adnexa. A remarkable right hematocolpus hematosalpynx was seen that was due to longitudinal vaginal septum and hemivaginal obstruction. The right kidney was not observed (Figures 1, 2). Her problem was detected as HWW syndrome infected with pyocolpos.
We did the second laparotomy in less than 48 hr after the first surgery with the same incision in the presence of an expert surgeon. Our patient had severe intestinal adhesion and perforated appendix fistulated to the right fallopian tube beside distal small intestinal obstruction. We saw pelvic inflammatory mass beside endometriosis. We did an appendectomy, right salpingectomy, entrolysis, and abscess drainage. Cefepim (Maxipim) and cloxacillin (Jaber-ibn-Hayyan pharmaceutical co) were administrated intravenously as specific infectious disease drugs until seven days after the surgery according to the specimen culture. We ordered continuous low-dosage contraceptive drugs for preventing the progression of endometriosis. Our patient was discharged from the hospital after seven days with a good condition.

Ethical consideration
After the completion of treatment, we asked the patient for the permission to publish her anomaly as a case report. She accepted and gave us an oral consent.
Dongan and colleagues classified the HWW syndrome into two types: complete or incomplete vaginal septum (4). Tong and colleagues stated that the age of pelvic endometriosis onset is earlier than the age of finding endometriosis. Approximately, in 88.89% of HWW syndrome cases, the patients are affected by endometriosis (9). They are usually diagnosed in the pubertal or post-pubertal period, but Angotti and colleagues reported six cases of this problem in girls younger than five years old (8). The resectioning of the vaginal septum in obstructive hemivagina should be done through an abdominal or transvaginal approach (8).
In our case after confirming the HWW syndrome with the computed tomographic scan, we did a vaginal septum resection. Our case was complicated because of pyosalpinx. So, investigative laparotomy was done. A two-step surgery is recommended in similar cases by pyocolpus for a complete vaginal septum resection (6). Sometimes, the closure of an opening will occur at the end of one year (4). Doing a complete vaginal septum resection is necessary for assuring the future fertility, while uterus didelphys has no effect on reducing the infertility. So, fertility prognoses remain good after surgery in uncomplicated cases (2, 4).
This report described a case of the unusual type of HWW syndrome with fever and acute abdominal pain. The main complaint of our patient was only severe dysmenorrhea. Cyclic abdominal pain, abdominal mass, dysmenorrhea, with or without urinary disorders, can lead to this problem in adolescence. So, the symptoms should be emphasized in early puberty to prevent more complications. Well-timed removal of the vaginal septum can improve fertility and endometriosis. Also, it decreases pyosalpinx, acute abdominal pain, and further surgeries.
A limitation of our work was doing the surgery twice. If the patient was in a better condition, we could have done the surgery same as many other cases with opening the obstruction of vagina and laparoscopy. However, because of the different situation of the studied case and that she had a acute abdominal pain that could be a sign of infection, we tried to avoid sepsis with doing the surgery in two steps.
Conclusion
Although dysmenorrhea is among girls in puberty, it is advised to follow-up acute dysmenorrhea soon to avoid further medical consequences.
Acknowledgments
The authors would like to thank the patient for her consent on publishing the case. They are also thankful to Muhammed Hussein Mousavinasab for editing this text.
Conflict of interest
The authors report no conflicts of interest.
Full-Text: (670 Views)
- Introduction
In this report, we described an unusual case of a young girl with HWW syndrome with pyocolpus, peritonitis, and endometriosis that was successfully treated by resectioning vaginal septum, salpingectomy, and pus drainage.
- Case presentation
We decided to do abdominal and pelvic computed tomography scan to evaluate the cystic mass which was reported in abdominal ultrasound imaging. We had planned to do the surgery in an appropriate condition. This meant with patient’s intestinal preparation after evaluating computed tomography results, and in the presence of an expert general surgeon. However, a few hours after the admission, we had to do an emergency surgery on the same night because she had a high fever, increased ESR and CRP, and a possible risk of septic shock. We administered many antibiotics before the emergency surgery because of the acute abdominal pain.
During the first surgery, we did a physical examination while she was under anesthesia. The hymen was normal and intact. But a buldge was found in the right side of her vagina during the rectoabdominal examination. This was confirmed by vaginal examination with a speculum. The right longitudinal septum was revealed with a closed end. At first, we cut the closed end of the hemilateral obstruction of the vagina and then the vaginal septum was resected with an electrocautery device. Afterward, a 200-cc pus was drained out, and this sample was sent to a laboratory for culture and antibiogram.
The patient’s abdomen was opened with a midline incision. There was a severe adhesion of the intestine and omentum to the abdominal wall. Since no intestinal preparation had been done and there was a high risk of intestinal rupture, the general surgeon decided that it would be better to end this surgery and prepare the patient for another abdominal surgery in better conditions.
Abdominopelvic-computed tomography scan (with and without contrast which was done after the first surgery) confirmed the ultrasound imaging findings of uterus didelphys with multi-cystic mass with severe development in the right adnexa. A remarkable right hematocolpus hematosalpynx was seen that was due to longitudinal vaginal septum and hemivaginal obstruction. The right kidney was not observed (Figures 1, 2). Her problem was detected as HWW syndrome infected with pyocolpos.
We did the second laparotomy in less than 48 hr after the first surgery with the same incision in the presence of an expert surgeon. Our patient had severe intestinal adhesion and perforated appendix fistulated to the right fallopian tube beside distal small intestinal obstruction. We saw pelvic inflammatory mass beside endometriosis. We did an appendectomy, right salpingectomy, entrolysis, and abscess drainage. Cefepim (Maxipim) and cloxacillin (Jaber-ibn-Hayyan pharmaceutical co) were administrated intravenously as specific infectious disease drugs until seven days after the surgery according to the specimen culture. We ordered continuous low-dosage contraceptive drugs for preventing the progression of endometriosis. Our patient was discharged from the hospital after seven days with a good condition.

Ethical consideration
After the completion of treatment, we asked the patient for the permission to publish her anomaly as a case report. She accepted and gave us an oral consent.
- Discussion
Dongan and colleagues classified the HWW syndrome into two types: complete or incomplete vaginal septum (4). Tong and colleagues stated that the age of pelvic endometriosis onset is earlier than the age of finding endometriosis. Approximately, in 88.89% of HWW syndrome cases, the patients are affected by endometriosis (9). They are usually diagnosed in the pubertal or post-pubertal period, but Angotti and colleagues reported six cases of this problem in girls younger than five years old (8). The resectioning of the vaginal septum in obstructive hemivagina should be done through an abdominal or transvaginal approach (8).
In our case after confirming the HWW syndrome with the computed tomographic scan, we did a vaginal septum resection. Our case was complicated because of pyosalpinx. So, investigative laparotomy was done. A two-step surgery is recommended in similar cases by pyocolpus for a complete vaginal septum resection (6). Sometimes, the closure of an opening will occur at the end of one year (4). Doing a complete vaginal septum resection is necessary for assuring the future fertility, while uterus didelphys has no effect on reducing the infertility. So, fertility prognoses remain good after surgery in uncomplicated cases (2, 4).
This report described a case of the unusual type of HWW syndrome with fever and acute abdominal pain. The main complaint of our patient was only severe dysmenorrhea. Cyclic abdominal pain, abdominal mass, dysmenorrhea, with or without urinary disorders, can lead to this problem in adolescence. So, the symptoms should be emphasized in early puberty to prevent more complications. Well-timed removal of the vaginal septum can improve fertility and endometriosis. Also, it decreases pyosalpinx, acute abdominal pain, and further surgeries.
A limitation of our work was doing the surgery twice. If the patient was in a better condition, we could have done the surgery same as many other cases with opening the obstruction of vagina and laparoscopy. However, because of the different situation of the studied case and that she had a acute abdominal pain that could be a sign of infection, we tried to avoid sepsis with doing the surgery in two steps.
Conclusion
Although dysmenorrhea is among girls in puberty, it is advised to follow-up acute dysmenorrhea soon to avoid further medical consequences.
Acknowledgments
The authors would like to thank the patient for her consent on publishing the case. They are also thankful to Muhammed Hussein Mousavinasab for editing this text.
Conflict of interest
The authors report no conflicts of interest.
Type of Study: Case Report |
References
1. Ma I, Williamson A, Rowe D, Ritchey M, Graziano K. OHVIRA with a twist: obstructed hemivagina ipsilateral renal anomaly with urogenital sinus in 2 patients. J Pediatr Adolesc Gynecol 2014; 27: 104-106. [DOI:10.1016/j.jpag.2013.06.015] [PMID]
2. Sanghvi Y, Shastri P, Mane SB, Dhende NP. Prepubertal presentation of Herlyn-Werner-Wunderlich syndrome: a case report. J Pediatr Surg 2011; 46: 1277-1280. [DOI:10.1016/j.jpedsurg.2011.02.067] [PMID]
3. Guducu N, Gonenc G, Isci H, Yigiter AB, Dunder I. Herlyn-werner-wunderlich syndrome-timely diagnosis is important to preserve fertility. J Pediatr Adolesc Gynecol 2012; 25: e111-e112. [DOI:10.1016/j.jpag.2012.05.013] [PMID]
4. Dogan A, Uyar I, Demirtas GS, Ekin A, Gulhan I, Ertas IE, et al. Urinary incontinence in puberty: a rare clinical presentation of the herlyn-werner-wunderlich syndrome. J Pediatr Adolesc Gynecol 2016; 29: e101-e103. [DOI:10.1016/j.jpag.2016.07.013] [PMID]
5. Yavuz A, Bora A, Kurdoglu M, Goya C, Kurdoglu Z, Beyazal M, et al. Herlyn-werner-wunderlich syndrome: merits of sonographic and magnetic resonance imaging for accurate diagnosis and patient management in 13 cases. J Pediatr Adolesc Gynecol 2015; 28: 47-52. [DOI:10.1016/j.jpag.2014.03.004] [PMID]
6. Jung EJ, Cho MH, Kim DH, Byun JM, Kim YN, Jeong DH, et al. Herlyn-werner-wunderlich syndrome: an unusual presentation with pyocolpos. Obstet Gynecol Sci 2017; 60: 374-377. [DOI:10.5468/ogs.2017.60.4.374] [PMID] [PMCID]
7. Yung SS, Ngu SF, Cheung VY. Late presentation of a variant of Herlyn-Werner-Wunderlich syndrome. Int J Gynaecol Obstet 2016; 133: 238-239. [DOI:10.1016/j.ijgo.2015.10.006] [PMID]
8. Angotti R, Molinaro F, Bulotta AL, Bindi E, Cerchia E, Sica M, et al. Herlyn-Werner-Wunderlich syndrome: An "early" onset case report and review of Literature. Int J Surg Case Rep 2015; 11: 59-63. [DOI:10.1016/j.ijscr.2015.04.027] [PMID] [PMCID]
9. Tong J, Zhu L, Chen N, Lang J. Endometriosis in association with Herlyn-Werner-Wunderlich syndrome. Fertil Steril 2014; 102: 790-794. [DOI:10.1016/j.fertnstert.2014.05.025] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








