Mon, Dec 22, 2025
[Archive]
Volume 19, Issue 11 (November 2021)
IJRM 2021, 19(11): 969-978 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sadatinejad S M, Farokhian A, Taghadosi M, Mosavi S G. The effect of sexual counseling on depression, anxiety, stress, sexual knowledge and sexual quality of life in men who have undergone invasive coronary interventions: An RCT. IJRM 2021; 19 (11) :969-978
URL: http://ijrm.ir/article-1-1826-en.html
URL: http://ijrm.ir/article-1-1826-en.html
1- Pediatric Group, Bahrami Children Hospital, Tehran University of Medical Sciences, Tehran, Iran. Students Research Committee, Kashan University of Medical Sciences, Kashan, Iran.
2- Internal Medicine Group, Medicine Faculty, Kashan University of Medical Sciences, Kashan, Iran.
3- Medical Surgical Nursing, Trauma Nursing Research Center, Faculty of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran. ,taghadosi_m@kaums.ac.ir
4- Biostatistics Group, Health Faculty, Kashan University of Medical Sciences, Kashan, Iran.
2- Internal Medicine Group, Medicine Faculty, Kashan University of Medical Sciences, Kashan, Iran.
3- Medical Surgical Nursing, Trauma Nursing Research Center, Faculty of Nursing and Midwifery, Kashan University of Medical Sciences, Kashan, Iran. ,
4- Biostatistics Group, Health Faculty, Kashan University of Medical Sciences, Kashan, Iran.
Keywords: Percutaneous transluminal coronary angioplasty, Coronary artery bypass graft, Life quality, Depression, Anxiety neuroses, Sex counseling.
Full-Text [PDF 306 kb]
(1386 Downloads)
| Abstract (HTML) (2483 Views)
Full-Text: (562 Views)
Introduction
Ischemic heart events occur more frequently in men than in women, and occur at younger ages and cause more complications. Sexual dysfunction is a common complication of cardiac events (experienced by over 93% of patients) which may lead to imbalances in the interpersonal relations and affect their quality of life (1, 2). Also, their medications may cause sexual dysfunction (3). Sexual dysfunction occurs in more than half of individuals undergoing open-heart surgery (4). Studies have indicated that 47–85% of patients, mostly men, experience sexual dysfunction after invasive coronary interventions (5-9), and in some cases these complications increase with angioplasty or coronary artery bypass graft (CABG) (10, 11).
Treatment of mental health issues may affect the sexual dysfunction (12). In this regard, education and improvement of couples’ relationships are among the therapeutic methods used. Additionally, providing education in the hospital is a key point (13). Some of the mental health issues (such as stress and anxiety) are caused by a lack of knowledge and information on appropriate sexual and intimate relationships and a lack of physician recommendations before discharge (14).
Studies have reported varied results on sexual counseling. Overemphasis on the increased risk of cardiac attack during coitus by the health care team in sexual counseling may cause sexual dysfunction (15). On the other hand, excessive reassurance may bring harmful consequences by leading to cardiac attacks and readmissions, which will highly affect future sexual relationships. Some counseling interventions improve sexual knowledge, performance, and satisfaction and early patient recovery to normal sexual activities after cardiac events (12) while some results demonstrate the opposite effect (15, 16).
Given the potential positive effects of sexual dysfunction treatment on improving the sexual quality of life, the early diagnosis and treatment of these complications is important (17).
Due to the low sexual quality of life of many cardiac patients (16), increased use of invasive interventions for cardiovascular diseases (10), widespread ignorance about patients’ sexual disorders (18), lack of knowledge and communication skills of health care staff surrounding sexual counseling (14), common concerns of men with cardiovascular disease about their sexual life (19), and lack of comprehensive guidance for sexual counseling of patients with cardiovascular diseases (20), this study was designed to assess the effect of sexual counseling before discharge on sexual knowledge, sexual quality of life, stress, anxiety, and depression in men that have undergone invasive coronary interventions. The results of this study could be used in the rehabilitation of men with cardiovascular diseases to improve their sexual quality of life.
2. Materials and Methods
This was a randomized controlled trial which involved 156 male participants who had undergone invasive coronary interventions (CABG or percutaneous transluminal coronary angioplasty) in the post catheterization department of Shahid Beheshti hospital (Kashan, Iran) from April to September 2018. A continuous sampling method was used. Participants were allocated to the intervention or control group randomly by random computer numbers (performed by the researcher using a calculator). As is convention, multiples of the number two placed the participants in the intervention group, and other numbers placed the participants in the control group.
The inclusion criteria were: married men (living with their wife), aged 35-65 yr, who had undergone invasive coronary interventions. The exclusion criteria were: heart, liver, pulmonary or kidney failure; malignancy; any systemic disease; use of antipsychotic or cytotoxic drugs; severe heart failure (function class III or IV (by New York Heart Association classification)); alcohol or opium abuse (reported by the participants); current depression, anxiety, or stress (based on a DASS-21 score of < 10 for depression, < 8 for anxiety or < 15 for stress); current known sexual dysfunction; or current known psychological disorder.
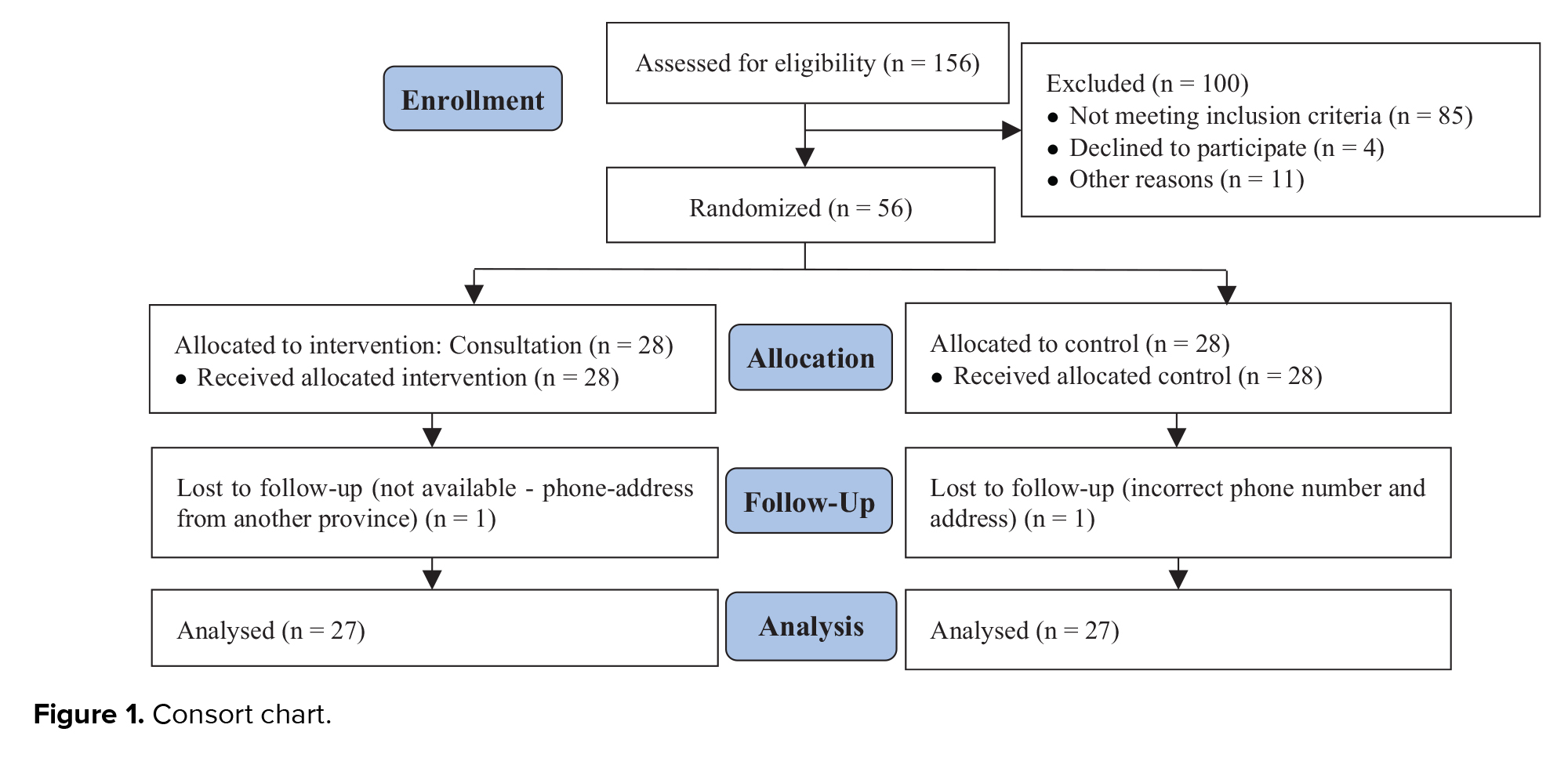
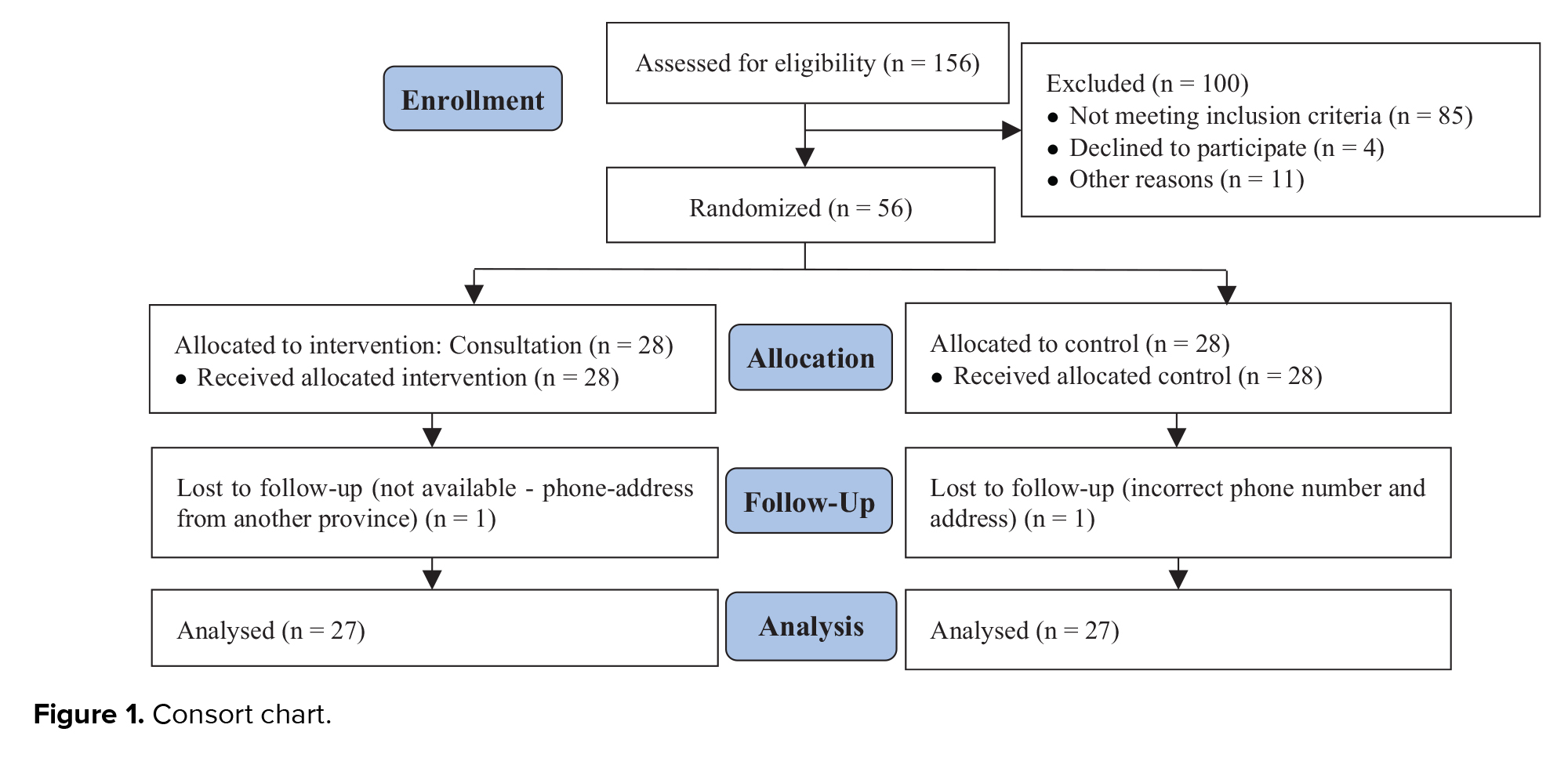
Details are shown in the consort diagram (Figure 1). Demographic information such as age, sex, level of education, history of cardiovascular interventions, occupation, underlying diseases, and medications were recorded, with a focus on confidentiality. Self-reported questionnaires were given to the participants. The questionnaires used were the DASS-21 depression, anxiety, and stress scale, Abraham’s Sexual Quality of Life scale (21), and a sexual knowledge scale (4).
Abraham’s Sexual Quality of Life Scale (for men) has been validated in Persian with a content validity index of 0.87 and a Cronbach’s alpha of 0.82 (21). This scale consists of 11 items, and each item can be rated 1 to 6 points (Likert scale); higher points indicate a higher quality of life. The sexual knowledge scale that was used is a 20-item scale for Men after invasive coronary interventions; its content validity and reliability were shown by Lai et al. (4). Participants were asked to answer questions about sexual knowledge as true or false. The correct answer scored a 1, whereas an incorrect answer was scored as 0. Total scores ranged from 0 to 20, with higher scores indicating greater sexual knowledge. This sexual knowledge scale (4) had a content validity index of 0.78 and a Cronbach’s alpha of 0.73. During translation into the Persian language, three questions (items 18-20) were eliminated as part of cultural adaptation. The reliability of the tool was rechecked and the new Cronbach’s alpha was 0.72 (22). The DASS-21 score validity and reliability have already been demonstrated (23).
The questionnaires were completed twice: before discharge and again two months after discharge (to record prolonged changes). For illiterate participants, the researchers wrote down their exact words.
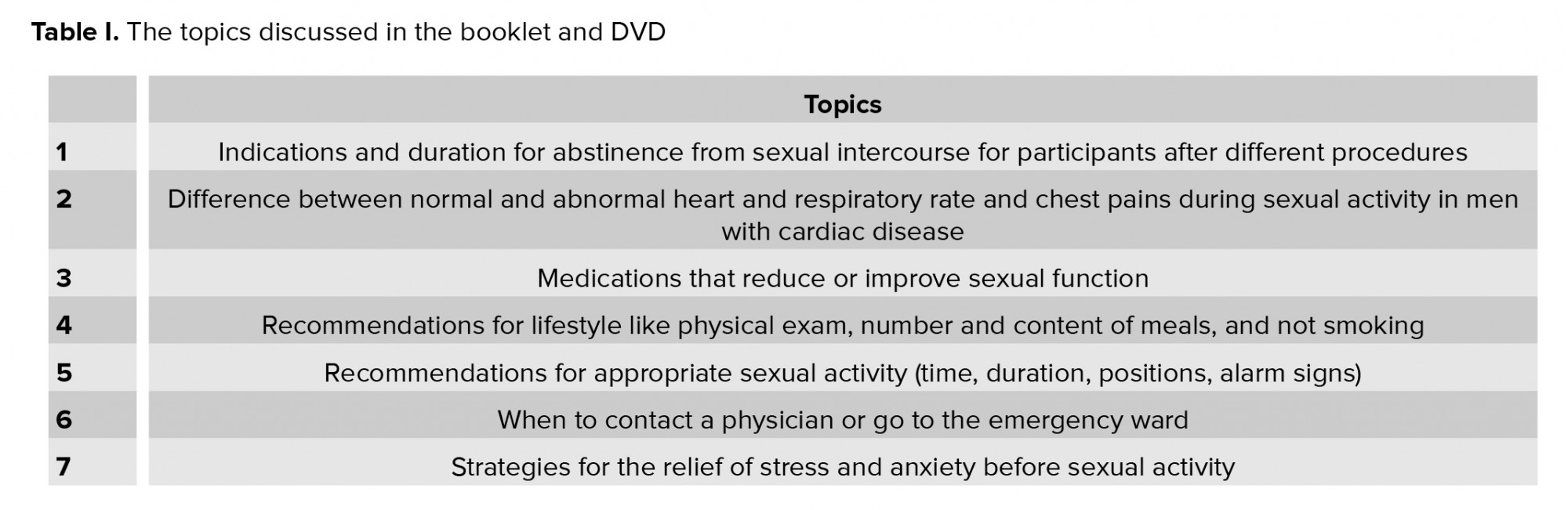
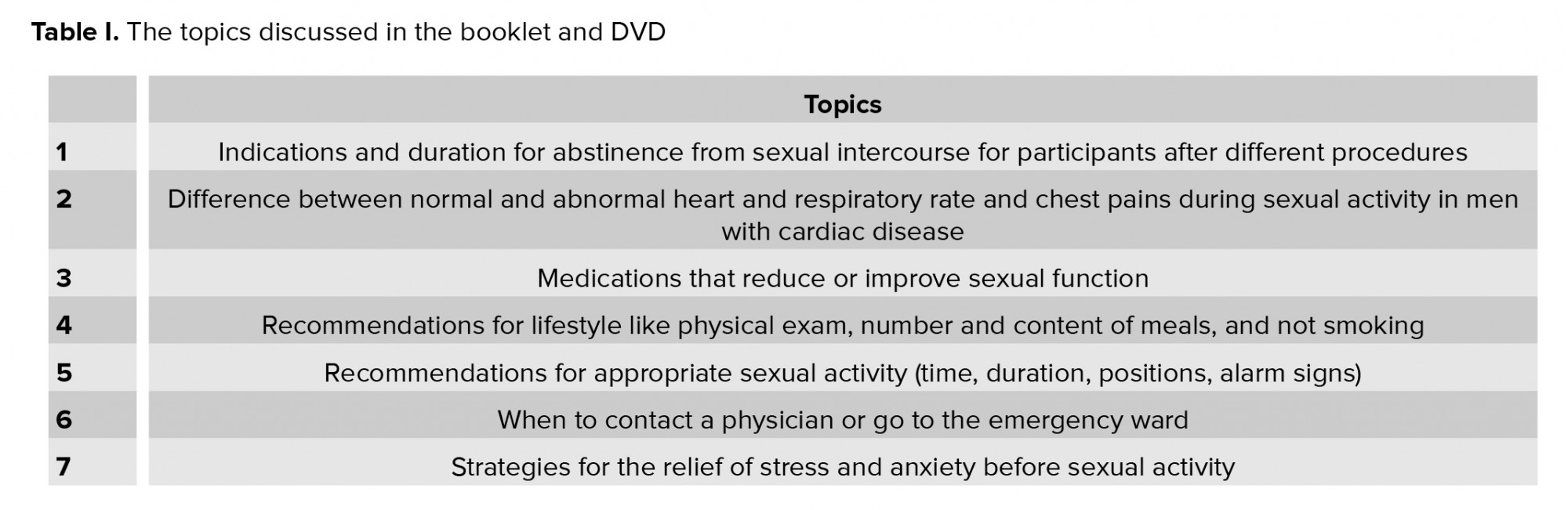
After completing the first questionnaire, participants in the intervention group received sexual counseling along with routine advice, while participants in the control group underwent routine discharge procedures (at a similar meeting, they received the usual health advice). In the intervention group, patients were counseled for 20 min by the researcher and then they were given a booklet and DVD with additional information adapted from authoritative cardiovascular references (24-27) approved by cardiologists and cardiac nurses (Table I). We tried not to let the groups know about each other's training program. The face-to-face counseling session discussed the information in the booklet and participants’ questions were clearly answered. The counseling took place before discharge to reduce bias due to participants’ interactions.
After discharge, the researcher communicated with the participants several times through telephone calls and virtual networks (e.g. WhatsApp) to ensure the participants used the booklet and DVD. Also, participants could ask the researcher any questions. After two months, the same questionnaires were completed again (by telephone call or in-person session).
2.1. Ethical considerations
The study was approved by the Kashan University of Medical Science Research Ethics Committee (Code: IR.KAUMS.MEDNT.REC.1396.97). Informed consent was taken before the intervention and confidentiality was prioritized. Participants were consulted alone to maintain confidentiality and collected data were kept anonymous. Participants could withdraw from the study at any time. In accordance with participants’ rights, participants in the control group received a 20- to 30-minute sexual counseling session by telephone after filling out the questionnaires for the second time.
2.2. Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS, version 16, IBM Company), by Chi-square, t test, paired t test, Leven test, Fisher’s exact test, Kolmogorov-Simonov, Wilcoxon, and ANCOVA. A significance level of p < 0.05 was used.
3. Results
Of the 156 participants initially deemed eligible, 85 did not meet the inclusion criteria. Also 11 participants were excluded due to mental health conditions or sexual dysfunction and four participants did not consent to participate in the study. Two participants could not be contacted for the two-month follow-up (one in the intervention group and one in the control group). Finally, 54 participants remained in the study.
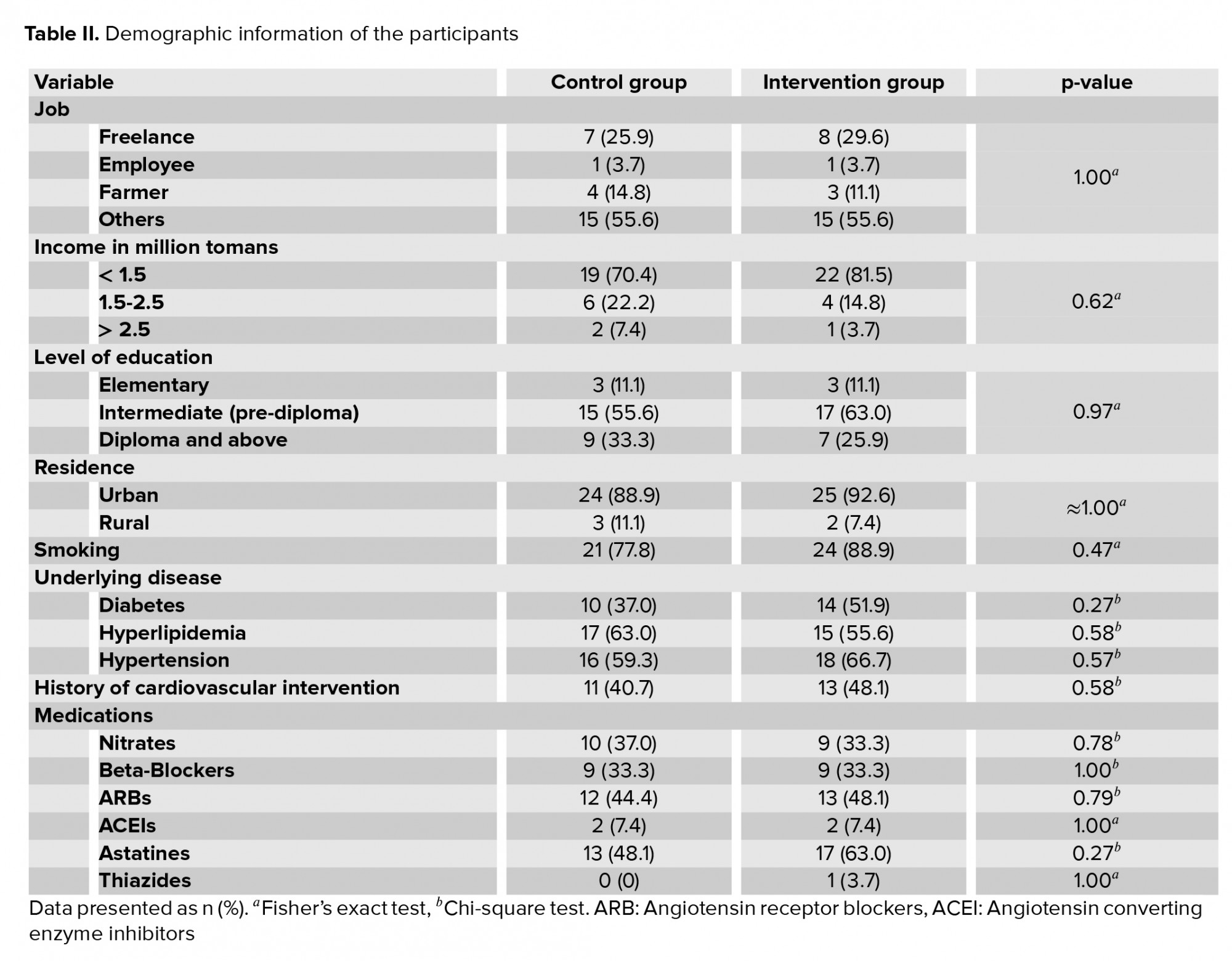
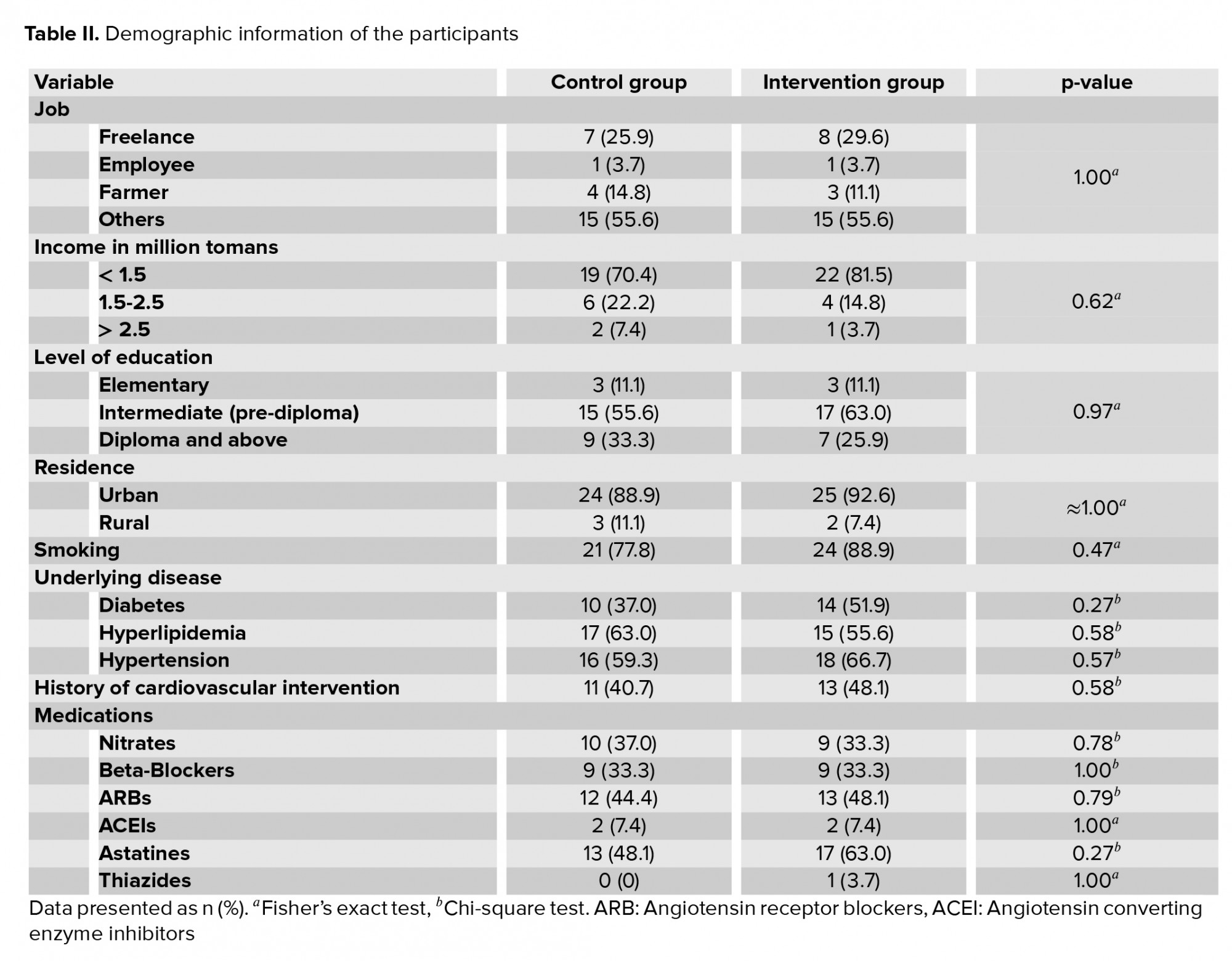
participants of the control and intervention groups were not significantly different in terms of the level of education, occupation, residence, smoking status, history of invasive interventions, underlying diseases (such as diabetes mellitus, hypertensions and hyperlipidemia), or drug classes of previous prescribed medications (Table II).
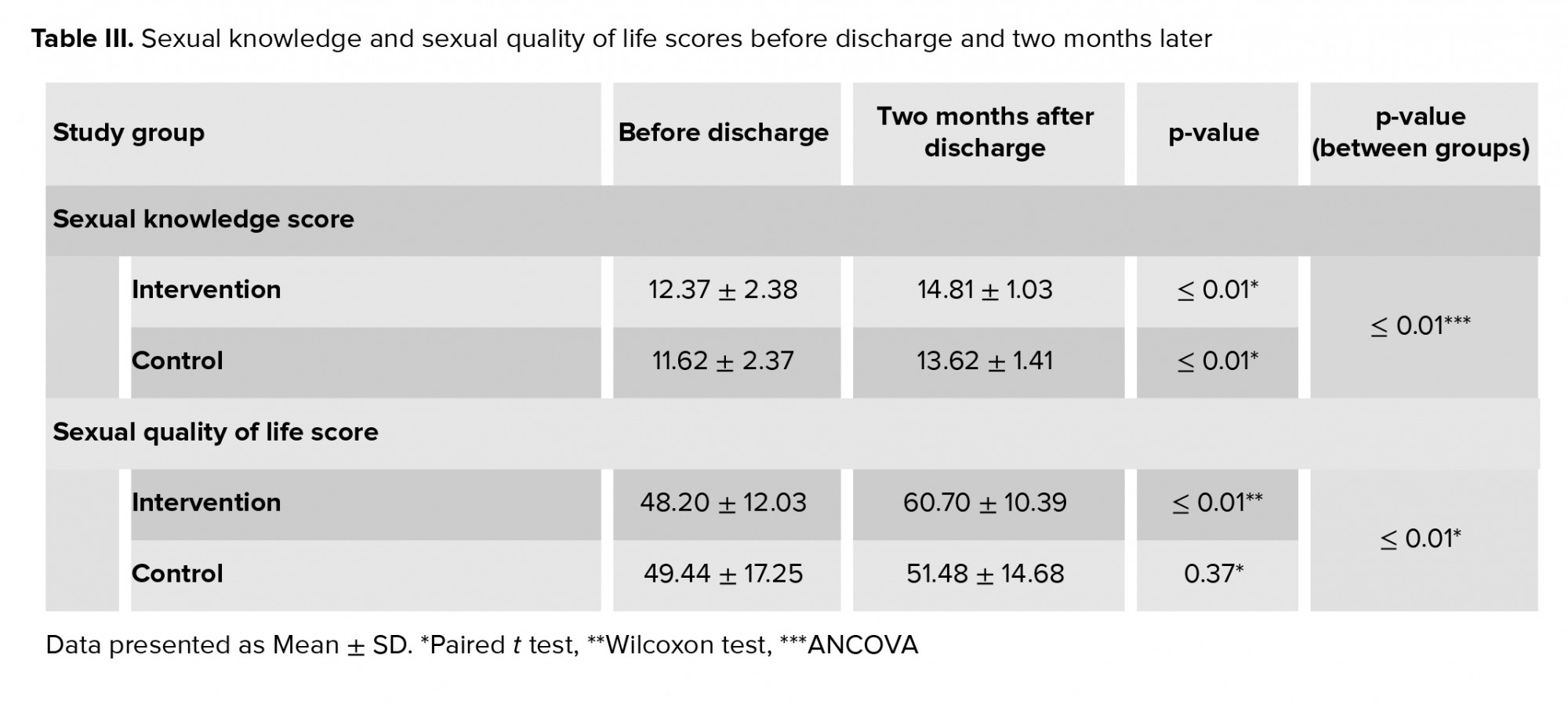
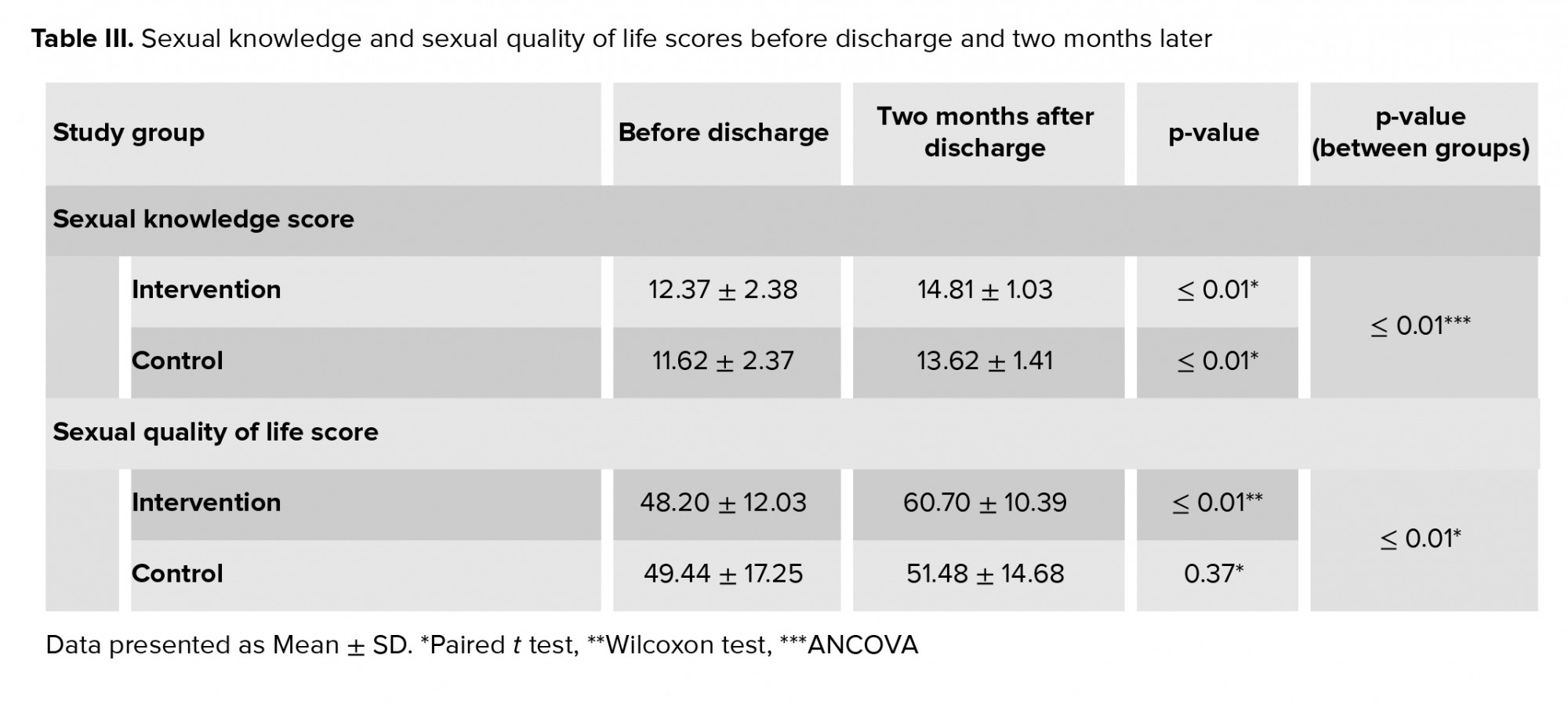
Covariance analysis was performed on the sexual knowledge score data. As demonstrated in table III, this analysis showed that sexual counseling seemed to affect the sexual knowledge scores (f = 11.13, p ≤ 0.01). The difference in sexual quality of life scores before and two months after counseling was measured and compared (Table III). This analysis showed that the sexual quality of life score was significantly related to the counseling (t = 2.98, p ≤ 0.01).
The depression scores two months after discharge were not normally distributed. The difference in depression scores before and two months after counseling was measured and compared (Table IV), which showed that depression was not affected by sexual counseling. Covariance analysis was also performed for the anxiety and stress data (Table IV). This analysis showed that sexual counseling affected anxiety scores (f = 7.018, p = 0.01) but there was no relationship between counseling and stress scores.

4. Discussion
In present study, the mean sexual knowledge score in the intervention group increased from 12.37 to 14.81 (Table III). A systematic review reported that in some cases, counseling improved sexual knowledge, performance, and satisfaction while in the other case, counseling did not make a difference (28). Several study showed that the sexual education of patients with cardiovascular diseases improved their sexual performance (12, 13, 29). Another study reported that most patients leave the hospital without their questions on sexual relationships being answered. Most patients in their study were willing to receive information on sexual activity after discharge, while 69% of them did not receive any sexual counseling before discharge (18).
In present study, the mean sexual quality of life score in the intervention group increased from 48.2 to 60.7 (Table III). Several studies showed that invasive cardiac interventions improved the quality of life score of patients with cardiovascular diseases within several months, though this increase was not significant (30) or the effect on the sexual quality of life was unclear in their study (31). We can infer that sexual satisfaction improvement required sexual counseling and rehabilitation in their study (9).
Studies reported up to 85% sexual dysfunction in patients undergoing invasive interventions (6). Sexual knowledge an important factor regarding the sexual quality of life after invasive cardiac interventions, i.e. some studies stated that poor sexual knowledge can highly affect sexual health, performance, satisfaction, and quality (4, 32). Inappropriate sexual knowledge and activity is one of the main causes of readmission within six months after discharge, which is partly caused by a lack of patient awareness of the appropriate approach to coitus after discharge (33).
Some researchers suggested initiating sexual counseling as soon as possible in the hospital before patient discharge (13), as was done in this study.
The results of this study indicated that mean anxiety scores in the intervention group decreased from 11.18 to 5.25 but while this change was significant, no significant difference was observed regarding the stress and depression scores (Table IV).
Fear was the main cause of reduced sexual satisfaction and improved knowledge significantly reduced fear (34). Sexual education and rehabilitation of men with cardiovascular diseases may reduce stress, anxiety, and depression (35). But, there are some controversies that sexual counseling reduced the sexual satisfaction due to increased fear and stress, since the counseling overemphasized the high risk of cardiac attack during coitus (15). These differences in findings may be attributed to the different content and presentation of the counseling sessions.
Studies demonstrated that organic factors such as erectile dysfunction only account for 15-20% of sexual dysfunction and the other cases are related to psychological factors such as stress and anxiety (5). Psychological factors may be resolved by increasing sexual knowledge, though for many reasons sexual issues are ignored in hospitals by the health care team (14). Psychological issues such as fear can significantly affect the sexual quality of life. Wives of many patients with cardiovascular disease are scared of the consequences of sexual activity which may lead to avoidance of sexual relationships and anger towards a patient’s health (36). Failure to reduce stress and depression may be due to counseling that is performed by an unreliable, inexperienced counsellor and social taboos of sexual issues; future studies are needed to investigate this. The reduced stress scores demonstrated in both groups (Table IV) may be related to the passage of time after a stressful procedure (percutaneous transluminal coronary angioplasty/CABG). We suggest that further studies evaluate stress over multiple short time periods of follow-up after consult (due to the rapid variability in stress with daily events and short-term stress responses to consultations). Also, we suggest longer follow-up studies are conducted with several sessions of counseling for evaluating depression.
5. Conclusion
Face-to-face sexual counseling combined with an educational video and booklet increased sexual knowledge and sexual quality of life and reduced patient anxiety scores in the intervention group compared with the control group, but stress and depression scores were not significantly changed. Thus, we recommend that cardiologists acquire sexual counseling skills to perform sexual counseling along with the standard medical treatment in the rehabilitation of patients. Further studies are needed to investigate the impact of counseling on stress and depression.
Acknowledgements
The authors appreciate the Vice-President of Research of Kashan University of Medical Sciences for funding the project, and the management of Shahid Beheshti Hospital and head nurse of the post catheterization department for their cooperation, as well as the participants who patiently participated in the study. This study was financially supported by Kashan University of Medical Sciences.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ischemic heart events occur more frequently in men than in women, and occur at younger ages and cause more complications. Sexual dysfunction is a common complication of cardiac events (experienced by over 93% of patients) which may lead to imbalances in the interpersonal relations and affect their quality of life (1, 2). Also, their medications may cause sexual dysfunction (3). Sexual dysfunction occurs in more than half of individuals undergoing open-heart surgery (4). Studies have indicated that 47–85% of patients, mostly men, experience sexual dysfunction after invasive coronary interventions (5-9), and in some cases these complications increase with angioplasty or coronary artery bypass graft (CABG) (10, 11).
Treatment of mental health issues may affect the sexual dysfunction (12). In this regard, education and improvement of couples’ relationships are among the therapeutic methods used. Additionally, providing education in the hospital is a key point (13). Some of the mental health issues (such as stress and anxiety) are caused by a lack of knowledge and information on appropriate sexual and intimate relationships and a lack of physician recommendations before discharge (14).
Studies have reported varied results on sexual counseling. Overemphasis on the increased risk of cardiac attack during coitus by the health care team in sexual counseling may cause sexual dysfunction (15). On the other hand, excessive reassurance may bring harmful consequences by leading to cardiac attacks and readmissions, which will highly affect future sexual relationships. Some counseling interventions improve sexual knowledge, performance, and satisfaction and early patient recovery to normal sexual activities after cardiac events (12) while some results demonstrate the opposite effect (15, 16).
Given the potential positive effects of sexual dysfunction treatment on improving the sexual quality of life, the early diagnosis and treatment of these complications is important (17).
Due to the low sexual quality of life of many cardiac patients (16), increased use of invasive interventions for cardiovascular diseases (10), widespread ignorance about patients’ sexual disorders (18), lack of knowledge and communication skills of health care staff surrounding sexual counseling (14), common concerns of men with cardiovascular disease about their sexual life (19), and lack of comprehensive guidance for sexual counseling of patients with cardiovascular diseases (20), this study was designed to assess the effect of sexual counseling before discharge on sexual knowledge, sexual quality of life, stress, anxiety, and depression in men that have undergone invasive coronary interventions. The results of this study could be used in the rehabilitation of men with cardiovascular diseases to improve their sexual quality of life.
2. Materials and Methods
This was a randomized controlled trial which involved 156 male participants who had undergone invasive coronary interventions (CABG or percutaneous transluminal coronary angioplasty) in the post catheterization department of Shahid Beheshti hospital (Kashan, Iran) from April to September 2018. A continuous sampling method was used. Participants were allocated to the intervention or control group randomly by random computer numbers (performed by the researcher using a calculator). As is convention, multiples of the number two placed the participants in the intervention group, and other numbers placed the participants in the control group.
The inclusion criteria were: married men (living with their wife), aged 35-65 yr, who had undergone invasive coronary interventions. The exclusion criteria were: heart, liver, pulmonary or kidney failure; malignancy; any systemic disease; use of antipsychotic or cytotoxic drugs; severe heart failure (function class III or IV (by New York Heart Association classification)); alcohol or opium abuse (reported by the participants); current depression, anxiety, or stress (based on a DASS-21 score of < 10 for depression, < 8 for anxiety or < 15 for stress); current known sexual dysfunction; or current known psychological disorder.
Details are shown in the consort diagram (Figure 1). Demographic information such as age, sex, level of education, history of cardiovascular interventions, occupation, underlying diseases, and medications were recorded, with a focus on confidentiality. Self-reported questionnaires were given to the participants. The questionnaires used were the DASS-21 depression, anxiety, and stress scale, Abraham’s Sexual Quality of Life scale (21), and a sexual knowledge scale (4).
Abraham’s Sexual Quality of Life Scale (for men) has been validated in Persian with a content validity index of 0.87 and a Cronbach’s alpha of 0.82 (21). This scale consists of 11 items, and each item can be rated 1 to 6 points (Likert scale); higher points indicate a higher quality of life. The sexual knowledge scale that was used is a 20-item scale for Men after invasive coronary interventions; its content validity and reliability were shown by Lai et al. (4). Participants were asked to answer questions about sexual knowledge as true or false. The correct answer scored a 1, whereas an incorrect answer was scored as 0. Total scores ranged from 0 to 20, with higher scores indicating greater sexual knowledge. This sexual knowledge scale (4) had a content validity index of 0.78 and a Cronbach’s alpha of 0.73. During translation into the Persian language, three questions (items 18-20) were eliminated as part of cultural adaptation. The reliability of the tool was rechecked and the new Cronbach’s alpha was 0.72 (22). The DASS-21 score validity and reliability have already been demonstrated (23).
The questionnaires were completed twice: before discharge and again two months after discharge (to record prolonged changes). For illiterate participants, the researchers wrote down their exact words.
After completing the first questionnaire, participants in the intervention group received sexual counseling along with routine advice, while participants in the control group underwent routine discharge procedures (at a similar meeting, they received the usual health advice). In the intervention group, patients were counseled for 20 min by the researcher and then they were given a booklet and DVD with additional information adapted from authoritative cardiovascular references (24-27) approved by cardiologists and cardiac nurses (Table I). We tried not to let the groups know about each other's training program. The face-to-face counseling session discussed the information in the booklet and participants’ questions were clearly answered. The counseling took place before discharge to reduce bias due to participants’ interactions.
After discharge, the researcher communicated with the participants several times through telephone calls and virtual networks (e.g. WhatsApp) to ensure the participants used the booklet and DVD. Also, participants could ask the researcher any questions. After two months, the same questionnaires were completed again (by telephone call or in-person session).
2.1. Ethical considerations
The study was approved by the Kashan University of Medical Science Research Ethics Committee (Code: IR.KAUMS.MEDNT.REC.1396.97). Informed consent was taken before the intervention and confidentiality was prioritized. Participants were consulted alone to maintain confidentiality and collected data were kept anonymous. Participants could withdraw from the study at any time. In accordance with participants’ rights, participants in the control group received a 20- to 30-minute sexual counseling session by telephone after filling out the questionnaires for the second time.
2.2. Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS, version 16, IBM Company), by Chi-square, t test, paired t test, Leven test, Fisher’s exact test, Kolmogorov-Simonov, Wilcoxon, and ANCOVA. A significance level of p < 0.05 was used.
3. Results
Of the 156 participants initially deemed eligible, 85 did not meet the inclusion criteria. Also 11 participants were excluded due to mental health conditions or sexual dysfunction and four participants did not consent to participate in the study. Two participants could not be contacted for the two-month follow-up (one in the intervention group and one in the control group). Finally, 54 participants remained in the study.
participants of the control and intervention groups were not significantly different in terms of the level of education, occupation, residence, smoking status, history of invasive interventions, underlying diseases (such as diabetes mellitus, hypertensions and hyperlipidemia), or drug classes of previous prescribed medications (Table II).
Covariance analysis was performed on the sexual knowledge score data. As demonstrated in table III, this analysis showed that sexual counseling seemed to affect the sexual knowledge scores (f = 11.13, p ≤ 0.01). The difference in sexual quality of life scores before and two months after counseling was measured and compared (Table III). This analysis showed that the sexual quality of life score was significantly related to the counseling (t = 2.98, p ≤ 0.01).
The depression scores two months after discharge were not normally distributed. The difference in depression scores before and two months after counseling was measured and compared (Table IV), which showed that depression was not affected by sexual counseling. Covariance analysis was also performed for the anxiety and stress data (Table IV). This analysis showed that sexual counseling affected anxiety scores (f = 7.018, p = 0.01) but there was no relationship between counseling and stress scores.

4. Discussion
In present study, the mean sexual knowledge score in the intervention group increased from 12.37 to 14.81 (Table III). A systematic review reported that in some cases, counseling improved sexual knowledge, performance, and satisfaction while in the other case, counseling did not make a difference (28). Several study showed that the sexual education of patients with cardiovascular diseases improved their sexual performance (12, 13, 29). Another study reported that most patients leave the hospital without their questions on sexual relationships being answered. Most patients in their study were willing to receive information on sexual activity after discharge, while 69% of them did not receive any sexual counseling before discharge (18).
In present study, the mean sexual quality of life score in the intervention group increased from 48.2 to 60.7 (Table III). Several studies showed that invasive cardiac interventions improved the quality of life score of patients with cardiovascular diseases within several months, though this increase was not significant (30) or the effect on the sexual quality of life was unclear in their study (31). We can infer that sexual satisfaction improvement required sexual counseling and rehabilitation in their study (9).
Studies reported up to 85% sexual dysfunction in patients undergoing invasive interventions (6). Sexual knowledge an important factor regarding the sexual quality of life after invasive cardiac interventions, i.e. some studies stated that poor sexual knowledge can highly affect sexual health, performance, satisfaction, and quality (4, 32). Inappropriate sexual knowledge and activity is one of the main causes of readmission within six months after discharge, which is partly caused by a lack of patient awareness of the appropriate approach to coitus after discharge (33).
Some researchers suggested initiating sexual counseling as soon as possible in the hospital before patient discharge (13), as was done in this study.
The results of this study indicated that mean anxiety scores in the intervention group decreased from 11.18 to 5.25 but while this change was significant, no significant difference was observed regarding the stress and depression scores (Table IV).
Fear was the main cause of reduced sexual satisfaction and improved knowledge significantly reduced fear (34). Sexual education and rehabilitation of men with cardiovascular diseases may reduce stress, anxiety, and depression (35). But, there are some controversies that sexual counseling reduced the sexual satisfaction due to increased fear and stress, since the counseling overemphasized the high risk of cardiac attack during coitus (15). These differences in findings may be attributed to the different content and presentation of the counseling sessions.
Studies demonstrated that organic factors such as erectile dysfunction only account for 15-20% of sexual dysfunction and the other cases are related to psychological factors such as stress and anxiety (5). Psychological factors may be resolved by increasing sexual knowledge, though for many reasons sexual issues are ignored in hospitals by the health care team (14). Psychological issues such as fear can significantly affect the sexual quality of life. Wives of many patients with cardiovascular disease are scared of the consequences of sexual activity which may lead to avoidance of sexual relationships and anger towards a patient’s health (36). Failure to reduce stress and depression may be due to counseling that is performed by an unreliable, inexperienced counsellor and social taboos of sexual issues; future studies are needed to investigate this. The reduced stress scores demonstrated in both groups (Table IV) may be related to the passage of time after a stressful procedure (percutaneous transluminal coronary angioplasty/CABG). We suggest that further studies evaluate stress over multiple short time periods of follow-up after consult (due to the rapid variability in stress with daily events and short-term stress responses to consultations). Also, we suggest longer follow-up studies are conducted with several sessions of counseling for evaluating depression.
5. Conclusion
Face-to-face sexual counseling combined with an educational video and booklet increased sexual knowledge and sexual quality of life and reduced patient anxiety scores in the intervention group compared with the control group, but stress and depression scores were not significantly changed. Thus, we recommend that cardiologists acquire sexual counseling skills to perform sexual counseling along with the standard medical treatment in the rehabilitation of patients. Further studies are needed to investigate the impact of counseling on stress and depression.
Acknowledgements
The authors appreciate the Vice-President of Research of Kashan University of Medical Sciences for funding the project, and the management of Shahid Beheshti Hospital and head nurse of the post catheterization department for their cooperation, as well as the participants who patiently participated in the study. This study was financially supported by Kashan University of Medical Sciences.
Conflict of Interest
The authors declare that they have no conflict of interest.
Type of Study: Original Article |
Subject:
Reproductive Psycology
References
1. Arenhall E, Eriksson M, Nilsson U, Steinke EE, Fridlund B. Decreased sexual function in partners after patients' first-time myocardial infarction. Eur J Cardiovasc Nurs 2018; 17: 521-526. [DOI:10.1177/1474515117751904] [PMID]
2. Rusiecki L, Zdrojowy R, Gebala J, Rabijewski M, Sobieszczańska M, Smoliński R, et al. Sexual health in Polish elderly men with coronary artery disease: Importance, expectations, and reality. Asian J Androl 2020; 22: 526-531. [DOI:10.4103/aja.aja_131_19] [PMID] [PMCID]
3. Roushias S, Ossei-Gerning N. Sexual function and cardiovascular disease: What the general cardiologist needs to know. Heart 2019; 105: 160-168. [DOI:10.1136/heartjnl-2016-310762] [PMID]
4. Lai YH, Hsieh SR, Ho WC, Chiou AF. Factors associated with sexual quality of life in patients before and after coronary artery bypass grafting surgery. J Cardiovasc Nurs 2011; 26: 487-496. [DOI:10.1097/JCN.0b013e3182050269] [PMID]
5. Schumann J, Zellweger MJ, Di Valentino M, Piazzalonga S, Hoffmann A. Sexual dysfunction before and after cardiac rehabilitation. Rehabil Res Pract 2010; 2010: 823060. [DOI:10.1155/2010/823060] [PMID] [PMCID]
6. Pournaghash Tehrani S, Etemadi S, Dehdari T, Lavasani MG, Sadeghian S. [Assessment of the relationship between psychological factors and impotency with quality of life of male patients following CABG]. Razi J Med Sci 2013; 19: 34-42. (in Persian)
7. Murphy PJ, Noone C, D'Eath M, Casey D, Doherty S, Jaarsma T, et al. The CHARMS pilot study: A multi-method assessment of the feasibility of a sexual counselling implementation intervention in cardiac rehabilitation in Ireland. Pilot Feasibil Stud 2018; 4: 88. [DOI:10.1186/s40814-018-0278-4] [PMID] [PMCID]
8. Khodaminasab A, Reisi M, Vahedparast H, Tahmasebi R, Javadzade H. Utilizing a health-promotion model to predict self-care adherence in patients undergoing coronary angioplasty in Bushehr, iran. Patient Prefer Adherence 2019; 13: 409-417. [DOI:10.2147/PPA.S181755] [PMID] [PMCID]
9. Palm P, Zwisler ADO, Svendsen JH, Thygesen LC, Giraldi A, Jensen KG, et al. Sexual rehabilitation for cardiac patients with erectile dysfunction: A randomised clinical trial. Heart 2019; 105: 775-782. [DOI:10.1136/heartjnl-2018-313778] [PMID]
10. Rahimi A, Taghipour H, Ebadi A, Pourebrahimi M. [Sexual function of male patients before and after coronary artery bypass graft surgery]. Iran J Rehabil Res 2019; 5: 41-46.(in Persian)
11. Saleem M, Adeeb M, Durrani AK, Siddique AR. Sexual desire and marital satisfaction among coronary angioplasty patients-pre and post design. Pak Heart J 2019; 52: 31-35.
12. Doulatyari PK, Gholami M, Toulabi T, Birjandi M, Abdi A. The effect of modified cardiac rehabilitation on erectile dysfunction and coping with stress in men undergoing coronary artery bypass graft (CABG): A clinical trial. Sexual Disabil 2019; 37: 455-469. [DOI:10.1007/s11195-019-09578-3]
13. Haji Mohammad Hoseini M, Ghanbari Afra L, Asayesh H, Goudarzi M, Ghanbari Afra M. The effect of self-care educational program on sexual function and quality of life in patients with ischemic heart disease. J Res Med Dental Sci 2018; 6: 226-235.
14. Blakey EP, Aveyard H. Student nurses' competence in sexual health care: A literature review. J Clin Nurs 2017; 26: 3906-3916. [DOI:10.1111/jocn.13810] [PMID]
15. Sarhadi M, Navidian A, Fasihi Harandy T, Ansari Moghadam A. [Comparing quality of marital relationship of spouses of patients with and without a history of myocardial infarction]. J Health Promot Manage 2013; 2: 39-48. (in Persian)
16. Boothby CA, Dada BR, Rabi DM, Campbell TS, Tang KL. The effect of cardiac rehabilitation attendance on sexual activity outcomes in cardiovascular disease patients: A systematic review. Can J Cardiol 2018; 34: 1590-1599. [DOI:10.1016/j.cjca.2018.08.020] [PMID]
17. Miri A, Ghanbari MA, Najafi A. [The relationship between health literacy and the recovery rate of cardiovascular patients after bypass surgery]. J Health Literacy 2016; 1: 83-91. (in Persian)
18. Lunelli RP, Rabello ER, Stein R, Goldmeier S, Moraes MA. Sexual activity after myocardial infarction: Taboo or lack of knowledge? Arq Bras Cardiol 2008; 90: 156-159. [DOI:10.1590/S0066-782X2008000300003] [PMID]
19. Maheu-Cadotte MA, Fontaine G, Duchaine C, Durel N, Roussy C, Mailhot T. Assessing and addressing sexual concerns in individuals diagnosed with coronary artery disease. Br J Cardiac Nurs 2019; 14: 1-10. [DOI:10.12968/bjca.2019.0008]
20. Lamyian M, Zarei F, Montazeri A, Hajizadeh E, Maasoumi R. [Exploring the factors affecting Iranian women's quality of sexual life]. Hayat 2016; 22: 185-200. (in Persian)
21. Sadat Z, Ghofranipour F, Goshtasebi A, Azin SA. [Validity and relibility of the Persian version of the sexual quality of life-male questionnaire]. Payesh 2017; 16: 73-80. (in Persian)
22. Taqizade Firoozjaei I, Taghadosi M, Sadat Z. Determining the sexual quality of life and related factors in patients referred to the department of cardiac rehabilitation: A cross-sectional study. Int J Reprod Biomed 2021; 19: 261-270. [DOI:10.18502/ijrm.v19i3.8574] [PMID] [PMCID]
23. Samani S, Joukar B. A study on the reliability and validity of the short form of the depression anxiety stress scale (Dass-21). J Soc Sci Human 2007; 26: 65-77.
24. Hoeman SP. Rehabilitation nursing: Prevention, intervention, and outcomes.4th Ed. USA: Mosby Co.; 2008.
25. Moser DK, Riegel B. Cardiac Nursing: A companion to braunwald's heart disease. Philadelphia, USA: Saunders; 2008.
26. Woods SL, Froelicher ESS, Bridges EJ. Cardiac nursing. Philadelphia, USA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010.
27. Steinke EE, Jaarsma T. Sexual counseling and cardiovascular disease: Practical approaches. Asian J Androl 2015; 17: 32-39. [DOI:10.4103/1008-682X.135982] [PMID] [PMCID]
28. Byrne M, Doherty S, Fridlund BG, Mårtensson J, Steinke EE, Jaarsma T, et al. Sexual counselling for sexual problems in patients with cardiovascular disease. Cochrane Database Syst Rev 2016; 2: CD010988. [DOI:10.1002/14651858.CD010988.pub2] [PMID] [PMCID]
29. Rakhshan M, Toufigh A, Dehghani A, Yaktatalab S. Effect of cardiac rehabilitation on sexual satisfaction among patients after coronary artery bypass graft surgery. J Cardiopulmonar Rehabil Prevent 2019; 39: E26-E30. [DOI:10.1097/HCR.0000000000000434] [PMID]
30. Li R, Yan BP, Dong M, Zhang Q, Yip GWK, Chan CP, et al. Quality of life after percutaneous coronary intervention in the elderly with acute coronary syndrome. Int J Cardiol 2012; 155: 90-96. [DOI:10.1016/j.ijcard.2010.09.050] [PMID]
31. Rahnama Z, Taghadosi M, Mazochi M. Comparison of quality of life before and after the therapeutic interventions in patients with acute coronary syndrome. Feyz 2014; 18: 440-447.
32. Abu Bdair IA, Abushaikha L. Jordanian patients knowledge regarding sexual health following coronary artery diseases. Int J Healthcare Med Sci 2018; 4: 90-98.
33. Arenhall E, Kristofferzon ML, Fridlund B, Malm D, Nilsson U. The male partners' experiences of the intimate relationships after a first myocardial infarction. Eur J Cardiovasc Nurs 2011; 10: 108-114. [DOI:10.1016/j.ejcnurse.2010.05.003] [PMID]
34. Soroush A, Komasi S, Heydarpour B, Ezzati P, Saeidi M. The effectiveness of psychosexual education program on psychological dimensions of sexual function and its quality in cardiac rehabilitation patients. Res Cardiovasc Med 2018; 7: 82-86. [DOI:10.4103/rcm.rcm_5_17]
35. Tirgari B, Rafati F, Mehdipour Rabori R. Effect of sexual rehabilitation program on anxiety, stress, depression and sexual function among men with coronary artery disease. J Sex Marital Ther 2019; 45: 632-642. [DOI:10.1080/0092623X.2019.1599091] [PMID]
36. Pouraboli B, Azizzadeh F, Mohammad A. [Knowledge and attitudes of nurses in sexual activity and educate it to patients with myocardial infarction and their spouses]. Iran J Crit Care Nurs 2010; 2: 5-6. (in Persian)
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








