Thu, Feb 19, 2026
[Archive]
Volume 20, Issue 5 (May 2022)
IJRM 2022, 20(5): 405-412 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alipour M R, Moradi H, Namayandeh S M, Majidpour F, Pezeskpour Z, Sarebanhassanabadi M. Abnormal findings in fetal echocardiography and maternal disease: A cross-sectional study. IJRM 2022; 20 (5) :405-412
URL: http://ijrm.ir/article-1-2049-en.html
URL: http://ijrm.ir/article-1-2049-en.html
Mohammad Reza Alipour1 

 , Hossein Moradi2
, Hossein Moradi2 

 , Seyedeh Mahdieh Namayandeh3
, Seyedeh Mahdieh Namayandeh3 

 , Fatemeh Majidpour3
, Fatemeh Majidpour3 

 , Zohreh Pezeskpour *4
, Zohreh Pezeskpour *4 

 , Mohammadtaghi Sarebanhassanabadi3
, Mohammadtaghi Sarebanhassanabadi3 




 , Hossein Moradi2
, Hossein Moradi2 

 , Seyedeh Mahdieh Namayandeh3
, Seyedeh Mahdieh Namayandeh3 

 , Fatemeh Majidpour3
, Fatemeh Majidpour3 

 , Zohreh Pezeskpour *4
, Zohreh Pezeskpour *4 

 , Mohammadtaghi Sarebanhassanabadi3
, Mohammadtaghi Sarebanhassanabadi3 


1- Assistant Professor in Pediatric Cardiology, Yazd Cardiovascular Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2- Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Yazd Cardiovascular Research Center, Non-communicable Diseases Research Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Research and Clinical Center Infertility, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,dr.zpezeshkpour@gmail.com
2- Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Yazd Cardiovascular Research Center, Non-communicable Diseases Research Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Research and Clinical Center Infertility, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Full-Text [PDF 366 kb]
(1346 Downloads)
| Abstract (HTML) (2128 Views)
1. Introduction
Congenital heart disease (CHD) is usually triggered by an abnormal development in the fetal heart structure in early embryonic stage (1). Some abnormalities may occur when the heart splits into 4 chambers and the valves form. Conotruncal disorders or valvular formation anomalies occur during these stages. These defects do not trigger prenatal or dynamic problems (2). Congenital vascular malformations are the most common group of birth defects and affect about 6-8 per thousand newborns (3). According to the previous studies, the prevalence of CHD is 6 times higher than chromosomal abnormalities and 4 times higher than neural tube defects. There are several risk factors involved in these diseases, which are generally divided into 2 categories maternal and fetal (4). In most cases, the cause is unknown; some are genetic, and some are environmental (5). Although in most cases they are multifactorial, several are also associated with chromosomal abnormalities, congenital defects, teratogens, or maternal metabolic disease. The range of lesions varies from asymptomatic to fatal anomalies (6).
Due to the high prevalence of congenital heart defects, fetal echocardiography is an important part of screening during pregnancy to diagnose fetal heart defects and arrhythmias (7). Fetal echocardiography has high sensitivity and specificity in diagnosing CHD in low- and high-risk populations (8). Fetal echocardiography is considered a standard part of pregnancy services (9). Techniques such as fetal heart magnetic resonance imaging and electrocardiogram are performed in only a few facilities due to their high cost and difficulty of access and are used only in research protocols. Fetal cardiac magnetic resonance imaging and fetal electrocardiography alternatives are acceptable procedures in diagnosing fetal atrial and ventricular arrhythmias (10). Although in fetal echocardiography, it is impossible to calculate details such as the p-wave axis or the width of QRS and QTC interval, the type of arrhythmia can only be identified based on changes in Doppler waves (11).
Moreover, in several other cases, such as fetal tachyarrhythmias, it is possible to prevent or treat heart failure by drugs prescribed to the mother. Another application of echocardiography in the treatment of non-autoimmune hydrops associated with fetal heart failure is performed by prescribing high-dose digoxin to the pregnant mother and monthly follow-up (4). Also, with early diagnosis of these diseases, fetal heart interventions can be used to treat these defects. One of the most successful of these interventions is transplacental drug therapy to treat fetal tachyarrhythmias (7).
Therefore, this study aimed to assess abnormal findings observed in fetal heart based on echocardiography and maternal disease.
2. Materials and Methods
This cross-sectional study was performed on 114 pregnant women referring to Afshar hospital, Yazd, Iran, from October 2016 and March 2017. Our inclusion criteria were pregnant women with a gestational age of 12 wk referred by gynecologists or radiologists for fetal echocardiography based on the international society of ultrasound in obstetrics and gynecology. All women in the first trimester of pregnancy, having a pregnancy with intrauterine fetal death, threatened with abortion fetuses, and incomplete abortion were excluded.
We intend to initially evaluate the diagnostic value of fetal echocardiography for early diagnosis of congenital diseases and also regarding the fact that some of these diseases are hard to cure. Although the standard time for fetal echocardiography to diagnose cardiac anomalies was before 19 wk of gestation, since several mothers were referred to evaluate diseases that could be medically intervened at any time (including fetal arrhythmia and heart failure), therefore, the referrals that after 19 wk of gestation were also included in the study. A pediatric cardiologist performed all echocardiography to prevent information bias. Participants' information including maternal age, gestational age, number of fetuses, underlying maternal disease, history of drug use or addiction in the mother, family history of CHD, history of infertility or use of assisted reproductive techniques, history of infectious diseases in the mother such as rubella, referral indication as well as final diagnosis after accurate fetal echocardiography was recorded. Echocardiography was performed by Color Doppler Echocardiograph, the Vivid 3 expert model (GE Healthcare, made in the USA), version 2011, and transducer containing crystal sets for 2-dimensional image (3.5 MHz with second harmonic technology). Also, follow-up echocardiography was done during 1st wk after birth for matching pre and post-natal diagnosis.
2.1. Ethical considerations
The Ethical Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran was approved the study proposal (Code: IR.SSU.MEDICINE.REC.1397.149). The oral consent was obtained from all participants.
2.1. Statistical analysis
The qualitative variables were reported as frequency and percentage. Data were analyzed by SPSS19 (IBM Corporation, New York, USA).
3. Results
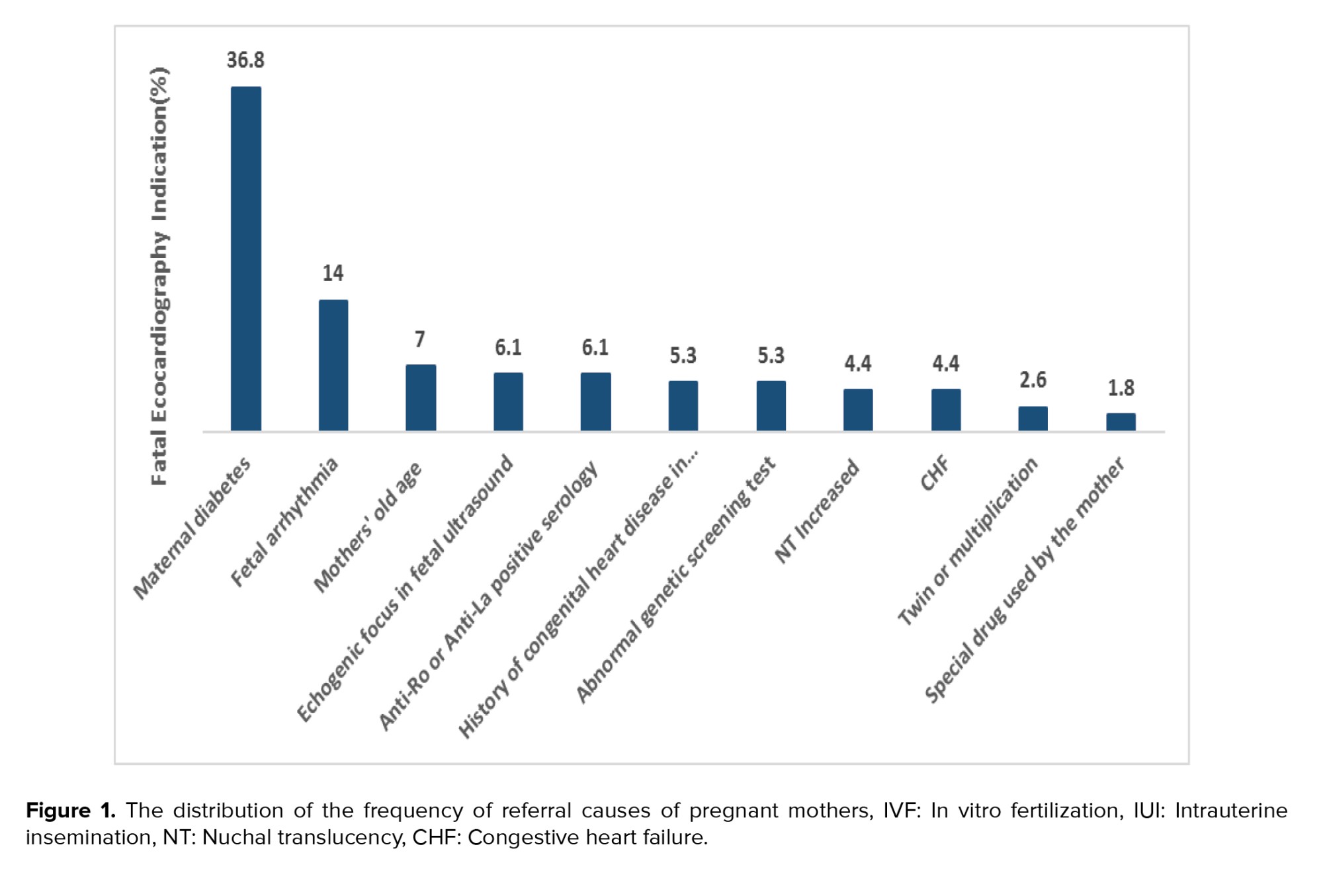
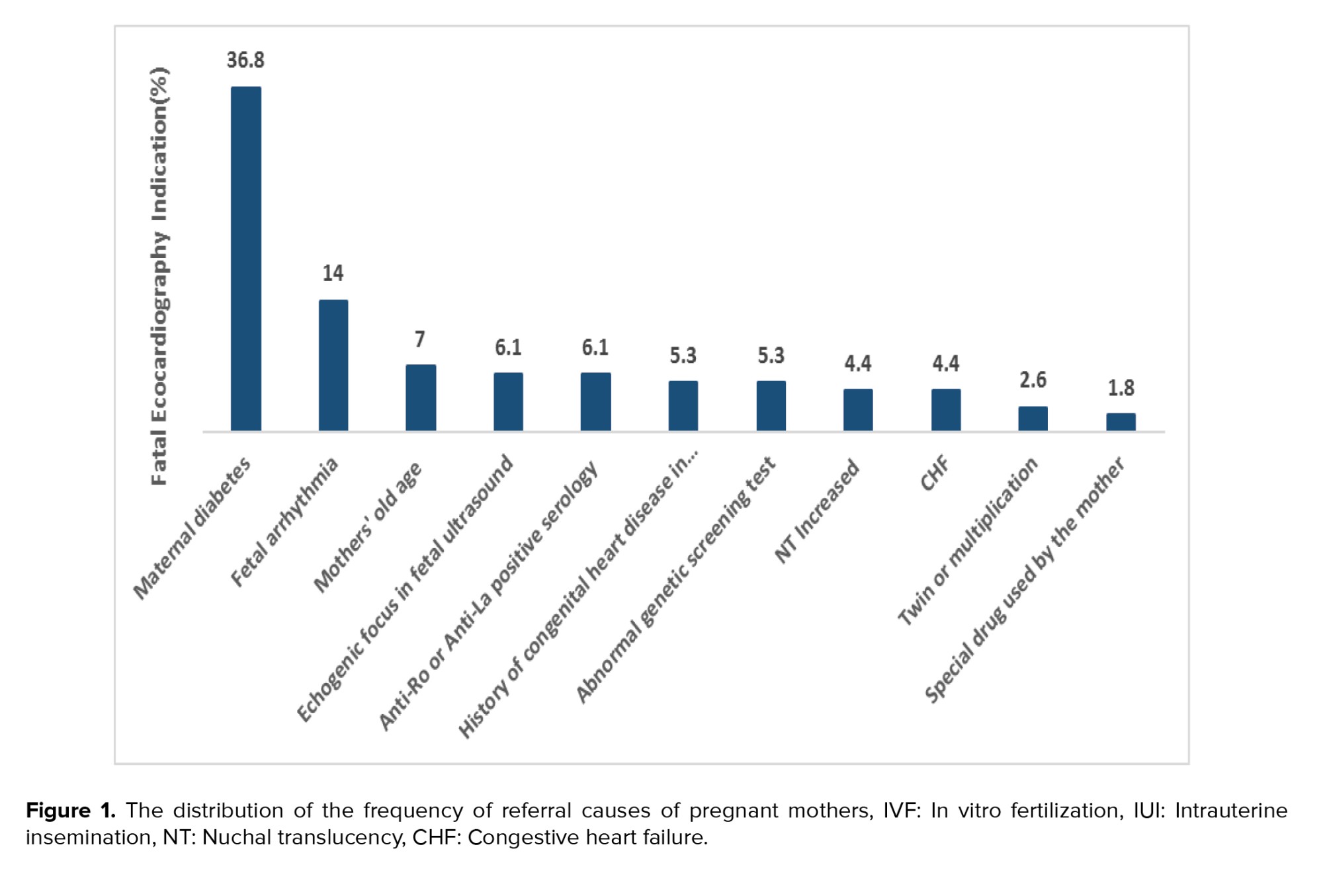
A total of 114 pregnant women who underwent complete echocardiography and follow-up were included. The mean age of the pregnant women and their mean gestational age were 27 yr and 20 wk, respectively. The most common reason was diabetes (36.8%). While, 14% (n = 16) of referrals were due to fetal arrhythmia [Premature atrial complex (n = 6), bradyarrhythmia (n = 4), tachyarrhythmia (n = 3), and complete heart block (n = 3)]. The results of fetal echocardiography revealed that 68.4% (n = 78) were normal, 17.6% (n = 20) had cardiac anomalies, and 14% (n = 16) had arrhythmia (Figure 1).
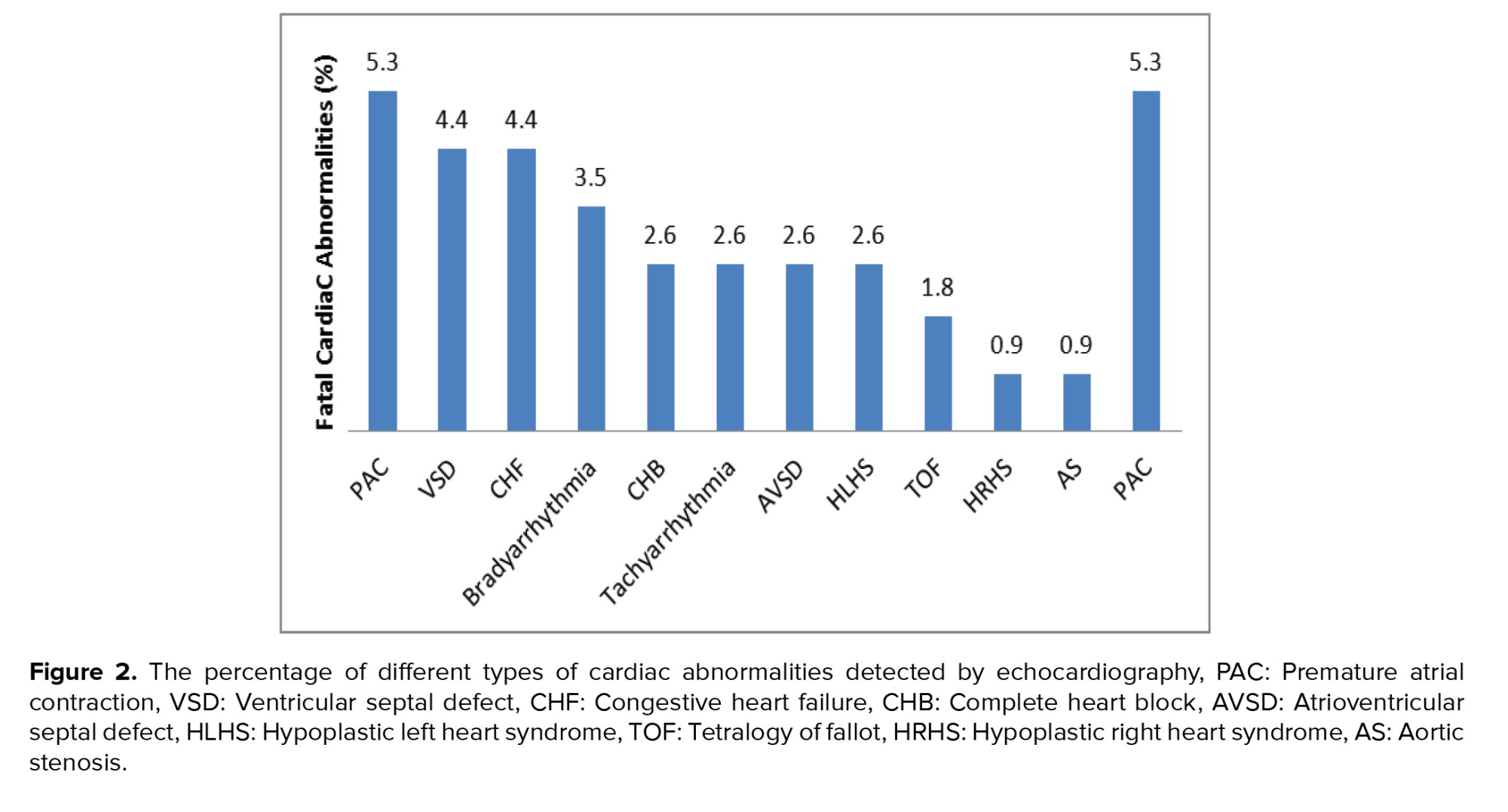
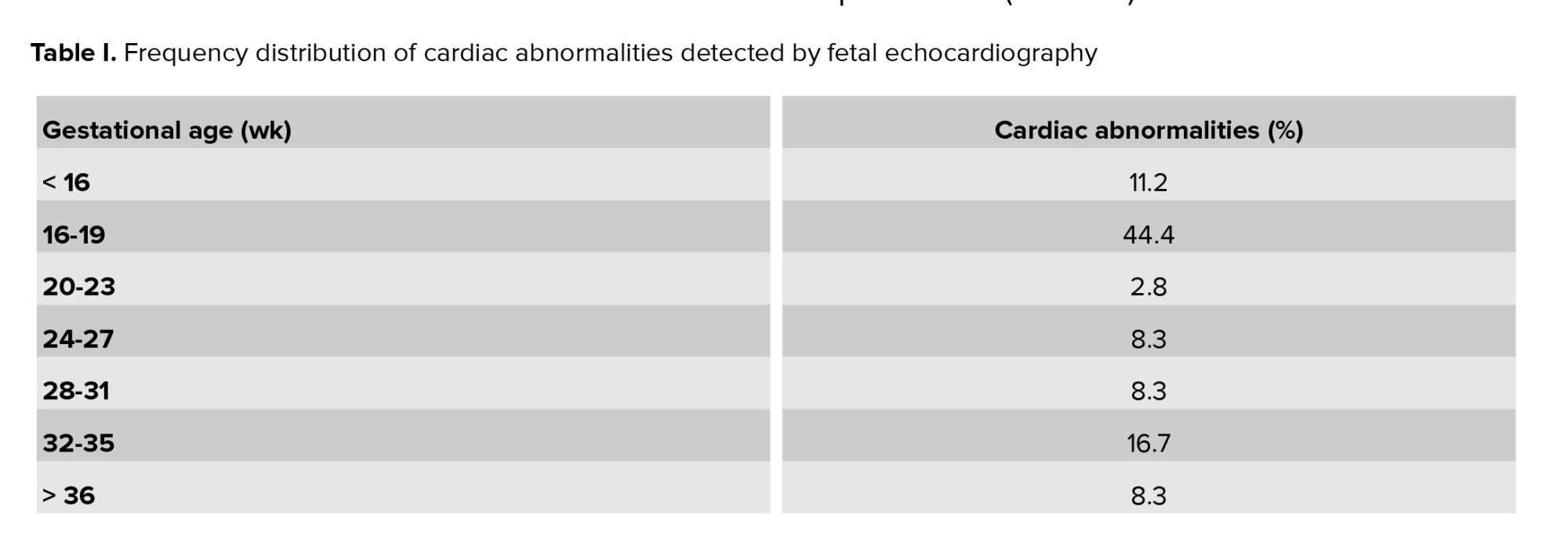
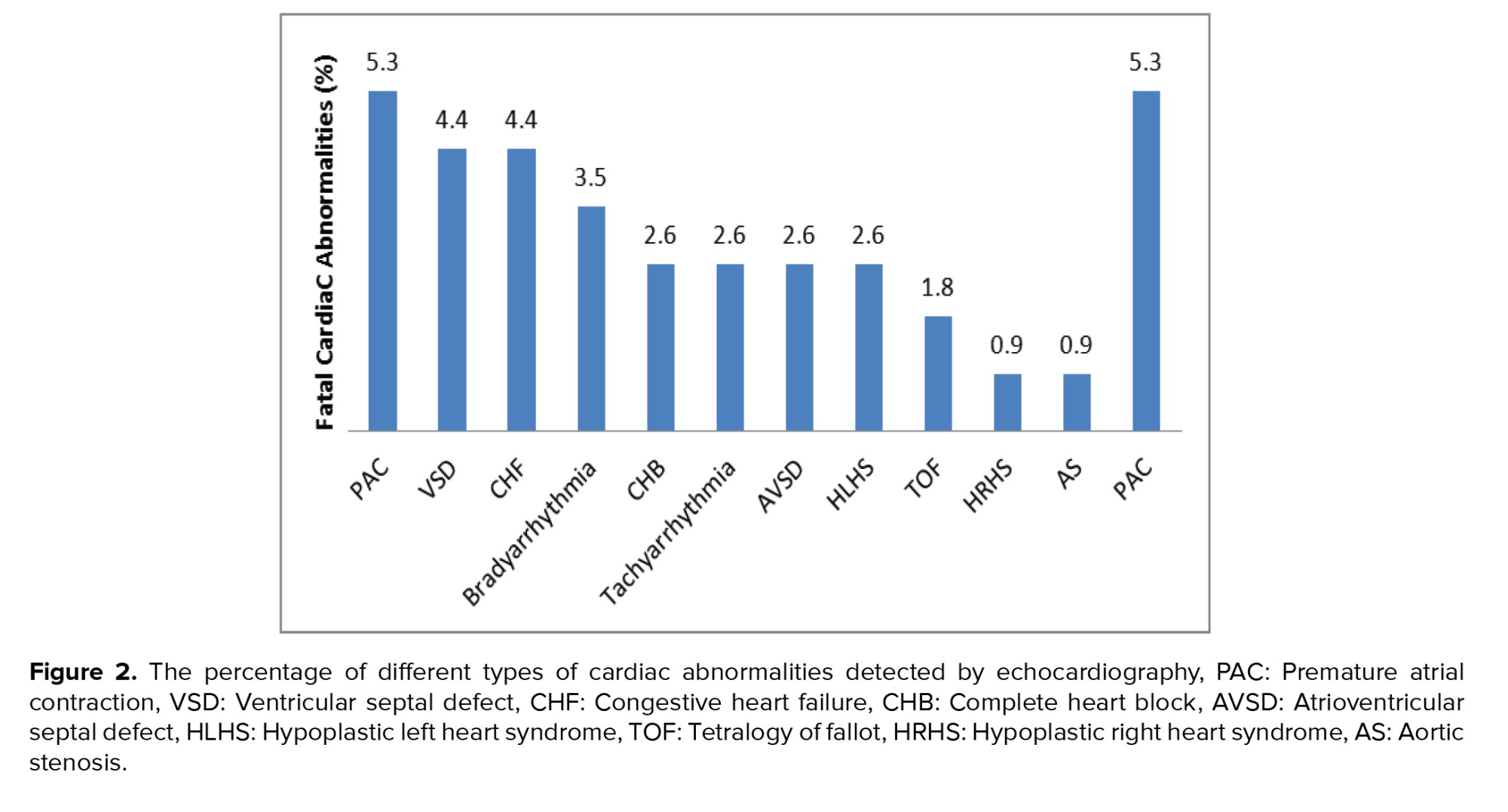
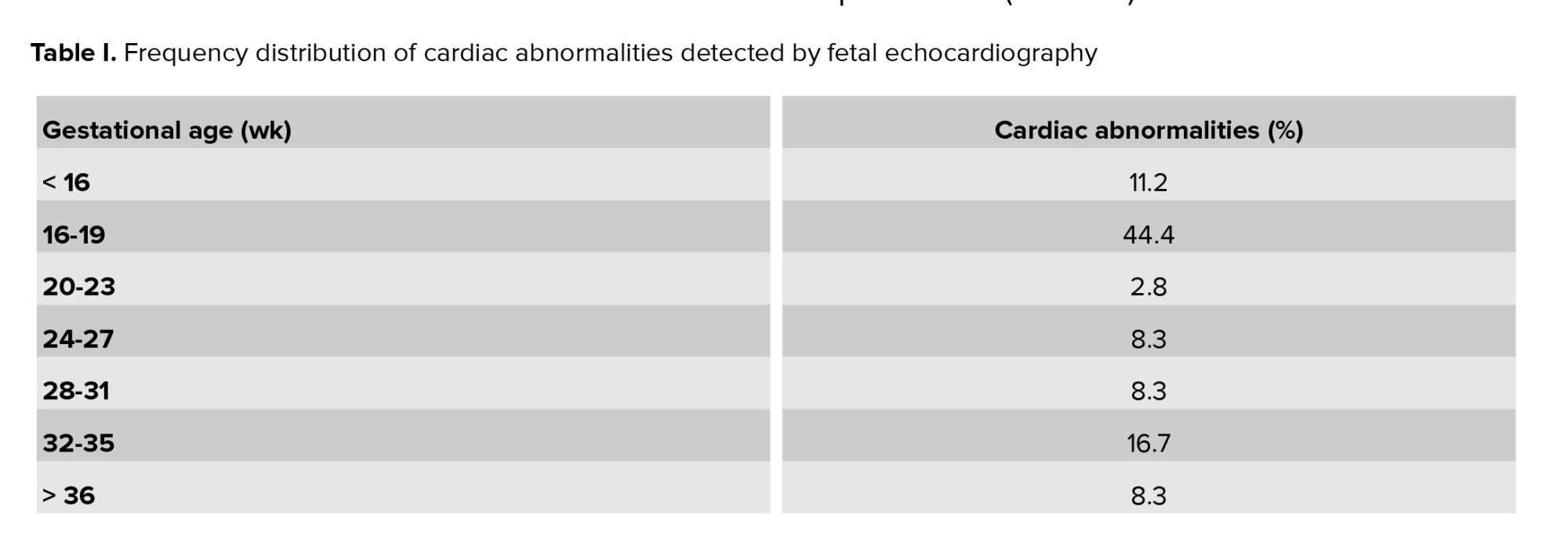
Figure 2 shows the percentage of different types of cardiac abnormalities detected by echocardiography. The distribution of the frequency percentage of cardiac abnormalities detected by fetal echocardiography in each gestational age interval is reported in the table I, the highest rate found in 16-19 wk of pregnancy (44.4%).
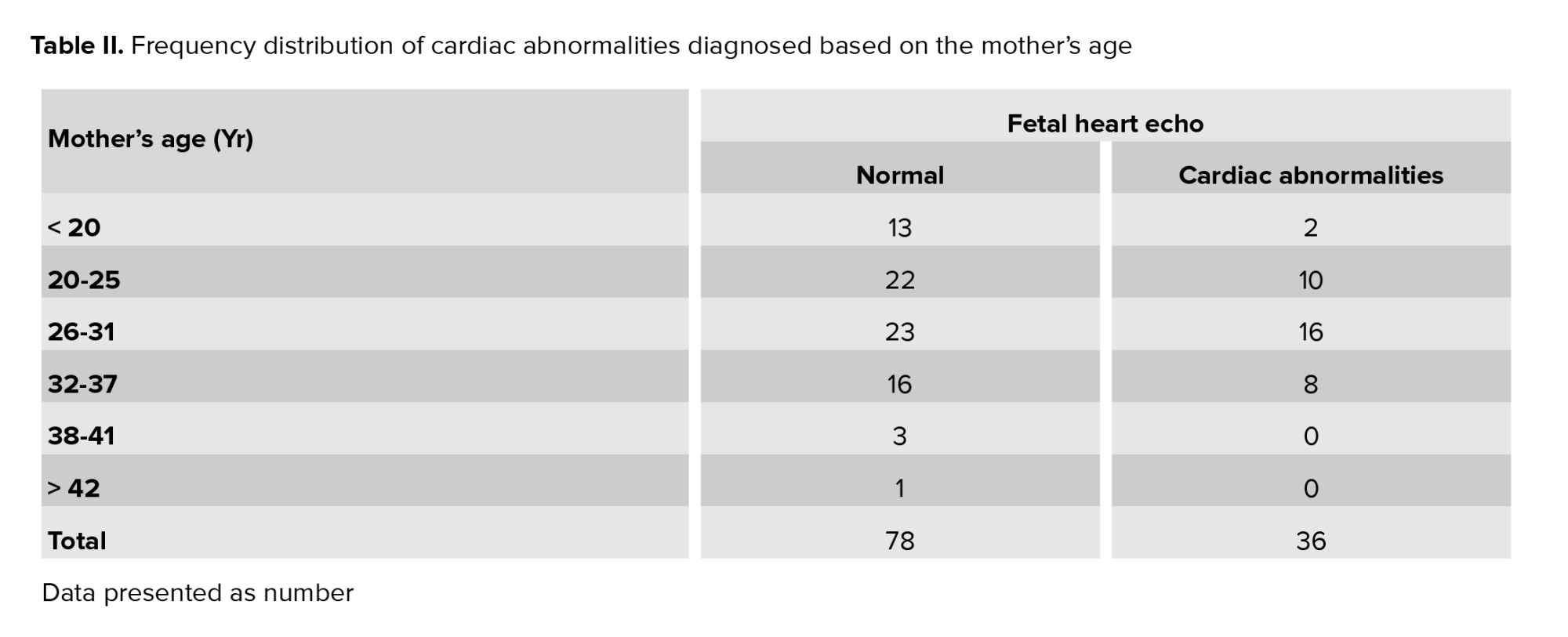
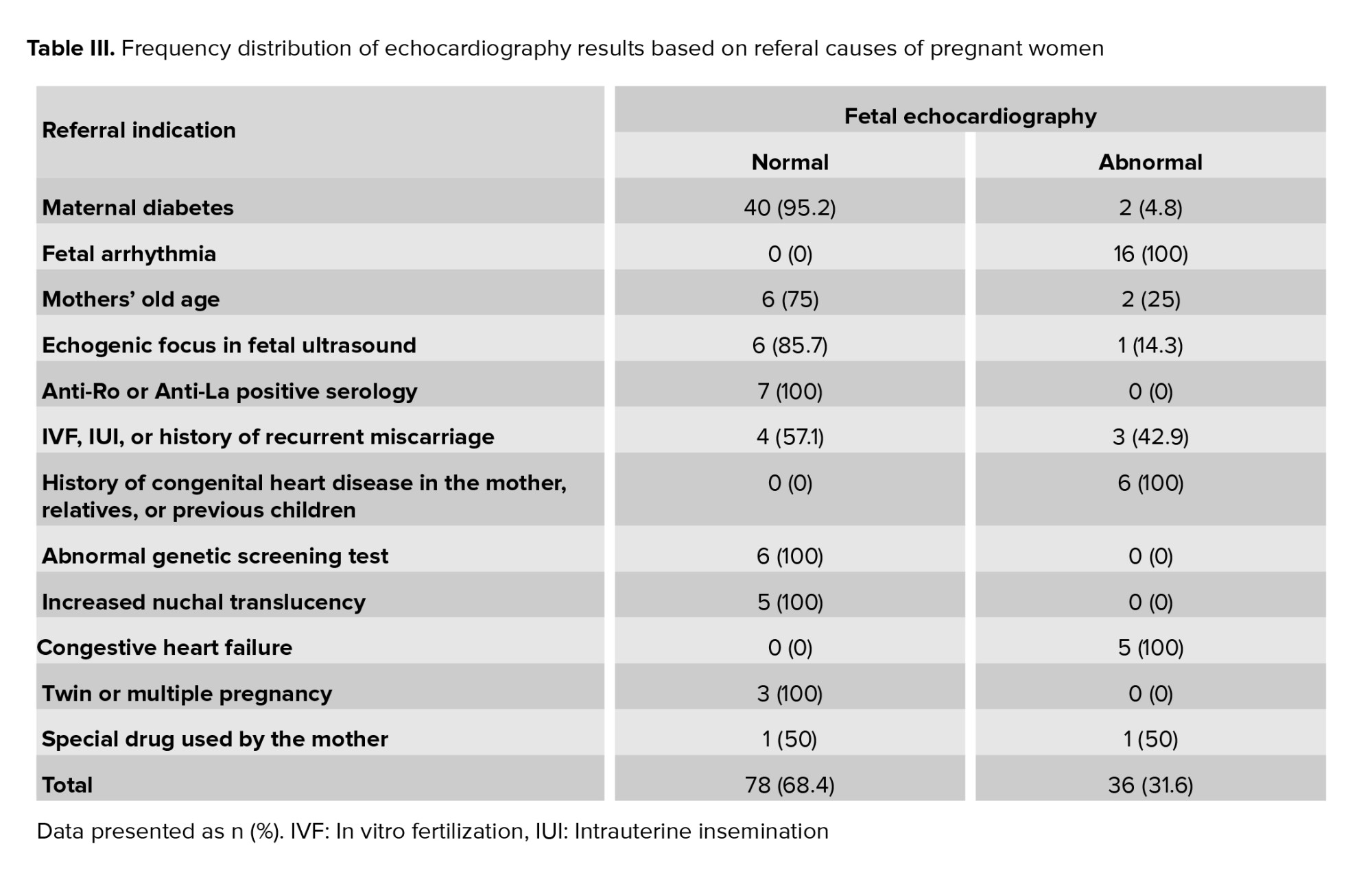
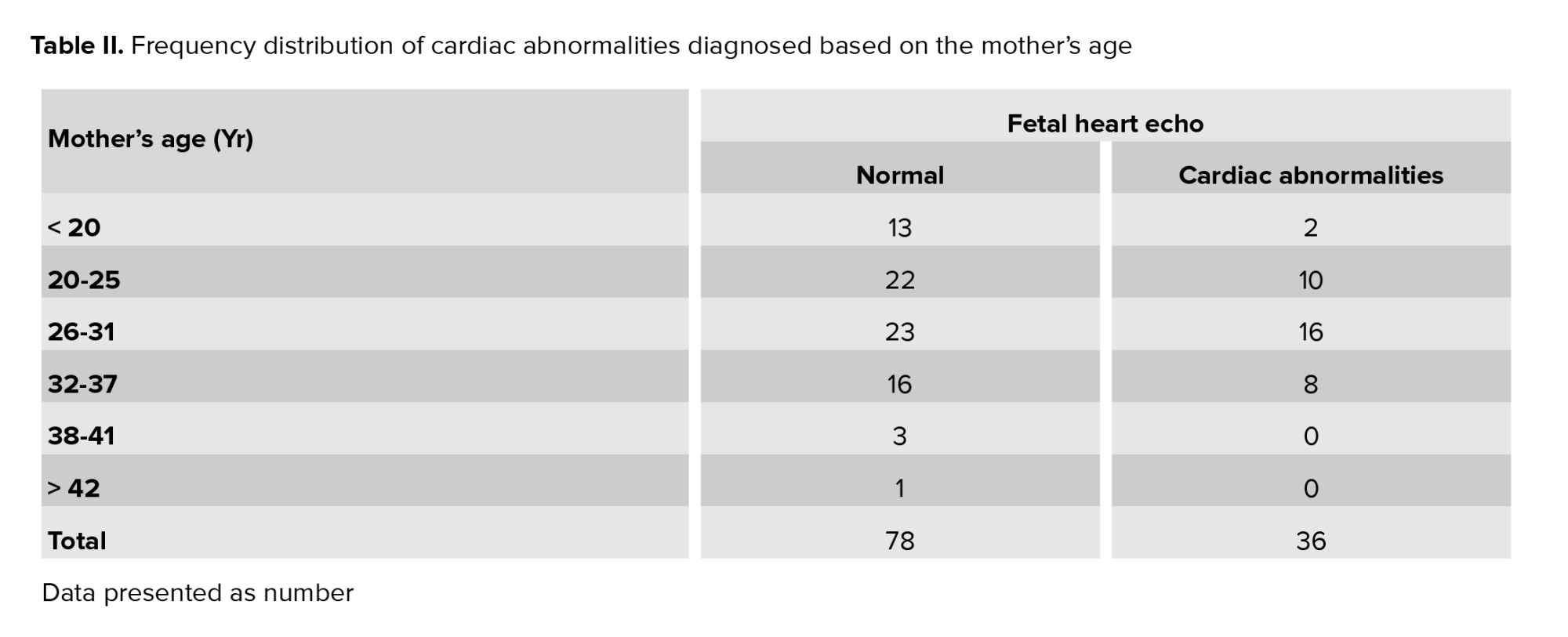
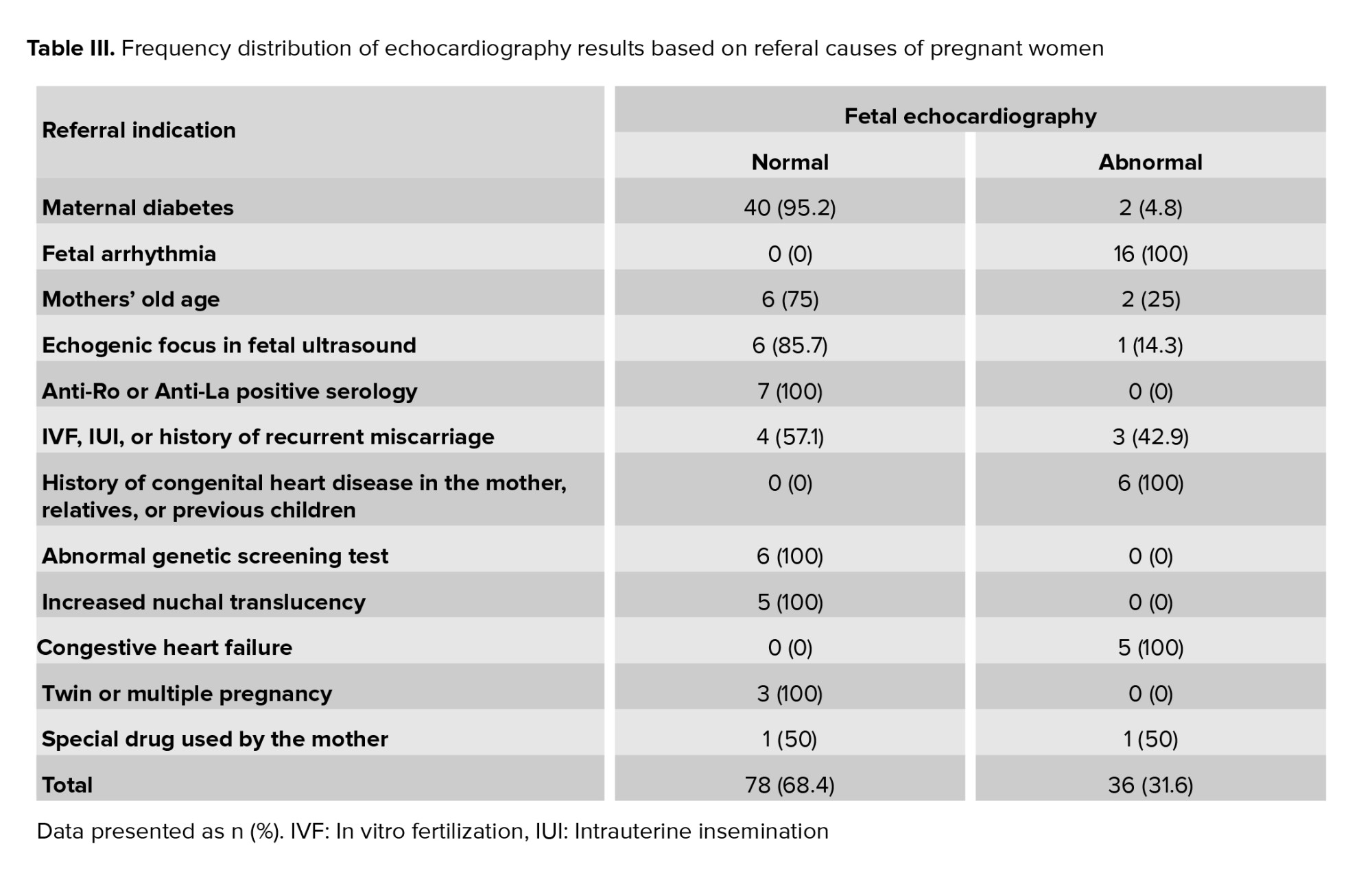
Table II shows the frequency distribution of cardiac abnormalities diagnosed based on the age of pregnant women. The highest rate of these abnormalities was in mothers aged 26-31 yr, which included 16 cases. Out of 42 (36.8%) pregnant women referred due to diabetes, 11 (9.6%) women had type 1 diabetes, and 31 (27.2%) were affected by type 2. On echocardiography 2 (1.8%) women were reported with cardiac abnormalities, both of which were related to type 1 diabetes. Of 5 cases (4.4%) of pregnant women who were referred due to in vitro fertilization, a cardiac abnormality was identified in 1 case (0.9%), whereas 4 other cases (3.5%) were normal. Also, 2 cases (1.8%) of pregnant women were referred due to a history of abortion; in both cases, a cardiac abnormality was observed. Among 6 women (5.3%) with a positive family history, 2 cases (1.8%) had a history of CHD in the mother or relatives and 4 women (3.5%) had a history disease in their previous children or fetuses. Cardiac abnormalities were observed in all 6 cases. Also, 2 cases (1.8%) were referred due to drug use in the mother; one of which (0.9%) was diagnosed with cardiac abnormality (Table III).
In postnatal echocardiography, out of 114 cases, only the results of 2 cases didn't match the prenatal results [2 cases of the small ventricular septal defect (VSD) which missed in fetal echocardiography]. Thus, the sensitivity of fetal echocardiography for early diagnosis of CHD and specificity were determined as 94.7 and 100%, respectively. Out of 114 referred pregnant women, 3 were treated with tachyarrhythmia, 3 with complete heart block, and 5 others with congestive heart failure, all showed signs of improvement (Table III).
4. Discussion
In this study, of 114 referred pregnant women, the most common reason for fetal echocardiography was diabetes (36.8%), 14% of referrals were due to fetal arrhythmia, and 49.2% were because of other problems. The results of fetal echocardiography revealed that 68.4% of cases were normal, 17.6% had cardiac anomalies, and 14% had abnormal cardiac rhythm.
In fetal echocardiography, we are faced with a host of images that fail to be sequenced, all of which may lead to errors in the correct diagnosis of fetal heart abnormalities or arrhythmias, thus warning us of the need for postnatal follow-up echocardiography (12).
In this study, the prevalence of CHD was 13.1%. However, in a study that had examined 1,200 cases of pregnancy for a year, the incidence of CHD was reported to be 15 per 1,000 births (4). Further, in research, the frequency was detected as 20.3 per 1000 births (4, 13). However, this in other studies has averaged 8 per thousand births, and the AHA guideline reports it as 6-12 per thousand live births. Of course, it must be taken into account our study population was selected based on the international society of ultrasound in obstetrics and gynecology guidelines, while in other similar studies, they were selected from the general population of pregnant women.
In the present study, the mean age of the mothers referred was 26.9 yr, while in another study, it reached 27.6 yr (4). Also, the mean gestational age of mothers in the present study was 19.75 wk. This rate amounted to 20.37 wk in Sharma's probe but 23.1 wk in Barsoom (4, 14). The highest cardiac abnormality diagnosed by fetal echocardiography was 16-19 wk of gestation. In reviewing other literature, the best time for diagnosis was attributed to referral in the second trimester; considering that the gestational age of the mothers referred in the present study was at the range of 12-37 wk, it seems that the age for referral has been late. Due to the need for religious and legal restrictions to terminate the pregnancy, this referral should preferably be before 19 wk. In this study, the most common reason for referral was maternal diabetes, which accounted for 36.8% of the cases. Fetal arrhythmias being 14% and maternal old age of 7% were other reasons for referral of the mothers. Of course, this rate can be justified due to the high prevalence of diabetes in Yazd, Iran, while in Barsoom and co-workers study, aneuploidy risk with 37.2% and echogenic focus with 12.1% were the most causes of fetal echocardiography, and maternal diabetes was identified in only 7.7%. Also, in another survey, the presence of echogenic focus was detected in 48% of cases, an increase in nuchal translucency thickness in 13%, and maternal age in 10% as the reasons for the referral of the mothers. In our study, the most common type of CHD identified was VSD with 4.4%. Also, the most common type of arrhythmia was related to premature atrial complex with 5.3% while in Mottaghi's research, CHD complex with 11.2%, in Sharma's study, VSD with 44.4%, in Nayak's study, endocardial cushion defect with 19.2% and in Chitra's study, VSD with 18.4% were the most common types of CHD reported (4, 13, 15, 16). Comparing the fetal and postnatal echocardiography results in this study, 94.4% sensitivity and 100% specificity were obtained for fetal echocardiography, while in Rakha and co-worker study; sensitivity and specificity were evaluated as 97.03 and 99.07%, respectively (17). Also, Sharma and colleagues reported a complete association between the 2 echocardiography amounting to 68.17% (4). Further, in another study, the sensitivity and specificity of the method were expressed as 85.5 and 100%, respectively (18).
5. Conclusion
This study showed that fetal echocardiography is a non-invasive method suitable for early diagnosis of CHDs with high sensitivity and specificity, being appropriate in high-risk and low-risk pregnancies. Also, it could be employed in early diagnosis and treatment of CHD if present or in abortion therapy.
Acknowledgments
We would like to thank our colleagues in Afshar hospital, Yazd, Iran, for helping us do the study.
Conflict of Interest
There was no conflict of interest in the study.
Full-Text: (421 Views)
1. Introduction
Congenital heart disease (CHD) is usually triggered by an abnormal development in the fetal heart structure in early embryonic stage (1). Some abnormalities may occur when the heart splits into 4 chambers and the valves form. Conotruncal disorders or valvular formation anomalies occur during these stages. These defects do not trigger prenatal or dynamic problems (2). Congenital vascular malformations are the most common group of birth defects and affect about 6-8 per thousand newborns (3). According to the previous studies, the prevalence of CHD is 6 times higher than chromosomal abnormalities and 4 times higher than neural tube defects. There are several risk factors involved in these diseases, which are generally divided into 2 categories maternal and fetal (4). In most cases, the cause is unknown; some are genetic, and some are environmental (5). Although in most cases they are multifactorial, several are also associated with chromosomal abnormalities, congenital defects, teratogens, or maternal metabolic disease. The range of lesions varies from asymptomatic to fatal anomalies (6).
Due to the high prevalence of congenital heart defects, fetal echocardiography is an important part of screening during pregnancy to diagnose fetal heart defects and arrhythmias (7). Fetal echocardiography has high sensitivity and specificity in diagnosing CHD in low- and high-risk populations (8). Fetal echocardiography is considered a standard part of pregnancy services (9). Techniques such as fetal heart magnetic resonance imaging and electrocardiogram are performed in only a few facilities due to their high cost and difficulty of access and are used only in research protocols. Fetal cardiac magnetic resonance imaging and fetal electrocardiography alternatives are acceptable procedures in diagnosing fetal atrial and ventricular arrhythmias (10). Although in fetal echocardiography, it is impossible to calculate details such as the p-wave axis or the width of QRS and QTC interval, the type of arrhythmia can only be identified based on changes in Doppler waves (11).
Moreover, in several other cases, such as fetal tachyarrhythmias, it is possible to prevent or treat heart failure by drugs prescribed to the mother. Another application of echocardiography in the treatment of non-autoimmune hydrops associated with fetal heart failure is performed by prescribing high-dose digoxin to the pregnant mother and monthly follow-up (4). Also, with early diagnosis of these diseases, fetal heart interventions can be used to treat these defects. One of the most successful of these interventions is transplacental drug therapy to treat fetal tachyarrhythmias (7).
Therefore, this study aimed to assess abnormal findings observed in fetal heart based on echocardiography and maternal disease.
2. Materials and Methods
This cross-sectional study was performed on 114 pregnant women referring to Afshar hospital, Yazd, Iran, from October 2016 and March 2017. Our inclusion criteria were pregnant women with a gestational age of 12 wk referred by gynecologists or radiologists for fetal echocardiography based on the international society of ultrasound in obstetrics and gynecology. All women in the first trimester of pregnancy, having a pregnancy with intrauterine fetal death, threatened with abortion fetuses, and incomplete abortion were excluded.
We intend to initially evaluate the diagnostic value of fetal echocardiography for early diagnosis of congenital diseases and also regarding the fact that some of these diseases are hard to cure. Although the standard time for fetal echocardiography to diagnose cardiac anomalies was before 19 wk of gestation, since several mothers were referred to evaluate diseases that could be medically intervened at any time (including fetal arrhythmia and heart failure), therefore, the referrals that after 19 wk of gestation were also included in the study. A pediatric cardiologist performed all echocardiography to prevent information bias. Participants' information including maternal age, gestational age, number of fetuses, underlying maternal disease, history of drug use or addiction in the mother, family history of CHD, history of infertility or use of assisted reproductive techniques, history of infectious diseases in the mother such as rubella, referral indication as well as final diagnosis after accurate fetal echocardiography was recorded. Echocardiography was performed by Color Doppler Echocardiograph, the Vivid 3 expert model (GE Healthcare, made in the USA), version 2011, and transducer containing crystal sets for 2-dimensional image (3.5 MHz with second harmonic technology). Also, follow-up echocardiography was done during 1st wk after birth for matching pre and post-natal diagnosis.
2.1. Ethical considerations
The Ethical Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran was approved the study proposal (Code: IR.SSU.MEDICINE.REC.1397.149). The oral consent was obtained from all participants.
2.1. Statistical analysis
The qualitative variables were reported as frequency and percentage. Data were analyzed by SPSS19 (IBM Corporation, New York, USA).
3. Results
A total of 114 pregnant women who underwent complete echocardiography and follow-up were included. The mean age of the pregnant women and their mean gestational age were 27 yr and 20 wk, respectively. The most common reason was diabetes (36.8%). While, 14% (n = 16) of referrals were due to fetal arrhythmia [Premature atrial complex (n = 6), bradyarrhythmia (n = 4), tachyarrhythmia (n = 3), and complete heart block (n = 3)]. The results of fetal echocardiography revealed that 68.4% (n = 78) were normal, 17.6% (n = 20) had cardiac anomalies, and 14% (n = 16) had arrhythmia (Figure 1).
Figure 2 shows the percentage of different types of cardiac abnormalities detected by echocardiography. The distribution of the frequency percentage of cardiac abnormalities detected by fetal echocardiography in each gestational age interval is reported in the table I, the highest rate found in 16-19 wk of pregnancy (44.4%).
Table II shows the frequency distribution of cardiac abnormalities diagnosed based on the age of pregnant women. The highest rate of these abnormalities was in mothers aged 26-31 yr, which included 16 cases. Out of 42 (36.8%) pregnant women referred due to diabetes, 11 (9.6%) women had type 1 diabetes, and 31 (27.2%) were affected by type 2. On echocardiography 2 (1.8%) women were reported with cardiac abnormalities, both of which were related to type 1 diabetes. Of 5 cases (4.4%) of pregnant women who were referred due to in vitro fertilization, a cardiac abnormality was identified in 1 case (0.9%), whereas 4 other cases (3.5%) were normal. Also, 2 cases (1.8%) of pregnant women were referred due to a history of abortion; in both cases, a cardiac abnormality was observed. Among 6 women (5.3%) with a positive family history, 2 cases (1.8%) had a history of CHD in the mother or relatives and 4 women (3.5%) had a history disease in their previous children or fetuses. Cardiac abnormalities were observed in all 6 cases. Also, 2 cases (1.8%) were referred due to drug use in the mother; one of which (0.9%) was diagnosed with cardiac abnormality (Table III).
In postnatal echocardiography, out of 114 cases, only the results of 2 cases didn't match the prenatal results [2 cases of the small ventricular septal defect (VSD) which missed in fetal echocardiography]. Thus, the sensitivity of fetal echocardiography for early diagnosis of CHD and specificity were determined as 94.7 and 100%, respectively. Out of 114 referred pregnant women, 3 were treated with tachyarrhythmia, 3 with complete heart block, and 5 others with congestive heart failure, all showed signs of improvement (Table III).
4. Discussion
In this study, of 114 referred pregnant women, the most common reason for fetal echocardiography was diabetes (36.8%), 14% of referrals were due to fetal arrhythmia, and 49.2% were because of other problems. The results of fetal echocardiography revealed that 68.4% of cases were normal, 17.6% had cardiac anomalies, and 14% had abnormal cardiac rhythm.
In fetal echocardiography, we are faced with a host of images that fail to be sequenced, all of which may lead to errors in the correct diagnosis of fetal heart abnormalities or arrhythmias, thus warning us of the need for postnatal follow-up echocardiography (12).
In this study, the prevalence of CHD was 13.1%. However, in a study that had examined 1,200 cases of pregnancy for a year, the incidence of CHD was reported to be 15 per 1,000 births (4). Further, in research, the frequency was detected as 20.3 per 1000 births (4, 13). However, this in other studies has averaged 8 per thousand births, and the AHA guideline reports it as 6-12 per thousand live births. Of course, it must be taken into account our study population was selected based on the international society of ultrasound in obstetrics and gynecology guidelines, while in other similar studies, they were selected from the general population of pregnant women.
In the present study, the mean age of the mothers referred was 26.9 yr, while in another study, it reached 27.6 yr (4). Also, the mean gestational age of mothers in the present study was 19.75 wk. This rate amounted to 20.37 wk in Sharma's probe but 23.1 wk in Barsoom (4, 14). The highest cardiac abnormality diagnosed by fetal echocardiography was 16-19 wk of gestation. In reviewing other literature, the best time for diagnosis was attributed to referral in the second trimester; considering that the gestational age of the mothers referred in the present study was at the range of 12-37 wk, it seems that the age for referral has been late. Due to the need for religious and legal restrictions to terminate the pregnancy, this referral should preferably be before 19 wk. In this study, the most common reason for referral was maternal diabetes, which accounted for 36.8% of the cases. Fetal arrhythmias being 14% and maternal old age of 7% were other reasons for referral of the mothers. Of course, this rate can be justified due to the high prevalence of diabetes in Yazd, Iran, while in Barsoom and co-workers study, aneuploidy risk with 37.2% and echogenic focus with 12.1% were the most causes of fetal echocardiography, and maternal diabetes was identified in only 7.7%. Also, in another survey, the presence of echogenic focus was detected in 48% of cases, an increase in nuchal translucency thickness in 13%, and maternal age in 10% as the reasons for the referral of the mothers. In our study, the most common type of CHD identified was VSD with 4.4%. Also, the most common type of arrhythmia was related to premature atrial complex with 5.3% while in Mottaghi's research, CHD complex with 11.2%, in Sharma's study, VSD with 44.4%, in Nayak's study, endocardial cushion defect with 19.2% and in Chitra's study, VSD with 18.4% were the most common types of CHD reported (4, 13, 15, 16). Comparing the fetal and postnatal echocardiography results in this study, 94.4% sensitivity and 100% specificity were obtained for fetal echocardiography, while in Rakha and co-worker study; sensitivity and specificity were evaluated as 97.03 and 99.07%, respectively (17). Also, Sharma and colleagues reported a complete association between the 2 echocardiography amounting to 68.17% (4). Further, in another study, the sensitivity and specificity of the method were expressed as 85.5 and 100%, respectively (18).
5. Conclusion
This study showed that fetal echocardiography is a non-invasive method suitable for early diagnosis of CHDs with high sensitivity and specificity, being appropriate in high-risk and low-risk pregnancies. Also, it could be employed in early diagnosis and treatment of CHD if present or in abortion therapy.
Acknowledgments
We would like to thank our colleagues in Afshar hospital, Yazd, Iran, for helping us do the study.
Conflict of Interest
There was no conflict of interest in the study.
Type of Study: Original Article |
Subject:
Pregnancy Health
References
1. Loscalzo J. Harrison's Cardiovascular Medicine 2/E. 3rd Ed. New York: McGraw-Hill Education; 2013.
2. Nelson LS, Hoffman RS, Howland MA, Lewin NA, Goldfrank LR. Goldfrank's toxicologic emergencies. New York: McGraw Hill Professional; 2018.
3. Hoffman J. Incidence, mortality and natural history. In: Anderson RH, Macortney FJ, Shinebourne EA. All pediatric cardiology. London: Churchill Livinstone; 1997.
4. Sharma Sh, Kaur N, Kaur Kh, Pawar NCh. Role of echocardiography in prenatal screening of congenital heart diseases and its correlation with postnatal outcome. J Clin Diagn Res 2017; 11: TC12-TC14. [DOI:10.7860/JCDR/2017/25929.9750] [PMID] [PMCID]
5. Buskens E, Grobbee DE, Frohn-Mulder IM, Wladimiroff JW, Hess J. Aspects of the aetiology of congenital heart disease. Eur Heart J 1995; 16: 584-587. [DOI:10.1093/oxfordjournals.eurheartj.a060960] [PMID]
6. Hoffman RS, Howland MA, Lewin NA, Nelson LS, Goldfrank LR. Goldfrank's toxicologic emergencies. New York: McGraw Hill Professional; 2014.
7. Hunter LE, Seale AN. Educational series in congenital heart disease: Prenatal diagnosis of congenital heart disease. Echo Res Pract 2018; 5: R81-R100. [DOI:10.1530/ERP-18-0027] [PMID] [PMCID]
8. Chu Ch, Yan Y, Ren Y, Li X, Gui Y. Prenatal diagnosis of congenital heart diseases by fetal echocardiography in second trimester: A Chinese multicenter study. Acta Obstet Gynecol Scand 2017; 96: 454-463. [DOI:10.1111/aogs.13085] [PMID]
9. Alves deRocha L, Júnior EA, Marcondes Machado Nardozz L, Fernandes Moron A. Screening of fetal congenital heart disease: The challenge continues. Rev Bras Cir Cardiovasc 2013; 28: V-VII. [DOI:10.5935/1678-9741.20130048] [PMID]
10. Fouron JC, Proulx F, Miró J, Gosselin J. Doppler and M-mode ultrasonography to time fetal atrial and ventricular contractions. Obstet Gynecol 2000; 96: 732-736.
https://doi.org/10.1097/00006250-200011000-00016 [DOI:10.1016/S0029-7844(00)01007-3] [PMID]
11. Jaeggi E, Fouron JC, Fournier A, van Doesburg N, Drblik SP, Proulx F. Ventriculo-atrial time interval measured on M-mode echocardiography: A determining element in diagnosis, treatment, and prognosis of fetal supraventricular tachycardia. Heart 1998; 79: 582-587. [DOI:10.1136/hrt.79.6.582] [PMID] [PMCID]
12. Mosaed P. Fetal echocardiography; Introduction and approaches. Sarem J Reprod Med 2018; 2: 31-34. [DOI:10.29252/sjrm.2.1.31]
13. Nayak K, Naveen Chandra GS, Shetty R, Narayan PK. Evaluation of fetal echocardiography as a routine antenatal screening tool for detection of congenital heart disease. Cardiovasc Diagn Ther 2016; 6: 44-49.
14. Barsoom MJ, Feldman DM, Borgida AF, Esters D, Diana D, Egan J. Is an isolated fetal cardiac echogenic focus an indication for fetal echocardiography? J Ultrasound Med 2001; 20: 1043-1046. [DOI:10.7863/jum.2001.20.10.1043] [PMID]
15. Ghiasi SS, Mottaghi Moghaddam Shahri H, Heidari E. Fetal echocardiography indications: A single-center experience. Int J Pediatr 2019; 7: 8969-8976.
16. Chitra N, Vijayalakshmi IB. Fetal echocardiography for early detection of congenital heart diseases. J Echocardiogr 2017; 15: 13-17. [DOI:10.1007/s12574-016-0308-2] [PMID]
17. Rakha S, El Marsafawy H. Sensitivity, specificity, and accuracy of fetal echocardiography for high-risk pregnancies in a tertiary center in Egypt. Arch Pédiatr 2019; 26: 337-341. [DOI:10.1016/j.arcped.2019.08.001] [PMID]
18. Stümpflen I, Stümpflen A, Wimmer M, Bernaschek G. Effect of detailed fetal echocardiography as part of routine prenatal ultrasonographic screening on detection of congenital heart disease. Lancet 1996; 348: 854-857.
https://doi.org/10.1016/S0140-6736(96)04069-X [DOI:10.1016/S0140-6736(05)65853-9]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |