Sat, Jul 12, 2025
[Archive]
Volume 20, Issue 7 (July 2022)
IJRM 2022, 20(7): 591-600 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mansour Ghanaei M, Asgharnia M, Farokhfar M, Asghari Ghalebin S M, Rafie E, Haryalchi K. The effect of consuming evening primrose oil on cervical preparation before hysteroscopy: An RCT. IJRM 2022; 20 (7) :591-600
URL: http://ijrm.ir/article-1-2301-en.html
URL: http://ijrm.ir/article-1-2301-en.html
Mandana Mansour Ghanaei1 

 , Maryam Asgharnia2
, Maryam Asgharnia2 

 , Maryam Farokhfar1
, Maryam Farokhfar1 

 , Seyed Mohammah Asghari Ghalebin1
, Seyed Mohammah Asghari Ghalebin1 

 , Elahe Rafie3
, Elahe Rafie3 

 , Katayoun Haryalchi *4
, Katayoun Haryalchi *4 




 , Maryam Asgharnia2
, Maryam Asgharnia2 

 , Maryam Farokhfar1
, Maryam Farokhfar1 

 , Seyed Mohammah Asghari Ghalebin1
, Seyed Mohammah Asghari Ghalebin1 

 , Elahe Rafie3
, Elahe Rafie3 

 , Katayoun Haryalchi *4
, Katayoun Haryalchi *4 


1- Reproductive Health Research Center, Department of Obstetrics and Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran.
2- Mehr Fertility Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Razi Clinical Research Development Unit, Guilan University of Medical Science, Rasht, Iran.
4- Reproductive Health Research Center, Department of Obstetrics and Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,K_haryalchi@yahoo.com
2- Mehr Fertility Research Center, Guilan University of Medical Sciences, Rasht, Iran.
3- Razi Clinical Research Development Unit, Guilan University of Medical Science, Rasht, Iran.
4- Reproductive Health Research Center, Department of Obstetrics and Gynecology, Alzahra Hospital, School of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,
Full-Text [PDF 321 kb]
(1596 Downloads)
| Abstract (HTML) (1379 Views)
1. Introduction
Hysteroscopy is a procedure in which a gynecologist evaluates the cervix by inserting a small telescope (hysteroscope) into the vagina and cervix (1). Approximately 50% of hysteroscopy complications are related to difficulties entering the cervix (2). Potential complications include cervical tears, false passage creation, uterine perforation, and difficulty in cervical entry (2-4).
Proper cervical ripening (CR) prior to hysteroscopy reduces the risk of complications associated with a difficult entry into the cervix (5). Cervical preparation is a complex process that results in physical softening, increased effacement, and dilatation due to enzymatic activity that decomposes collagen fibers and improves interstitial water (6, 7). CR agents include oral or vaginal prostaglandins that are either synthetic such as misoprostol, or natural like dinoprostone and vaginal osmotic dilators like laminaria (1, 8).
E series prostaglandins effectively dilate and prime the cervix, but some of them, such as dinoprostone, require special temperatures for preservation (9). In recent years, misoprostol (synthetic prostaglandin E1) has been used for obstetric and gynecological conditions such as in abortion therapy, treatment of postpartum hemorrhage as well as preparation treatment for hysteroscopy, vacuum aspiration, and dilatation (10-14). Some side effects of misoprostol include nausea, vomiting, diarrhea, vaginal bleeding, and abdominal cramps (11, 12). Misoprostol is the drug of choice for CR, but an alternative is needed due to its high price and instability (11, 12, 14). According to a meta-analysis, current evidence does not support routine administration of misoprostol before surgical hysteroscopy for all cases (15).
Evening primrose is a plant with yellow flowers that bloom at sunset. It is a native of North America and grows wild in parts of Europe (16). Iran has one of the most suitable climates for the cultivation of evening primrose (17).
Evening primrose oil (EPO) is a natural extract of the plant seeds. Because of its high content of polyunsaturated fatty acids, especially linoleic acid and gamma-linolenic acid as well as vitamin E, it is used as a dietary supplement (18). Gamma-linolenic acid is a well-known precursor to prostaglandin E (19) and is metabolized to arachidonic acid (20). The therapeutic effect of this plant is also attributed to the omega-6 essential fatty acid, which indirectly affects the synthesis of vaginal prostaglandins and cytokines (21). Consumption of EPO causes a significant increase in gammallenolic acid in the blood (22). A small number of controversial studies have been published about the effect of EPO on CR during pregnancy (23-26). Some studies have also claimed that the use of EPO in CR prior to hysteroscopy is safe and effective (27-29).
It is important to find less expensive alternatives for prostaglandins with fewer side effects to use in CR to prepare for hysteroscopy. For this reason, and because of the shortage of studies into the effect of EPO on CR before hysteroscopy, it was decided to investigate the effect of administrating EPO on cervical preparation.
2. Materials and Methods
This study was conducted using a double-blind, randomized controlled clinical trial design with 160 women who referred to Alzahra hospital, Rasht, Iran and candidates for diagnostic hysteroscopy from August 2019-March 2020.
Potential participants were assessed based on inclusion and exclusion criteria through clinical examinations and individual statements. The inclusion criterion was women candidates for hysteroscopy. The exclusion criteria were: present pregnancy, systemic diseases, cervical or vaginal infections, contraindications for the use of EPO (women with bleeding disorders, consumers of anticoagulants, schizophrenic individuals receiving phenothiazine, epileptics and those on medication for antihypertension), anomalies and cervical insufficiency, or müllerian type of delivery in case of previous childbirth (28).
The randomization method used was the stratified blocked randomization method, using quadruple blocks for 160 cases. Eligible subjects were divided into 2 groups: EPO and placebo, based on random allocation. The website https://www.sealedenvelope.com was used to make a randomization list of persons divided into study groups.
The intervention group (A) received 1000 mg of EPO (provided by Barij Esans Pharmaceutical Company, Iran) in the form of a soft gel capsule (2 pieces of 500 mg each) 6 hr before hysteroscopy in the posterior fornix of the vagina. The control group (B) received a placebo (placebo capsule provided by Barij Esans Pharmaceutical Company, Iran) in the same dose and shape as the evening primrose capsules in the same way as the intervention group (28). The researchers and participants were not aware of the sample randomization.
The same surgeon performed the hysteroscopy under general anesthesia using a resectoscope with an 11 mm outer sheath and a 30° lens.
Cervical dilatation began by using a size 3 Hegar dilator. The number of the dilator at the first resistance and the interval between the first resistance and the dilatation generated with size 10 Hegar were also recorded.
Factors considered in the study included: the time until the first resistance, duration of dilatation until the use of a size 10 Hegar, duration of hysteroscopy, size of the first Hegar, ease of dilation, and the need for mechanical dilatation. These factors were regarded as the primary outcomes to be measured throughout the surgery. Complications in the uterus and cervix (uterine rupture or bleeding, cervical rupture, and false passage), drug-related side effects, and preoperative pain due to medication were considered as secondary outcomes. Secondary outcomes were measured during the surgery and throughout the 24 hr after the surgery. A surgeon then evaluated all outcomes.
2.1. Ethical considerations
Ethical approval was obtained from the ethics committee of the Vice-Chancellor of Research at Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.193). Informed consent was taken from all participants. All participants' information was kept anonymous.
2.2. Statistical analysis
The data collected from the different stages were assessed, coded and analyzed using the SPSS software )Statistical Package for the Social Sciences, version 21.0, SPSS Inc, Chicago, Illinois, USA(. The median and mid-quadratic ranges were used to describe the abnormally distributed quantitative variables. Qualitative variables were described based on number and percentage. The subgroups' normal distribution of the quantitative variables was measured using elongation and skewness, histogram diagrams, Q-Q plots, and the Wilk-Shapiro test. To compare the quantitative abnormal variables in both groups, the Mann-Whitney test, Chi-square test, and Fisher’s exact test were used. The statistical significance of the tests was determined to be p < 0.05.
3. Results
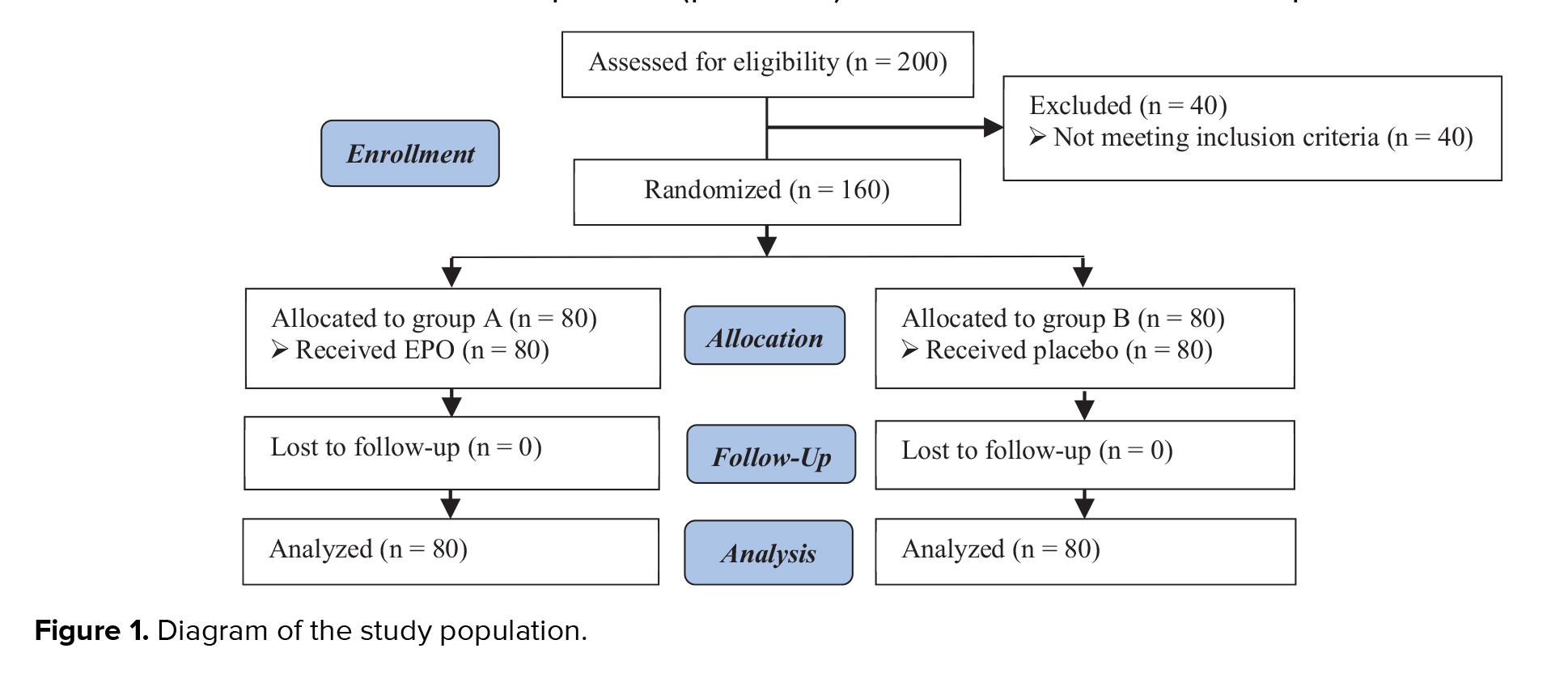
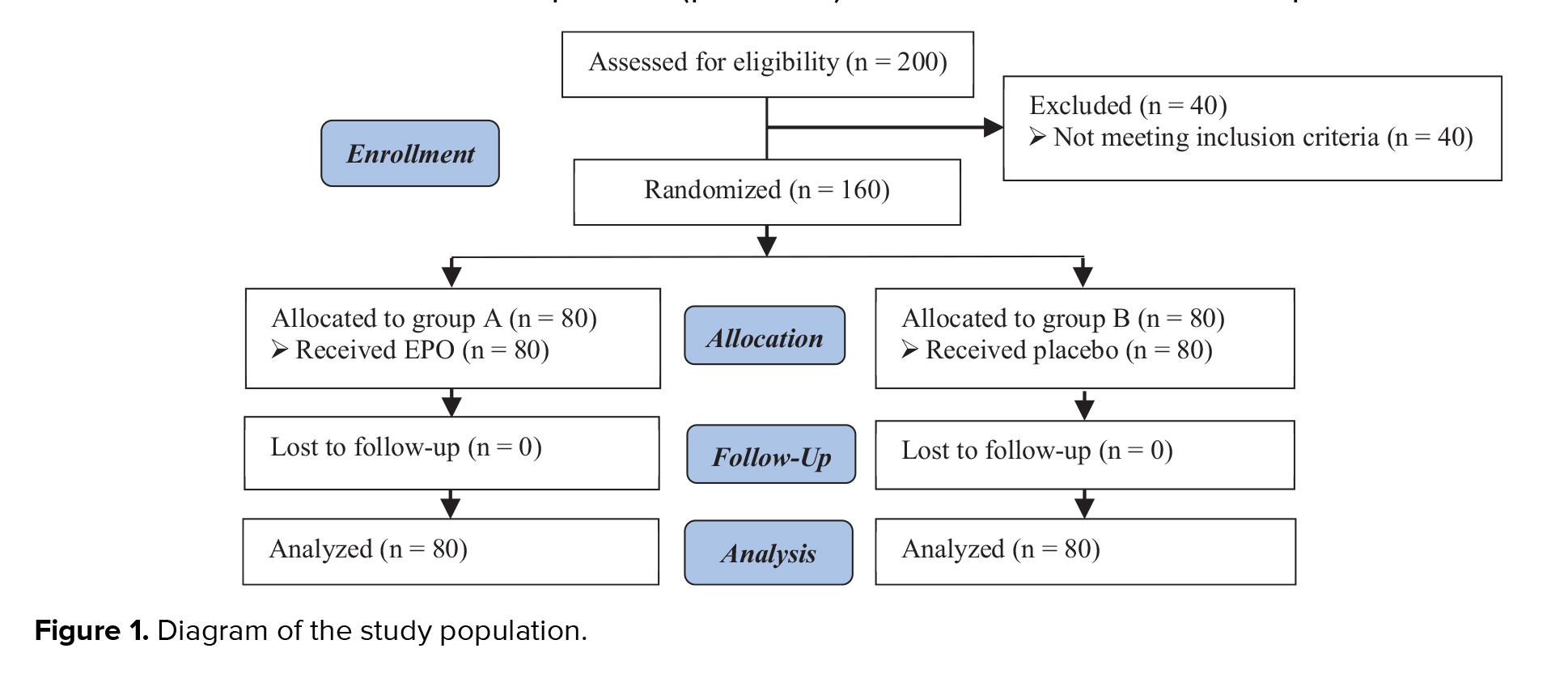
In this study, 200 subjects were interviewed. 40 did not meet the inclusion criteria, and 160 female candidates for hysteroscopy in 2 different groups of EPO and placebo) completed the study. The selection process and status of subjects in the study are given in figure 1.
Full-Text: (407 Views)
1. Introduction
Hysteroscopy is a procedure in which a gynecologist evaluates the cervix by inserting a small telescope (hysteroscope) into the vagina and cervix (1). Approximately 50% of hysteroscopy complications are related to difficulties entering the cervix (2). Potential complications include cervical tears, false passage creation, uterine perforation, and difficulty in cervical entry (2-4).
Proper cervical ripening (CR) prior to hysteroscopy reduces the risk of complications associated with a difficult entry into the cervix (5). Cervical preparation is a complex process that results in physical softening, increased effacement, and dilatation due to enzymatic activity that decomposes collagen fibers and improves interstitial water (6, 7). CR agents include oral or vaginal prostaglandins that are either synthetic such as misoprostol, or natural like dinoprostone and vaginal osmotic dilators like laminaria (1, 8).
E series prostaglandins effectively dilate and prime the cervix, but some of them, such as dinoprostone, require special temperatures for preservation (9). In recent years, misoprostol (synthetic prostaglandin E1) has been used for obstetric and gynecological conditions such as in abortion therapy, treatment of postpartum hemorrhage as well as preparation treatment for hysteroscopy, vacuum aspiration, and dilatation (10-14). Some side effects of misoprostol include nausea, vomiting, diarrhea, vaginal bleeding, and abdominal cramps (11, 12). Misoprostol is the drug of choice for CR, but an alternative is needed due to its high price and instability (11, 12, 14). According to a meta-analysis, current evidence does not support routine administration of misoprostol before surgical hysteroscopy for all cases (15).
Evening primrose is a plant with yellow flowers that bloom at sunset. It is a native of North America and grows wild in parts of Europe (16). Iran has one of the most suitable climates for the cultivation of evening primrose (17).
Evening primrose oil (EPO) is a natural extract of the plant seeds. Because of its high content of polyunsaturated fatty acids, especially linoleic acid and gamma-linolenic acid as well as vitamin E, it is used as a dietary supplement (18). Gamma-linolenic acid is a well-known precursor to prostaglandin E (19) and is metabolized to arachidonic acid (20). The therapeutic effect of this plant is also attributed to the omega-6 essential fatty acid, which indirectly affects the synthesis of vaginal prostaglandins and cytokines (21). Consumption of EPO causes a significant increase in gammallenolic acid in the blood (22). A small number of controversial studies have been published about the effect of EPO on CR during pregnancy (23-26). Some studies have also claimed that the use of EPO in CR prior to hysteroscopy is safe and effective (27-29).
It is important to find less expensive alternatives for prostaglandins with fewer side effects to use in CR to prepare for hysteroscopy. For this reason, and because of the shortage of studies into the effect of EPO on CR before hysteroscopy, it was decided to investigate the effect of administrating EPO on cervical preparation.
2. Materials and Methods
This study was conducted using a double-blind, randomized controlled clinical trial design with 160 women who referred to Alzahra hospital, Rasht, Iran and candidates for diagnostic hysteroscopy from August 2019-March 2020.
Potential participants were assessed based on inclusion and exclusion criteria through clinical examinations and individual statements. The inclusion criterion was women candidates for hysteroscopy. The exclusion criteria were: present pregnancy, systemic diseases, cervical or vaginal infections, contraindications for the use of EPO (women with bleeding disorders, consumers of anticoagulants, schizophrenic individuals receiving phenothiazine, epileptics and those on medication for antihypertension), anomalies and cervical insufficiency, or müllerian type of delivery in case of previous childbirth (28).
The randomization method used was the stratified blocked randomization method, using quadruple blocks for 160 cases. Eligible subjects were divided into 2 groups: EPO and placebo, based on random allocation. The website https://www.sealedenvelope.com was used to make a randomization list of persons divided into study groups.
The intervention group (A) received 1000 mg of EPO (provided by Barij Esans Pharmaceutical Company, Iran) in the form of a soft gel capsule (2 pieces of 500 mg each) 6 hr before hysteroscopy in the posterior fornix of the vagina. The control group (B) received a placebo (placebo capsule provided by Barij Esans Pharmaceutical Company, Iran) in the same dose and shape as the evening primrose capsules in the same way as the intervention group (28). The researchers and participants were not aware of the sample randomization.
The same surgeon performed the hysteroscopy under general anesthesia using a resectoscope with an 11 mm outer sheath and a 30° lens.
Cervical dilatation began by using a size 3 Hegar dilator. The number of the dilator at the first resistance and the interval between the first resistance and the dilatation generated with size 10 Hegar were also recorded.
Factors considered in the study included: the time until the first resistance, duration of dilatation until the use of a size 10 Hegar, duration of hysteroscopy, size of the first Hegar, ease of dilation, and the need for mechanical dilatation. These factors were regarded as the primary outcomes to be measured throughout the surgery. Complications in the uterus and cervix (uterine rupture or bleeding, cervical rupture, and false passage), drug-related side effects, and preoperative pain due to medication were considered as secondary outcomes. Secondary outcomes were measured during the surgery and throughout the 24 hr after the surgery. A surgeon then evaluated all outcomes.
2.1. Ethical considerations
Ethical approval was obtained from the ethics committee of the Vice-Chancellor of Research at Guilan University of Medical Sciences, Rasht, Iran (Code: IR.GUMS.REC.1398.193). Informed consent was taken from all participants. All participants' information was kept anonymous.
2.2. Statistical analysis
The data collected from the different stages were assessed, coded and analyzed using the SPSS software )Statistical Package for the Social Sciences, version 21.0, SPSS Inc, Chicago, Illinois, USA(. The median and mid-quadratic ranges were used to describe the abnormally distributed quantitative variables. Qualitative variables were described based on number and percentage. The subgroups' normal distribution of the quantitative variables was measured using elongation and skewness, histogram diagrams, Q-Q plots, and the Wilk-Shapiro test. To compare the quantitative abnormal variables in both groups, the Mann-Whitney test, Chi-square test, and Fisher’s exact test were used. The statistical significance of the tests was determined to be p < 0.05.
3. Results
In this study, 200 subjects were interviewed. 40 did not meet the inclusion criteria, and 160 female candidates for hysteroscopy in 2 different groups of EPO and placebo) completed the study. The selection process and status of subjects in the study are given in figure 1.
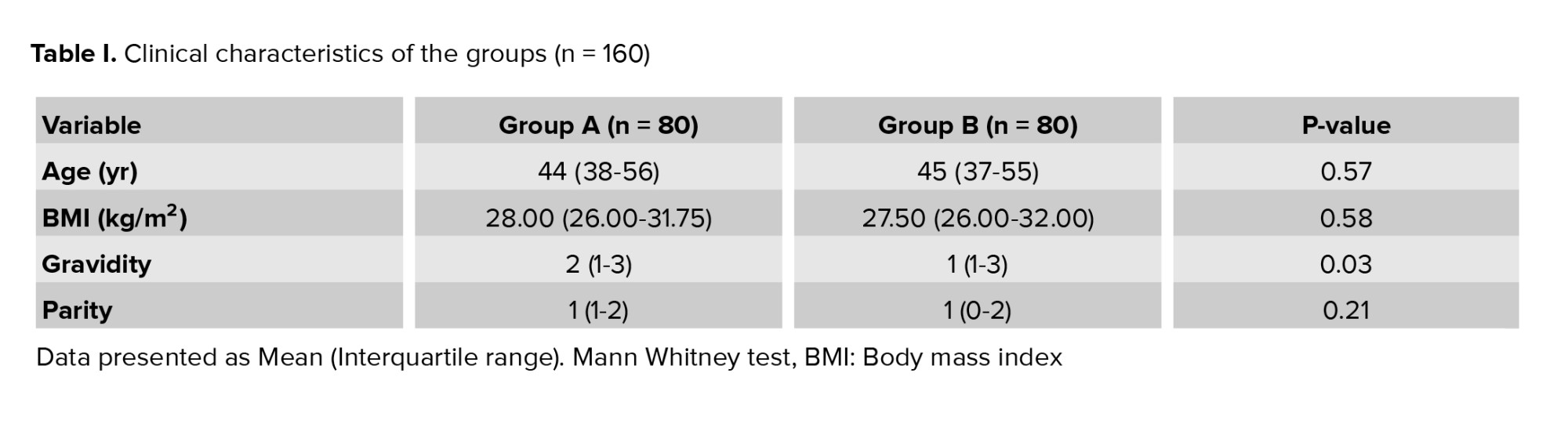
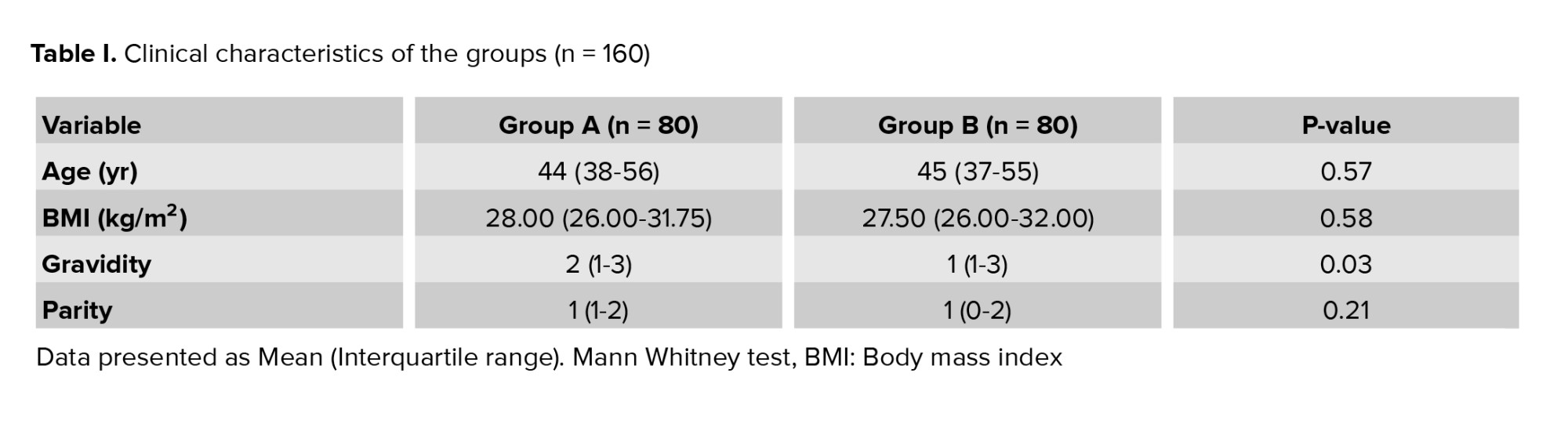
In the female candidates for hysteroscopy there was no statistically significant difference in age (p = 0.57), body mass index (p = 0.58) and parity (p = 0.21) between the 2 groups receiving EPO and placebo. However, in terms of gravidity, there was a statistically significant difference between the 2 groups (p = 0.03) (Table I).
For the menopausal women who were candidates for hysteroscopy, there was a statistically significant difference between the 2 groups in gravidity, first Hegar size, first resistance enteral and dilatation interval. There was not a statistically significant difference between the 2 treatment groups in gravidity, regarded as a variable interfering in the linear relationship with factors under investigation in the study. In candidates for non-menopausal hysteroscopy, there was a significantly different first Hegar size, first resistance enteral and dilatation interval between the 2 groups (Table II).
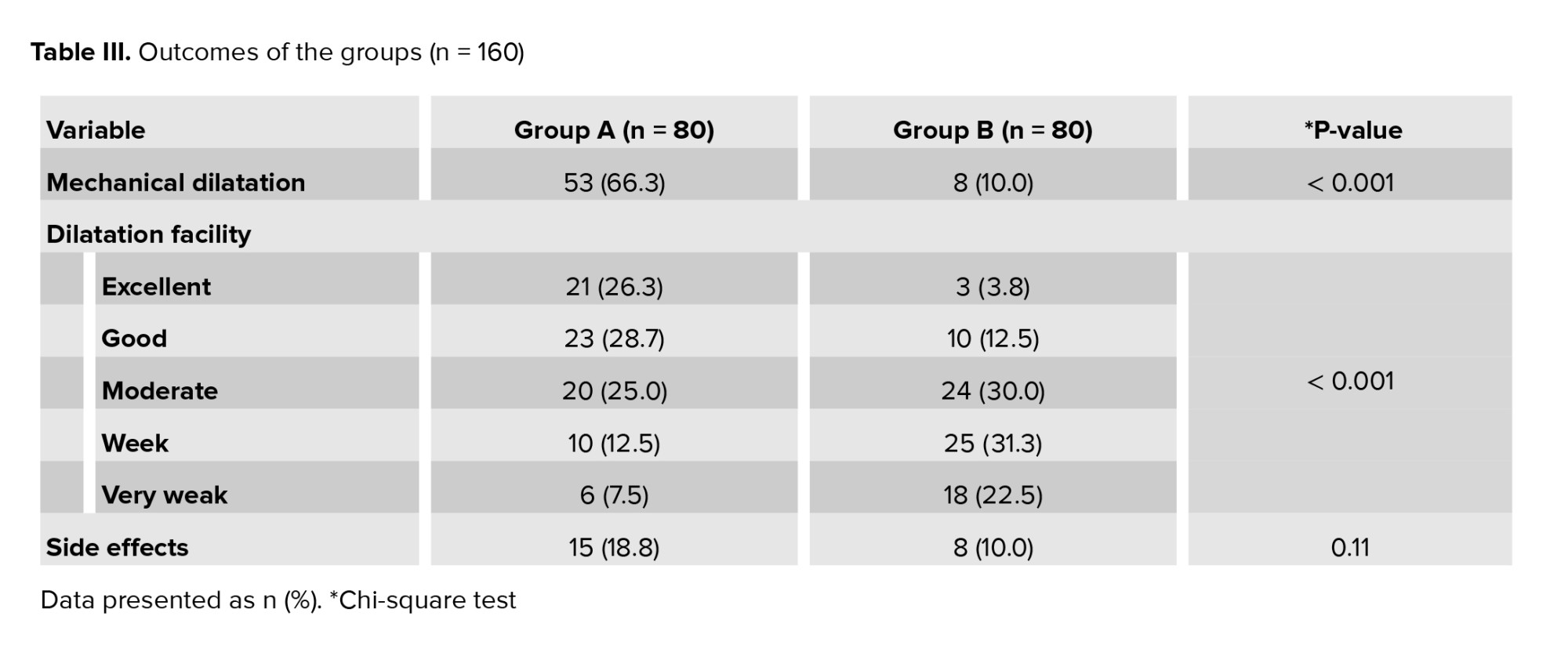
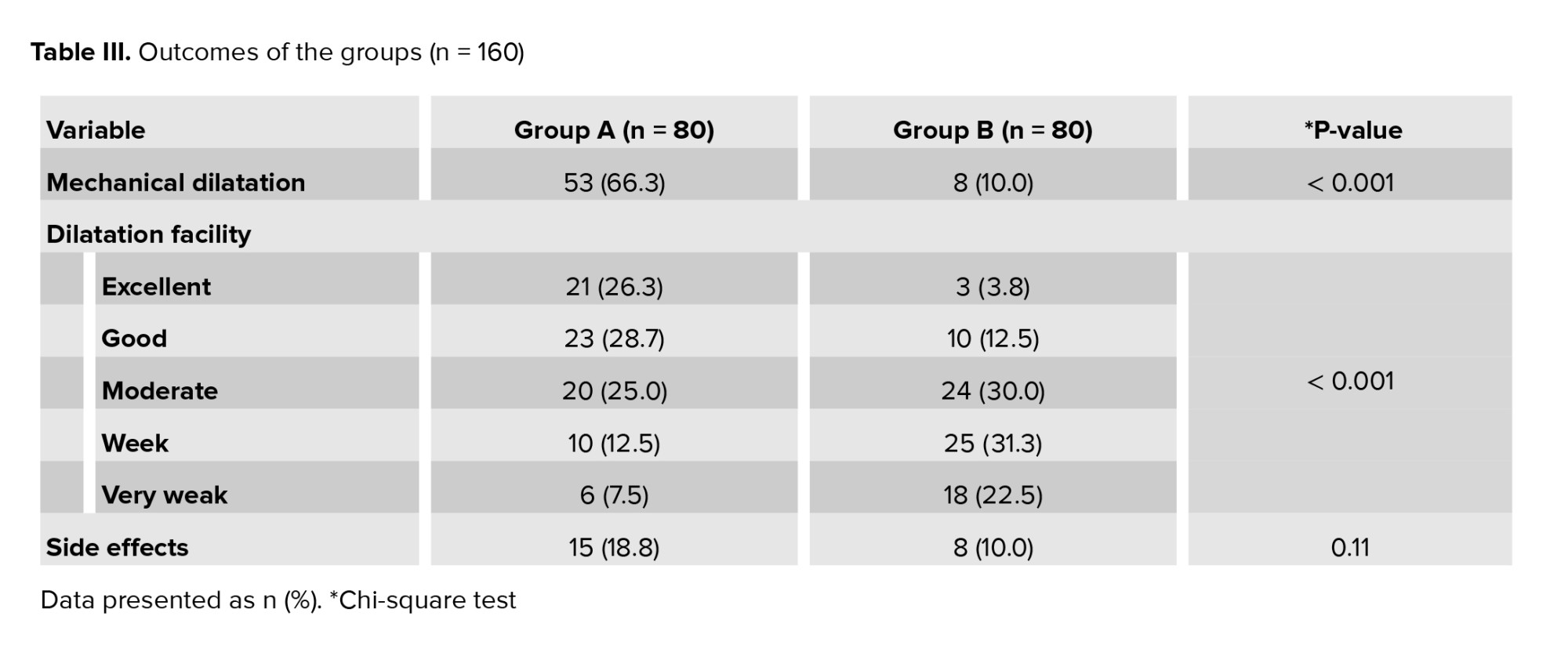
The percentage of those requiring mechanical dilatation and the time of dilation in the EPO group were significantly lower than in the placebo group (p < 0.001) (Table III). Dilatation in the EPO group was generally easier than in the placebo group (p < 0.001) as 100% of the subjects did not report preoperative pain (n = 0). The difference in the level of preoperative pain in the EPO vs. control groups was not statistically significant (p = 0.23). The percentage of adverse effects in the EPO group was higher than in the placebo group. Reported complications included 23 cases of spotting (15 cases in the EPO group and 8 cases in the placebo group) and 1 case of bleeding in the EPO group. However, the difference between the 2 groups was not statistically significant (p = 0.11). No side effects such as uterine rupture, cervical rupture, false passage, allergic reactions, abdominal pain, nausea, diarrhea, headache, or increased bowel movements were observed (Table III).
In the subgroup of menopausal candidates for hysteroscopy, there was no statistically significant difference between the 2 groups in terms of the size of the first Hegar used (p < 0.001) (Table III). The percentage of those needing mechanical dilatation in the EPO group was significantly lower than in the placebo group (p < 0.01). The time spent until the first resistance (p < 0.001) and the duration of completing the dilation (p < 0.001) in the EPO group were also significantly shorter than in the placebo one. The duration of the operation in the EPO group was shorter than in the placebo group; however, this difference was not statistically significant (p = 0.96).
There was greater ease of dilatation in the EPO group than in the placebo group (p < 0.001). The difference in the preoperative pain levels in the EPO and placebo groups was not statistically significant (p > 0.99). The percentage of side effects in the EPO group was higher than in the placebo group; however, the observed difference was not statistically significant (p = 0.47). Complications reported included 9 cases of spotting (6 cases in the EPO group and 3 cases in the placebo group). Side effects such as bleeding, uterine rupture, false passage, cervical rupture, allergic reactions, abdominal pain, nausea, diarrhea, headache, and increased bowel movements were not observed in any cases.
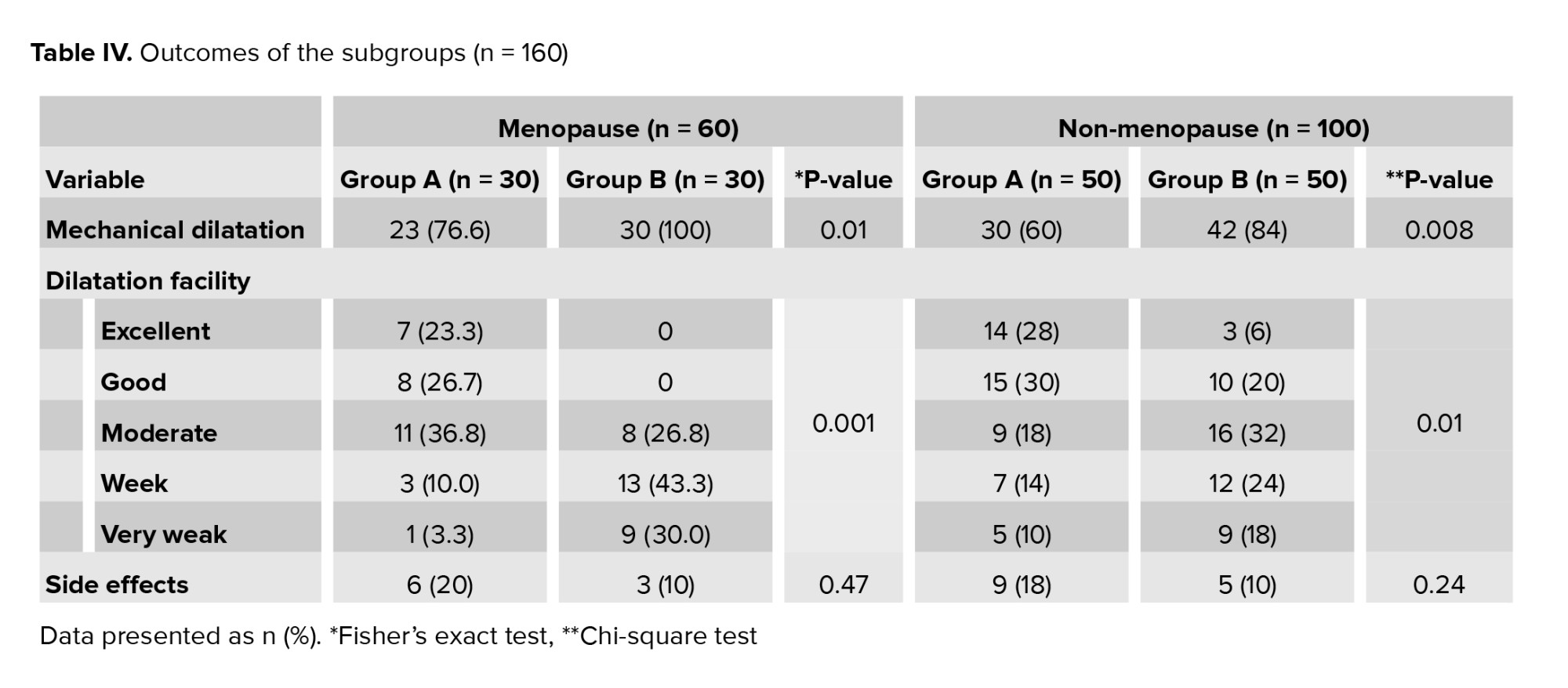
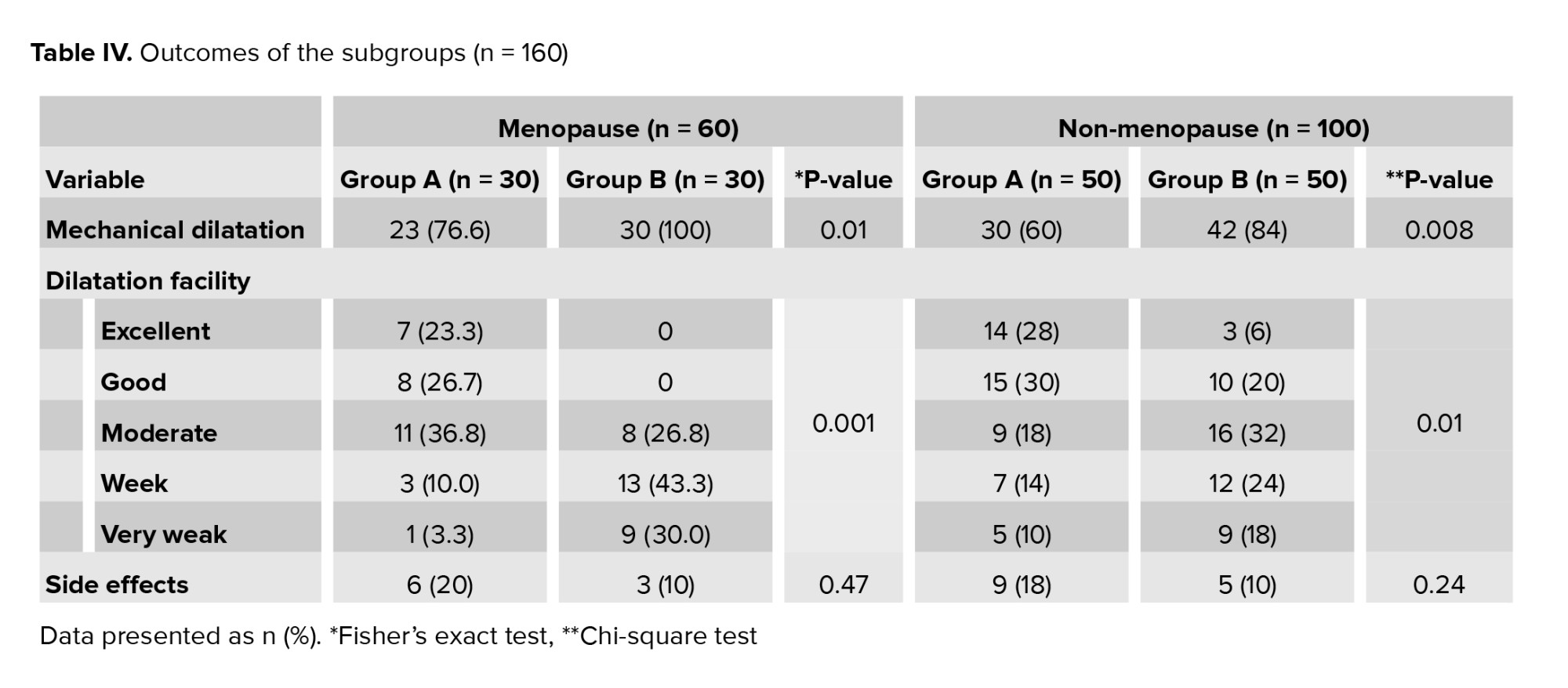
In the subgroup of non-menopausal women who were candidates for hysteroscopy, there was a statistically significant difference between the 2 groups in the size of the first Hegar used (p < 0.01). The percentage of the need for mechanical dilatation in the EPO group was significantly lower than in the placebo group (p = 0.01) (Table IV).
The time taken until the first resistance (p = 0.01), and the time of dilatation completion (p < 0.01) in the EPO group were also significantly shorter than in the placebo group. The duration of the operation in the EPO group was shorter than in the placebo one; however, the observed difference was not statistically significant (p = 0.13). There was a greater ease of dilatation in the EPO group than in the placebo group (p = 0.01). The preoperative pain in the EPO and placebo groups did not differ significantly (p = 0.19).
The percentage of side effects in the EPO group was higher than in the placebo one; however, the difference was not statistically significant (p = 0.24). Side effects included 13 cases of spotting (8 cases in the EPO group vs. 5 cases in the placebo group), and 1 case of bleeding was observed in the EPO group. Adverse effects such as uterine rupture, false passage, cervical rupture, allergic reactions, nausea, diarrhea, headache, and increased bowel movements were not reported.

4. Discussion
The increasing use of medicinal plants by women, especially during their reproductive periods and pregnancy, has attracted the attention of researchers in pursuit of more effective treatments (30).
Modern medical sciences tries to treat individuals with the least invasive method possible. The results showed a difference between the 2 groups in the size of the first Hegar used, which was larger in the EPO group. Also, the need for mechanical dilation, the time taken until the first resistance, and the time of dilatation completion in the EPO group were significantly less than in the placebo group. The dilatation in the EPO group was easier than in the placebo group. There was no significant difference between the 2 groups in terms of complications. There were similar results in the 2 groups in cases of menopausal candidates for hysteroscopy.
Most of the Iranian review studies conducted in recent years have focused on EPO with regards to premenstrual syndrome and polycystic ovary syndrome. The results of all those studies have confirmed the positive effect of EPO in reducing premenstrual syndrome symptoms (31, 32). Another review study conducted in 2019 indicated that EPO was generally effective in improving the health of Iranian women within 4-6 months at most (33). Few previous studies on EPO have concentrated on its effect on dilatation and cervical preparation before hysteroscopy (23). Therefore, more extensive studies are required in this regard.
A study on non-menopausal women without a history of normal vaginal delivery and on menopausal women under hysteroscopy confirmed the positive effect of EPO in preparing the cervix before hysteroscopy. Duration of cervical dilatation was shorter in the EPO group, and the size of the first Hegar used in that group was larger than in the placebo one (28). In the present study, the median length of Hegar was bigger in the EPO group.
A randomized clinical trial compared the performance of intracervical laminaria vs. intravaginal EPO before hysteroscopy. They showed that both medicines were effective in cervical dilatation. However, cervical dilatation was induced in a shorter time and more easily in the EPO group compared to in the laminaria group. The researchers also showed that EPO could even be used 6 hr before gynecological surgery procedures such as hysteroscopy and curettage to improve cervical dilation and firmness. About 85% of cases showed improvement in cervical dilatation and effacement as well as a change of the bishop score 4 hr after the intervention with the EPO capsule (34). In the present study, ease of dilatation was better in the EPO group.
Based on the results of the present study, there was no difference in the rate of complications between the 2 groups. Also, there were no side effects such as uterine rupture, false passage, cervical rupture, allergic reactions, abdominal pain, nausea, diarrhea, headache, and increased bowel movements. Similar results were reported in a pilot study on menopausal women and nulliparous women with menopause. In this study, no patient in the EPO group showed any adverse effects (29).
In the present study, the percentage of patients requiring mechanical dilation and the time taken to complete dilatation in the EPO group was significantly less than in the placebo one. In a double-blind clinical trial, there was similarly a statistically significant difference between the EPO and placebo groups (7.8 mm vs. 4.3 mm) due to the initial dilation of the cervix. In the EPO group, only 47.6% of subjects needed mechanical dilation of the cervix. The mean time to achieve a dilation of 10 mm was shorter in the EPO group (53.5 sec vs. 17.3 sec) (27). In another study, oral EPO and intracervical gel of dinoprostone were equally effective on cervical preparation before hysteroscopy (35).
One of the advantages of the present study was the use of EPO in a larger sample size compared to previous studies.
5. Conclusion
Based on the findings of the present study and other similar studies conducted in recent years, we can conclude that EPO is effective for cervical preparation in women candidates before hysteroscopy. Therefore, it is recommended as an alternative treatment to improve women's health because of its convenience and cost-effectiveness.
Acknowledgments
This study was financially supported by the Vice-Chanceller of Research and Technology, Guilan University of Medical Science, Rasht, Iran. We would like to express gratitude to all participants who accepted to be in our trial.
Conflict of Interest
The authors declare that there is no conflict of interest.
The percentage of those requiring mechanical dilatation and the time of dilation in the EPO group were significantly lower than in the placebo group (p < 0.001) (Table III). Dilatation in the EPO group was generally easier than in the placebo group (p < 0.001) as 100% of the subjects did not report preoperative pain (n = 0). The difference in the level of preoperative pain in the EPO vs. control groups was not statistically significant (p = 0.23). The percentage of adverse effects in the EPO group was higher than in the placebo group. Reported complications included 23 cases of spotting (15 cases in the EPO group and 8 cases in the placebo group) and 1 case of bleeding in the EPO group. However, the difference between the 2 groups was not statistically significant (p = 0.11). No side effects such as uterine rupture, cervical rupture, false passage, allergic reactions, abdominal pain, nausea, diarrhea, headache, or increased bowel movements were observed (Table III).
In the subgroup of menopausal candidates for hysteroscopy, there was no statistically significant difference between the 2 groups in terms of the size of the first Hegar used (p < 0.001) (Table III). The percentage of those needing mechanical dilatation in the EPO group was significantly lower than in the placebo group (p < 0.01). The time spent until the first resistance (p < 0.001) and the duration of completing the dilation (p < 0.001) in the EPO group were also significantly shorter than in the placebo one. The duration of the operation in the EPO group was shorter than in the placebo group; however, this difference was not statistically significant (p = 0.96).
There was greater ease of dilatation in the EPO group than in the placebo group (p < 0.001). The difference in the preoperative pain levels in the EPO and placebo groups was not statistically significant (p > 0.99). The percentage of side effects in the EPO group was higher than in the placebo group; however, the observed difference was not statistically significant (p = 0.47). Complications reported included 9 cases of spotting (6 cases in the EPO group and 3 cases in the placebo group). Side effects such as bleeding, uterine rupture, false passage, cervical rupture, allergic reactions, abdominal pain, nausea, diarrhea, headache, and increased bowel movements were not observed in any cases.
In the subgroup of non-menopausal women who were candidates for hysteroscopy, there was a statistically significant difference between the 2 groups in the size of the first Hegar used (p < 0.01). The percentage of the need for mechanical dilatation in the EPO group was significantly lower than in the placebo group (p = 0.01) (Table IV).
The time taken until the first resistance (p = 0.01), and the time of dilatation completion (p < 0.01) in the EPO group were also significantly shorter than in the placebo group. The duration of the operation in the EPO group was shorter than in the placebo one; however, the observed difference was not statistically significant (p = 0.13). There was a greater ease of dilatation in the EPO group than in the placebo group (p = 0.01). The preoperative pain in the EPO and placebo groups did not differ significantly (p = 0.19).
The percentage of side effects in the EPO group was higher than in the placebo one; however, the difference was not statistically significant (p = 0.24). Side effects included 13 cases of spotting (8 cases in the EPO group vs. 5 cases in the placebo group), and 1 case of bleeding was observed in the EPO group. Adverse effects such as uterine rupture, false passage, cervical rupture, allergic reactions, nausea, diarrhea, headache, and increased bowel movements were not reported.

4. Discussion
The increasing use of medicinal plants by women, especially during their reproductive periods and pregnancy, has attracted the attention of researchers in pursuit of more effective treatments (30).
Modern medical sciences tries to treat individuals with the least invasive method possible. The results showed a difference between the 2 groups in the size of the first Hegar used, which was larger in the EPO group. Also, the need for mechanical dilation, the time taken until the first resistance, and the time of dilatation completion in the EPO group were significantly less than in the placebo group. The dilatation in the EPO group was easier than in the placebo group. There was no significant difference between the 2 groups in terms of complications. There were similar results in the 2 groups in cases of menopausal candidates for hysteroscopy.
Most of the Iranian review studies conducted in recent years have focused on EPO with regards to premenstrual syndrome and polycystic ovary syndrome. The results of all those studies have confirmed the positive effect of EPO in reducing premenstrual syndrome symptoms (31, 32). Another review study conducted in 2019 indicated that EPO was generally effective in improving the health of Iranian women within 4-6 months at most (33). Few previous studies on EPO have concentrated on its effect on dilatation and cervical preparation before hysteroscopy (23). Therefore, more extensive studies are required in this regard.
A study on non-menopausal women without a history of normal vaginal delivery and on menopausal women under hysteroscopy confirmed the positive effect of EPO in preparing the cervix before hysteroscopy. Duration of cervical dilatation was shorter in the EPO group, and the size of the first Hegar used in that group was larger than in the placebo one (28). In the present study, the median length of Hegar was bigger in the EPO group.
A randomized clinical trial compared the performance of intracervical laminaria vs. intravaginal EPO before hysteroscopy. They showed that both medicines were effective in cervical dilatation. However, cervical dilatation was induced in a shorter time and more easily in the EPO group compared to in the laminaria group. The researchers also showed that EPO could even be used 6 hr before gynecological surgery procedures such as hysteroscopy and curettage to improve cervical dilation and firmness. About 85% of cases showed improvement in cervical dilatation and effacement as well as a change of the bishop score 4 hr after the intervention with the EPO capsule (34). In the present study, ease of dilatation was better in the EPO group.
Based on the results of the present study, there was no difference in the rate of complications between the 2 groups. Also, there were no side effects such as uterine rupture, false passage, cervical rupture, allergic reactions, abdominal pain, nausea, diarrhea, headache, and increased bowel movements. Similar results were reported in a pilot study on menopausal women and nulliparous women with menopause. In this study, no patient in the EPO group showed any adverse effects (29).
In the present study, the percentage of patients requiring mechanical dilation and the time taken to complete dilatation in the EPO group was significantly less than in the placebo one. In a double-blind clinical trial, there was similarly a statistically significant difference between the EPO and placebo groups (7.8 mm vs. 4.3 mm) due to the initial dilation of the cervix. In the EPO group, only 47.6% of subjects needed mechanical dilation of the cervix. The mean time to achieve a dilation of 10 mm was shorter in the EPO group (53.5 sec vs. 17.3 sec) (27). In another study, oral EPO and intracervical gel of dinoprostone were equally effective on cervical preparation before hysteroscopy (35).
One of the advantages of the present study was the use of EPO in a larger sample size compared to previous studies.
5. Conclusion
Based on the findings of the present study and other similar studies conducted in recent years, we can conclude that EPO is effective for cervical preparation in women candidates before hysteroscopy. Therefore, it is recommended as an alternative treatment to improve women's health because of its convenience and cost-effectiveness.
Acknowledgments
This study was financially supported by the Vice-Chanceller of Research and Technology, Guilan University of Medical Science, Rasht, Iran. We would like to express gratitude to all participants who accepted to be in our trial.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Reproductive Urology
References
1. Al-Fozan H, Firwana B, Al Kadri H, Hassan S, Tulandi T. Preoperative ripening of the cervix before operative hysteroscopy. Cochrane Database Syst Rev 2015; 4: Cd005998. [DOI:10.1002/14651858.CD005998.pub2] [PMID]
2. Stankova T, Ganovska A, Stoianova M, Kovachev S. Complications of diagnostic and operative hysteroscopy: Review. Akush Ginekol 2015; 54: 21-27. (in Bulgarian)
3. Manchanda R., Sharma R. Complications of hysteroscopy and management. In: Tandulwadkar S., Pal B. Hysteroscopy simplified by masters. Singapore: Springer; 2021. [DOI:10.1007/978-981-15-2505-6_26]
4. Kotdawala P, Kotdawala S, Nagar N. Evaluation of endometrium in peri-menopausal abnormal uterine bleeding. J Midlife Health 2013; 4: 16-21. [DOI:10.4103/0976-7800.109628] [PMID] [PMCID]
5. Gupta S. Complications of hysteroscopy. In: Jain S, Amdar D. Manual of fertility enhancing hysteroscopy. Singapore: Springer; 2018. [DOI:10.1007/978-981-10-8028-9_12] [PMCID]
6. Levine LD. Cervical ripening: Why we do what we do. Semin Perinatol 2020; 44: 151216. [DOI:10.1016/j.semperi.2019.151216] [PMID]
7. De Silva PM, Wilson L, Carnegy A, Smith PP, Clark TJ. Cervical dilatation and preparation prior to outpatient hysteroscopy: A systematic review and meta-analysis. BJOG 2021; 128: 1112-1123. [DOI:10.1111/1471-0528.16604] [PMID]
8. Cunningham FG, Leveno KJ, Bloom SL, Dashe JS, Hoffman BL, Casey BM, et al. Williams Obstetrics. 25th Ed. New York: McGraw Hill Education; 2014.
9. Choo SN, Kanneganti A, Abdul Aziz MNDB, Loh L, Hargreaves C, Gopal V, et al. Mechanical Dilatation of the cervix in a scarred uterus (MEDICS): The study protocol of a randomised controlled trial comparing a single cervical catheter balloon and prostaglandin PGE2 for cervical ripening and labour induction following caesarean delivery. BMJ Open 2019; 9: e028896. [DOI:10.1136/bmjopen-2019-028896] [PMID] [PMCID]
10. Rund NMA, El Shenoufy H, Islam BA, El Husseiny T, Nassar SA, Mohsen RA, et al. Determining the optimal time interval between vaginal dinoprostone administration and diagnostic office hysteroscopy in nulliparous women: A randomized, double-blind trial. J Minim Invasive Gynecol 2022; 29: 85-93. [DOI:10.1016/j.jmig.2021.06.021] [PMID]
11. Handa VL, Van Le L. Te Linde's operative gynecology. 12th Ed. Philadelphia: Lippincott Williams and Wilkins; 2020: 255-273.
12. Munro MG, Parker WH. Gynecologic Endoscopy. In: Berek JS. Berek & Novak's gynecology. 16th Ed. Philadelphia: Lippincott Williams and Wilkins; 2019: 595-653.
13. Campo R, Santangelo F, Gordts S, Di Cesare C, Van Kerrebroeck H, De Angelis MC, et al. Outpatient hysteroscopy. Facts Views Visn ObGyn 2018; 10: 115-122.
14. Hagen N, Khuluza F, Heide L. Quality, availability and storage conditions of oxytocin and misoprostol in Malawi. BMC Pregnancy Childbirth 2020; 20: 184. [DOI:10.1186/s12884-020-2810-9] [PMID] [PMCID]
15. Nakano FY, Yela DA, Pinto JPL, Riegas T, Benetti-Pinto CL, Pedro AO, et al. Efficacy of misoprostol before diagnostic hysteroscopy in menopausal women: A randomized clinical trial. Menopause 2018; 25: 789-794. [DOI:10.1097/GME.0000000000001074] [PMID]
16. Timoszuk M, Bielawska K, Skrzydlewska E. Evening primrose (Oenothera biennis) biological activity dependent on chemical composition. Antioxidants 2018; 7: 108. [DOI:10.3390/antiox7080108] [PMID] [PMCID]
17. Nikoomazhab S, Haghdoust MR, Honarmandpour A. [The effect of evening primrose oil on duration of postpartum blues among primiparous women: A double-blind, randomized controlled clinical trial]. Iran J Obstet Gynecol Infertil 2017; 20: 64-73. (in Persian)
18. Mahady GB, Fong HHS, Farnsworth NR. Botanical dietary supplements. 1st Ed. USA: CRC Press; 2001.
19. Lee SM, Kim HS, Park HJ, Oh KY, Kim JY, Lee SH, et al. Comparison of antioxidant properties of evening primrose seeds by different processing methods, and physiological properties of evening primrose seed powder. Prev Nutr Food Sci 2020; 25: 422-431. [DOI:10.3746/pnf.2020.25.4.422] [PMID] [PMCID]
20. Fecker R, Buda V, Alexa E, Avram S, Pavel IZ, Muntean D, et al. Phytochemical and biological screening of Oenothera biennis L. hydroalcoholic extract. Biomolecules 2020; 10: 818. [DOI:10.3390/biom10060818] [PMID] [PMCID]
21. Pan F, Li Y, Luo X, Wang X, Wang C, Wen B, et al. Effect of the chemical refining process on composition and oxidative stability of evening primrose oil. J Food Proc Preserv 2020; 44: e14800. [DOI:10.1111/jfpp.14800]
22. Freitas HR, Isaac AR, Malcher-Lopes R, Diaz BL, Trevenzoli IH, de Melo Reis RA. Polyunsaturated fatty acids and endocannabinoids in health and disease. Nutr Neurosci 2018; 21: 695-714. [DOI:10.1080/1028415X.2017.1347373] [PMID]
23. Diansuy NN, Aguilar AS. The effectiveness of evening primrose oil gel capsule as a cervical ripening agent during labor induction as measured by bishop score on term singleton pregnant patients. Philippine J Obstet Gynecol 2017; 41: 1-4.
24. Moradi M, Niazi A, Heydarian Miri H, Lopez V. The effect of evening primrose oil on labor induction and cervical ripening: A systematic review and meta‐analysis. Phytother Res 2021; 35: 5374-5383. [DOI:10.1002/ptr.7147] [PMID]
25. 25 Bahmani S, Hesamy K, Shahgheibi S, Roshani D, Shahoei R. Comparison of the effect of vaginal capsule of evening primrose oil and misoprostol on cervical ripening of nulliparous women with post-term pregnancy. J Pharmaceutical Res Int 2019; 26: 47396. [DOI:10.9734/jpri/2019/v26i330140]
26. Kalati M, Kashanian M, Jahdi F, Naseri M, Haghani H, Sheikhansari N. Evening primrose oil and labour, is it effective? A randomised clinical trial. J Obstet Gynaecol 2018; 38: 488-492. [DOI:10.1080/01443615.2017.1386165] [PMID]
27. Tanchoco ML, Aguilar AS. Cervical priming prior to operative hysteroscopy: A randomized controlled study comparing the efficacy of laminaria versus evening primrose oil (EPO). J Minim Invasive Gynecol 2015; 22: S45. [DOI:10.1016/j.jmig.2015.08.122] [PMID]
28. Vahdat M, Tahermanesh K, Mehdizadeh Kashi A, Ashouri M, Solaymani Dodaran M, Kashanian M, et al. Evening primrose oil effect on the ease of cervical ripening and dilatation before operative hysteroscopy. Thrita 2015; 4: e29876. [DOI:10.5812/thrita.29876]
29. Nouri B, Baghestani AR, Pooransari P. Evening primrose versus misoprostol for cervical dilatation before gynecologic surgeries: A double-blind randomized clinical trial. J Obstet Gynecol Cancer Res 2021; 6: 87-94. [DOI:10.30699/jogcr.6.2.87]
30. Mahboubi M. Evening primrose (Oenothera biennis) oil in management of female ailments. J Menopausal Med 2019; 25: 74-82. [DOI:10.6118/jmm.18190] [PMID] [PMCID]
31. Maddineshat M, Keyvanloo S, Lashkardoost H, Arki M, Tabatabaeichehr M. Effectiveness of group cognitive-behavioral therapy on symptoms of premenstrual syndrome (PMS). Iran J Psychiatry 2016; 11: 30-36.
32. Zand Vakili F, Zare SH, Rahimi K, Riahi M. [The effect of evening primrose oil on changes in polycystic ovary syndrome induced by estradiol valerate in Rat]. Armaghane Danesh 2018; 22: 714-724. (in Persian)
33. 33 Faghani Aghoozi M, Fayazi S, Mohammadi S, Tehranian N, Amerian M. The effects of evening primerose on clinical obstetrics of Iran: A review study. Sci J Nurs Midwifery Paramed Faculty 2019; 5: 15-28.
34. Tanchoco M, Aguilar AS. Cervical priming prior to operative hysteroscopy: A randomized controlled study comparing the efficacy of laminaria versus evening primrose oil (EPO). J Minim Invasive Gynecol 2015; 22: S45. [DOI:10.1016/j.jmig.2015.08.122] [PMID]
35. Carreon GA, Tanangonan GG. Cervical priming prior to operative hystroscopy: A randomized clinical trial comparing evening primrose oil versus dinoprostone gel. J Menopausal Med 2012; 9: 74-81.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |