Wed, Jan 28, 2026
[Archive]
Volume 22, Issue 3 (March 2024)
IJRM 2024, 22(3): 229-234 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ganikyzy Shaimerdenova G, Narkenovna Abuova G, Nalibekkyzy Kulbayeva S. Features of the course of severe and critical COVID-19 in pregnant women: A prospective cross-sectional study. IJRM 2024; 22 (3) :229-234
URL: http://ijrm.ir/article-1-2756-en.html
URL: http://ijrm.ir/article-1-2756-en.html
1- South Kazakhstan Medical Academy, Shymkent, Kazakhstan. , gulbanu1008@mail.ru
2- South Kazakhstan Medical Academy, Shymkent, Kazakhstan.
2- South Kazakhstan Medical Academy, Shymkent, Kazakhstan.
Full-Text [PDF 320 kb]
(841 Downloads)
| Abstract (HTML) (965 Views)
1. Introduction
The 21st century began with a fundamental revision of the epidemic and pandemic potential of betacoronaviruses, which required the immediate deployment of a system of control as deep as for influenza, starting from the natural reservoir-bats (chiroptera, microchiroptera) to the organization of preventive and anti-epidemic measures (1). As a result, by December 2019, 6 representatives of the Coronaviridae family were known to humankind among 40 viruses.
The coronavirus disease 2019 (COVID-19) epidemic led to the discovery of the 7th human coronavirus (2, 3). According to statistics, as of October 17, 2022, there were 629,959,595 people with COVID-19 coronavirus infection worldwide, with 6,571,489 deaths. In the Republic of Kazakhstan, 139,287 were registered, with 13,692 deaths (4). At the same time, 38,149 cases were registered in the city of Shymkent, Kazakhstan of which 1646 were pregnant for 2020-2022; 537 in 2020, 892 in 2021, and 217 women in 2022 (5).
According to recent studies, the risk of progression to severe disease in pregnant women was higher than in non-pregnant women (6-8). It should be noted that in pregnant women, the factors for the transition to a severe form are concomitant diseases of the cardiovascular system (arterial hypertension, chronic heart failure, concomitant respiratory chronic diseases, fibrotic changes in the lungs); endocrinopathies (diabetes mellitus, metabolic syndrome), obesity (body mass index > 40), and others; immunodeficiency states (oncological, hematological diseases); other severe chronic diseases (chronic kidney disease, liver disease, etc.) (9). The age group from 33-42 yr and the period from 22-36 wk of pregnancy also aggravate the course of COVID-19 (10). Severe infection is observed in 15% of patients, critical in 5%, mild and moderate in 80% which, according to the World Health Organization, is close to population indicators (11).
We studied the frequency and spectrum of complications, as well as the outcomes of pregnant women, the timing of the onset of COVID-19 complications, timely seeking medical help, and the risk of developing critical forms in case of late treatment. We detected the early onset of complications and timely identification of risk groups for severe and critical courses for early diagnosis and prescribed treatment, in a timely manner. Therefore, this study aimed to investigate the patterns of coronavirus COVID-19 infection in pregnant women.
2. Materials and Methods
2.1. Setting
This prospective cross-sectional study compared the medical records of 120 pregnant women with severe and very severe COVID-19 treated at the Infectious Disease Center, Shymkent, Kazakhstan from December 2021 to May 2022. Factors such as time of hospital admission, hospitalization period, maternal comorbidities, age, pregnancy and postpartum complications, pregnancy outcomes, and treatment type were analyzed.
Women aged from 18-49 yr entered the study during COVID-19 and were followed up for 9 months.
The severity criteria included dyspnoea with slight exertion, when talking, at rest, respiratory rate 23-30 per min, resting SpO2 < 92% with room air breathing, and persistent lymphopenia.
2.2. Participants
Pregnant women with confirmed, severe, and critical COVID-19 infection; receiving treatment in infectious diseases hospitals of Shymkent city in 2020-2021; those who were independent from race and nationality; and the women of reproductive age were included in the study. Any condition incompatible with the study treatment (pregnancy without severe and critical COVID-19); mild to moderate severity of COVID-19 in pregnant women, absence of pregnancy, women of non-reproductive age, receiving treatment in non-infectious hospitals in Shymkent city, Kazakhstan in 2020-2021 were excluded from the study.
2.3. Sample size
A confidence level of 95% and a power of 80% were considered to determine the sample size. We used G.power software (version 3.1) and was designed for 120 patients.
2.4. Outcome
There is a risk of disease progression to severe and critical COVID-19 in pregnant women older than 33 yr of age and at 28-40 wk gestation. Early referral to a doctor in hospital, timely hospitalization, and initiated treatment may reduce the risk of aggravation of the patient’s condition and development of formidable complications.
2.5. Ethical considerations
The Local Bioethical Committee of South Kazakhstan Medical Academy, Shymkent, Kazakhstan, approved the study proposal (Code: 044-65/) (12).
2.6. Statistical analysis
The normality of the distribution was tested according to Kolmogorov-Smirnov with the correction of Lillifors and Shapiro-Wilk. Because all data showed normal and non-normal distributions, the mean, standard deviation, median confidence interval, and interquartile range were subsequently used (13). Categorical variables are presented as absolute numbers, percentages, and frequencies. A p < 0.05 was considered statistically significant. The obtained data were processed using the IBM SPSS Statistics program (version 26.0, SPSS Inc Chicago, IL, USA). Nominal variables were analyzed using the Mann-Whitney, Pearson's Chi-square, and Fisher's exact tests.
3. Results
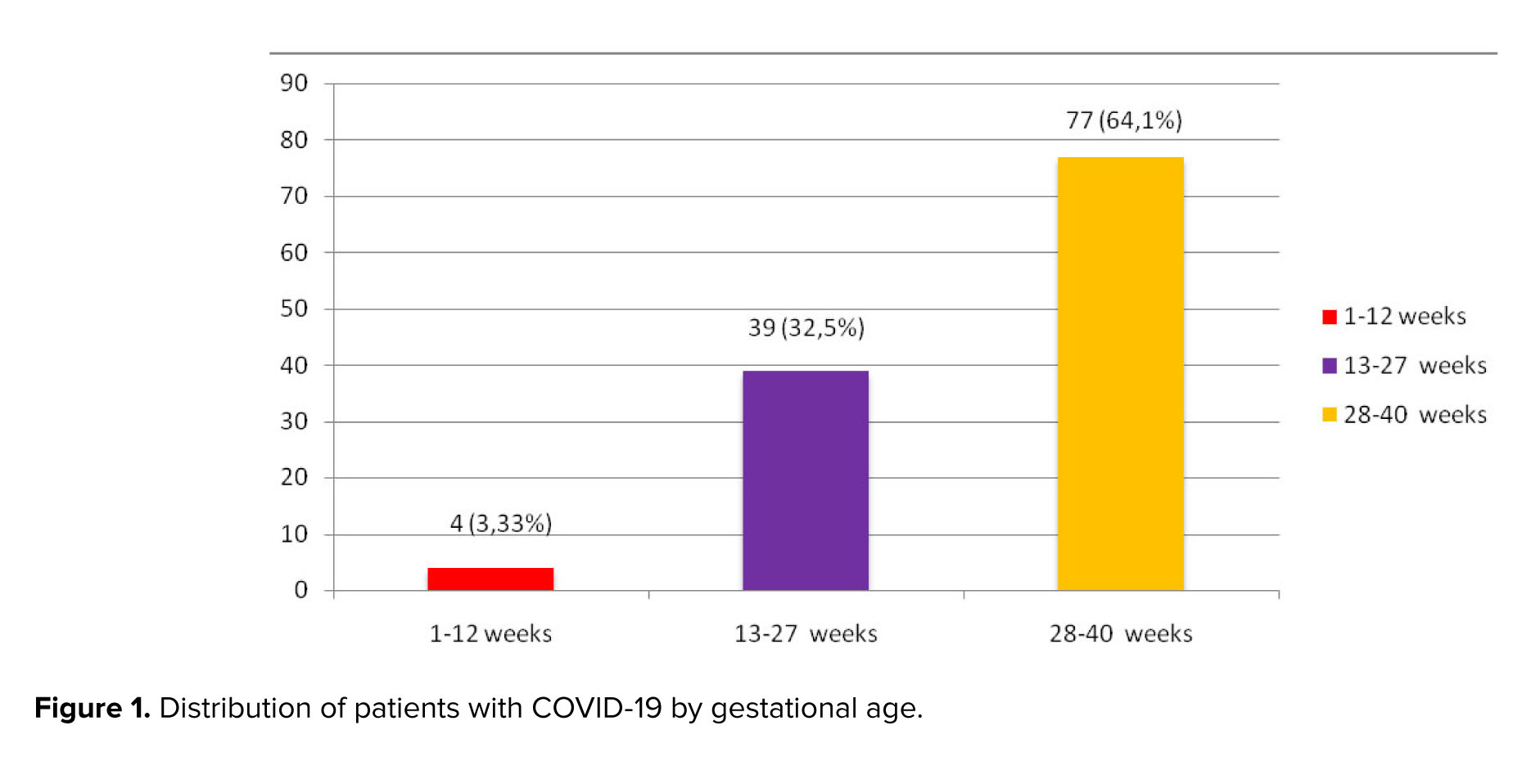
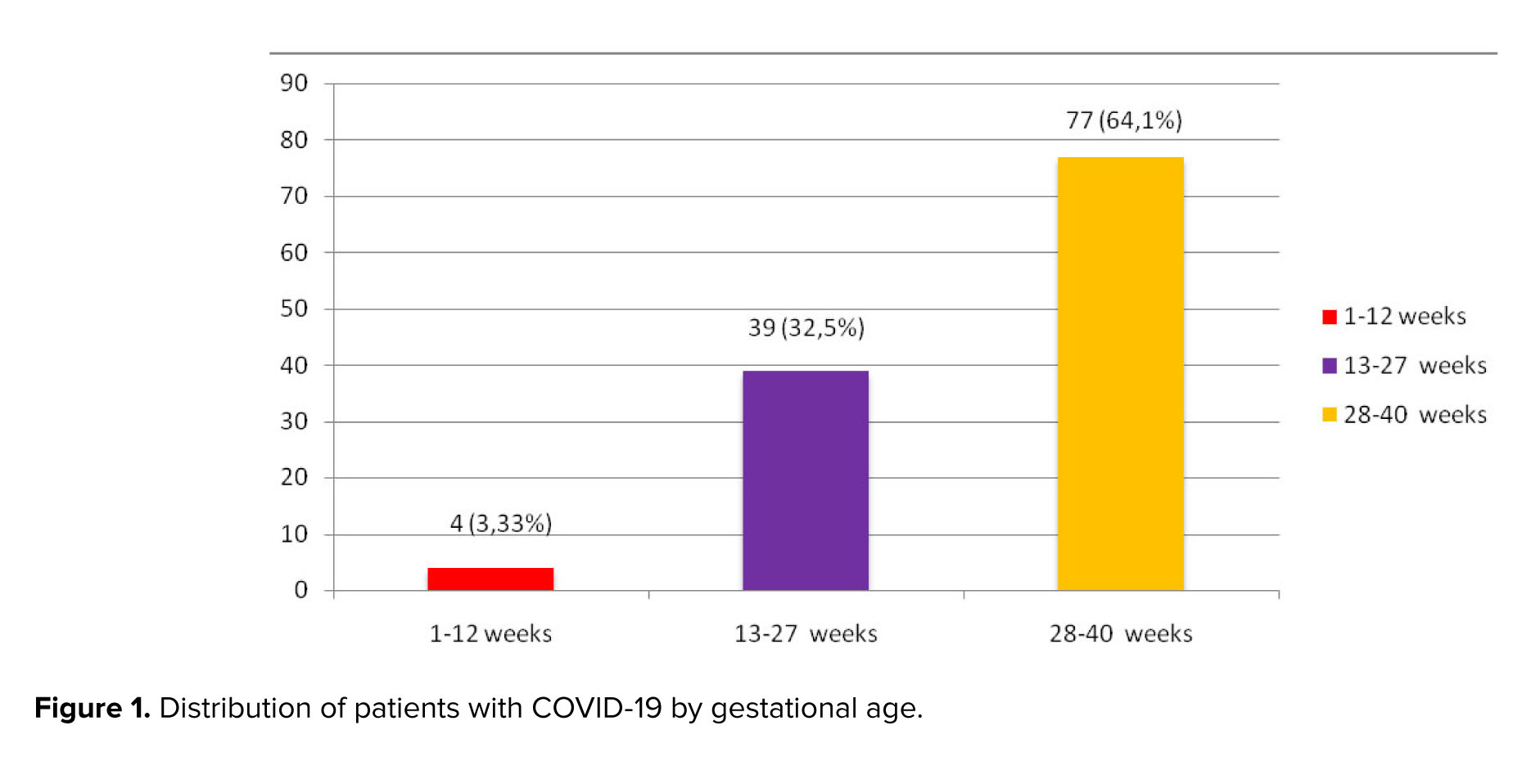
The study included 87 (72.5%) women with severe COVID-19 and 33 (27.5%) pregnant women with a highly severe form of COVID-19. 4 (3.33%) women were in 1st, 39 (32.5%) in 2nd, and 77 (64.1%) were in the 3rd trimester of pregnancy (Figure 1). Consequently, most women were hospitalized in the 3rd trimester.
When comparing the birth parity of the subjects, depending on the gestational age we got next data: in 1-12 wk (3.75 ± 0.95). In the period of 13-27 wk 3.00 (Q1-Q3: 2.00-4.00), at 28-40 wk 3.00 (Q1-Q3: 2.00-4.00). Analysis of birth parity showed that the most common indications for hospitalization are the presence of 3 or more pregnancies. This confirms the availability of severe courses of COVID-19 in multiparous women.
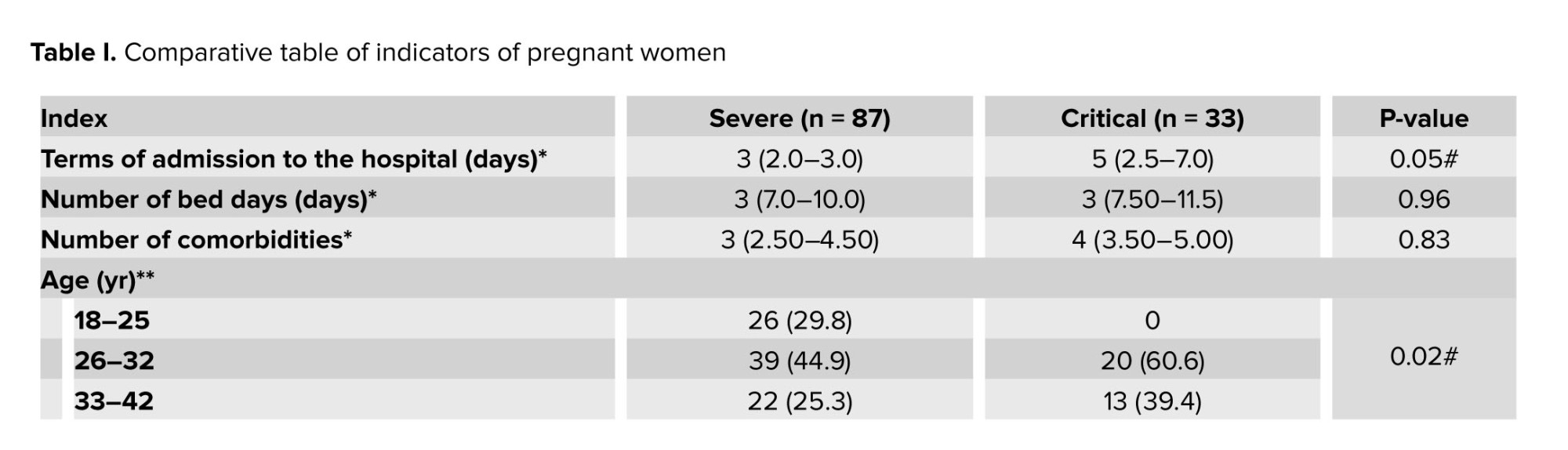
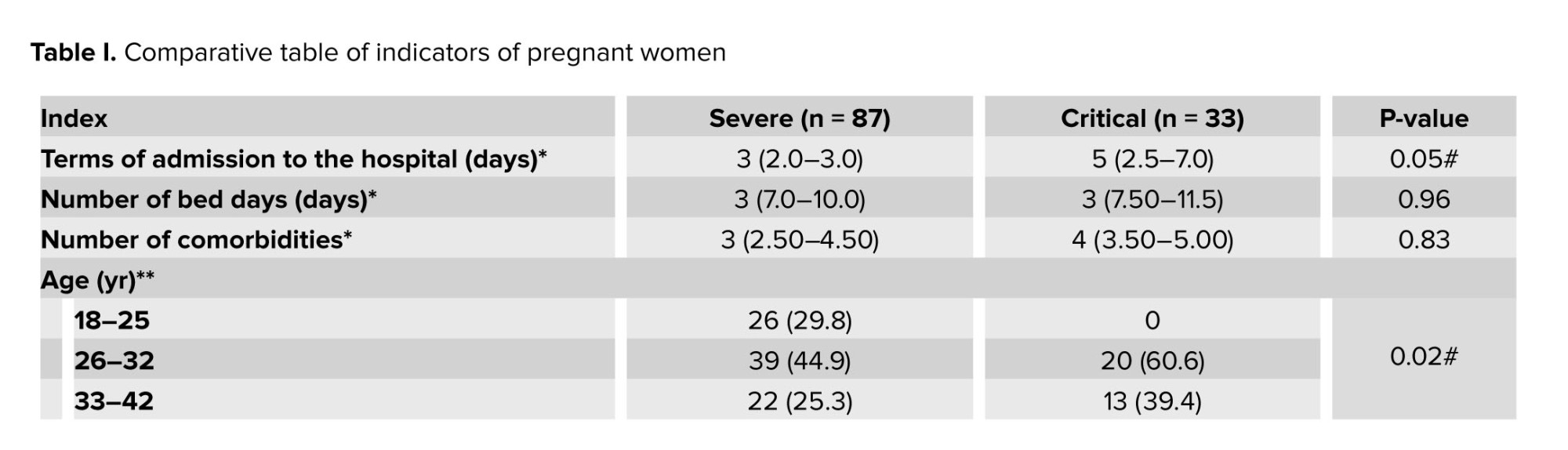
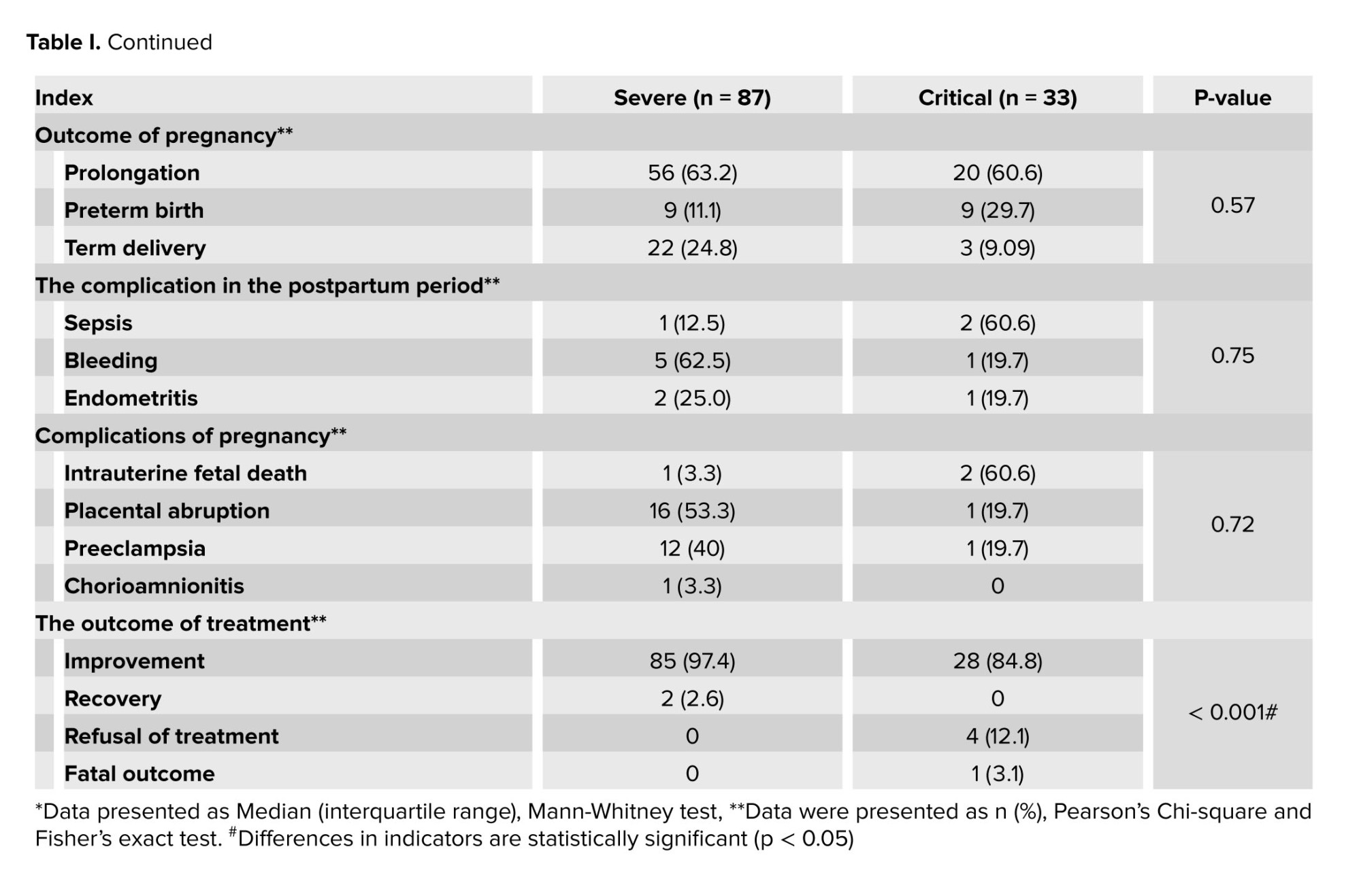
We studied the following indicators, admission and hospitalization time, the number of comorbidities, age in admission time, complications of pregnancy and the postpartum period, pregnancy outcomes, and treatment (Table I).
When comparing patients with severe and critical forms of COVID-19, depending on the time of admission to the hospital, statistically significant differences were obtained (p = 0.05). Women with a critical form of COVID-19 infection were admitted to a medical facility later than pregnant women with a severe form. Analysis of the age of pregnant women showed statistically significant differences (p = 0.02) in severe form. The study found that pregnant women in the 18-25 age group had only 26 case of severe COVID-19 (26 [29.8]). Older age groups dominated the critical group. Older pregnant women are more likely to progress to a more severe form of COVID-19. The relationship between the compared features was medium (V = 0.270).
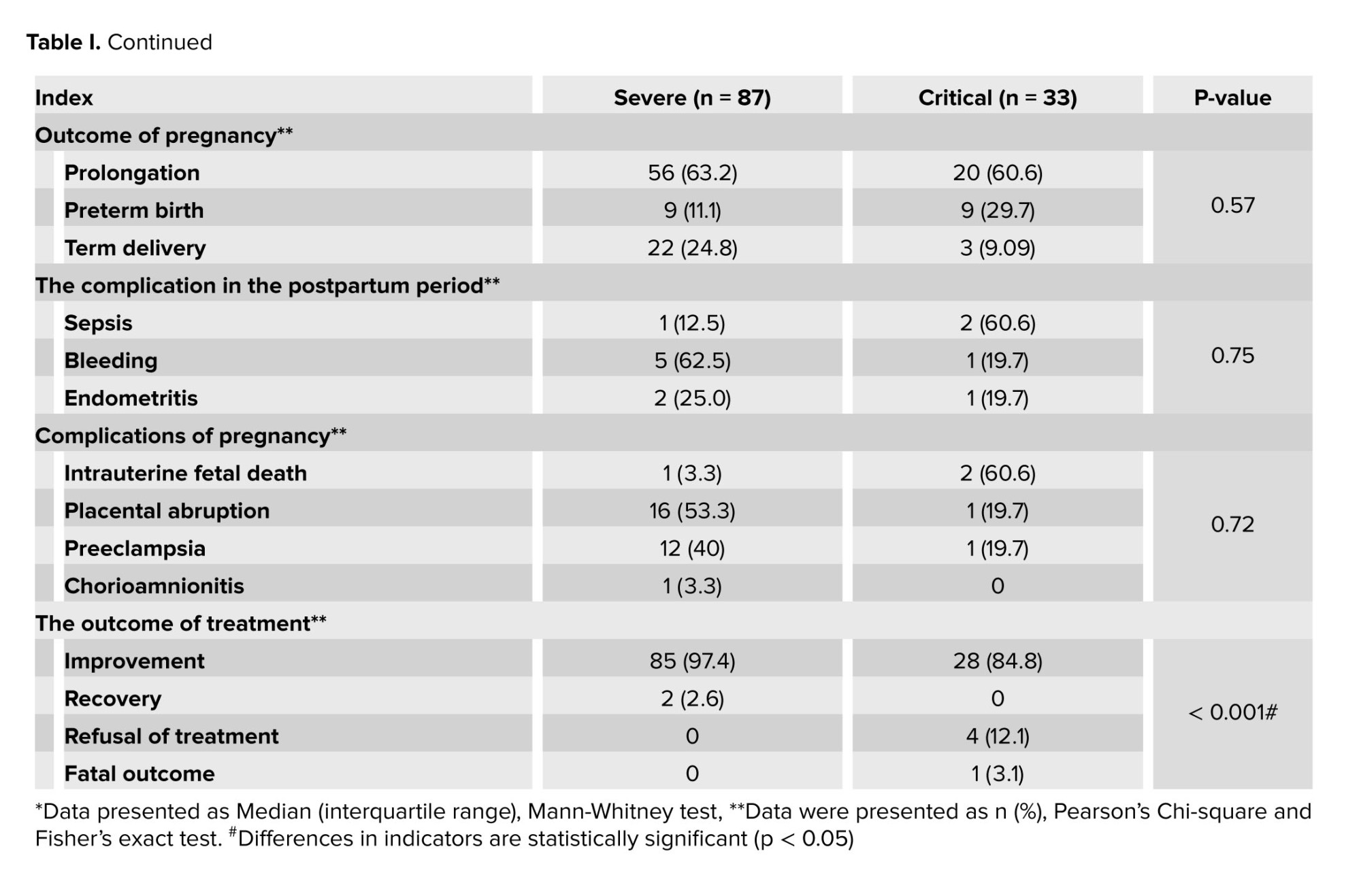
In the results of outcomes and pregnancy complications, no statistical significance (p = 0.06) was observed in the outcomes of the postpartum period. However, it should be noted that there were 18 cases of premature births. More than half of pregnancy complications were due to placental abruption, 17 cases. There were also 3 cases of intrauterine fetal death. During the study in the postpartum period, 6 cases of bleeding and 3 cases of sepsis were observed. A fatal case occurred in a pregnant woman with a highly severe form of COVID-19.
4. Discussion
The study included 87 (72.5%) women with a severe COVID-19 infection and 33 pregnant women with a highly severe form (27.5%). The following data were obtained, when comparing the pregnancy parity of the subjects, depending on the gestational age: in the 1-12 wk period, the indicator was 3.75 ± 0.95. In 13-27 wk 3.00 (Q1-Q3: 2.00-4.00), in 28-40 wk 3.00 (Q1-Q3: 2.00-4.00). The number of bed days spent in the hospital ranged from one to 23 days.
COVID-19 is an urgent problem around the world. Increased susceptibility to respiratory disease and severe pneumonia in pregnant women leads to severe hospitalization in intensive care units and mechanical ventilation (14-17). Pregnant women are characterized by a decrease in the immune response and other physiological changes during gestation, which is the cause of the above process. The severity of COVID-19 is associated with the entry of the virus into host cells after binding to angiotensin-converting enzyme 2. It should be noted that angiotensin-converting enzyme 2 replicates on cell membranes, which in turn has the property of being tropic to the placenta throughout the entire period of pregnancy. This phenomenon is a possible etiology of the susceptibility of pregnant women to COVID-19 (15-18). All these changes in a pregnant woman's body suggest a greater vulnerability to COVID-19 than other population categories.
It should be noted that most of the sick women in the gestation period of 28-40 wk. These patients is associated with an increasing load on the mother's body due to a sharp increase in the weight of the fetus. Increasing in the load on the cardiovascular and respiratory system of the mother and the needs rapidly growing fetus in this period of pregnancy. Multiparous patients were hospitalized more often than primiparas. Women with a severe form of COVID-19 were hospitalized later than pregnant women with a severe condition. Also, the older age group is a risk factor for transitioning to a more severe form of the disease. Comorbidities affect the prognosis of acute illness and an increased risk of severe symptoms. About 70% of patients requiring treatment in the intensive care unit have comorbidities (17-19). This was also confirmed in our study.
One limitation is that this study carried out in single center that does not provide extended results. Also the sample size was relatively small.
5. Conclusion
Thus, our study showed that a more severe coronavirus infection occurs in women with more than 3 pregnancies. In addition, pregnant women older than 33 yr and in 28-40 wk have a risk of transitioning to a severe form of the disease. Also, earlier treatment for inpatient care reduces the risk of aggravating the patient's condition.
Data availability
The data that support the findings of this study are available on a reasonable request from the corresponding author.
Author contributions
Gulbanu Ganikyzy Shaimerdenova: concept and design had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, statistical analysis, drafting of the manuscript, and supervision. Gulzhan Narkenovna Abuova: drafting of the manuscript, critical revision of the manuscript for important intellectual content. Saltanat Kulbayeva Nalibekkyzy: critical revision of the manuscript for important intellectual content, acquisition, analysis, or interpretation of data, and drafting of the manuscript. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
This article was financially supported by South Kazakhstan Medical Academy, Shymkent, Kazakhstan (Grant number: 10391). The authors thank Gasparyan Armen for his helpful comments on the manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest.
Full-Text: (199 Views)
1. Introduction
The 21st century began with a fundamental revision of the epidemic and pandemic potential of betacoronaviruses, which required the immediate deployment of a system of control as deep as for influenza, starting from the natural reservoir-bats (chiroptera, microchiroptera) to the organization of preventive and anti-epidemic measures (1). As a result, by December 2019, 6 representatives of the Coronaviridae family were known to humankind among 40 viruses.
The coronavirus disease 2019 (COVID-19) epidemic led to the discovery of the 7th human coronavirus (2, 3). According to statistics, as of October 17, 2022, there were 629,959,595 people with COVID-19 coronavirus infection worldwide, with 6,571,489 deaths. In the Republic of Kazakhstan, 139,287 were registered, with 13,692 deaths (4). At the same time, 38,149 cases were registered in the city of Shymkent, Kazakhstan of which 1646 were pregnant for 2020-2022; 537 in 2020, 892 in 2021, and 217 women in 2022 (5).
According to recent studies, the risk of progression to severe disease in pregnant women was higher than in non-pregnant women (6-8). It should be noted that in pregnant women, the factors for the transition to a severe form are concomitant diseases of the cardiovascular system (arterial hypertension, chronic heart failure, concomitant respiratory chronic diseases, fibrotic changes in the lungs); endocrinopathies (diabetes mellitus, metabolic syndrome), obesity (body mass index > 40), and others; immunodeficiency states (oncological, hematological diseases); other severe chronic diseases (chronic kidney disease, liver disease, etc.) (9). The age group from 33-42 yr and the period from 22-36 wk of pregnancy also aggravate the course of COVID-19 (10). Severe infection is observed in 15% of patients, critical in 5%, mild and moderate in 80% which, according to the World Health Organization, is close to population indicators (11).
We studied the frequency and spectrum of complications, as well as the outcomes of pregnant women, the timing of the onset of COVID-19 complications, timely seeking medical help, and the risk of developing critical forms in case of late treatment. We detected the early onset of complications and timely identification of risk groups for severe and critical courses for early diagnosis and prescribed treatment, in a timely manner. Therefore, this study aimed to investigate the patterns of coronavirus COVID-19 infection in pregnant women.
2. Materials and Methods
2.1. Setting
This prospective cross-sectional study compared the medical records of 120 pregnant women with severe and very severe COVID-19 treated at the Infectious Disease Center, Shymkent, Kazakhstan from December 2021 to May 2022. Factors such as time of hospital admission, hospitalization period, maternal comorbidities, age, pregnancy and postpartum complications, pregnancy outcomes, and treatment type were analyzed.
Women aged from 18-49 yr entered the study during COVID-19 and were followed up for 9 months.
The severity criteria included dyspnoea with slight exertion, when talking, at rest, respiratory rate 23-30 per min, resting SpO2 < 92% with room air breathing, and persistent lymphopenia.
2.2. Participants
Pregnant women with confirmed, severe, and critical COVID-19 infection; receiving treatment in infectious diseases hospitals of Shymkent city in 2020-2021; those who were independent from race and nationality; and the women of reproductive age were included in the study. Any condition incompatible with the study treatment (pregnancy without severe and critical COVID-19); mild to moderate severity of COVID-19 in pregnant women, absence of pregnancy, women of non-reproductive age, receiving treatment in non-infectious hospitals in Shymkent city, Kazakhstan in 2020-2021 were excluded from the study.
2.3. Sample size
A confidence level of 95% and a power of 80% were considered to determine the sample size. We used G.power software (version 3.1) and was designed for 120 patients.
2.4. Outcome
There is a risk of disease progression to severe and critical COVID-19 in pregnant women older than 33 yr of age and at 28-40 wk gestation. Early referral to a doctor in hospital, timely hospitalization, and initiated treatment may reduce the risk of aggravation of the patient’s condition and development of formidable complications.
2.5. Ethical considerations
The Local Bioethical Committee of South Kazakhstan Medical Academy, Shymkent, Kazakhstan, approved the study proposal (Code: 044-65/) (12).
2.6. Statistical analysis
The normality of the distribution was tested according to Kolmogorov-Smirnov with the correction of Lillifors and Shapiro-Wilk. Because all data showed normal and non-normal distributions, the mean, standard deviation, median confidence interval, and interquartile range were subsequently used (13). Categorical variables are presented as absolute numbers, percentages, and frequencies. A p < 0.05 was considered statistically significant. The obtained data were processed using the IBM SPSS Statistics program (version 26.0, SPSS Inc Chicago, IL, USA). Nominal variables were analyzed using the Mann-Whitney, Pearson's Chi-square, and Fisher's exact tests.
3. Results
The study included 87 (72.5%) women with severe COVID-19 and 33 (27.5%) pregnant women with a highly severe form of COVID-19. 4 (3.33%) women were in 1st, 39 (32.5%) in 2nd, and 77 (64.1%) were in the 3rd trimester of pregnancy (Figure 1). Consequently, most women were hospitalized in the 3rd trimester.
When comparing the birth parity of the subjects, depending on the gestational age we got next data: in 1-12 wk (3.75 ± 0.95). In the period of 13-27 wk 3.00 (Q1-Q3: 2.00-4.00), at 28-40 wk 3.00 (Q1-Q3: 2.00-4.00). Analysis of birth parity showed that the most common indications for hospitalization are the presence of 3 or more pregnancies. This confirms the availability of severe courses of COVID-19 in multiparous women.
We studied the following indicators, admission and hospitalization time, the number of comorbidities, age in admission time, complications of pregnancy and the postpartum period, pregnancy outcomes, and treatment (Table I).
When comparing patients with severe and critical forms of COVID-19, depending on the time of admission to the hospital, statistically significant differences were obtained (p = 0.05). Women with a critical form of COVID-19 infection were admitted to a medical facility later than pregnant women with a severe form. Analysis of the age of pregnant women showed statistically significant differences (p = 0.02) in severe form. The study found that pregnant women in the 18-25 age group had only 26 case of severe COVID-19 (26 [29.8]). Older age groups dominated the critical group. Older pregnant women are more likely to progress to a more severe form of COVID-19. The relationship between the compared features was medium (V = 0.270).
In the results of outcomes and pregnancy complications, no statistical significance (p = 0.06) was observed in the outcomes of the postpartum period. However, it should be noted that there were 18 cases of premature births. More than half of pregnancy complications were due to placental abruption, 17 cases. There were also 3 cases of intrauterine fetal death. During the study in the postpartum period, 6 cases of bleeding and 3 cases of sepsis were observed. A fatal case occurred in a pregnant woman with a highly severe form of COVID-19.
4. Discussion
The study included 87 (72.5%) women with a severe COVID-19 infection and 33 pregnant women with a highly severe form (27.5%). The following data were obtained, when comparing the pregnancy parity of the subjects, depending on the gestational age: in the 1-12 wk period, the indicator was 3.75 ± 0.95. In 13-27 wk 3.00 (Q1-Q3: 2.00-4.00), in 28-40 wk 3.00 (Q1-Q3: 2.00-4.00). The number of bed days spent in the hospital ranged from one to 23 days.
COVID-19 is an urgent problem around the world. Increased susceptibility to respiratory disease and severe pneumonia in pregnant women leads to severe hospitalization in intensive care units and mechanical ventilation (14-17). Pregnant women are characterized by a decrease in the immune response and other physiological changes during gestation, which is the cause of the above process. The severity of COVID-19 is associated with the entry of the virus into host cells after binding to angiotensin-converting enzyme 2. It should be noted that angiotensin-converting enzyme 2 replicates on cell membranes, which in turn has the property of being tropic to the placenta throughout the entire period of pregnancy. This phenomenon is a possible etiology of the susceptibility of pregnant women to COVID-19 (15-18). All these changes in a pregnant woman's body suggest a greater vulnerability to COVID-19 than other population categories.
It should be noted that most of the sick women in the gestation period of 28-40 wk. These patients is associated with an increasing load on the mother's body due to a sharp increase in the weight of the fetus. Increasing in the load on the cardiovascular and respiratory system of the mother and the needs rapidly growing fetus in this period of pregnancy. Multiparous patients were hospitalized more often than primiparas. Women with a severe form of COVID-19 were hospitalized later than pregnant women with a severe condition. Also, the older age group is a risk factor for transitioning to a more severe form of the disease. Comorbidities affect the prognosis of acute illness and an increased risk of severe symptoms. About 70% of patients requiring treatment in the intensive care unit have comorbidities (17-19). This was also confirmed in our study.
One limitation is that this study carried out in single center that does not provide extended results. Also the sample size was relatively small.
5. Conclusion
Thus, our study showed that a more severe coronavirus infection occurs in women with more than 3 pregnancies. In addition, pregnant women older than 33 yr and in 28-40 wk have a risk of transitioning to a severe form of the disease. Also, earlier treatment for inpatient care reduces the risk of aggravating the patient's condition.
Data availability
The data that support the findings of this study are available on a reasonable request from the corresponding author.
Author contributions
Gulbanu Ganikyzy Shaimerdenova: concept and design had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, statistical analysis, drafting of the manuscript, and supervision. Gulzhan Narkenovna Abuova: drafting of the manuscript, critical revision of the manuscript for important intellectual content. Saltanat Kulbayeva Nalibekkyzy: critical revision of the manuscript for important intellectual content, acquisition, analysis, or interpretation of data, and drafting of the manuscript. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
This article was financially supported by South Kazakhstan Medical Academy, Shymkent, Kazakhstan (Grant number: 10391). The authors thank Gasparyan Armen for his helpful comments on the manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Pregnancy Health
References
1. Hui DS, Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health: The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis 2020; 91: 264-266. [DOI:10.1016/j.ijid.2020.01.009] [PMID] [PMCID]
2. World Health Organization. Novel coronavirus (2019-nCoV). Situation report 22. Available at: https://www.who.int/ docs/default-source/coronaviruse/situation-reports/20200211-sitrep-22-ncov.pdf?sfvrsn=fb6d49b1_2. 11 February 2020.
3. Shchelkanov MY, Popova AY, Dedkov VG, Akimkin VG, Maleev VV. [The history of investigation and modern classification of coronaviruses (Nidovirales: Coronaviridae)]. Russian J Infect Immun 2020; 10: 221-246. (In Russian) [DOI:10.15789/2220-7619-HOI-1412]
4. Estimated cumulative excess deaths per 100,000 people during COVID-19. Available at: https://ourworldindata.org/explorers/coronavirus-data-explorer 07/16/2022.
5. Data of the committee for sanitary and epidemiological control of the city of Shymkent, 2022. Available at: https://www.gov.kz/memleket/entities/departament-kkbtu-shymkent?lang=ru 07/16/2022.
6. Elshafeey F, Magdi R, Hindi N, Elshebiny M, Farrag N, Mahdy S, et al. A systematic scoping review of COVID‐19 during pregnancy and childbirth. Int J Gynecol Obstet 2020; 150: 47-52. [DOI:10.1002/ijgo.13182] [PMID] [PMCID]
7. Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, et al. Perinatal transmission of 2019 coronavirus Disease: Associated severe acute respiratory syndrome coronavirus 2: Should we worry? Clin Infect Dis 2021; 72: 862-864. [DOI:10.1093/cid/ciaa226] [PMID] [PMCID]
8. Joseph NT, Collier AY. COVID-19 therapeutics and considerations for pregnancy. Obstet Gynecol Clin North Am 2023; 50: 163-182. [DOI:10.1016/j.ogc.2022.10.018] [PMID] [PMCID]
9. Shaimerdenova GG, Abuova GN, Saltanat S, Baimbetova S, Aidana A. Remdesevir antiviral therapy in pregnant women with COVID-19. Arch Clin Infect Dis 2023; 18: e132803. [DOI:10.5812/archcid-132803]
10. Moore CA, Staples JE, Dobyns WB, Pessoa A, Ventura CV, Da Fonseca EB, et al. Characterizing the pattern of anomalies in congenital Zika syndrome for pediatric clinicians. JAMA Pediatr 2017; 171: 288-295. [DOI:10.1001/jamapediatrics.2016.3982] [PMID] [PMCID]
11. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr 2020; 9: 51-60. [DOI:10.21037/tp.2020.02.06] [PMID] [PMCID]
12. Mehta P, Zimba O, Gasparyan AY, Seiil B, Yessirkepov M. Ethics committees: Structure, roles, and issues. J Korean Med Sci 2023; 38: e198. [DOI:10.3346/jkms.2023.38.e198] [PMID] [PMCID]
13. Misra DP, Zimba O, Gasparyan AY. Statistical data presentation: A primer for rheumatology researchers. Rheumatol Int 2021; 41: 43-55. [DOI:10.1007/s00296-020-04740-z] [PMID]
14. Kumar D, Verma S, Mysorekar IU. COVID-19 and pregnancy: Clinical outcomes; mechanisms, and vaccine efficacy. Transl Res 2022; 251: 84-95. [DOI:10.1016/j.trsl.2022.08.007] [PMID] [PMCID]
15. Clinical protocol for the diagnosis and treatment of coronavirus infection COVID-19 in pregnant women, women in labor and puerperas of August 5, 2021. Available at: http://www.rcrz.kz/index.php/ru/2017-03-12-10-50-44/press-reliz/2365-press-reliz. 16.07.2022.
16. Kurmanova A, Urazbayeva G, Terlikbayeva A, Salimbaeva D, Ayazbekov A. Diagnostic significance of blood lymphocyte activation markers in pre-eclampsia. Clin Exp Immunol 2024; 215: 94-103. [DOI:10.1093/cei/uxad121] [PMID]
17. Ayazbekov A, Nurkhasimova R, Kulbayeva S, Bolat K, Kurmanova AM, Yeskarayeva A, et al. Features of pregnancy, childbirth and postpartum period of young mothers. Electron J Gen Med 2020; 17: em260. [DOI:10.29333/ejgm/8459]
18. Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and pregnancy: What obstetricians need to know. Am J Obstet Gynecol 2020; 222: 415-426. [DOI:10.1016/j.ajog.2020.02.017] [PMID] [PMCID]
19. Bayakhmetova M, Abuova GN, Bukharbayev YB, Ablyazimov TN, Kamytbekova KZ, Baimbetova S. Q fever in individuals in the Eurasian continent: A 50-year literature review (1973-2022). Arch Clin Infect Dis 2023; 18: e136333. [DOI:10.5812/archcid-136333]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







