Sun, Feb 1, 2026
[Archive]
Volume 22, Issue 5 (May 2024)
IJRM 2024, 22(5): 411-416 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Trinh N B, Vuong A D B, Nguyen P N. Successful management of pregnancy in Turner syndrome (Monosomy X): A rare condition-based learning experience from Vietnam. IJRM 2024; 22 (5) :411-416
URL: http://ijrm.ir/article-1-3275-en.html
URL: http://ijrm.ir/article-1-3275-en.html
1- Department of High-Risk Pregnancy, Tu Du Hospital, Ho Chi Minh City, Vietnam.
2- Department of High-Risk Pregnancy, Tu Du Hospital, Ho Chi Minh City, Vietnam. & Tu Du Clinical Research Unit (TD-CRU), Tu Du Hospital, Ho Chi Minh City, Vietnam. ,docternhon@gmail.com
2- Department of High-Risk Pregnancy, Tu Du Hospital, Ho Chi Minh City, Vietnam. & Tu Du Clinical Research Unit (TD-CRU), Tu Du Hospital, Ho Chi Minh City, Vietnam. ,
Keywords: Cesarean section, Materno-fetal outcome, Oocyte donation, In vitro fertilization, Turner syndrome.
Full-Text [PDF 3058 kb]
(2254 Downloads)
| Abstract (HTML) (1551 Views)
Full-Text: (245 Views)
- Introduction
Turner syndrome (TS) is one of the most frequent chromosomal abnormalities affecting females, with a prevalence estimated to be 1 of 2500 live births (1). For most individuals with TS, the diagnosis is identified during the adolescence stage due to a lack of pubertal development (2). TS is potentially related to infertility because of primary ovarian insufficiency. The TS can carry a pregnancy at the rate of 8% and this increased in mosaic detection of TS (3). The role of in vitro fertilization with oocyte donation is an appropriate option choice for TS women who desire parenting (4, 5).
However, pregnancy in women with TS is known to be at high risk because of spontaneous miscarriages and potential cardiovascular complications which can be life-threatening and reduce the survival rate (6, 7). The large metacentric study relating to oocyte donation in TS in 10 French oocyte donation centers between 2012 and 2016, included 73 pregnant women with 39 pregnancies, of which only 24 children were born healthy. On the other hand, almost all cases were associated with adverse materno-fetal outcomes (1).
Therefore, all these women should be necessarily screened with comprehensive cardio-vascular counseling before pregnancy and have a proper follow-up during pregnancy as well as postpartum.
Herein, we present a rarely success case of 45, X TS pregnant women at our tertiary center, thus raising awareness among healthcare providers.
However, pregnancy in women with TS is known to be at high risk because of spontaneous miscarriages and potential cardiovascular complications which can be life-threatening and reduce the survival rate (6, 7). The large metacentric study relating to oocyte donation in TS in 10 French oocyte donation centers between 2012 and 2016, included 73 pregnant women with 39 pregnancies, of which only 24 children were born healthy. On the other hand, almost all cases were associated with adverse materno-fetal outcomes (1).
Therefore, all these women should be necessarily screened with comprehensive cardio-vascular counseling before pregnancy and have a proper follow-up during pregnancy as well as postpartum.
Herein, we present a rarely success case of 45, X TS pregnant women at our tertiary center, thus raising awareness among healthcare providers.
- Case Presentation
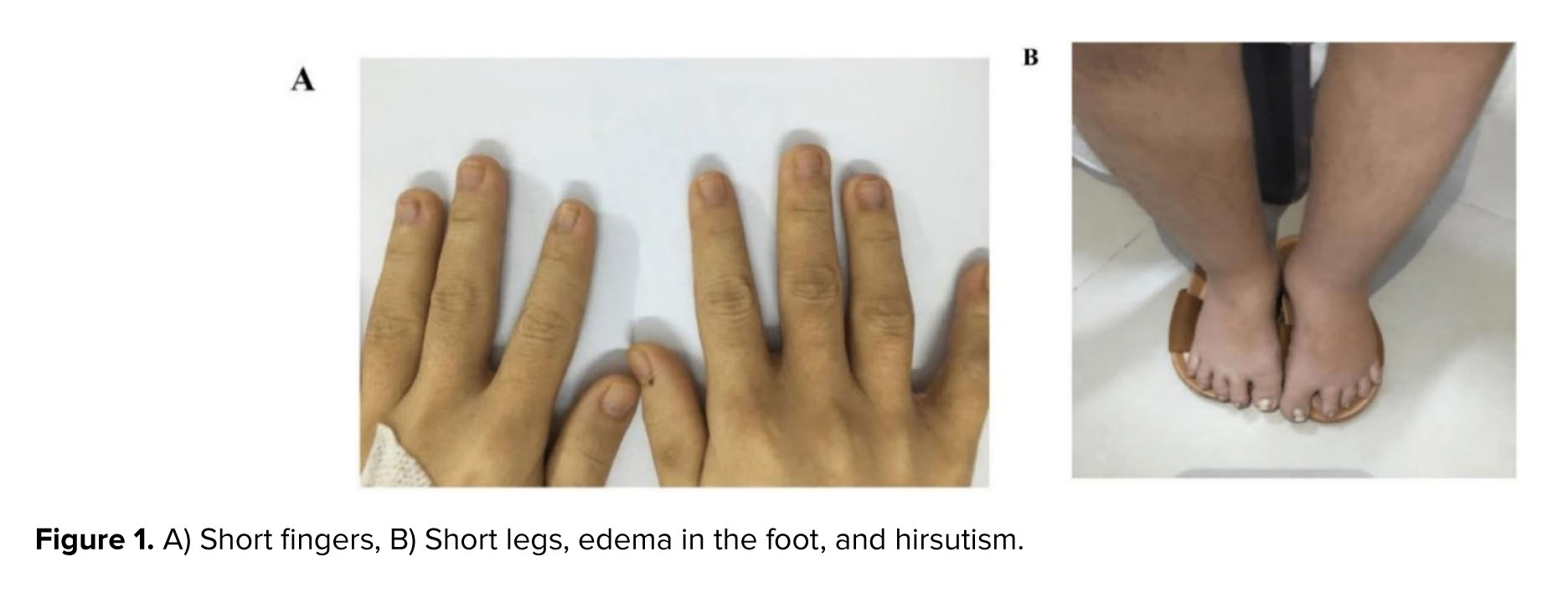
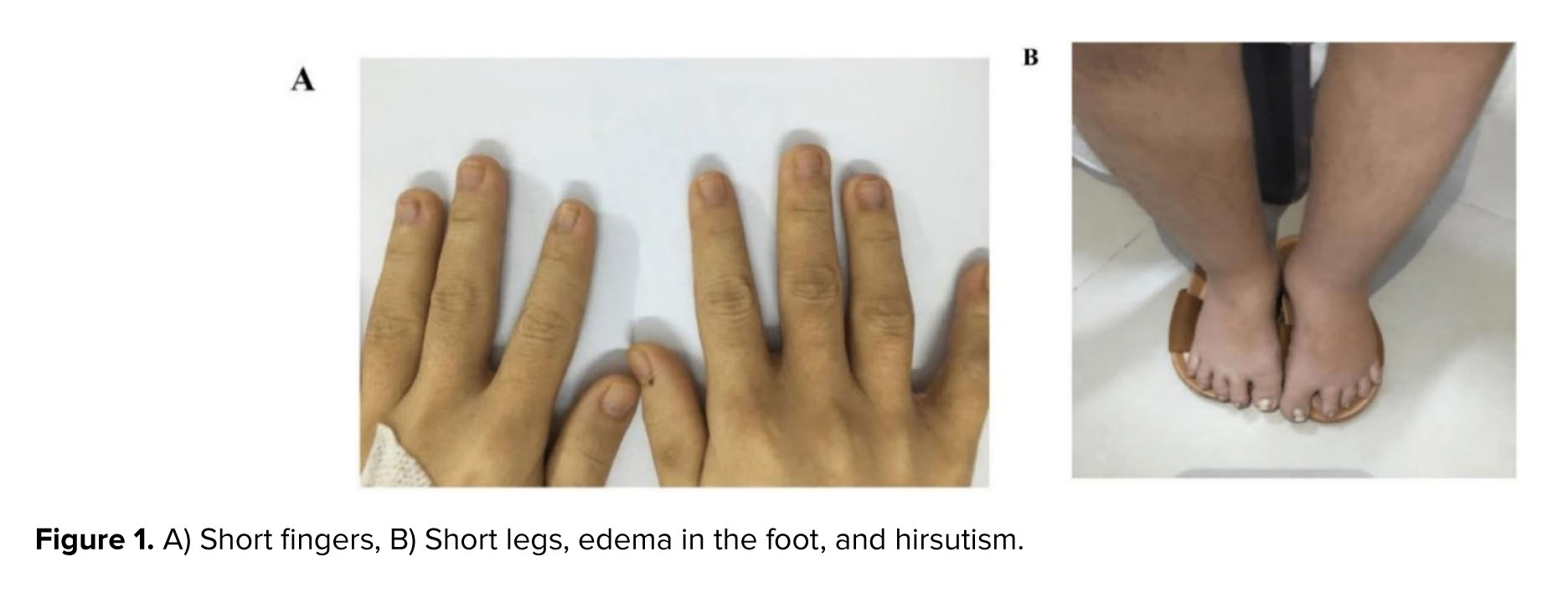
A 30-yr-old pregnant woman was hospitalized due to edema in her foot for 1 wk (Figure 1 A-B). The woman was diagnosed with TS on karyotype with 45, X monosomy when she was 15 yr old with short stature, amenorrhea, and no signs of puberty because of premature ovarian failure. Initially, she was treated with hormonal replacement therapy. Her medical record was also noted with congenital hypothyroidism, hydronephrosis, cholelithiasis (> 3 mm diameter), and bilateral kidney stone (> 8 mm diameter). She had no gestational diabetes. The protein excretion was normal. Due to the extremely low ovarian reserve (unmeasured anti-Mullerian hormone serum level), her pregnancy was conceived by in vitro fertilization with oocyte donation and preimplantation genetic testing for aneuploidy (PGT-A). In addition, the woman was diagnosed with gestational diabetes.
At admission, the vital signs were unremarkable, the woman’s height was 140 cm, and her weight was 44 kg. The woman increased to 6 kg during pregnancy. However, due to the intervention of cosmetic plastic surgery, her face was less likely to have TS syndrome. On obstetric examination, the uterus was measured at 28 cm in height and the cervix was closed without vaginal bleeding. The ultrasound finding in the first trimester showed normal nuchal translucency with a normal non-invasive prenatal test. The 4-dimension ultrasound demonstrated the fetal morphologic features as normal. The current ultrasound result revealed a viable fetus, small for gestational age, weighing 2690 gr, and corresponding to 38 wk of gestation. The amniotic fluid index was estimated at 23 cm. The current ultrasound measured a biparietal diameter of 87 mm, head circumference of 327 mm, abdominal circumference of 316 mm, and femur length of 67 mm, which corresponds to the percentile of 11%, 14%, 8%, and 1% following the Hadlock ultrasound measurement based on gestational age, respectively. The blood supply was normal and the fetal heart rate was normal at 146 beats/min according to the last Doppler ultrasound. The cardiotocography was classified as group 1 following the American College of Obstetricians and Gynecologists.
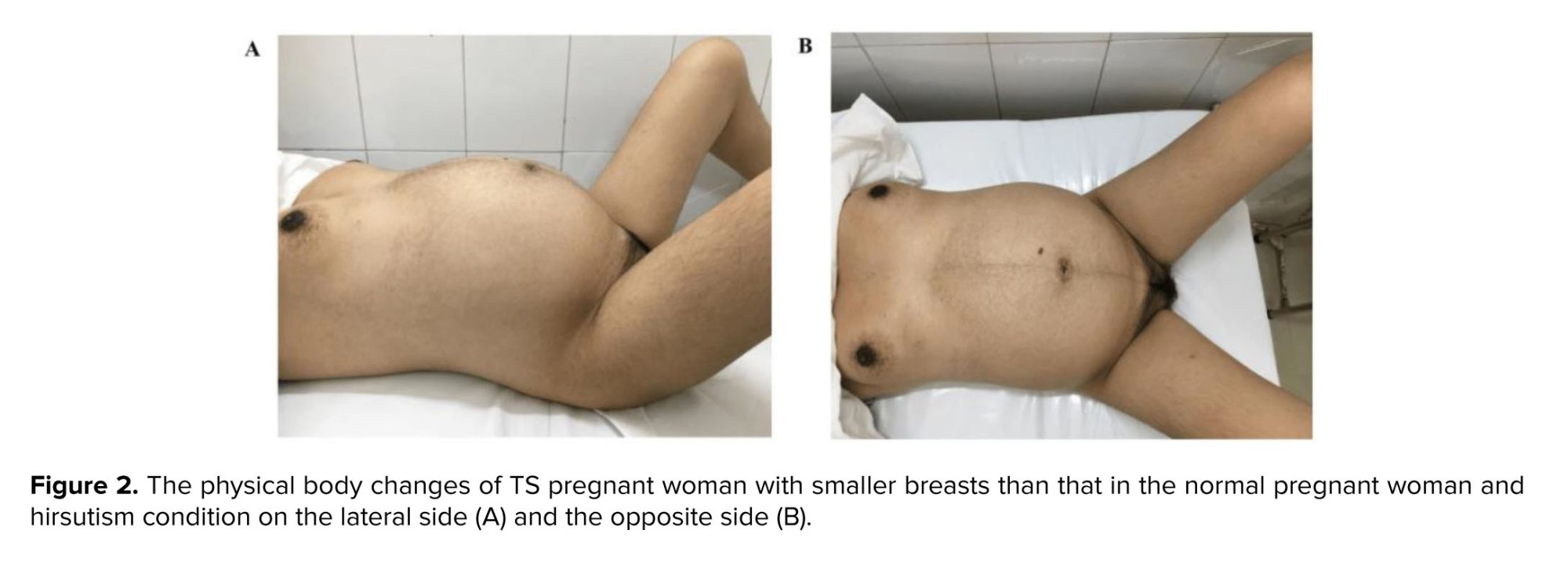
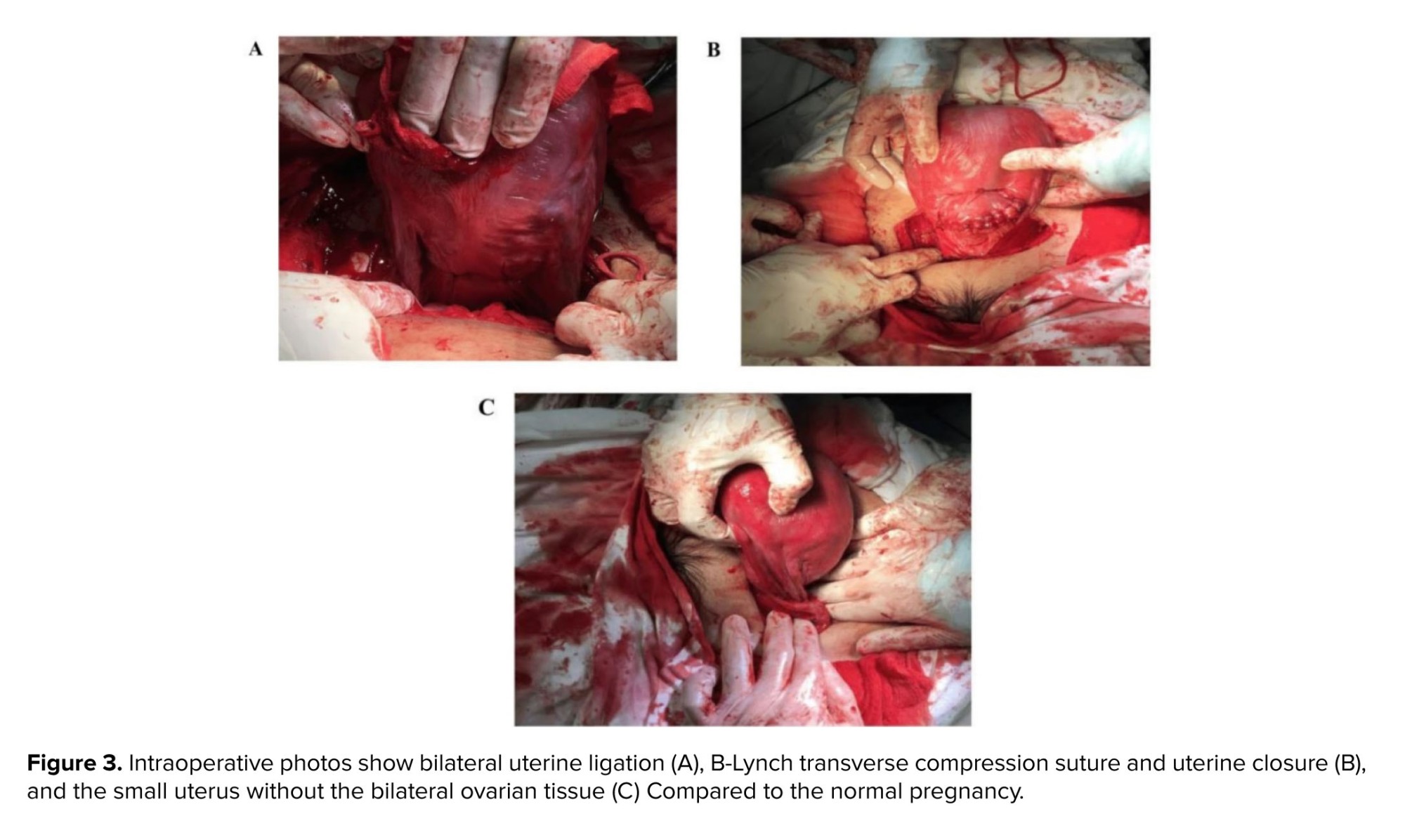
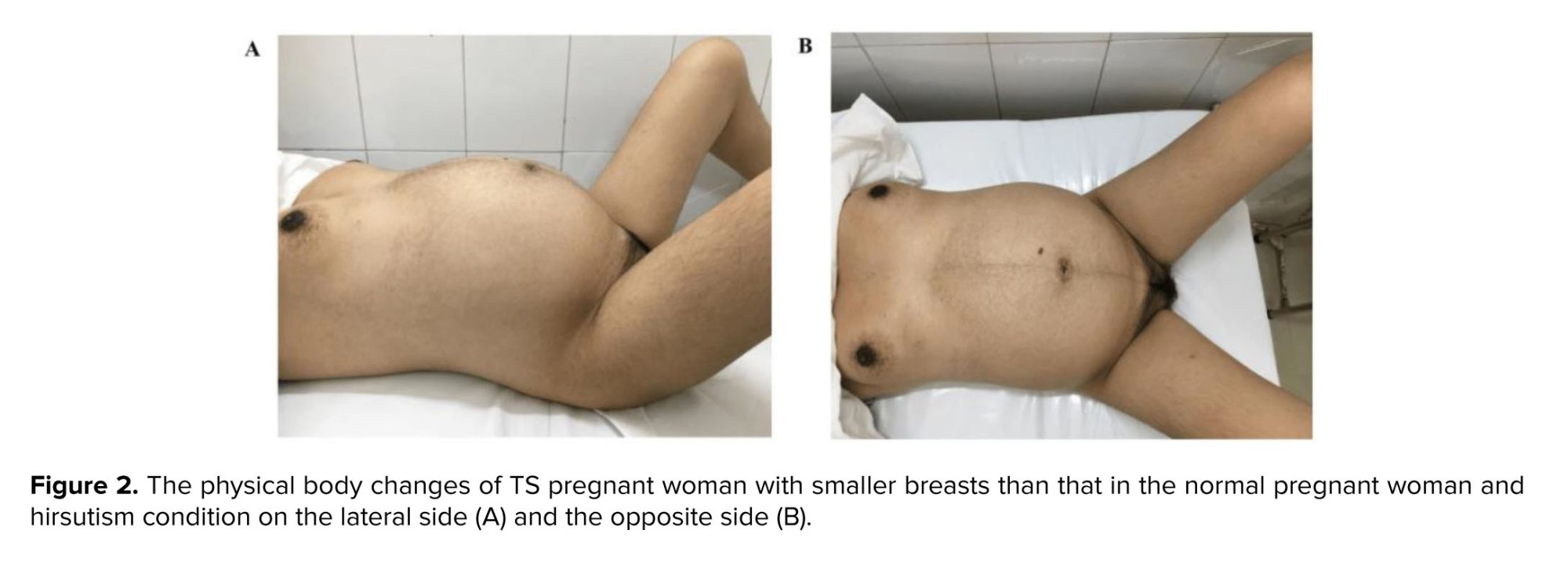
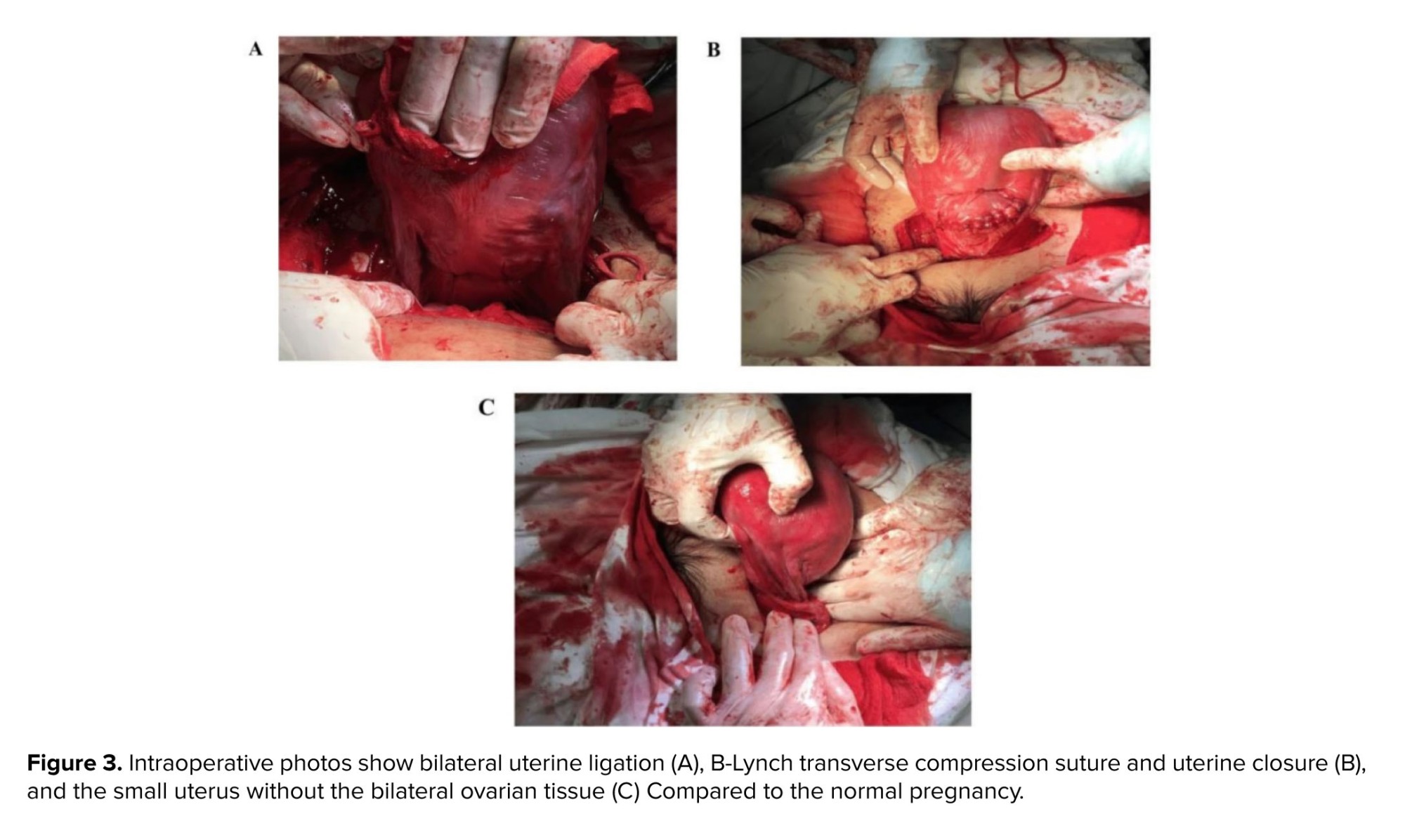
Nevertheless, because of the disproportion in size between the fetus and the maternal pelvis, the woman was indicated with elective cesarean section (CS) under regional anesthesia following lung maturation with corticosteroid therapy (intramuscular dexamethasone 6 mg × 4 in 48 hr). During surgery, the estimated blood loss was measured at 400 ml, the woman was treated with medicament such as carbetocin 100 mcg preventing the postpartum hemorrhage and underwent hemostatic procedures including placental bed suture, bilateral uterine ligation, and B-Lynch transverse compression suture. The bilateral ovaries were examinated with the atrophy appearance and the uterus size was smaller than the normal gravida uterus (Figure 2). The female newborn baby was evaluated with an Apgar score of 7 points at 1 min and of 8 points at 5 min (Figure 3). The newborn birthweight was 2800 gr. However, because of increased breathing frequency, the baby was sent to the neonatological care unit for monitoring and no further intervention was required. The postpartum course was experienced uneventfully. Both mother and baby were discharged on the 5th day of postpartum. Doppler ultrasound was detected normal (Figure 4).

2.1. Ethical considerations
This report was naturally waived by Tu Du Hospital Institutional Ethics Committee with a verbal agreement and was in accordance with the 1964 Helsinki Declaration. Informed consent was obtained from the woman before publication of this report and the use of accompanying images.
In our case, the woman had a successful pregnancy without spontaneous miscarriage or preterm birth although the complications of poor pregnancy outcomes are common. The fetus was assessed as small for gestational age on ultrasound. Small for gestational age was reported in approximately 18% of neonates of TS (13). Severely, congenital abnormalities such as fetal nuchal cystic hygroma, bilateral syndactyly of the hands and feet, and fetal hydrops can occur in TS pregnancy (14, 15).
Furthermore, besides the pregnancy outcomes, the poor events relating to aorta dissection and other adverse outcomes also increased since the women with TS have connective tissue defects (16). However, the complications relating to cardiovascular issues are not increased in pregnant women without prior structural heart diseases (13). A multidisciplinary team should be counseled for the strict management of TS pregnant women including materno-fetal medicine specialists and cardiologists. According to Gravholt et al., vaginal delivery is reasonable in women with TS with an ascending aortic size index below 2.0 cm/m2. On the contrary, a CS is recommended or a vaginal delivery with epidural anesthesia and expedited second stage may be considered in women with TS with an ascending > 2.5 cm/m2 (16). In the present case, the CS was indicated due to the disproportion in size between the fetus and the maternal birth canal, and the pregnant woman’s desire. Regardless of CS, anesthesia for cesarean delivery can be challenging since the anatomic features and low-dose combined spinal-epidural anesthesia may be the preferred technique, but the data remains limited (17).
Data availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author contributions
Ngoc Bich Trinh and Phuc Nhon Nguyen designed the study and conducted the research. Ngoc Bich Trinh and Phuc Nhon Nguyen monitored, evaluated, and analyzed the results of the study. Further, Phuc Nhon Nguyen contributed to writing, reviewing, and editing the article. Anh Dinh Bao Vuong was responsible for supervision and administrative procedures. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
The authors thank to the patient and her family who agreed to allow us to publish the clinical data. We are also grateful for all medical staffs who treated this patient at Tu Du Hospital and at the private fertility center. All of them attributed significantly to taking care of this success case. The artificial intelligence has not been used in this study.
Conflict of Interest
The authors declare that there is no conflict of interest.
At admission, the vital signs were unremarkable, the woman’s height was 140 cm, and her weight was 44 kg. The woman increased to 6 kg during pregnancy. However, due to the intervention of cosmetic plastic surgery, her face was less likely to have TS syndrome. On obstetric examination, the uterus was measured at 28 cm in height and the cervix was closed without vaginal bleeding. The ultrasound finding in the first trimester showed normal nuchal translucency with a normal non-invasive prenatal test. The 4-dimension ultrasound demonstrated the fetal morphologic features as normal. The current ultrasound result revealed a viable fetus, small for gestational age, weighing 2690 gr, and corresponding to 38 wk of gestation. The amniotic fluid index was estimated at 23 cm. The current ultrasound measured a biparietal diameter of 87 mm, head circumference of 327 mm, abdominal circumference of 316 mm, and femur length of 67 mm, which corresponds to the percentile of 11%, 14%, 8%, and 1% following the Hadlock ultrasound measurement based on gestational age, respectively. The blood supply was normal and the fetal heart rate was normal at 146 beats/min according to the last Doppler ultrasound. The cardiotocography was classified as group 1 following the American College of Obstetricians and Gynecologists.
Nevertheless, because of the disproportion in size between the fetus and the maternal pelvis, the woman was indicated with elective cesarean section (CS) under regional anesthesia following lung maturation with corticosteroid therapy (intramuscular dexamethasone 6 mg × 4 in 48 hr). During surgery, the estimated blood loss was measured at 400 ml, the woman was treated with medicament such as carbetocin 100 mcg preventing the postpartum hemorrhage and underwent hemostatic procedures including placental bed suture, bilateral uterine ligation, and B-Lynch transverse compression suture. The bilateral ovaries were examinated with the atrophy appearance and the uterus size was smaller than the normal gravida uterus (Figure 2). The female newborn baby was evaluated with an Apgar score of 7 points at 1 min and of 8 points at 5 min (Figure 3). The newborn birthweight was 2800 gr. However, because of increased breathing frequency, the baby was sent to the neonatological care unit for monitoring and no further intervention was required. The postpartum course was experienced uneventfully. Both mother and baby were discharged on the 5th day of postpartum. Doppler ultrasound was detected normal (Figure 4).

2.1. Ethical considerations
This report was naturally waived by Tu Du Hospital Institutional Ethics Committee with a verbal agreement and was in accordance with the 1964 Helsinki Declaration. Informed consent was obtained from the woman before publication of this report and the use of accompanying images.
- Discussion
In our case, the woman had a successful pregnancy without spontaneous miscarriage or preterm birth although the complications of poor pregnancy outcomes are common. The fetus was assessed as small for gestational age on ultrasound. Small for gestational age was reported in approximately 18% of neonates of TS (13). Severely, congenital abnormalities such as fetal nuchal cystic hygroma, bilateral syndactyly of the hands and feet, and fetal hydrops can occur in TS pregnancy (14, 15).
Furthermore, besides the pregnancy outcomes, the poor events relating to aorta dissection and other adverse outcomes also increased since the women with TS have connective tissue defects (16). However, the complications relating to cardiovascular issues are not increased in pregnant women without prior structural heart diseases (13). A multidisciplinary team should be counseled for the strict management of TS pregnant women including materno-fetal medicine specialists and cardiologists. According to Gravholt et al., vaginal delivery is reasonable in women with TS with an ascending aortic size index below 2.0 cm/m2. On the contrary, a CS is recommended or a vaginal delivery with epidural anesthesia and expedited second stage may be considered in women with TS with an ascending > 2.5 cm/m2 (16). In the present case, the CS was indicated due to the disproportion in size between the fetus and the maternal birth canal, and the pregnant woman’s desire. Regardless of CS, anesthesia for cesarean delivery can be challenging since the anatomic features and low-dose combined spinal-epidural anesthesia may be the preferred technique, but the data remains limited (17).
- Conclusion
Data availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author contributions
Ngoc Bich Trinh and Phuc Nhon Nguyen designed the study and conducted the research. Ngoc Bich Trinh and Phuc Nhon Nguyen monitored, evaluated, and analyzed the results of the study. Further, Phuc Nhon Nguyen contributed to writing, reviewing, and editing the article. Anh Dinh Bao Vuong was responsible for supervision and administrative procedures. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
The authors thank to the patient and her family who agreed to allow us to publish the clinical data. We are also grateful for all medical staffs who treated this patient at Tu Du Hospital and at the private fertility center. All of them attributed significantly to taking care of this success case. The artificial intelligence has not been used in this study.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Case Report |
Subject:
Assisted Reproductive Technologies
References
1. Andre H, Pimentel C, Veau S, Domin-Bernhard M, Letur-Konirsch H, Priou G, et al. Pregnancies and obstetrical prognosis after oocyte donation in Turner syndrome: A multicentric study. Eur J Obstet Gynecol Reprod Biol 2019; 238: 73-77. [DOI:10.1016/j.ejogrb.2019.05.012] [PMID]
2. Isojima T, Yokoya S. Growth in girls with Turner syndrome. Front Endocrinol 2022; 13: 1068128. [DOI:10.3389/fendo.2022.1068128] [PMID] [PMCID]
3. Mascarenhas M, Oliver J, Bhandari HM. Routes to parenthood for women with Turner syndrome. Obstet Gynaecol 2019; 21: 43-50. [DOI:10.1111/tog.12537]
4. Whigham C-A, Vollenhoven B, Vincent AJ. Reproductive health in Turner syndrome: A narrative review. Prenat Diagn 2023; 43: 261-271. [DOI:10.1002/pd.6261] [PMID]
5. Schleedoorn MJ, Fleischer K, Braat D, Oerlemans A, van der Velden A, Peek R. Why Turner patients with 45, X monosomy should not be excluded from fertility preservation services. Reprod Biol Endocrinol 2022; 20: 143. [DOI:10.1186/s12958-022-01015-z] [PMID] [PMCID]
6. Doğer E, Çakıroğlu Y, Ceylan Y, Ulak E, Özdamar Ö, Çalışkan E. Reproductive and obstetric outcomes in mosaic Turner's syndrome: A cross-sectional study and review of the literature. Reprod Biol Endocrinol 2015; 13: 59. [DOI:10.1186/s12958-015-0055-7] [PMID] [PMCID]
7. Fuchs MM, Attenhofer Jost C, Babovic-Vuksanovic D, Connolly HM, Egbe A. Long-term outcomes in patients with Turner syndrome: A 68-year follow-up. J Am Heart Assoc 2019; 8: e011501. [DOI:10.1161/JAHA.118.011501] [PMID] [PMCID]
8. Folsom LJ, Fuqua JS. Reproductive issues in women with Turner syndrome. Endocrinol Metab Clin North Am 2015; 44: 723-737. [DOI:10.1016/j.ecl.2015.07.004] [PMID] [PMCID]
9. Oktay K, Bedoschi G, Berkowitz K, Bronson R, Kashani B, McGovern P, et al. Fertility preservation in women with Turner syndrome: A comprehensive review and practical guidelines. J Pediatr Adolescent Gynecol 2016; 29: 409-416. [DOI:10.1016/j.jpag.2015.10.011] [PMID] [PMCID]
10. Ye M, Yeh J, Kosteria I, Li L. Progress in fertility preservation strategies in Turner syndrome. Front Med 2020; 7: 3. [DOI:10.3389/fmed.2020.00003] [PMID] [PMCID]
11. Liao J, Luo K, Cheng D, Xie P, Tan Y, Hu L, et al. Reproductive outcomes after preimplantation genetic testing in mosaic Turner syndrome: A retrospective cohort study of 100 cycles. J Assist Reprod Genet 2021; 38: 1247-1253. [DOI:10.1007/s10815-021-02127-y] [PMID] [PMCID]
12. Giles J, Meseguer M, Mercader A, Rubio C, Alegre L, Vidal C, et al. Preimplantation genetic testing for aneuploidy in patients with partial X monosomy using their own oocytes: Is this a suitable indication? Fertil Steril 2020; 114: 346-353. [DOI:10.1016/j.fertnstert.2020.04.003] [PMID]
13. Jasmine G, Anne Marie V, Alexander CE, Fred MW, Eric VK, Virginia PS, et al. Cardiovascular outcomes of pregnancy in Turner syndrome. Heart 2021; 107: 61-66. [DOI:10.1136/heartjnl-2020-316719] [PMID]
14. Chen H-Y, Zheng J-Q, Zhang H-P. A case report of Turner syndrome associated with fetal nuchal cystic hygroma and bilateral syndactyly of the hands and feet. Ital J Pediatr 2019; 45: 85. [DOI:10.1186/s13052-019-0680-4] [PMID] [PMCID]
15. Bedei IA, Graf A, Gloning KP, Meyer-Wittkopf M, Willner D, Krapp M, et al. Is fetal hydrops in Turner syndrome a risk factor for the development of maternal Mirror syndrome? J Clin Med 2022; 11: 4588. [DOI:10.3390/jcm11154588] [PMID] [PMCID]
16. Gravholt CH, Viuff MH, Brun S, Stochholm K, Andersen NH. Turner syndrome: Mechanisms and management. Nat Rev Endocrinol 2019; 15: 601-614. [DOI:10.1038/s41574-019-0224-4] [PMID]
17. Kalopita K, Michala L, Theofanakis C, Valsamidis D. Anesthetic management of mosaic Turner's syndrome posted for elective cesarean delivery after spontaneous pregnancy. Int J Obstet Anesthesia 2018; 34: 102-105. [DOI:10.1016/j.ijoa.2017.11.004] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







