Fri, Jan 30, 2026
[Archive]
Volume 22, Issue 12 (December 2024)
IJRM 2024, 22(12): 985-994 |
Back to browse issues page
Ethics code: IR.SUMS.MED.REC.1400.426
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sahraian A, Janipour M, Ebrahimi A, Zareizadeh Z, Habibi P, Babaei A. Comparing sexual dysfunction in cosmetic rhinoplasty candidates and normal population among married women in Shiraz, Iran: A case-control study. IJRM 2024; 22 (12) :985-994
URL: http://ijrm.ir/article-1-3289-en.html
URL: http://ijrm.ir/article-1-3289-en.html
Ali Sahraian1 

 , Masoud Janipour *2
, Masoud Janipour *2 

 , Atoosa Ebrahimi3
, Atoosa Ebrahimi3 

 , Zohre Zareizadeh3
, Zohre Zareizadeh3 

 , Pardis Habibi4
, Pardis Habibi4 

 , Amirhossein Babaei5
, Amirhossein Babaei5 




 , Masoud Janipour *2
, Masoud Janipour *2 

 , Atoosa Ebrahimi3
, Atoosa Ebrahimi3 

 , Zohre Zareizadeh3
, Zohre Zareizadeh3 

 , Pardis Habibi4
, Pardis Habibi4 

 , Amirhossein Babaei5
, Amirhossein Babaei5 


1- Research Center for Psychiatry and Behavioural Sciences, Shiraz University of Medical Sciences, Shiraz, Iran.
2- Otolaryngology Research Centre, Department of Otolaryngology, Shiraz University of Medical Sciences, Shiraz, Iran. ,masood.janipoor@gmail.com
3- Department of Psychiatry, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
4- Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran.
5- Otolaryngology Research Centre, Department of Otolaryngology, Shiraz University of Medical Sciences, Shiraz, Iran.
2- Otolaryngology Research Centre, Department of Otolaryngology, Shiraz University of Medical Sciences, Shiraz, Iran. ,
3- Department of Psychiatry, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
4- Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran.
5- Otolaryngology Research Centre, Department of Otolaryngology, Shiraz University of Medical Sciences, Shiraz, Iran.
Full-Text [PDF 233 kb]
(636 Downloads)
| Abstract (HTML) (931 Views)
1. Introduction
Sexual activity is an important aspect of life and plays an essential role in the feelings of success and happiness in married life (1, 2). Furthermore, sexual satisfaction is correlated with healthy aging, cardiovascular benefits, physical activity, lower pain sensitivity, and relaxation; it also significantly affects the quality of life (1, 3). Interpersonal communication skills, conflict resolution skills, sociocultural taboos, socioeconomic status, family responsibilities, number of children, frequency of sex, aging, infertility, genital tract surgeries, obesity, depression, anxiety, rheumatologic disorders, and other health conditions are among the factors that affect sexual satisfaction (4). The World Health Organization defines sexual health as the emotional, mental, physical, and social well-being related to sexuality (5). Sexual dysfunction in females is applied for pain disorders or any problems in sexual desire, arousal, lubrication, and orgasm (6, 7). According to the diagnostic and statistical manual of mental disorders, text revision, female sexual dysfunction is divided into sexual interest/arousal disorder, female orgasmic disorder, and genito-pelvic penetration pain disorder. Moreover, it classifies the disorders as other specified, unspecified, and substance/medication-induced sexual dysfunctions (8). Sexual dysfunction is associated with an increase in the occurrence of mental health disorders such as anxiety, as well as dissatisfaction with married life and divorce (9).
One of the factors that influence sexual performance is sexual self-esteem, which is one of the determinants of sexual self-image, and it has been proven that impaired sexual self-esteem is related to decreased sexual satisfaction (10). Disturbed self-esteem and self-image can also be found in body dysmorphic individuals, and sexual dysfunction is also more frequent among individuals with body dysmorphic disorder (11, 12).
In addition to the excessive role of social media in increasing cosmetic surgery tendency, psychiatric problems such as body dysmorphic disorder also contribute to the increased attempt for aesthetic rhinoplasty (13, 14). Body image concern is significant in candidates for cosmetic procedures, including rhinoplasty (15, 16). A previous study found an improvement in sexual self-esteem and sexual life following cosmetic surgeries (17). Although studies have shown an improvement in the sexual quality of life of women who undergo cosmetic rhinoplasty, their sexual function and sexual life satisfaction have not been compared to the normal population before their surgery.
Given the effect of women's sexual satisfaction on their quality of life and mental health, we aimed to compare the prevalence of women's sexual dysfunction in cosmetic rhinoplasty candidates with a control group.
2. Materials and Methods
2.1. Study design
This case-control study was conducted on 342 women from December 2021-2022 in Khalili and Dastgheib hospital affiliated with Shiraz University of Medical Sciences, Shiraz, Iran.
2.2. Participant recruitment and sample size
In this study, we used the convenience sampling method. Cosmetic rhinoplasty candidates were selected as the case group. Our control group consisted of women who visited the ear, nose, and throat outpatient department and were not candidates for cosmetic procedures. The inclusion criteria were female gender, married women, age > 18 yr old, marriage duration ≥ 6 months, and no acute or chronic physical or mental disorders. The exclusion criteria were drug abuse, living far from their husband, and any other conditions that affect sexual relationships, including pregnancy and gynaecologic problems during the past 6 months. The selected controls were matched with the case group for age.
2.3. Data gathering
Demographic data, including age, duration of the marriage, education, history of cigarette smoking, number of children, marital satisfaction, emotional relationship with husband, and the number of their sexual intercourse per month were gathered by face-to-face interview. The Persian-translated and validated female sexual function index (FSFI) questionnaire consisting of 19 questions was used to evaluate the female sexual function in different dimensions, including sexual desire, arousal, lubrication, orgasm, satisfaction, and sexual pain (18). The scores range from 2-36, and a higher score indicates better sexual function. An overall score below 28 is considered sexual dysfunction. The cut-off points for each dimension (sexual desire, arousal, lubrication, orgasm, satisfaction, and sexual pain) are 3.3, 3.4, 3.7, 3.4, 3.8, and 3.8, respectively (19).
2.4. Ethical Considerations
The institutional review board of Shiraz University of Medical Sciences, Shiraz, Iran approved the study protocol. We also obtained the approval of the university Ethics Committee (Code: IR.SUMS.MED.REC.1400.426). Written informed consent was obtained from all participants.
2.5. Statistical Analysis
In this study, the data of the numerical variables are shown as the mean ± standard deviation (SD), and the categorical variables are shown in percentages and frequencies. We used independent t test, Mann-Whitney, and Chi-square tests to evaluate the correlation between the variables. The Statistical Package for the Social Sciences (SPSS) software, version 23 (SPSS Inc. Chicago, IL), was used for performing the statistical analyses. A p-value < 0.05 was considered statistically significant.
3. Results
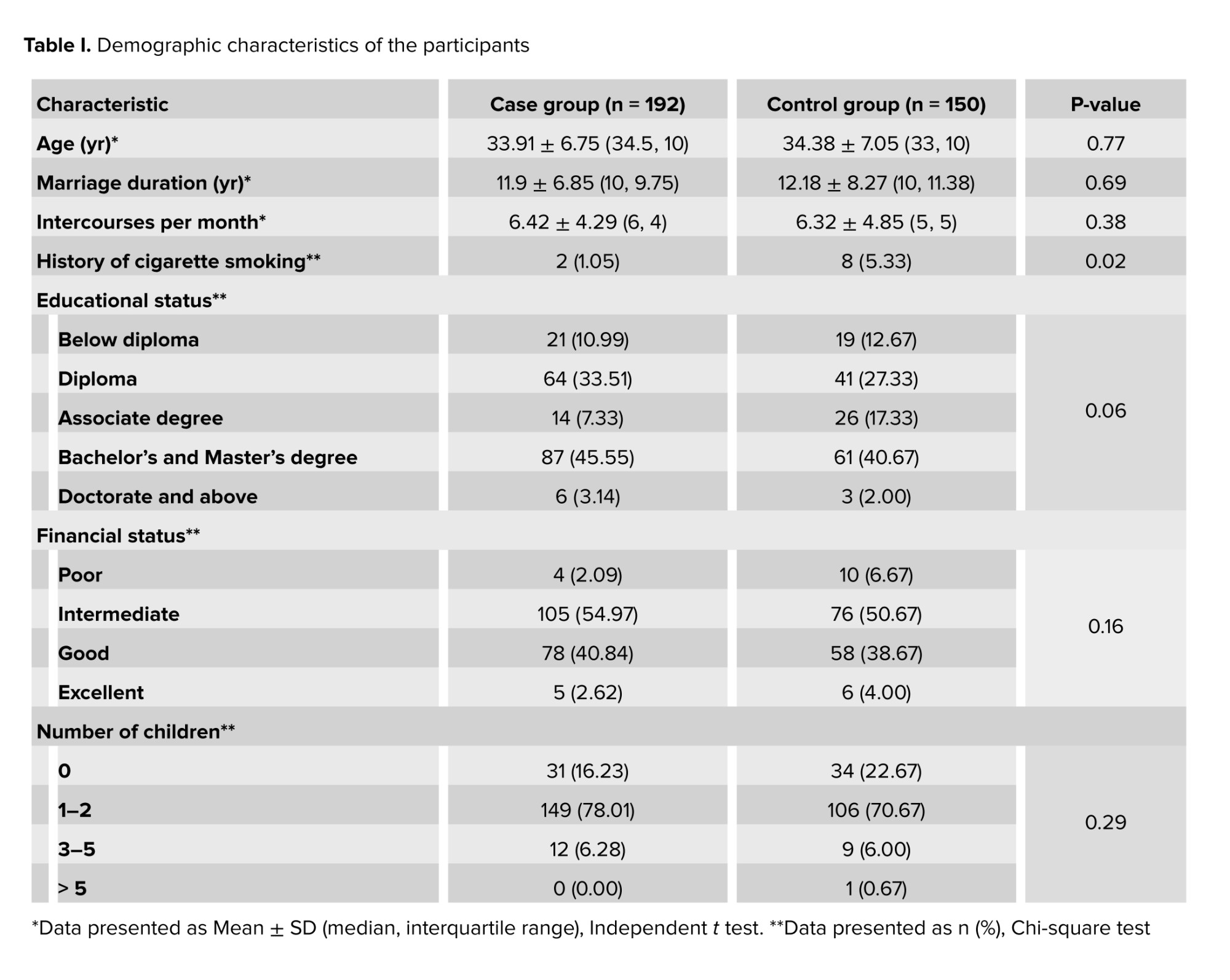
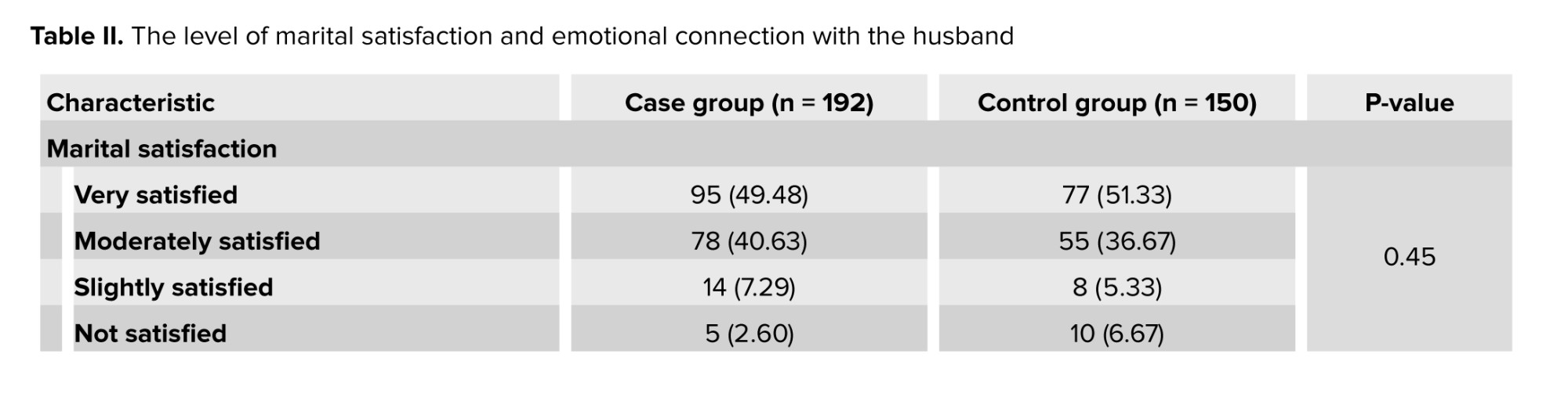
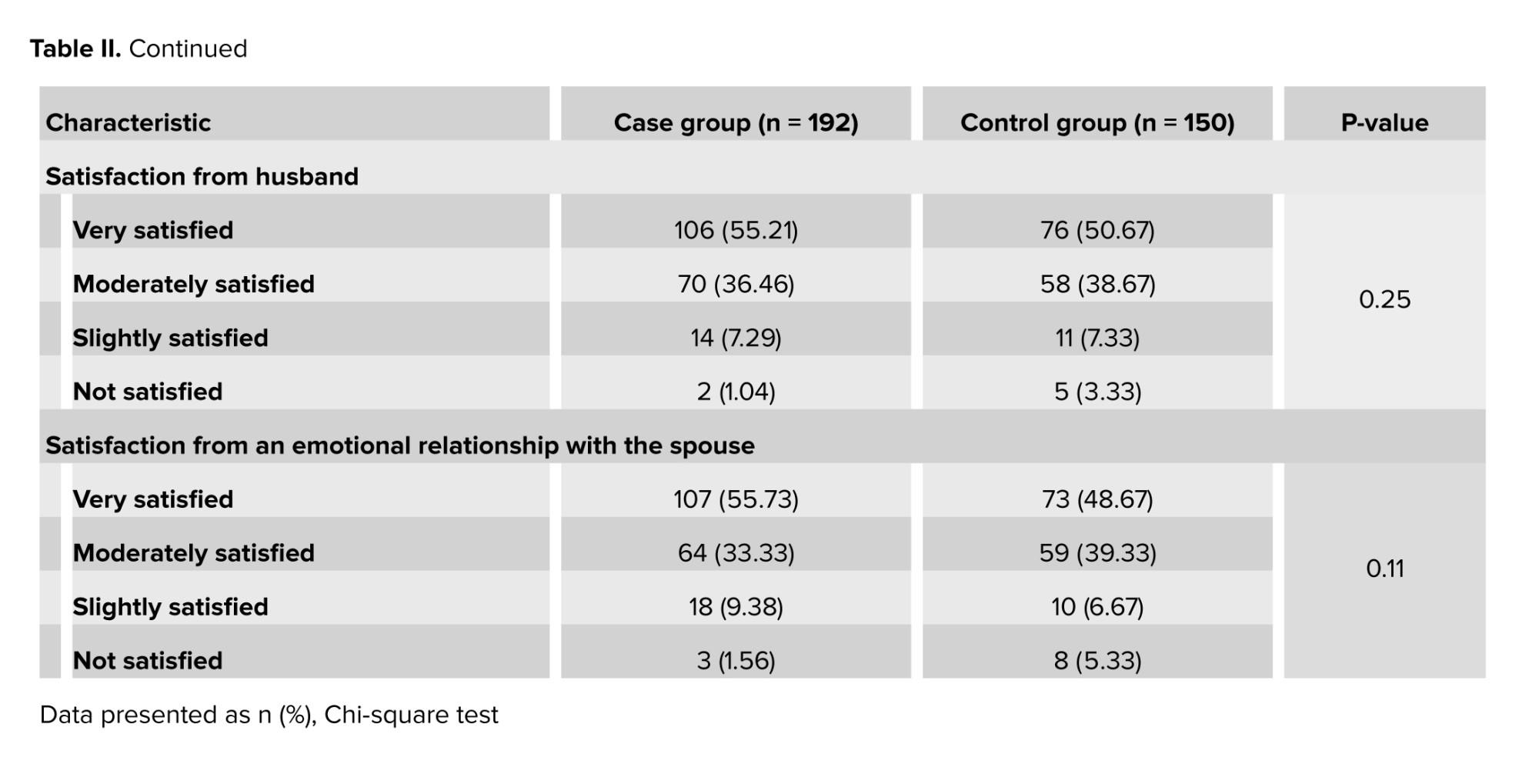
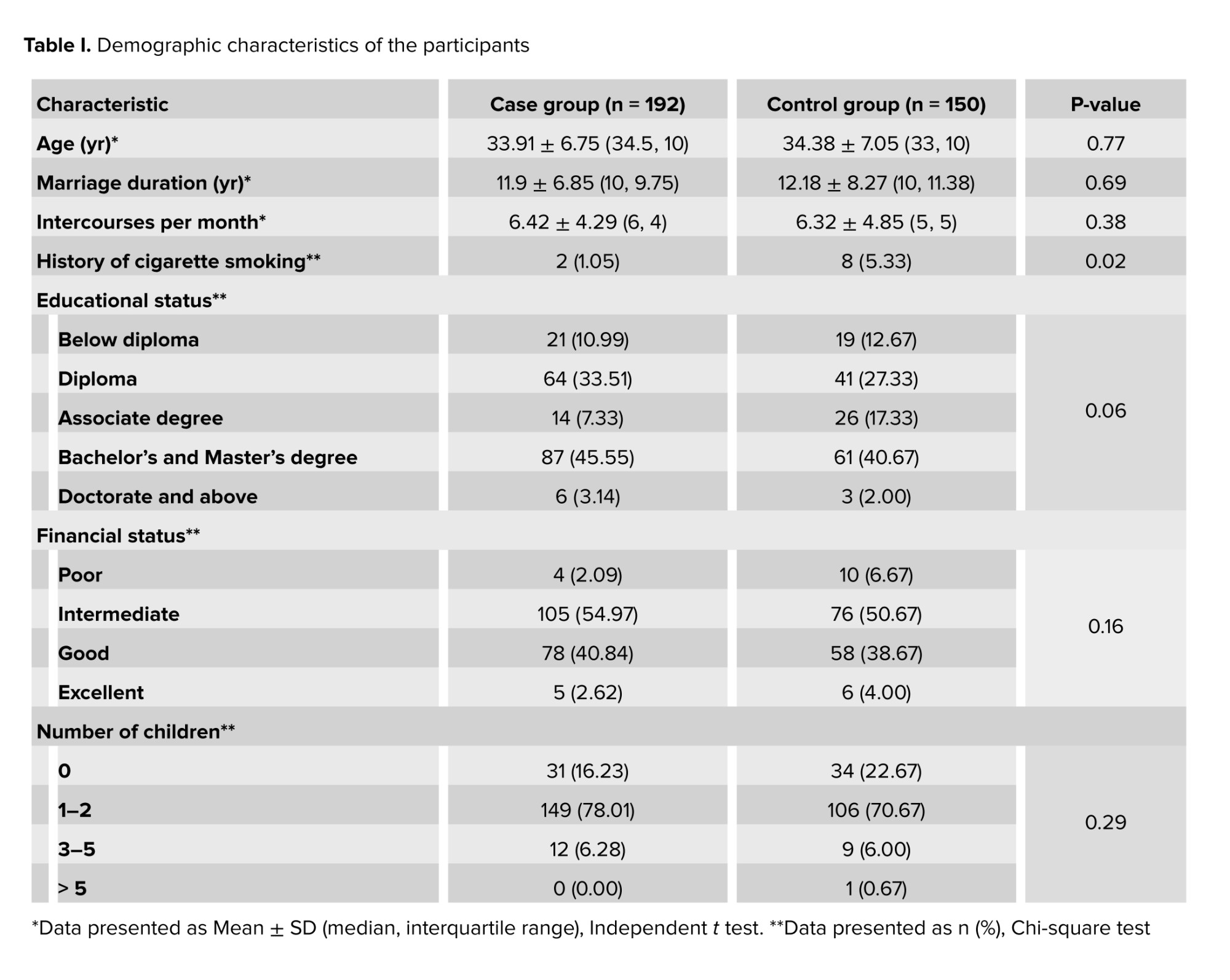
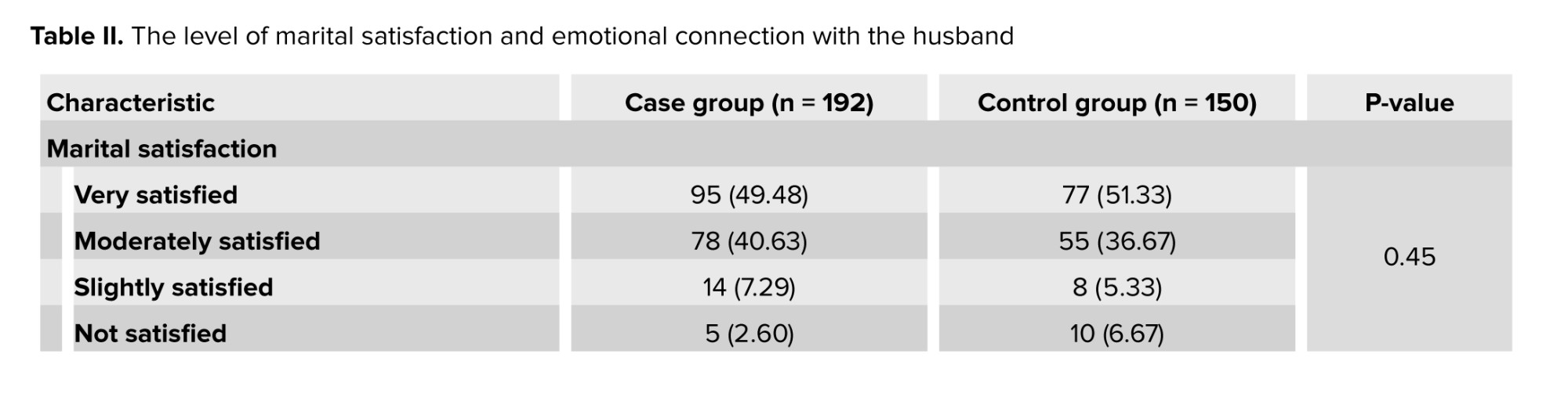
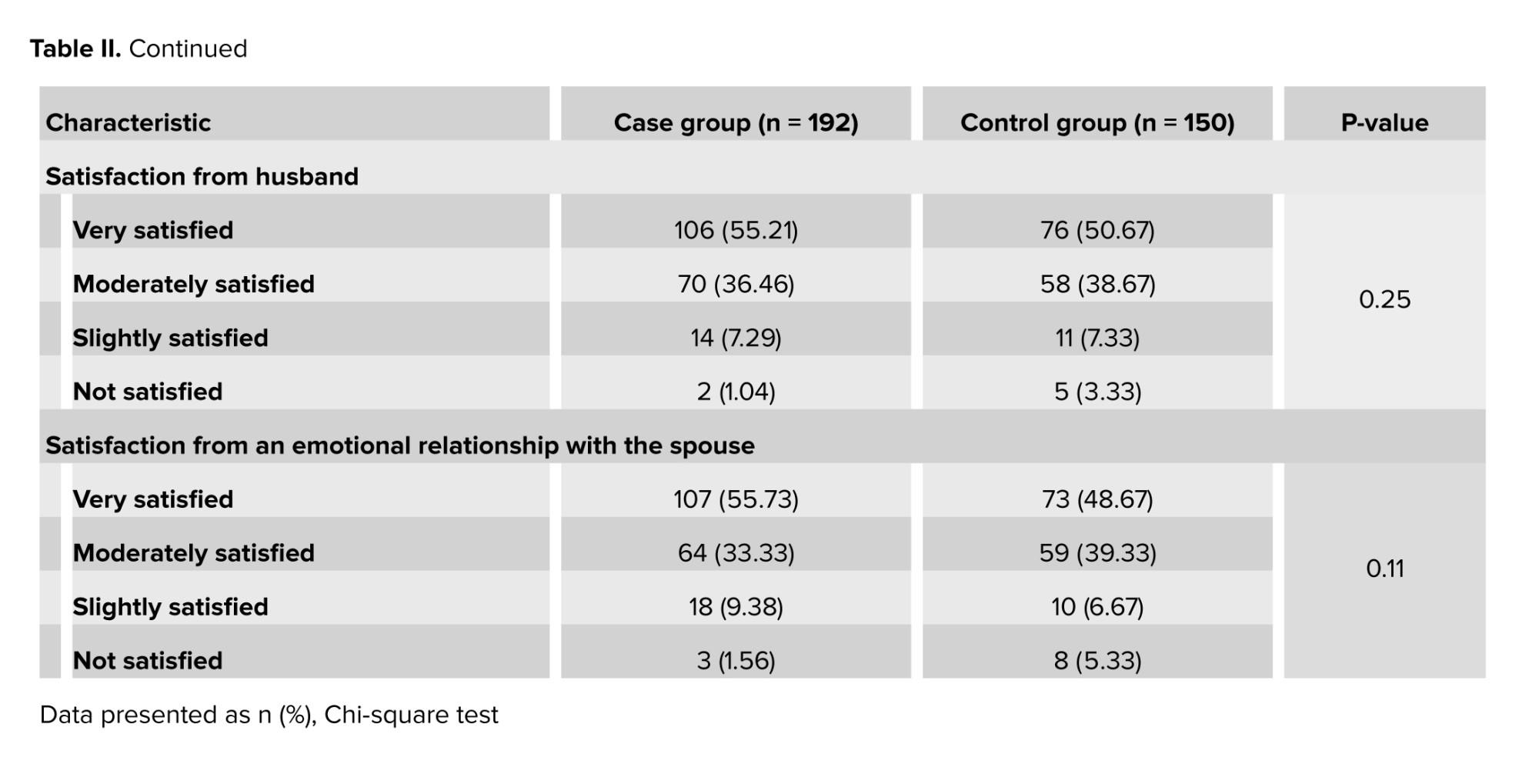
From a total of 353 participants, 11 out of the 203 female cosmetic rhinoplasty candidates were excluded from this study, and the final number of participants was 342. The rhinoplasty and control groups comprised 192 and 150 married women, respectively. No significant differences were found between the groups in age, marriage duration, education, financial status, number of children, and number of sexual intercourse per month (Table I). Marital satisfaction and emotional connection with their spouse were not significantly different between the groups (Table II).
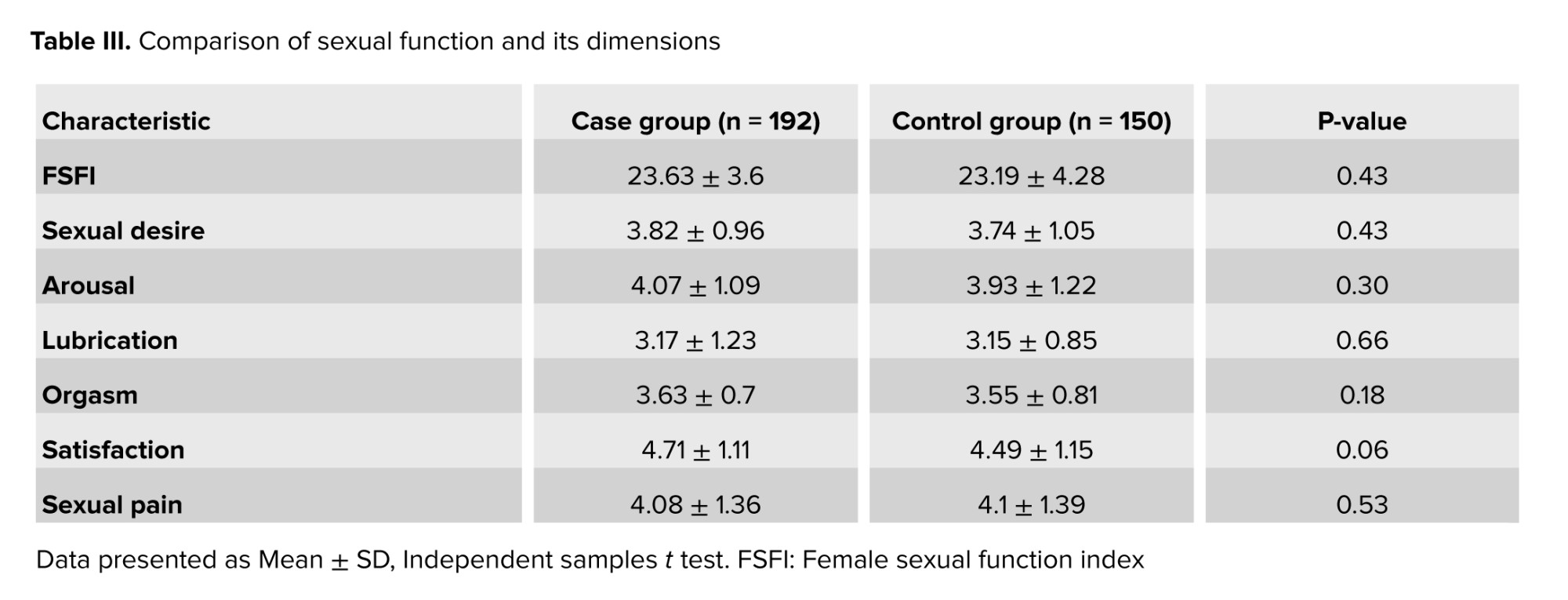
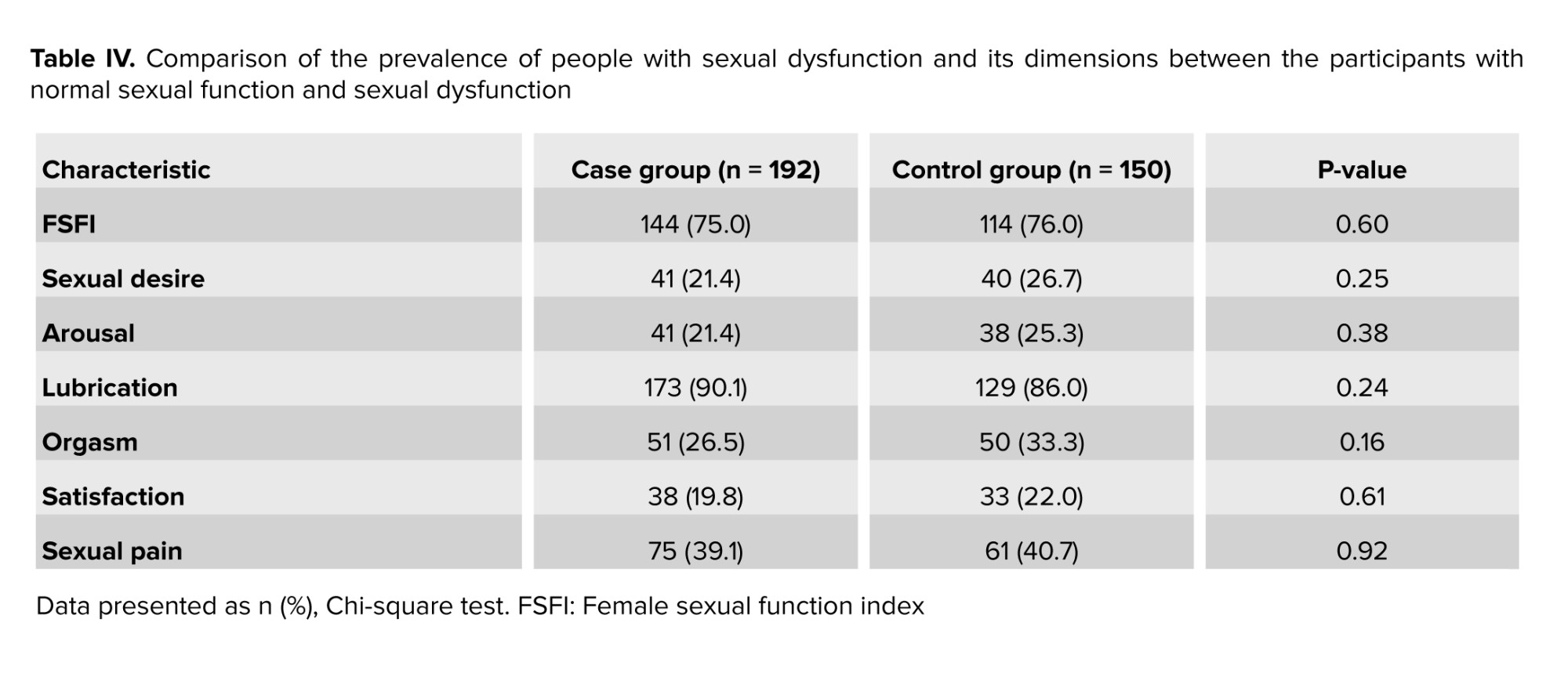
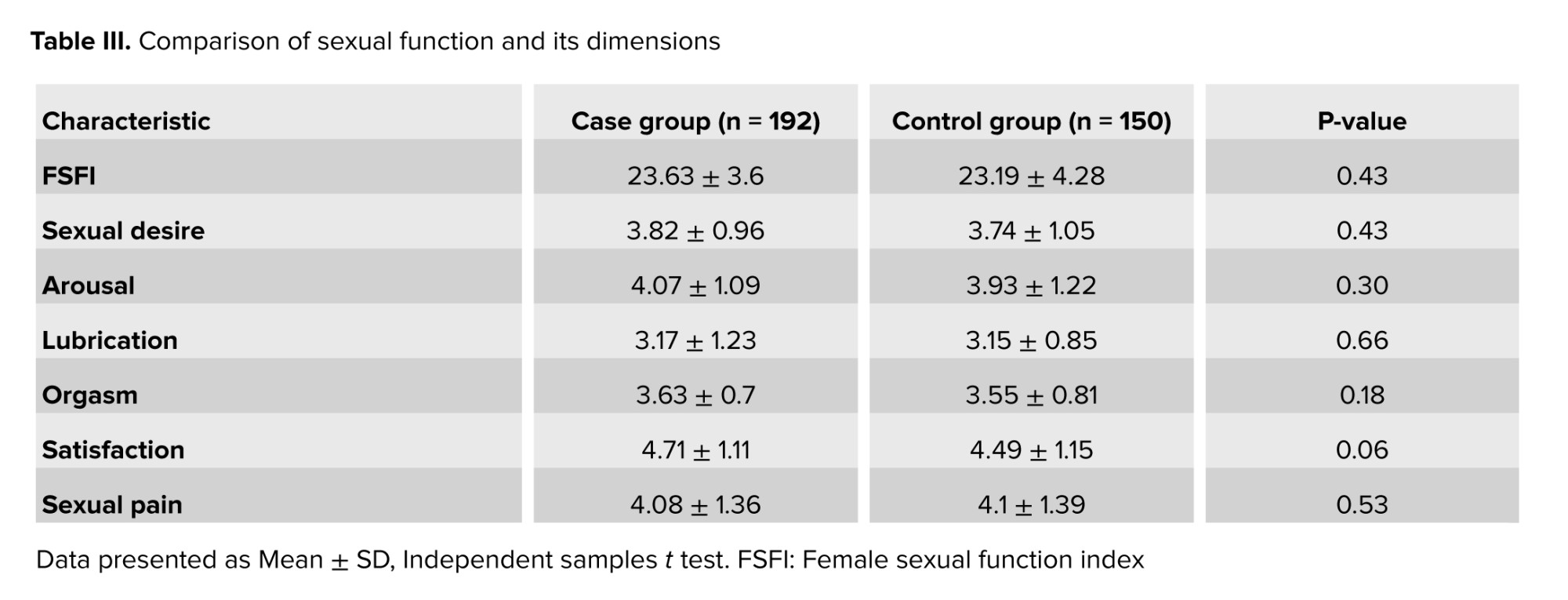
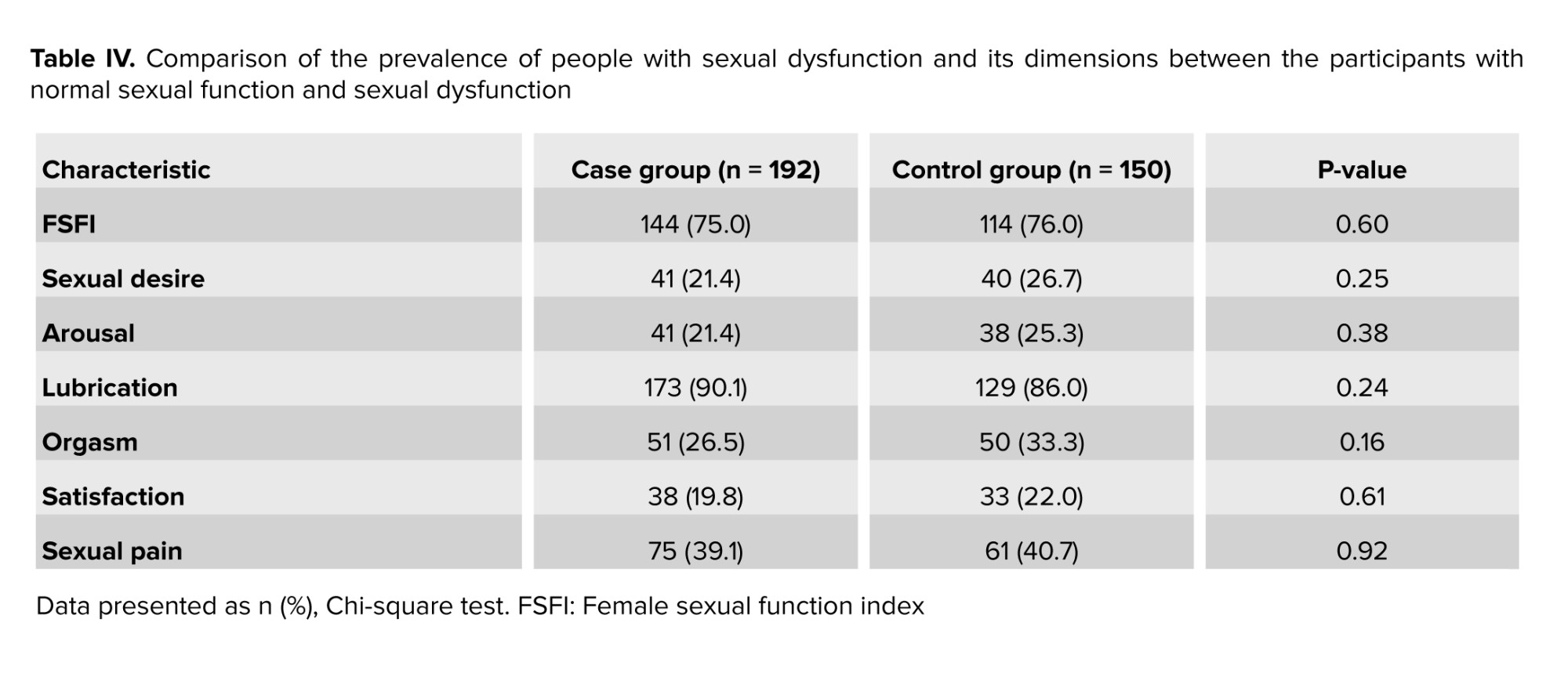
The mean ± SD of FSFI in the study population, case, and control groups were 23.43 ± 3.92, 23.63 ± 3.6, and 23.19 ± 4.28, respectively. No statistically significant differences were found between the mean scores of the rhinoplasty and the control group in terms of sexual dysfunction, sexual desire, arousal, lubrication, orgasm, satisfaction, and sexual pain (Table III). Lubrication was the dimension that caused the highest dysfunction rates among the individuals (Table IV).
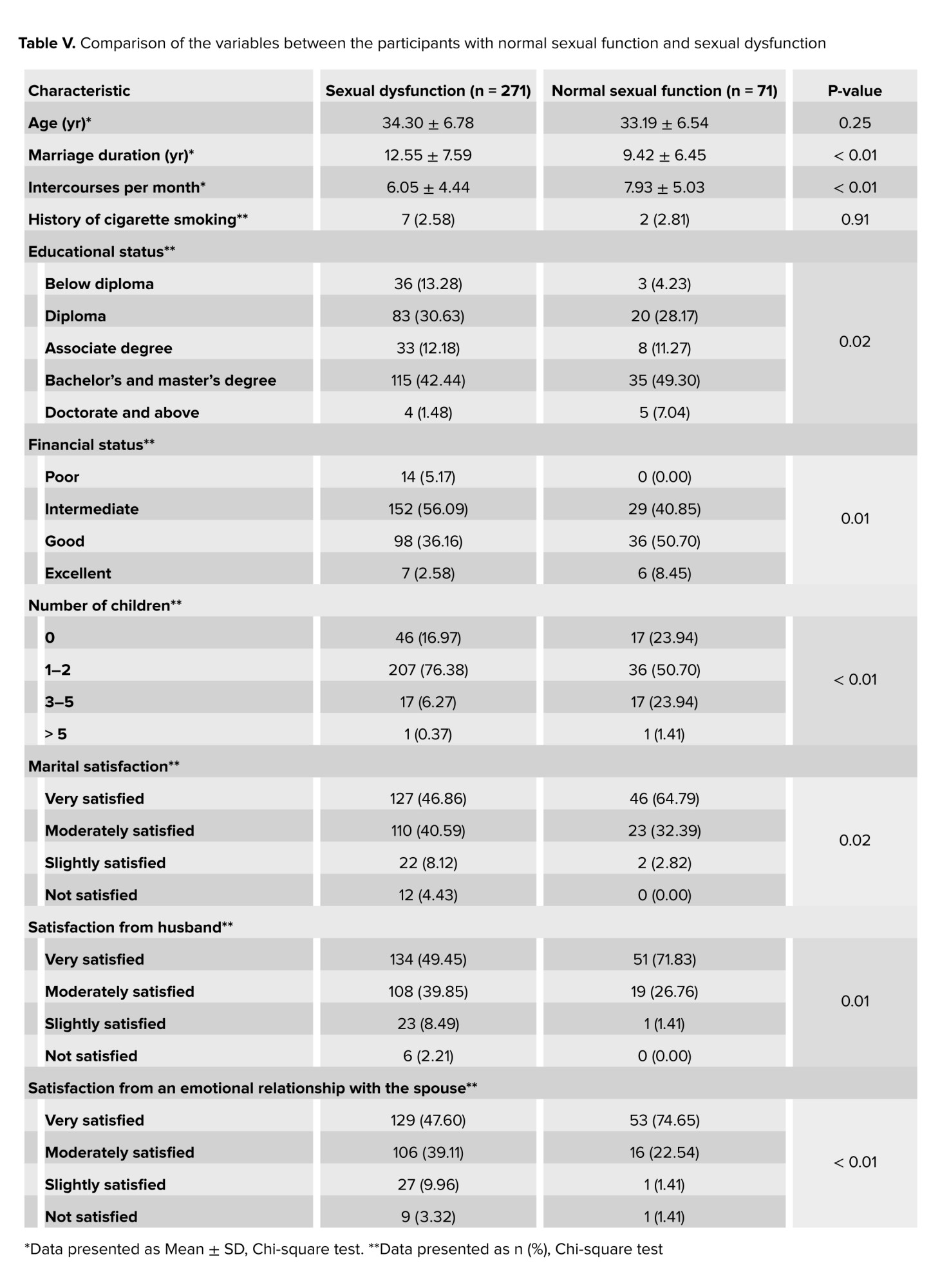
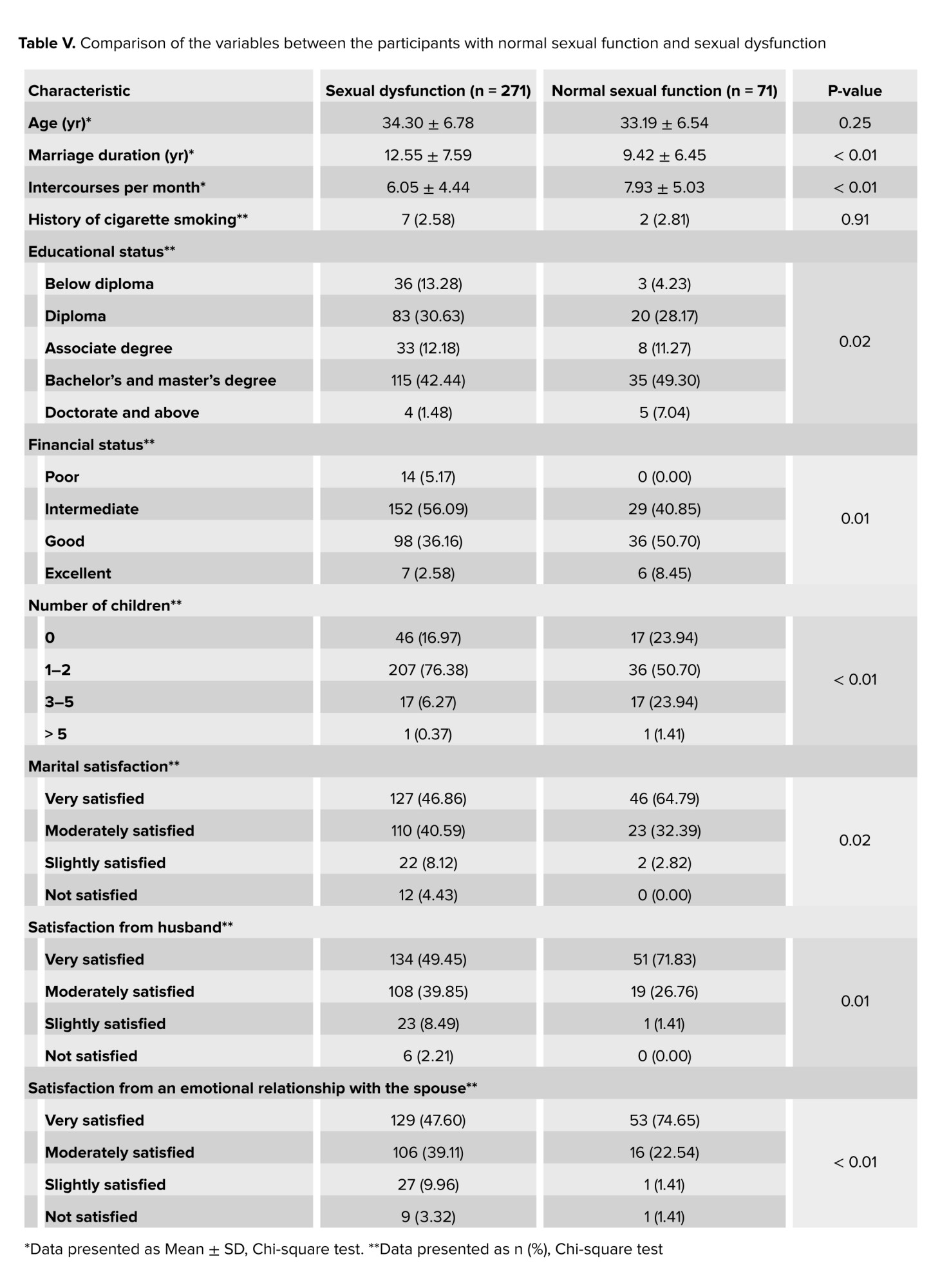
The mean duration of marriage in the sexual dysfunction group was significantly higher than the group with normal sexual function (p = 0.01). The number of intercourses per month was significantly higher in the group with normal sexual function than in the sexual dysfunction group (p < 0.01). The differences between these 2 groups regarding educational status, financial status, number of children, and marital satisfaction were also statistically significant (Table V).
4. Discussion
In our study, sexual dysfunction was found in 75.4% of the individuals. Lubrication was the most problematic dimension of sexual dysfunction and affected 88.3% of the participants. No significant difference was observed between the rhinoplasty and the control group regarding the prevalence of sexual dysfunction and its domains. In line with our findings, another study found that the prevalence of sexual dysfunction in Iranian women was 77.6% (20). The mean score of FSFI in women seeking radiofrequency of external genitalia was 25.41 ± 6.34, showing a lower sexual dysfunction than our study participants (21). In a systematic review and meta-analysis that included 7 original articles, 52% of the studied women suffered from sexual dysfunction. The prevalence of each sexual dysfunction domain, including sexual desire, arousal, lubrication, pain, and orgasm was 39%, 34%, 32%, 38%, and 30%, respectively. In contrast to our study results, decreased sexual desire and pain were more prevalent than the other dimensions of sexual dysfunction (22). In another study, the prevalence of sexual dysfunction among women was 31%, and the prevalence rates of decreased sexual desire, arousal, orgasm, and dyspareunia were 33%, 16.5%, 25%, and 45.5%, respectively. Hence, their findings were different from ours in terms of sexual dysfunction prevalence and the most prevalent domain of sexual dysfunction. They also found a statistically significant relationship between women's sexual dysfunction and marriage duration, history of mental disorder, and psychiatric drug consumption. These results are in line with those of our study in that we found a statistically significant relationship between the duration of marriage and sexual dysfunction. They also declared that educational status was not correlated to sexual dysfunction (23).
A study on women suffering from diabetes and hypertension in South Africa found that 94% of the sexually active women had an FSFI score < 26.55 and were considered to have sexual dysfunction. Lack of desire and sexual pain were observed in 90% and 83% of them, respectively, and all of them had lubrication and orgasm problems. Their underlying chronic diseases can be justified by the high prevalence of sexual dysfunction (24). In another study which was conducted on Singaporean women, 70.3% of the sexually active cases met the criteria for female sexual dysfunction. As opposed to the findings of our study, sexual dysfunction was positively associated with nulliparity (25). In a study that was conducted on Indian women, 63% of women reported desire dysfunction, 77% suffered arousal disorder, 51% had lubrication problems, and 56% had sexual pain. These higher dysfunction rates can be attributed to their different questionnaire structure (26).
In our study, marital satisfaction and emotional connection with the husband were related to decreased sexual dysfunction. It is known that sexual desire in women is highly sensitive to emotional intimacy with their partners. This condition may also make women the initiators of the sexual relationship, and they experience more pleasure in such situations (27). It seems that inadequate knowledge and feeling ashamed to talk about sexual issues are among the factors that contribute to the occurrence of sexual problems in Iranian women (28).
Various conditions such as diabetes, depression, intimate partner violence, and specific drug consumption contribute to female sexual dysfunction. Due to the numerous aetiologies of sexual dysfunction, a complete history should be taken, and a physical examination must be done. Based on the etiology inferred from the history taking and physical examination, education, medication therapy, psychological interventions, and physical therapy would be some of our therapeutic options (29). Regarding the significant prevalence of female sexual dysfunction, it is suggested that screening should be added to routine checkups (30).
Our study had some limitations. We can point out the lack of examination of body image concerns and sexual self-esteem. The availability of such data would let us investigate the relationship of sexual dysfunction with sexual self-esteem and body dysmorphic disorder among the study groups.
5. Conclusion
In conclusion, this study found that there was no significant difference in sexual dysfunction between married women who were candidates for cosmetic rhinoplasty and those in the control group. The prevalence of sexual dysfunction was high in both groups, highlighting the importance of searching for its underlying causes. In our research, we found a statistically significant relationship between sexual dysfunction and the number of children; socio-economic status and duration of marriage also affected sexual function.
Further research is needed to explore the impact of sexual orientation, body image concerns, and other mental health issues on the sexual function of women.
Data Availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author Contributions
A. Sahraian: Concept and design, critical revision of the manuscript, final approval of the version to be published, agreement to be accountable for all aspects of the work. M. Janipour: Concept and design, critical revision of the manuscript, final approval of the version to be published, and agreement to be accountable for all aspects of the work. A. Ebrahimi: Acquisition of data, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects of the work. Z. Zareizadeh: Acquisition of data, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects of the work. P. Habibi: Statistical analysis, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects of the work. A. Babaei: Statistical analysis, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects.
Acknowledgments
This study was supported by the Vice-Chancellor for Research of Shiraz University of Medical Sciences, Shiraz, Iran (grant number: 24258). We did not use artificial intelligence in any way (translation, revision, grammar check, etc.) in this manuscript. The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Namazee hospital and Dr. Nasrin Shokrpour for editorial assistance.
Conflict of Interest
The authors have no conflict of interest to disclose.
Full-Text: (169 Views)
1. Introduction
Sexual activity is an important aspect of life and plays an essential role in the feelings of success and happiness in married life (1, 2). Furthermore, sexual satisfaction is correlated with healthy aging, cardiovascular benefits, physical activity, lower pain sensitivity, and relaxation; it also significantly affects the quality of life (1, 3). Interpersonal communication skills, conflict resolution skills, sociocultural taboos, socioeconomic status, family responsibilities, number of children, frequency of sex, aging, infertility, genital tract surgeries, obesity, depression, anxiety, rheumatologic disorders, and other health conditions are among the factors that affect sexual satisfaction (4). The World Health Organization defines sexual health as the emotional, mental, physical, and social well-being related to sexuality (5). Sexual dysfunction in females is applied for pain disorders or any problems in sexual desire, arousal, lubrication, and orgasm (6, 7). According to the diagnostic and statistical manual of mental disorders, text revision, female sexual dysfunction is divided into sexual interest/arousal disorder, female orgasmic disorder, and genito-pelvic penetration pain disorder. Moreover, it classifies the disorders as other specified, unspecified, and substance/medication-induced sexual dysfunctions (8). Sexual dysfunction is associated with an increase in the occurrence of mental health disorders such as anxiety, as well as dissatisfaction with married life and divorce (9).
One of the factors that influence sexual performance is sexual self-esteem, which is one of the determinants of sexual self-image, and it has been proven that impaired sexual self-esteem is related to decreased sexual satisfaction (10). Disturbed self-esteem and self-image can also be found in body dysmorphic individuals, and sexual dysfunction is also more frequent among individuals with body dysmorphic disorder (11, 12).
In addition to the excessive role of social media in increasing cosmetic surgery tendency, psychiatric problems such as body dysmorphic disorder also contribute to the increased attempt for aesthetic rhinoplasty (13, 14). Body image concern is significant in candidates for cosmetic procedures, including rhinoplasty (15, 16). A previous study found an improvement in sexual self-esteem and sexual life following cosmetic surgeries (17). Although studies have shown an improvement in the sexual quality of life of women who undergo cosmetic rhinoplasty, their sexual function and sexual life satisfaction have not been compared to the normal population before their surgery.
Given the effect of women's sexual satisfaction on their quality of life and mental health, we aimed to compare the prevalence of women's sexual dysfunction in cosmetic rhinoplasty candidates with a control group.
2. Materials and Methods
2.1. Study design
This case-control study was conducted on 342 women from December 2021-2022 in Khalili and Dastgheib hospital affiliated with Shiraz University of Medical Sciences, Shiraz, Iran.
2.2. Participant recruitment and sample size
In this study, we used the convenience sampling method. Cosmetic rhinoplasty candidates were selected as the case group. Our control group consisted of women who visited the ear, nose, and throat outpatient department and were not candidates for cosmetic procedures. The inclusion criteria were female gender, married women, age > 18 yr old, marriage duration ≥ 6 months, and no acute or chronic physical or mental disorders. The exclusion criteria were drug abuse, living far from their husband, and any other conditions that affect sexual relationships, including pregnancy and gynaecologic problems during the past 6 months. The selected controls were matched with the case group for age.
2.3. Data gathering
Demographic data, including age, duration of the marriage, education, history of cigarette smoking, number of children, marital satisfaction, emotional relationship with husband, and the number of their sexual intercourse per month were gathered by face-to-face interview. The Persian-translated and validated female sexual function index (FSFI) questionnaire consisting of 19 questions was used to evaluate the female sexual function in different dimensions, including sexual desire, arousal, lubrication, orgasm, satisfaction, and sexual pain (18). The scores range from 2-36, and a higher score indicates better sexual function. An overall score below 28 is considered sexual dysfunction. The cut-off points for each dimension (sexual desire, arousal, lubrication, orgasm, satisfaction, and sexual pain) are 3.3, 3.4, 3.7, 3.4, 3.8, and 3.8, respectively (19).
2.4. Ethical Considerations
The institutional review board of Shiraz University of Medical Sciences, Shiraz, Iran approved the study protocol. We also obtained the approval of the university Ethics Committee (Code: IR.SUMS.MED.REC.1400.426). Written informed consent was obtained from all participants.
2.5. Statistical Analysis
In this study, the data of the numerical variables are shown as the mean ± standard deviation (SD), and the categorical variables are shown in percentages and frequencies. We used independent t test, Mann-Whitney, and Chi-square tests to evaluate the correlation between the variables. The Statistical Package for the Social Sciences (SPSS) software, version 23 (SPSS Inc. Chicago, IL), was used for performing the statistical analyses. A p-value < 0.05 was considered statistically significant.
3. Results
From a total of 353 participants, 11 out of the 203 female cosmetic rhinoplasty candidates were excluded from this study, and the final number of participants was 342. The rhinoplasty and control groups comprised 192 and 150 married women, respectively. No significant differences were found between the groups in age, marriage duration, education, financial status, number of children, and number of sexual intercourse per month (Table I). Marital satisfaction and emotional connection with their spouse were not significantly different between the groups (Table II).
The mean ± SD of FSFI in the study population, case, and control groups were 23.43 ± 3.92, 23.63 ± 3.6, and 23.19 ± 4.28, respectively. No statistically significant differences were found between the mean scores of the rhinoplasty and the control group in terms of sexual dysfunction, sexual desire, arousal, lubrication, orgasm, satisfaction, and sexual pain (Table III). Lubrication was the dimension that caused the highest dysfunction rates among the individuals (Table IV).
The mean duration of marriage in the sexual dysfunction group was significantly higher than the group with normal sexual function (p = 0.01). The number of intercourses per month was significantly higher in the group with normal sexual function than in the sexual dysfunction group (p < 0.01). The differences between these 2 groups regarding educational status, financial status, number of children, and marital satisfaction were also statistically significant (Table V).
4. Discussion
In our study, sexual dysfunction was found in 75.4% of the individuals. Lubrication was the most problematic dimension of sexual dysfunction and affected 88.3% of the participants. No significant difference was observed between the rhinoplasty and the control group regarding the prevalence of sexual dysfunction and its domains. In line with our findings, another study found that the prevalence of sexual dysfunction in Iranian women was 77.6% (20). The mean score of FSFI in women seeking radiofrequency of external genitalia was 25.41 ± 6.34, showing a lower sexual dysfunction than our study participants (21). In a systematic review and meta-analysis that included 7 original articles, 52% of the studied women suffered from sexual dysfunction. The prevalence of each sexual dysfunction domain, including sexual desire, arousal, lubrication, pain, and orgasm was 39%, 34%, 32%, 38%, and 30%, respectively. In contrast to our study results, decreased sexual desire and pain were more prevalent than the other dimensions of sexual dysfunction (22). In another study, the prevalence of sexual dysfunction among women was 31%, and the prevalence rates of decreased sexual desire, arousal, orgasm, and dyspareunia were 33%, 16.5%, 25%, and 45.5%, respectively. Hence, their findings were different from ours in terms of sexual dysfunction prevalence and the most prevalent domain of sexual dysfunction. They also found a statistically significant relationship between women's sexual dysfunction and marriage duration, history of mental disorder, and psychiatric drug consumption. These results are in line with those of our study in that we found a statistically significant relationship between the duration of marriage and sexual dysfunction. They also declared that educational status was not correlated to sexual dysfunction (23).
A study on women suffering from diabetes and hypertension in South Africa found that 94% of the sexually active women had an FSFI score < 26.55 and were considered to have sexual dysfunction. Lack of desire and sexual pain were observed in 90% and 83% of them, respectively, and all of them had lubrication and orgasm problems. Their underlying chronic diseases can be justified by the high prevalence of sexual dysfunction (24). In another study which was conducted on Singaporean women, 70.3% of the sexually active cases met the criteria for female sexual dysfunction. As opposed to the findings of our study, sexual dysfunction was positively associated with nulliparity (25). In a study that was conducted on Indian women, 63% of women reported desire dysfunction, 77% suffered arousal disorder, 51% had lubrication problems, and 56% had sexual pain. These higher dysfunction rates can be attributed to their different questionnaire structure (26).
In our study, marital satisfaction and emotional connection with the husband were related to decreased sexual dysfunction. It is known that sexual desire in women is highly sensitive to emotional intimacy with their partners. This condition may also make women the initiators of the sexual relationship, and they experience more pleasure in such situations (27). It seems that inadequate knowledge and feeling ashamed to talk about sexual issues are among the factors that contribute to the occurrence of sexual problems in Iranian women (28).
Various conditions such as diabetes, depression, intimate partner violence, and specific drug consumption contribute to female sexual dysfunction. Due to the numerous aetiologies of sexual dysfunction, a complete history should be taken, and a physical examination must be done. Based on the etiology inferred from the history taking and physical examination, education, medication therapy, psychological interventions, and physical therapy would be some of our therapeutic options (29). Regarding the significant prevalence of female sexual dysfunction, it is suggested that screening should be added to routine checkups (30).
Our study had some limitations. We can point out the lack of examination of body image concerns and sexual self-esteem. The availability of such data would let us investigate the relationship of sexual dysfunction with sexual self-esteem and body dysmorphic disorder among the study groups.
5. Conclusion
In conclusion, this study found that there was no significant difference in sexual dysfunction between married women who were candidates for cosmetic rhinoplasty and those in the control group. The prevalence of sexual dysfunction was high in both groups, highlighting the importance of searching for its underlying causes. In our research, we found a statistically significant relationship between sexual dysfunction and the number of children; socio-economic status and duration of marriage also affected sexual function.
Further research is needed to explore the impact of sexual orientation, body image concerns, and other mental health issues on the sexual function of women.
Data Availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author Contributions
A. Sahraian: Concept and design, critical revision of the manuscript, final approval of the version to be published, agreement to be accountable for all aspects of the work. M. Janipour: Concept and design, critical revision of the manuscript, final approval of the version to be published, and agreement to be accountable for all aspects of the work. A. Ebrahimi: Acquisition of data, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects of the work. Z. Zareizadeh: Acquisition of data, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects of the work. P. Habibi: Statistical analysis, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects of the work. A. Babaei: Statistical analysis, drafting of the manuscript, final approval of the version to be published; agreement to be accountable for all aspects.
Acknowledgments
This study was supported by the Vice-Chancellor for Research of Shiraz University of Medical Sciences, Shiraz, Iran (grant number: 24258). We did not use artificial intelligence in any way (translation, revision, grammar check, etc.) in this manuscript. The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran and also Center for Development of Clinical Research of Namazee hospital and Dr. Nasrin Shokrpour for editorial assistance.
Conflict of Interest
The authors have no conflict of interest to disclose.
Type of Study: Original Article |
Subject:
Reproductive Psycology
References
1. Panahi R, Anbari M, Javanmardi E, Jahangasht Ghoozlu Kh, Dehghankar L. The effect of women's sexual functioning on quality of their sexual life. J Prev Med Hyg 2021; 62: E776-E781.
2. Bilal A, Rasool S. Marital satisfaction and satisfaction with life: Mediating role of sexual satisfaction in married women. J Psychosexual Health 2020; 2: 77-86. [DOI:10.1177/2631831820912873]
3. Miguel I, von Humboldt S, Leal I. Sexual well-being across the lifespan: Is sexual satisfaction related to adjustment to aging? Sex Res Soc Policy 2024; 21: 1-12. [DOI:10.1007/s13178-024-00939-y]
4. Pious AA, Amaresha AC. Exploring factors of sexual function and sexual satisfaction among nonworking women: A qualitative study. J Psychosexual Health 2023; 5: 208-215. [DOI:10.1177/26318318231221932]
5. Narasimhan M, Gilmore K, Murillo R, Allotey P. Sexual health and well-being across the life course: Call for papers. Bull World Health Organ 2023; 101: 750. [DOI:10.2471/BLT.23.291043] [PMCID]
6. Hosseini SE, Ilkhani M, Rohani C, Nikbakht Nasrabadi A, Ghanei Gheshlagh R, Moini A. Prevalence of sexual dysfunction in women with cancer: A systematic review and meta-analysis. Int J Reprod BioMed 2022; 20: 1-12. [DOI:10.18502/ijrm.v20i1.10403] [PMID] [PMCID]
7. Andresen JB, Graugaard C, Andersson M, Bahnsen MK, Frisch M. Sexual inactivity and dysfunction in Denmark: A project SEXUS study. Arch Sex Behav 2022; 51: 3669-3688. [DOI:10.1007/s10508-022-02348-x] [PMID]
8. Prabhu SS, Hegde S, Sareen S. Female sexual dysfunction: A potential minefield. Indian J Sex Transm Dis AIDS 2022; 43: 128-134. [DOI:10.4103/ijstd.IJSTD_82_20] [PMID] [PMCID]
9. Khademi R, Hosseini SH, Sharif Nia H, Khani S. Evaluating co-occurrence of depression and sexual dysfunction and related factors among Iranian rural women: A population-based study. Biomedicine 2020; 10: 33-39. [DOI:10.37796/2211-8039.1003] [PMID] [PMCID]
10. Ziaei T, Farahmand Rad H, Rezaei Aval M, Roshandel Gh. The relationship between sexual self-concept and sexual function in women of reproductive age referred to health centers in Gorgan, North East of Iran. J Midwifery Reprod Health 2017; 5: 969-977.
11. Kuck N, Cafitz L, Bürkner P-C, Hoppen L, Wilhelm S, Buhlmann U. Body dysmorphic disorder and self-esteem: A meta-analysis. BMC Psychiatry 2021; 21: 310. [DOI:10.1186/s12888-021-03185-3] [PMID] [PMCID]
12. Henn AT, Taube CO, Vocks S, Hartmann AS. Body image as well as eating disorder and body dysmorphic disorder symptoms in heterosexual, homosexual, and bisexual women. Front Psychiatry 2019; 10: 531. [DOI:10.3389/fpsyt.2019.00531] [PMID] [PMCID]
13. Walker CE, Krumhuber EG, Dayan S, Furnham A. Effects of social media use on desire for cosmetic surgery among young women. Curr Psychol 2021; 40: 3355-3364. [DOI:10.1007/s12144-019-00282-1]
14. de Souza TSC, Patrial MTCRdO, Meneguetti AFC, de Souza MSC, Meneguetti ME, Rossato VF. Body dysmorphic disorder in rhinoplasty candidates: Prevalence and functional correlations. Aesthetic Plast Surg 2021; 45: 641-648. [DOI:10.1007/s00266-020-01930-9] [PMID]
15. Ghazizadeh Hashemi SA, Edalatnoor B, Edalatnoor B, Niksun O. A comparison of body image concern in candidates for rhinoplasty and therapeutic surgery. Electronic Physician 2017; 9: 5363-5368. [DOI:10.19082/5363] [PMID] [PMCID]
16. Sahraian A, Janipour M, Tarjan A, Zareizadeh Z, Habibi P, Babaei A. Body dysmorphic and narcissistic personality disorder in cosmetic rhinoplasty candidates. Aesthetic Plast Surg 2022; 46: 332-337.
https://doi.org/10.1007/s00266-021-02711-8 [DOI:10.1007/s00266-021-02603-x]
17. Heidarzadeh A, Shahmohammadipour P, Azzizadeh Forouzi M, Dehghan M, Khorasani Z. Body image, self-esteem, and psychological problems among applicants and non-applicants of cosmetic surgery. J Pract Clin Psychol 2019; 7: 33-42. [DOI:10.32598/jpcp.7.1.33]
18. Fakhri A, Pakpour AH, Burri A, Morshedi H, Mohammadi Zeidi I. The female sexual function index: Translation and validation of an Iranian version. J Sex Med 2012; 9: 514-523. [DOI:10.1111/j.1743-6109.2011.02553.x] [PMID]
19. Jafarzadeh Esfehani R, Fazel N, Dashti S, Moshkani S, Haghighi Hasanabad F, Foji S, et al. Female sexual dysfunction and its associated risk factors: An epidemiological study in the North-East of Iran. J Midwifery Reprod Health 2016; 4: 498-505.
20. Mohammadian S, Dolatshahi B. Sexual problems in Tehran: Prevalence and associated factors. J Educ Health Promot 2019; 8: 217. [DOI:10.4103/jehp.jehp_231_19] [PMID] [PMCID]
21. Lordêlo P, Leal MRD, Brasil CA, Santos JM, Lima MCNPC, Sartori MGF. Radiofrequency in female external genital cosmetics and sexual function: A randomized clinical trial. Int Urogynecol J 2016; 27: 1681-1687. [DOI:10.1007/s00192-016-3020-x] [PMID]
22. Ghiasi A, Keramat A. Prevalence of sexual dysfunction among reproductive-age women in Iran: A systematic review and meta-analysis. J Midwifery Reprod Health 2018; 6: 1390-1398.
23. Mazinani R, Akbari Mehr M, Kaskian A, Kashanian M. [Evaluation of prevalence of sexual dysfunctions and its related factors in women]. Razi Journal of Medical Sciences 2013; 19: 59-66. (in Persian)
24. Pretorius D, Couper ID, Mlambo MG. Neglected sexual dysfunction symptoms amongst chronic patients during routine consultations in rural clinics in the North West province. Afr J Prim Health Care Fam Med 2021; 13: e1-e7. [DOI:10.4102/phcfm.v13i1.2850] [PMID] [PMCID]
25. Logan S, Thu WPP, Ho K, Cauley JA, Kramer MS, Yong E-L. Sexual inactivity and sexual dysfunction in midlife Singaporean women: A prospective cross-sectional study of prevalence and risk factors. Maturitas 2021; 152: 1-9. [DOI:10.1016/j.maturitas.2021.07.002] [PMID]
26. Singh N, Sharma P, Mishra N. Female sexual dysfunction: Indian perspective and role of Indian gynecologists. Indian J Community Med 2020; 45: 333-337. [DOI:10.4103/ijcm.IJCM_365_19] [PMID] [PMCID]
27. Amanelahi A, Refahi N, Rajabi Gh. [Predicting sexual dysfunction based on sexual self-esteem and intimacy with spouse among female college students with and without sexual dysfunction disorder]. Iranian Journal of Psychiatric Nursing 2017; 5: 18-24. (in Persian) [DOI:10.21859/ijpn-05053]
28. Merghati Khoei E, Moeini B, Barati M, Soltanian AR, Shahpiri E, Ghaleiha A, et al. A qualitative inquiry of sexuality in Iranian couples using the information-motivation-behavioral skills paradigm. J Egypt Public Health Assoc 2019; 94: 27. [DOI:10.1186/s42506-019-0024-7] [PMID] [PMCID]
29. Clayton AH, Valladares Juarez EM. Female sexual dysfunction. Med Clin North Am 2019; 103: 681-698. [DOI:10.1016/j.mcna.2019.02.008] [PMID]
30. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Gynecology. Female sexual dysfunction: ACOG practice bulletin clinical management guidelines for obstetrician-gynecologists, number 213. Obstet Gynecol 2019; 134: e1-e18. [DOI:10.1097/AOG.0000000000003324]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |