Sun, Feb 1, 2026
[Archive]
Volume 23, Issue 3 (March 2025)
IJRM 2025, 23(3): 225-240 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Meamar F Z, Savabi-Esfahani M, Farajkhoda T. Prenatal screening of Down syndrome in assisted reproductive techniques pregnancies: A systematic review. IJRM 2025; 23 (3) :225-240
URL: http://ijrm.ir/article-1-3424-en.html
URL: http://ijrm.ir/article-1-3424-en.html
1- Department of Midwifery and Reproductive Health, Faculty of Nursing and Midwifery, Reproductive Sciences and Sexual Health Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Midwifery and Reproductive Health, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
3- Research Center for Nursing and Midwifery Care, Non-Communicable Diseases Research Institute, Department of Midwifery, School of Nursing and Midwifery, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,farajkhoda_t@yahoo.com
2- Department of Midwifery and Reproductive Health, Faculty of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran.
3- Research Center for Nursing and Midwifery Care, Non-Communicable Diseases Research Institute, Department of Midwifery, School of Nursing and Midwifery, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Keywords: Down syndrome, Prenatal diagnosis, Maternal serum screening tests, Assisted reproductive technique.
Full-Text [PDF 455 kb]
(1091 Downloads)
| Abstract (HTML) (933 Views)
Full-Text: (92 Views)
1. Introduction
Down syndrome (trisomy 21) is the most prevalent chromosomal abnormality in neonates with a higher chance of survival than other chromosomal disorders. Its overall prevalence is about 10 cases per 10,000 live births around the globe (1). Due to the high costs of caring for these children and the high burden of medical, emotional, and psychological services for the family, the life quality of these people's families is also influenced (2). Thus, prenatal diagnosis of these diseases and termination of pregnancy at the right time can reduce the amount of suffering caused by their occurrence.
Among the various types of prenatal screening protocols, the most widely used during the first trimester of pregnancy is the combination of nuchal translucency (NT) measurement and serum level measurement of free beta-human chorionic gonadotropin (fβHCG) and pregnancy-associated plasma protein-A (PAPP-A), the so-called integrated screening. The most widely used second trimester screening test is the quad test, which uses the mother's age, serum beta-human chorionic gonadotropin (βHCG), alpha-fetoprotein (AFP), unconjugated estriol (uE3), and inhibin A. In the combined screening protocol, the results of the first and second trimesters are integrated, and the sensitivity of Down syndrome diagnosis reaches 94-96%. Yet, it is still associated with 5% false-positive results (3). Assisted reproductive technology (ART) pregnancies may have levels of biochemical markers that are different, especially during the second trimester, compared to spontaneous pregnancies (4). The false-positive rate for diagnosing Down syndrome after ART pregnancies is also 5% in both screening rounds (5), leading to unnecessary invasive diagnostic measures in some cases (6).
Pregnancy can be a challenging and stressful period for women who have conceived through ART (7). One of the concerns of these couples is to perform prenatal screenings because there is a possibility that the screening in these women may be wrong. In other words, it may have been a false positive, and as a result, it will cause them a lot of anxiety. Moreover, invasive diagnostic procedures such as amniocentesis and chorionic villus sampling are necessary for them (8-10). In contrast, having screening methods to detect chromosomal disorders before birth is one of the reproductive health rights of couples, and they have the right to have a healthy child (11). Interpreting the results of chromosomal disease screenings using serum and sonographic markers after ART pregnancies is challenging. Firstly, the mean age of mothers is higher than spontaneous pregnancies. Secondly, if it leads to twins or multiples, relying on the mother's serum markers may show abnormal results despite the health of the fetus (12).
Considering that the majority of chromosomal problems in pregnancies resulting from ART have not been proven so far, but the serum markers of Down syndrome have been reported in some studies to be different in pregnancies resulting from ART compared to natural pregnancies, and considering that nowadays ART includes a large group of methods that have many differences, also knowing that couples with infertility have succeeded in experiencing pregnancy after paying a lot of financial and psychological costs and have the right to health diagnostic methods before birth, and having a normal fetus and baby, this study was designed with the aim of systematic review of types of prenatal imaging and serological screenings for the diagnosis of Down's syndrome in pregnancies resulting from assisted reproductive technologies using available valid documents in order to know and correctly interpret the results of prenatal screenings in these pregnancies.
2. Materials and Methods
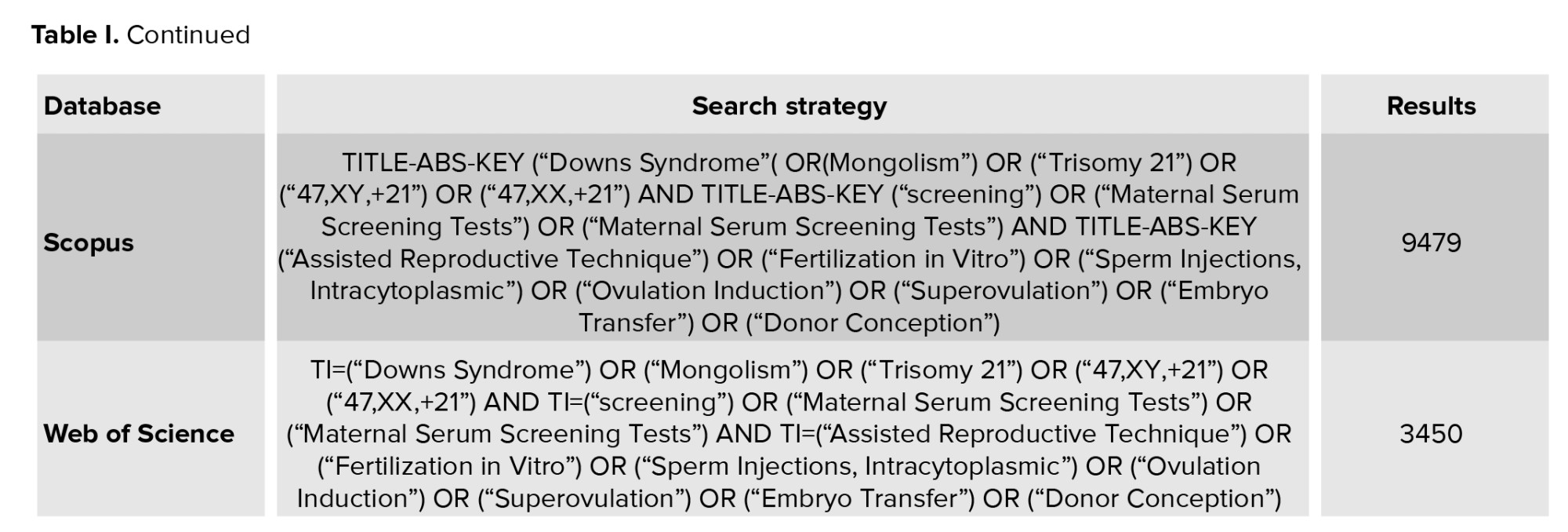
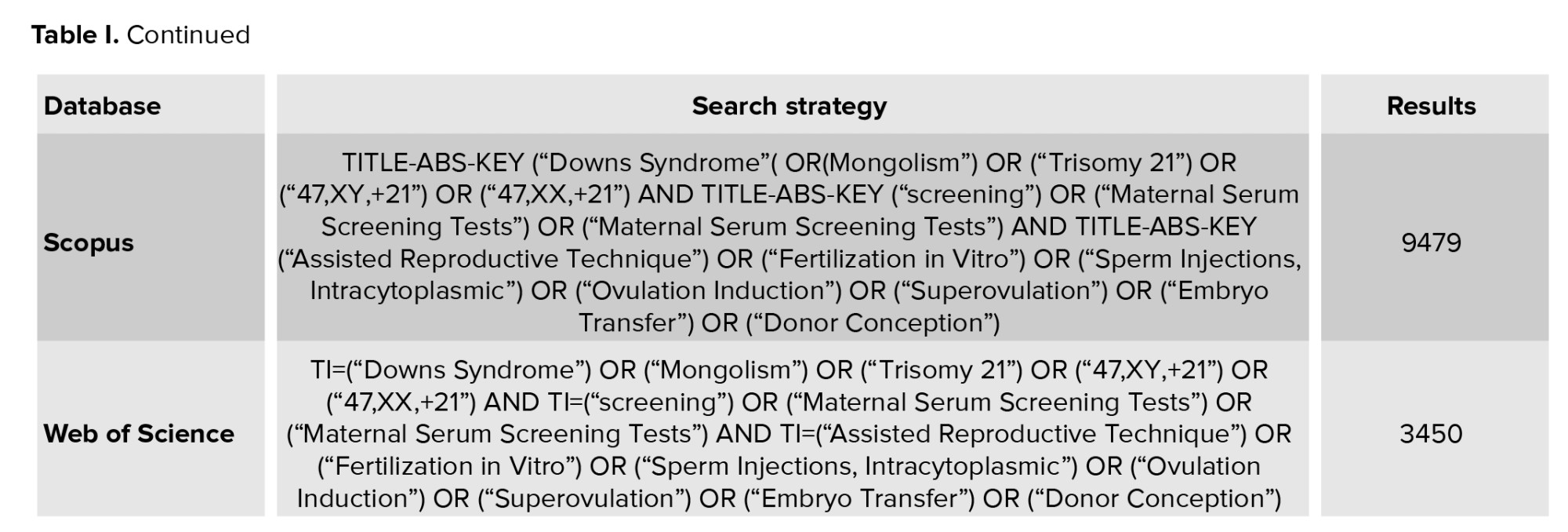
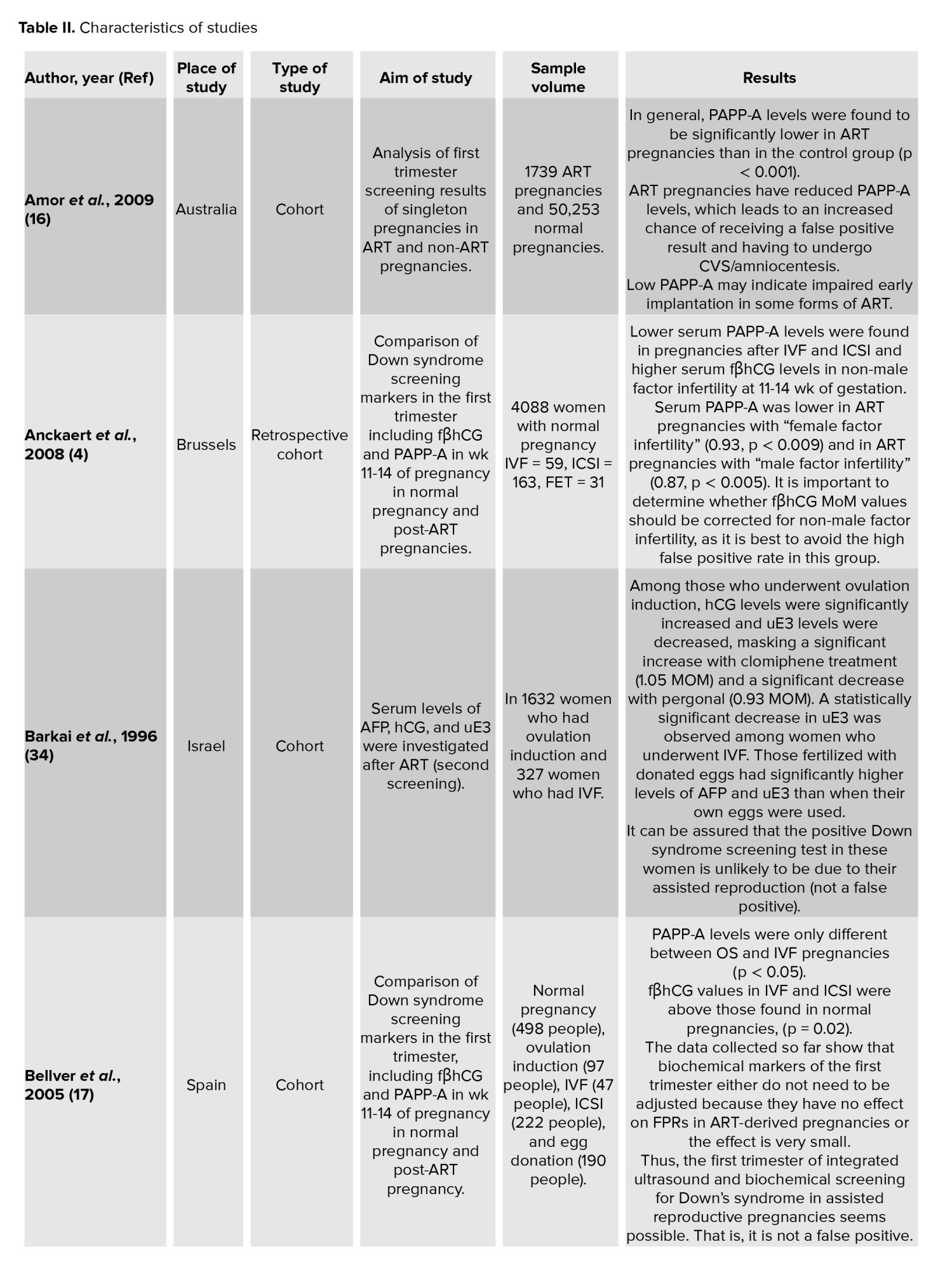
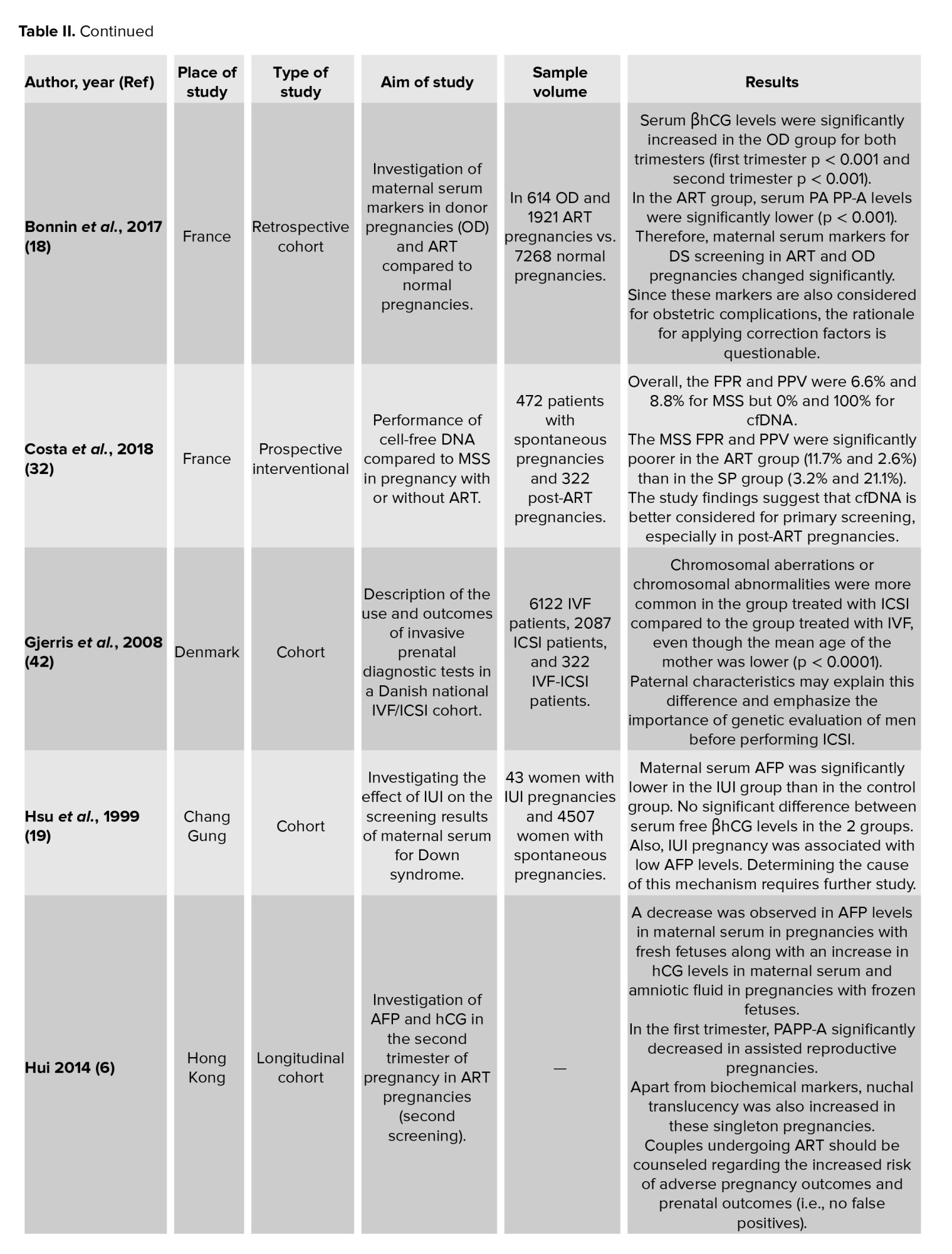
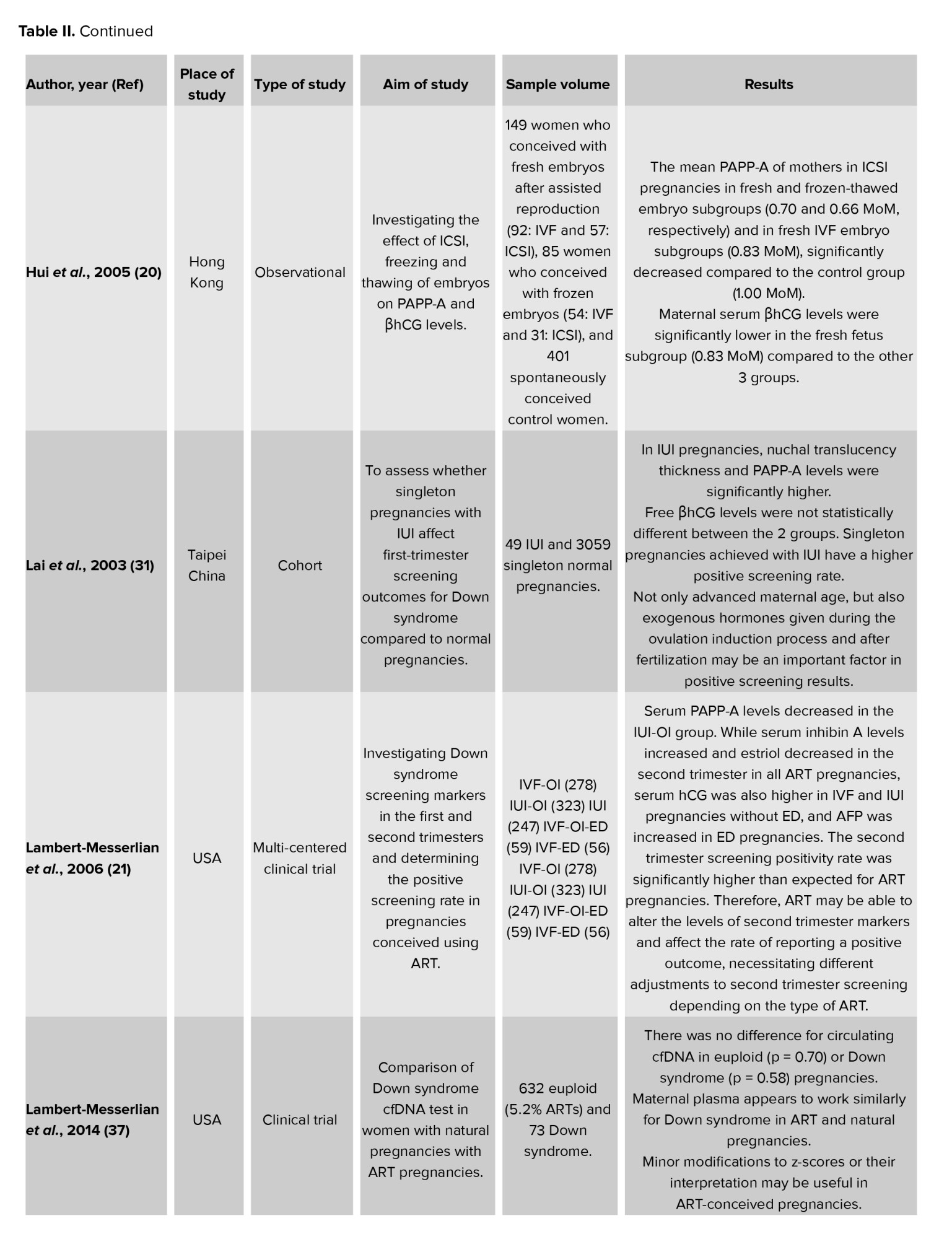
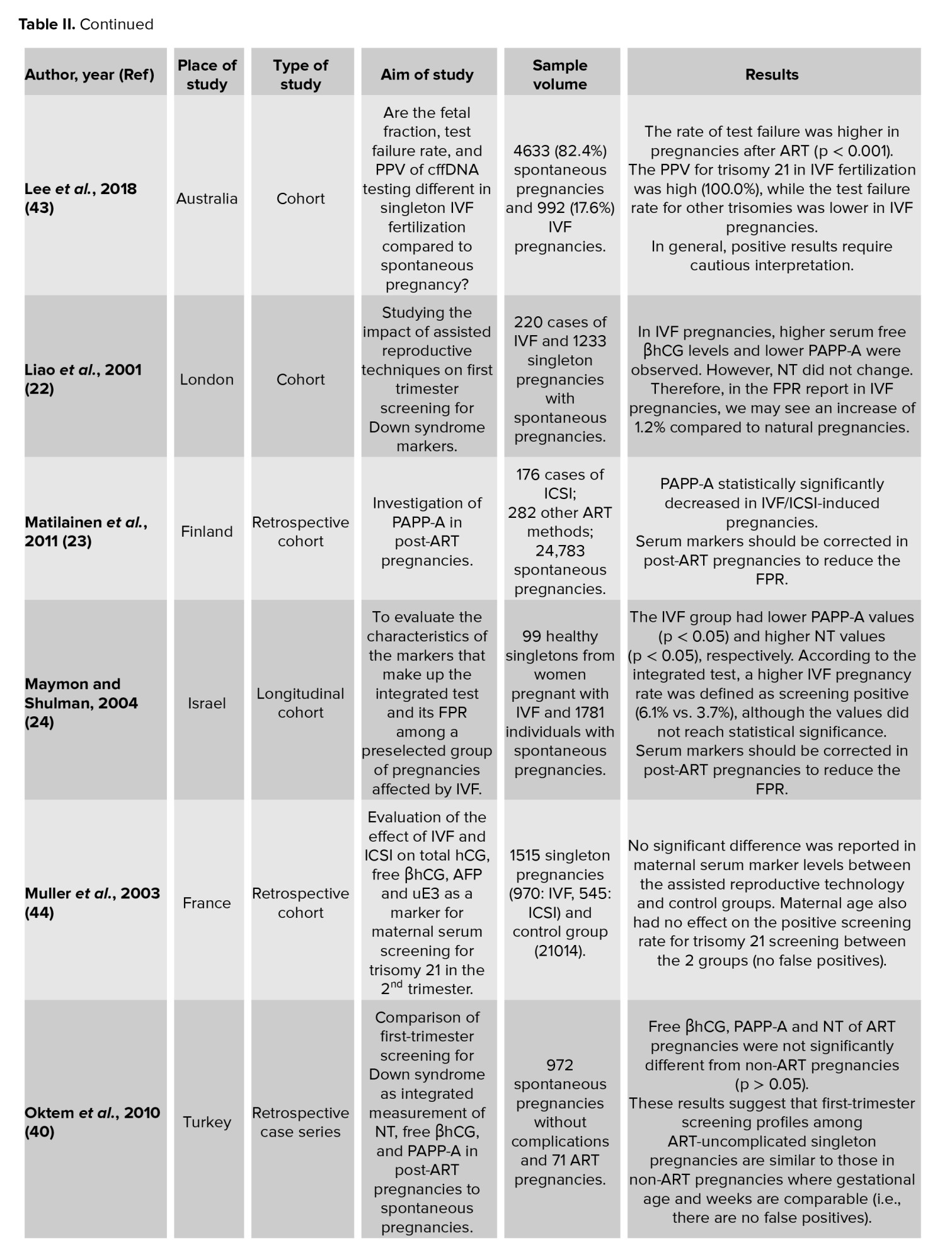
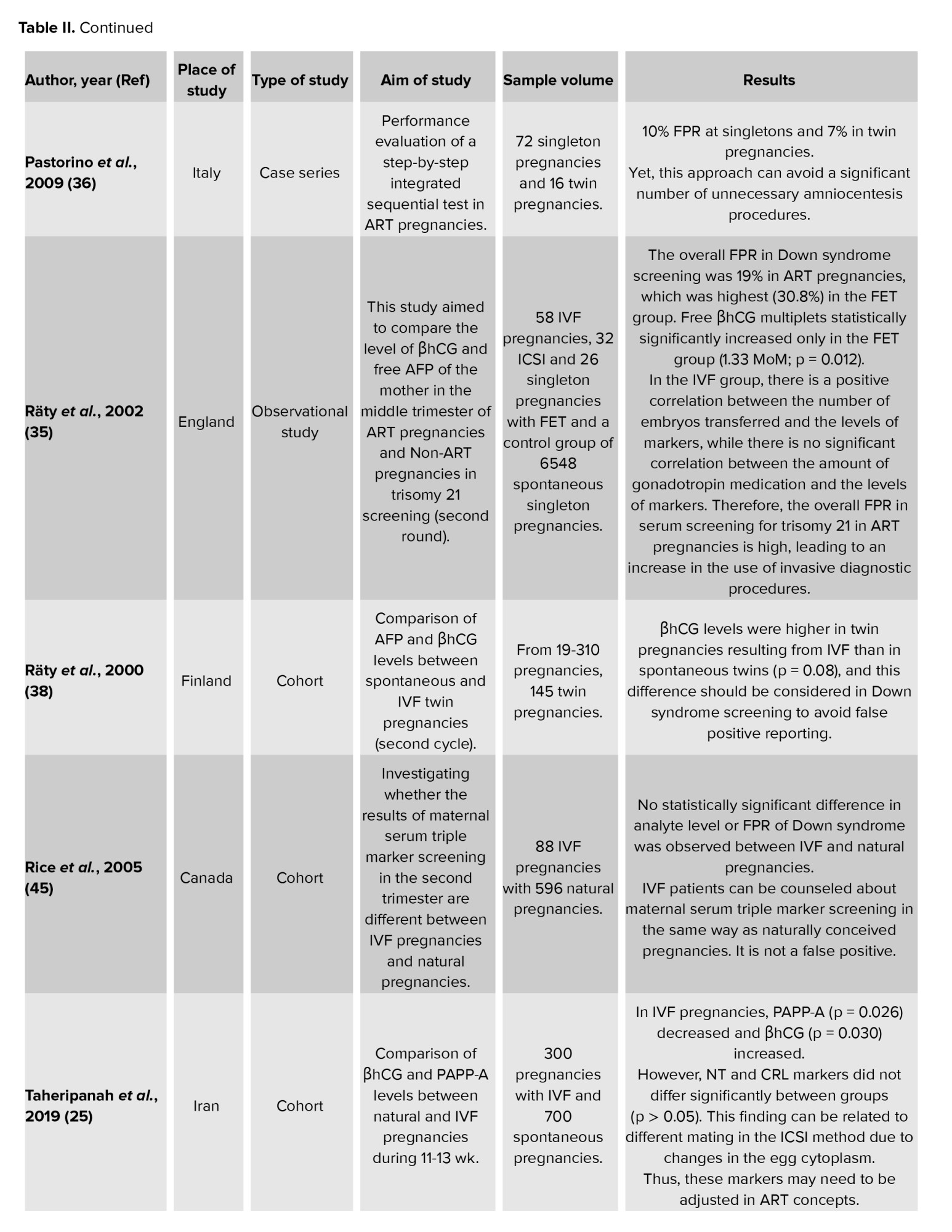
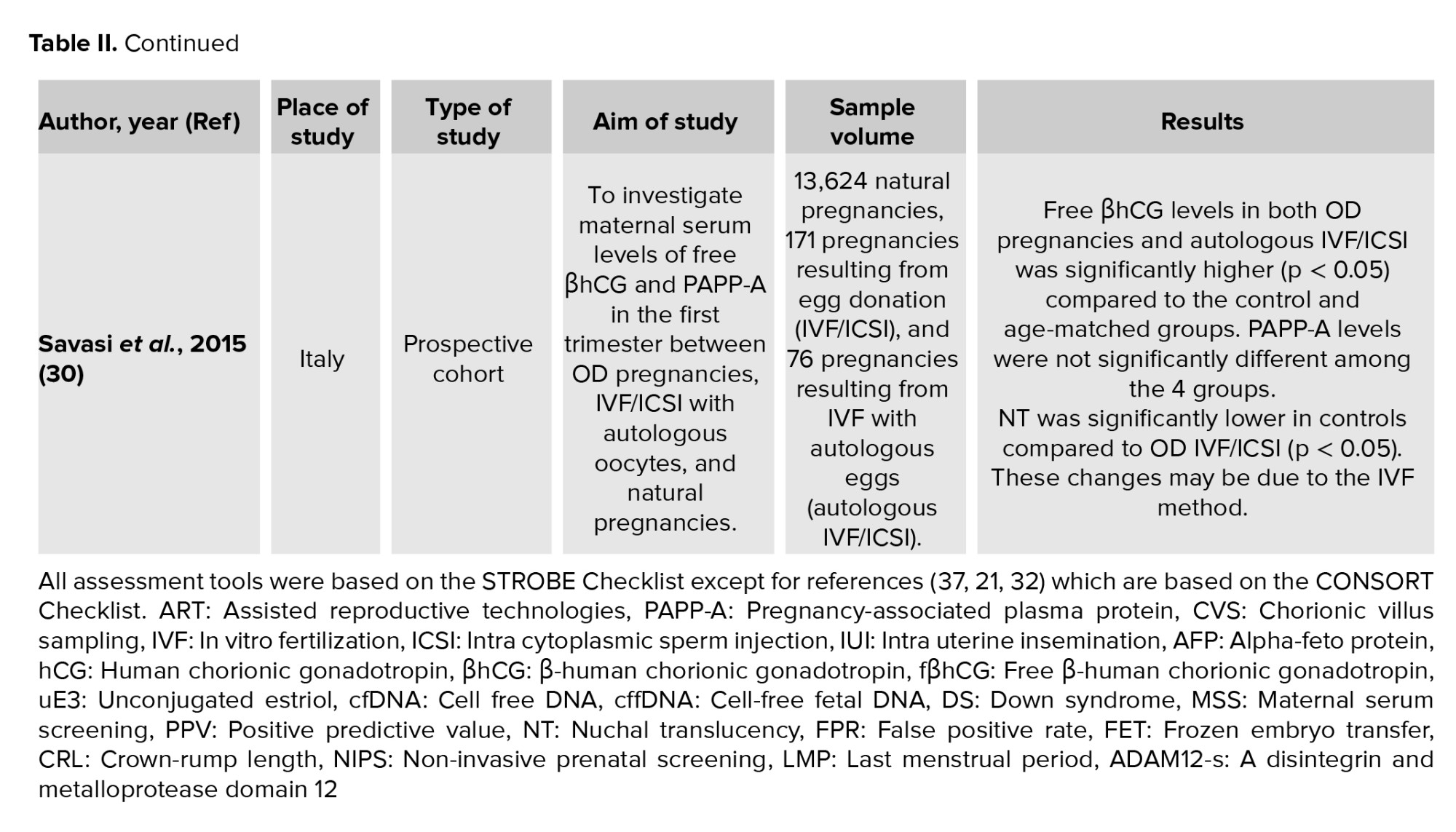
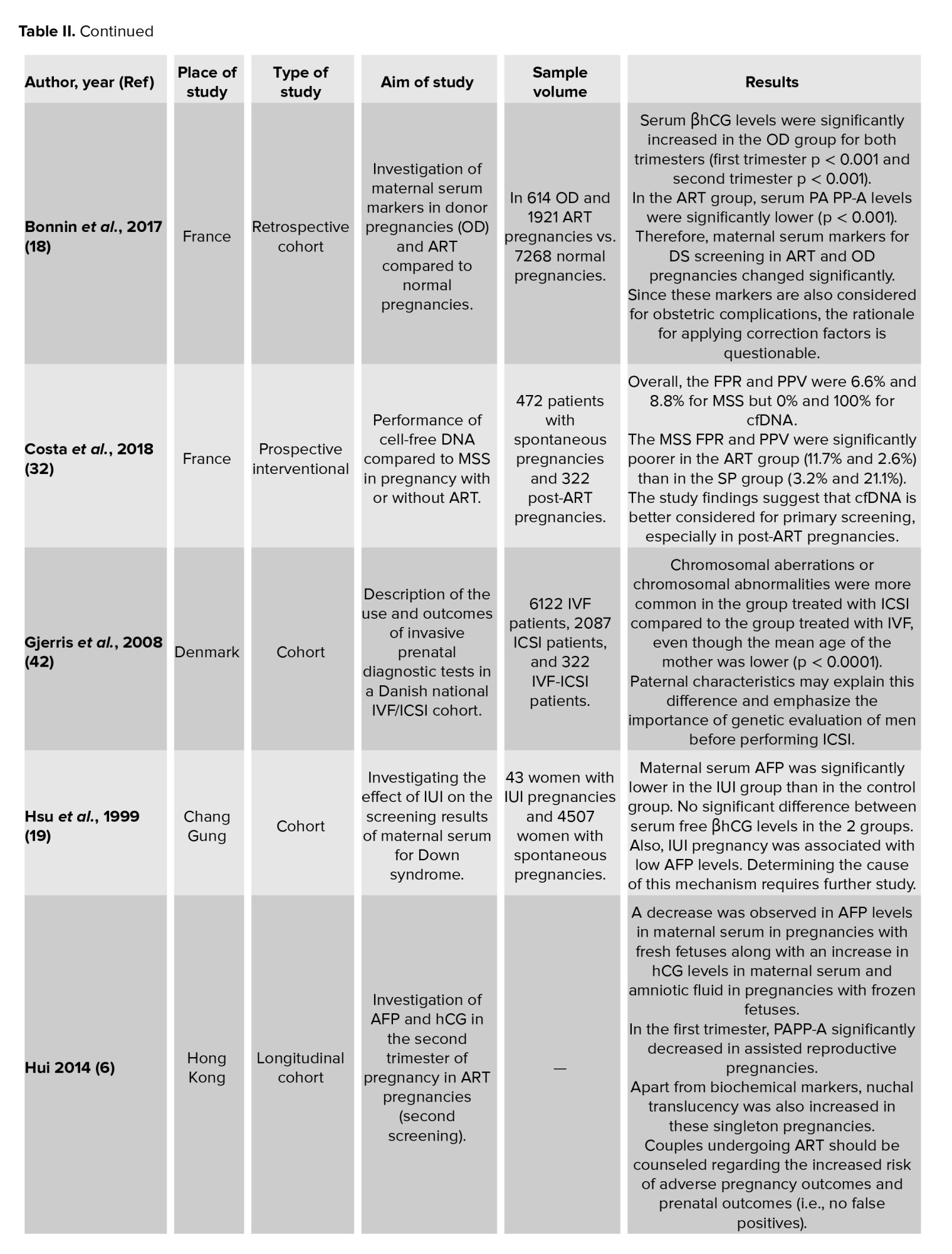
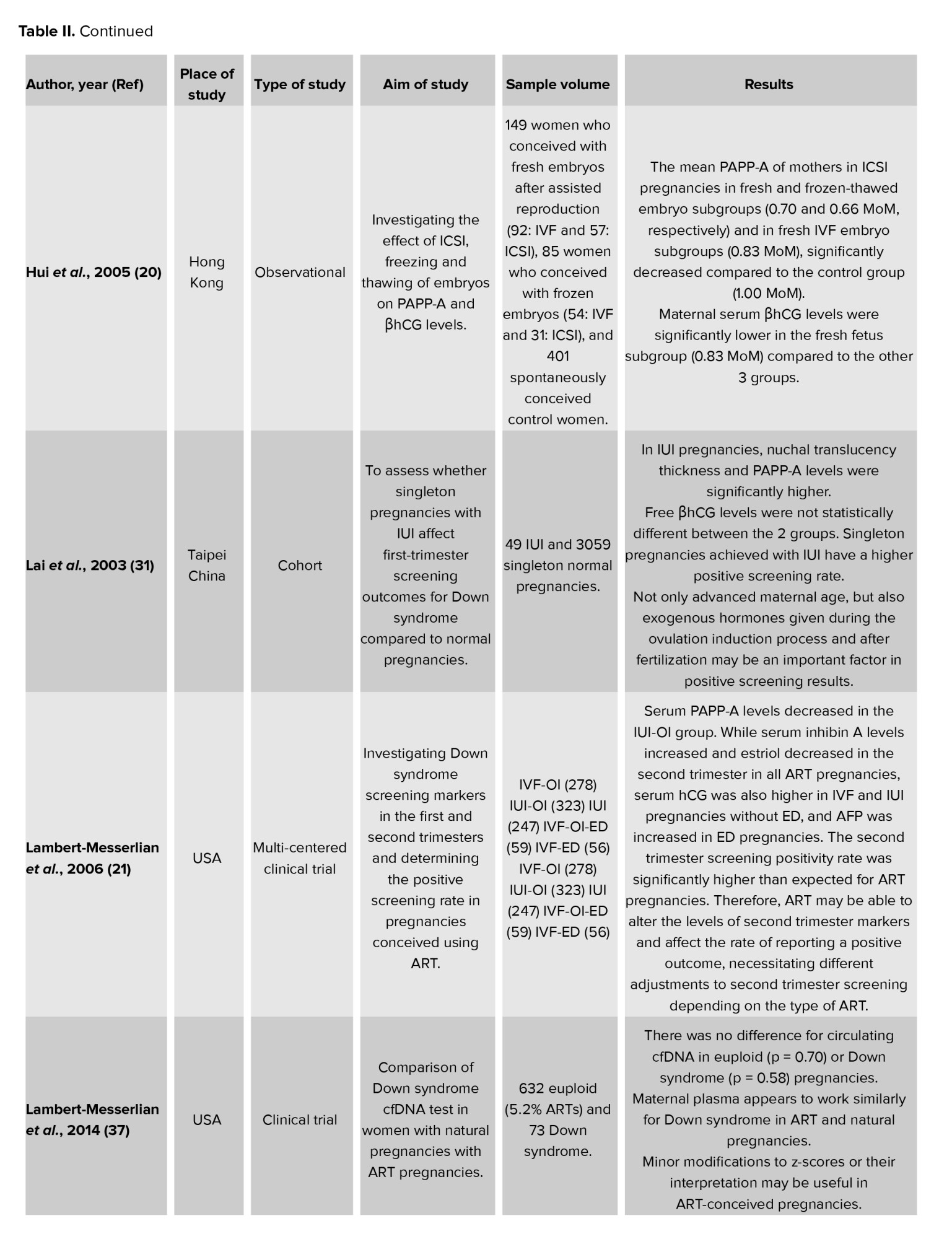
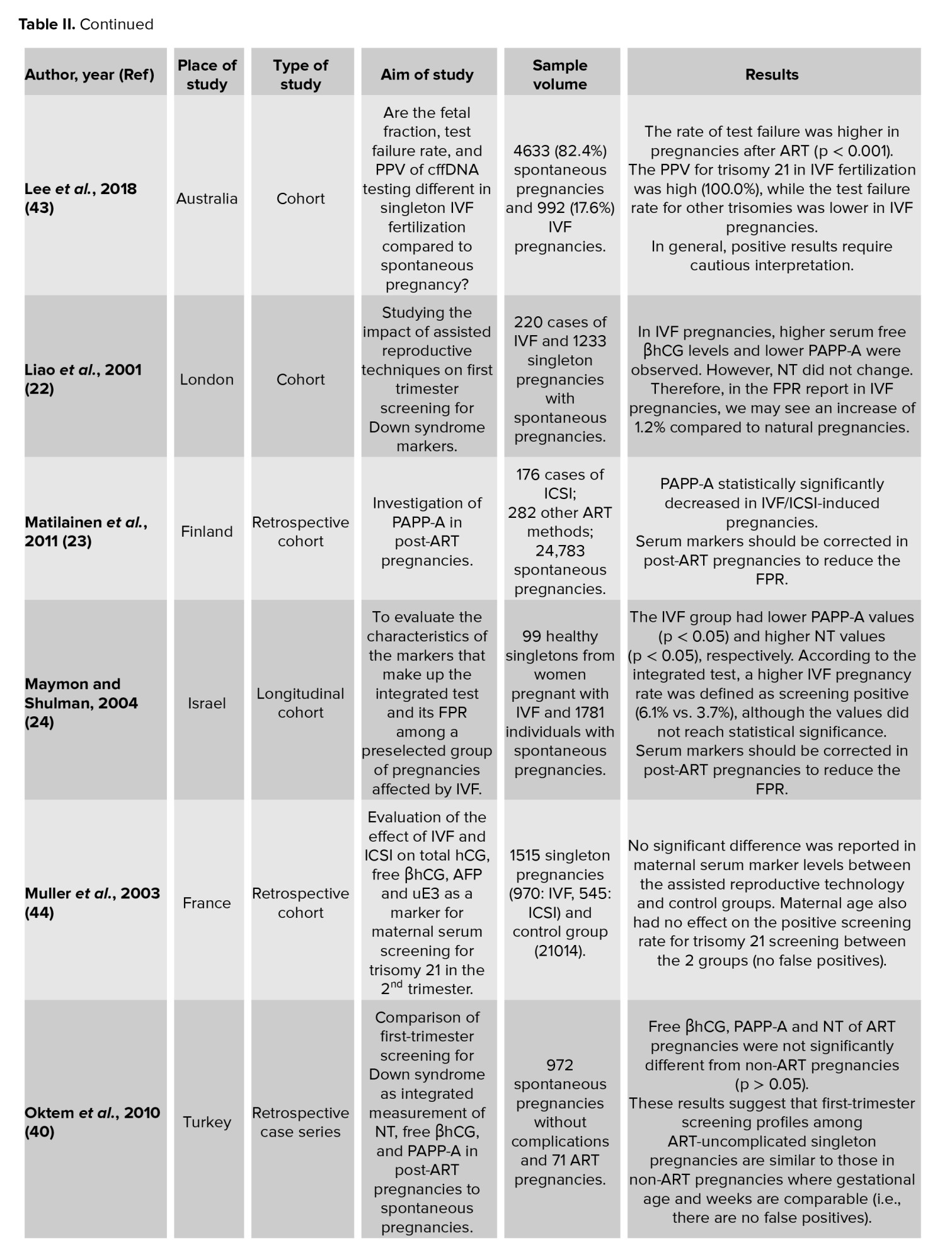
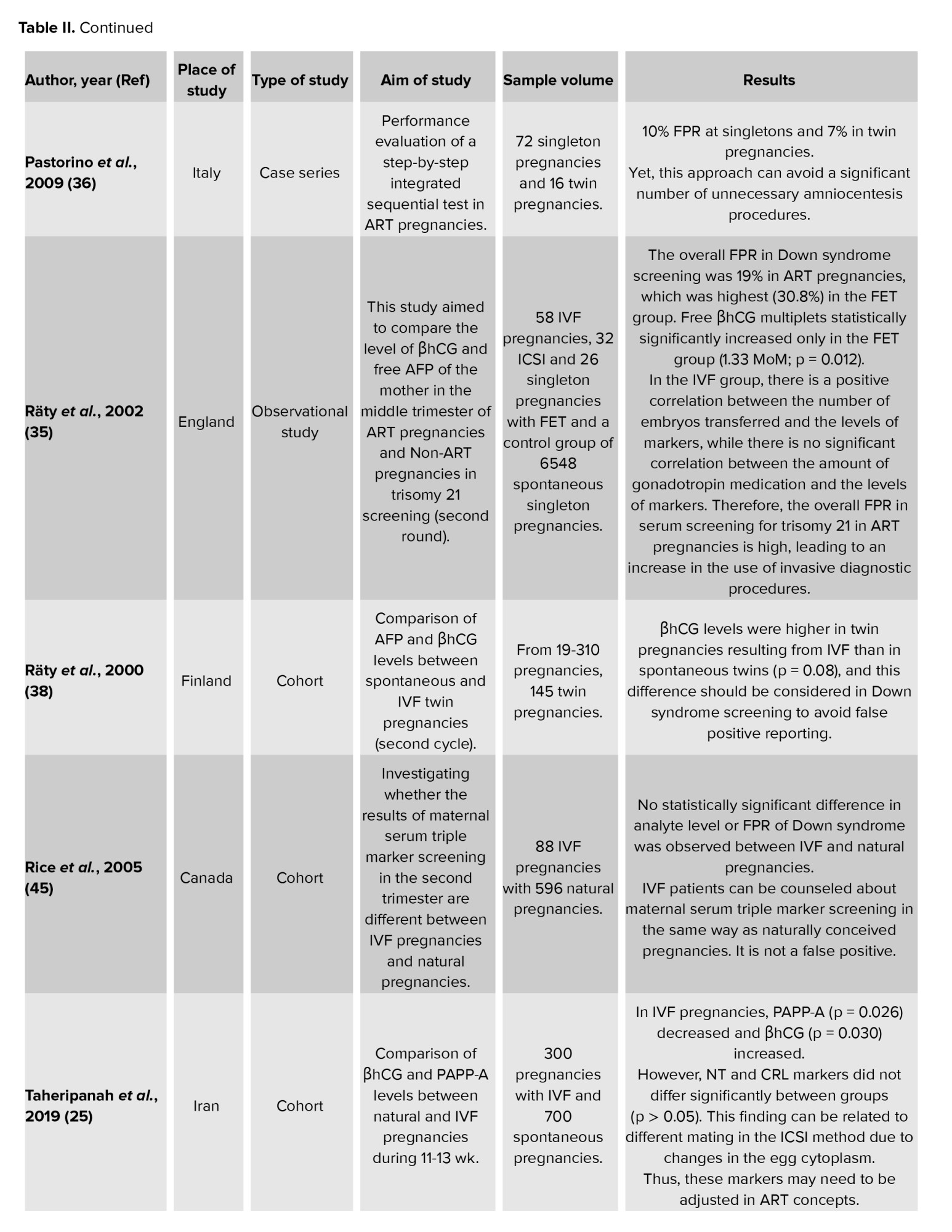
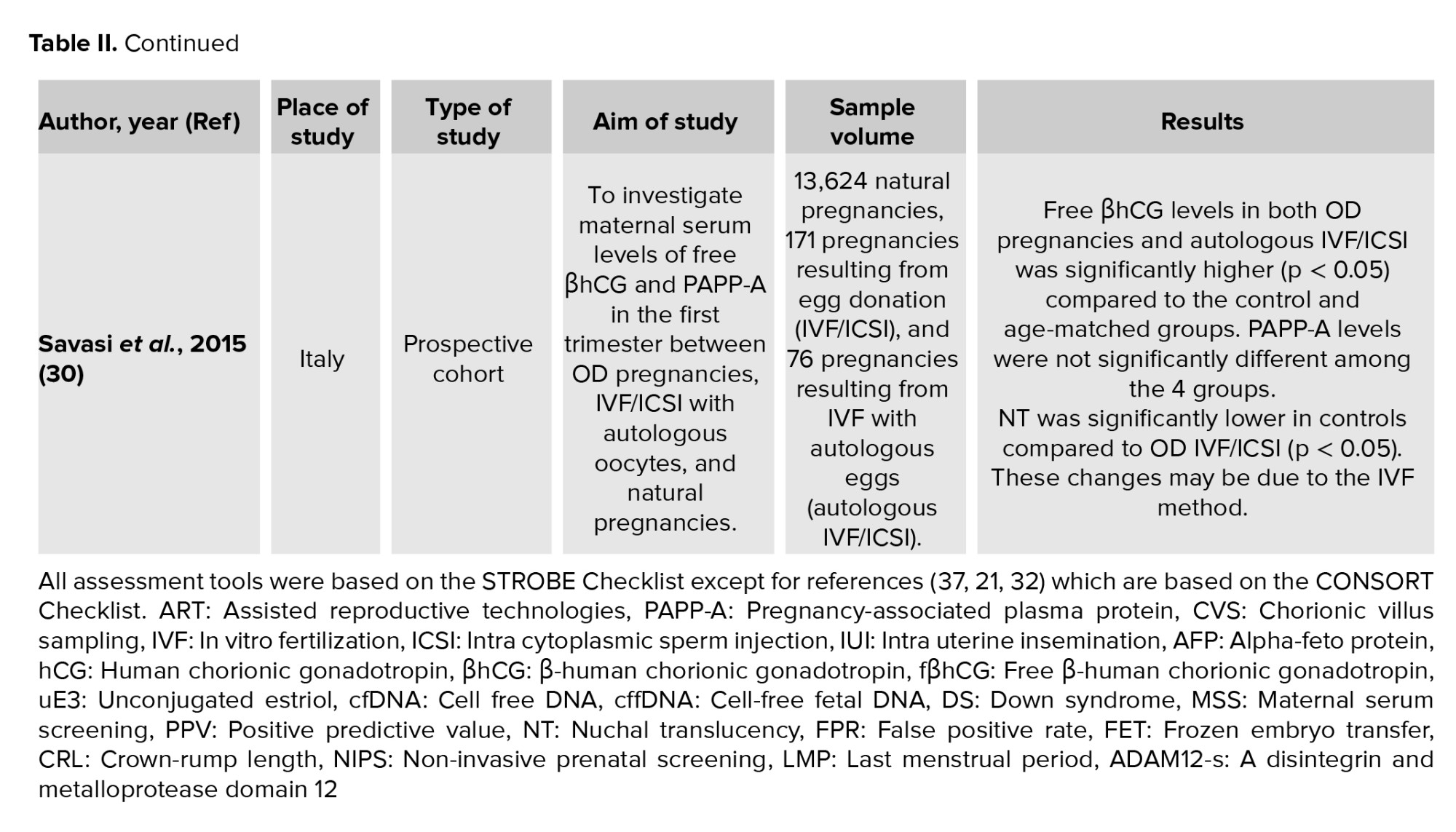
The present study is a systematic review. To determine the time interval and keywords, first, an extensive search was conducted in Persian and English in PubMed, Web of Science, Scopus, SID, and Google Scholar databases. Accordingly, to obtain a comprehensive number of documents, a search was made without applying a time limit until January 2024 (Table I). To strengthen the obtained information, the characteristics of the papers were also examined (Table II) (13). Further, to access all the information available on the subject, no limitations were considered in terms of the methodology of the papers, and every document in Persian and English that focused on prenatal screening for Down syndrome in post-ART pregnancies was considered. The papers in languages other than Persian and English were not included in the study. In addition, papers whose full text were not available or studies that focused on other trisomies, such as trisomy 13 and 18 were also excluded from the study. Based on the inclusion criteria, searching documents and evaluating the titles of the papers was carried out by one of the researchers. Then, the abstracts and titles of the resulting papers were evaluated based on the inclusion criteria by 2 other members of the research team. If 2 researchers had different opinions in evaluating the abstracts of papers, a third researcher decided on the inclusion of that paper. Subsequently, to check the quality of papers after preparing their full text, the STROBE checklist was used to evaluate descriptive studies. Besides, ‘15.5’ was considered as the minimum obtainable score for the STROBE checklist (14). The CONSORT scale quality scoring system was used for clinical trials. The total score of the scale based on these statements is 5. Papers with a score of 3 or higher were included in the study (15).
2.1. Search strategy
Down syndrome (trisomy 21) is the most prevalent chromosomal abnormality in neonates with a higher chance of survival than other chromosomal disorders. Its overall prevalence is about 10 cases per 10,000 live births around the globe (1). Due to the high costs of caring for these children and the high burden of medical, emotional, and psychological services for the family, the life quality of these people's families is also influenced (2). Thus, prenatal diagnosis of these diseases and termination of pregnancy at the right time can reduce the amount of suffering caused by their occurrence.
Among the various types of prenatal screening protocols, the most widely used during the first trimester of pregnancy is the combination of nuchal translucency (NT) measurement and serum level measurement of free beta-human chorionic gonadotropin (fβHCG) and pregnancy-associated plasma protein-A (PAPP-A), the so-called integrated screening. The most widely used second trimester screening test is the quad test, which uses the mother's age, serum beta-human chorionic gonadotropin (βHCG), alpha-fetoprotein (AFP), unconjugated estriol (uE3), and inhibin A. In the combined screening protocol, the results of the first and second trimesters are integrated, and the sensitivity of Down syndrome diagnosis reaches 94-96%. Yet, it is still associated with 5% false-positive results (3). Assisted reproductive technology (ART) pregnancies may have levels of biochemical markers that are different, especially during the second trimester, compared to spontaneous pregnancies (4). The false-positive rate for diagnosing Down syndrome after ART pregnancies is also 5% in both screening rounds (5), leading to unnecessary invasive diagnostic measures in some cases (6).
Pregnancy can be a challenging and stressful period for women who have conceived through ART (7). One of the concerns of these couples is to perform prenatal screenings because there is a possibility that the screening in these women may be wrong. In other words, it may have been a false positive, and as a result, it will cause them a lot of anxiety. Moreover, invasive diagnostic procedures such as amniocentesis and chorionic villus sampling are necessary for them (8-10). In contrast, having screening methods to detect chromosomal disorders before birth is one of the reproductive health rights of couples, and they have the right to have a healthy child (11). Interpreting the results of chromosomal disease screenings using serum and sonographic markers after ART pregnancies is challenging. Firstly, the mean age of mothers is higher than spontaneous pregnancies. Secondly, if it leads to twins or multiples, relying on the mother's serum markers may show abnormal results despite the health of the fetus (12).
Considering that the majority of chromosomal problems in pregnancies resulting from ART have not been proven so far, but the serum markers of Down syndrome have been reported in some studies to be different in pregnancies resulting from ART compared to natural pregnancies, and considering that nowadays ART includes a large group of methods that have many differences, also knowing that couples with infertility have succeeded in experiencing pregnancy after paying a lot of financial and psychological costs and have the right to health diagnostic methods before birth, and having a normal fetus and baby, this study was designed with the aim of systematic review of types of prenatal imaging and serological screenings for the diagnosis of Down's syndrome in pregnancies resulting from assisted reproductive technologies using available valid documents in order to know and correctly interpret the results of prenatal screenings in these pregnancies.
2. Materials and Methods
The present study is a systematic review. To determine the time interval and keywords, first, an extensive search was conducted in Persian and English in PubMed, Web of Science, Scopus, SID, and Google Scholar databases. Accordingly, to obtain a comprehensive number of documents, a search was made without applying a time limit until January 2024 (Table I). To strengthen the obtained information, the characteristics of the papers were also examined (Table II) (13). Further, to access all the information available on the subject, no limitations were considered in terms of the methodology of the papers, and every document in Persian and English that focused on prenatal screening for Down syndrome in post-ART pregnancies was considered. The papers in languages other than Persian and English were not included in the study. In addition, papers whose full text were not available or studies that focused on other trisomies, such as trisomy 13 and 18 were also excluded from the study. Based on the inclusion criteria, searching documents and evaluating the titles of the papers was carried out by one of the researchers. Then, the abstracts and titles of the resulting papers were evaluated based on the inclusion criteria by 2 other members of the research team. If 2 researchers had different opinions in evaluating the abstracts of papers, a third researcher decided on the inclusion of that paper. Subsequently, to check the quality of papers after preparing their full text, the STROBE checklist was used to evaluate descriptive studies. Besides, ‘15.5’ was considered as the minimum obtainable score for the STROBE checklist (14). The CONSORT scale quality scoring system was used for clinical trials. The total score of the scale based on these statements is 5. Papers with a score of 3 or higher were included in the study (15).
2.1. Search strategy
A systematic review was conducted in Persian and English in PubMed, Scopus, SID, Google Scholar, and Web of Science databases. The search was performed in PubMed using MeSh terms in combination with keywords (Downs Syndrome) or (Mongolism) or (47,XY,+21) or (47,XX,+21) or (Trisomy 21) and (screening) or (Maternal) (Serum Screening Tests) or (Prenatal Diagnosis) and (Assisted Reproductive Technique) or (Fertilization in Vitro) or (Sperm Injections, Intracytoplasmic) or (Ovulation Induction) or (Superovulation) or (Embryo Transfer) or (Donor Conception). This search strategy was adapted to other databases. For complete searching, all citations were imported into the EndNote basic database (Table I). Based on a comprehensive list of possible synonyms for each term, a search was followed up to April 2023. Synonyms combined with the conjunction "OR" and a search for all 4 characteristics together with "AND" yielded a list of sources used to search for related papers. Data extraction of eligible papers was conducted independently by 2 researchers.

2.2. Ethical Considerations

2.2. Ethical Considerations
This systematic review has been approved by the Ethics Committee of Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.RSI.REC.1403.001, project code: 17649).
3. Results
3. Results
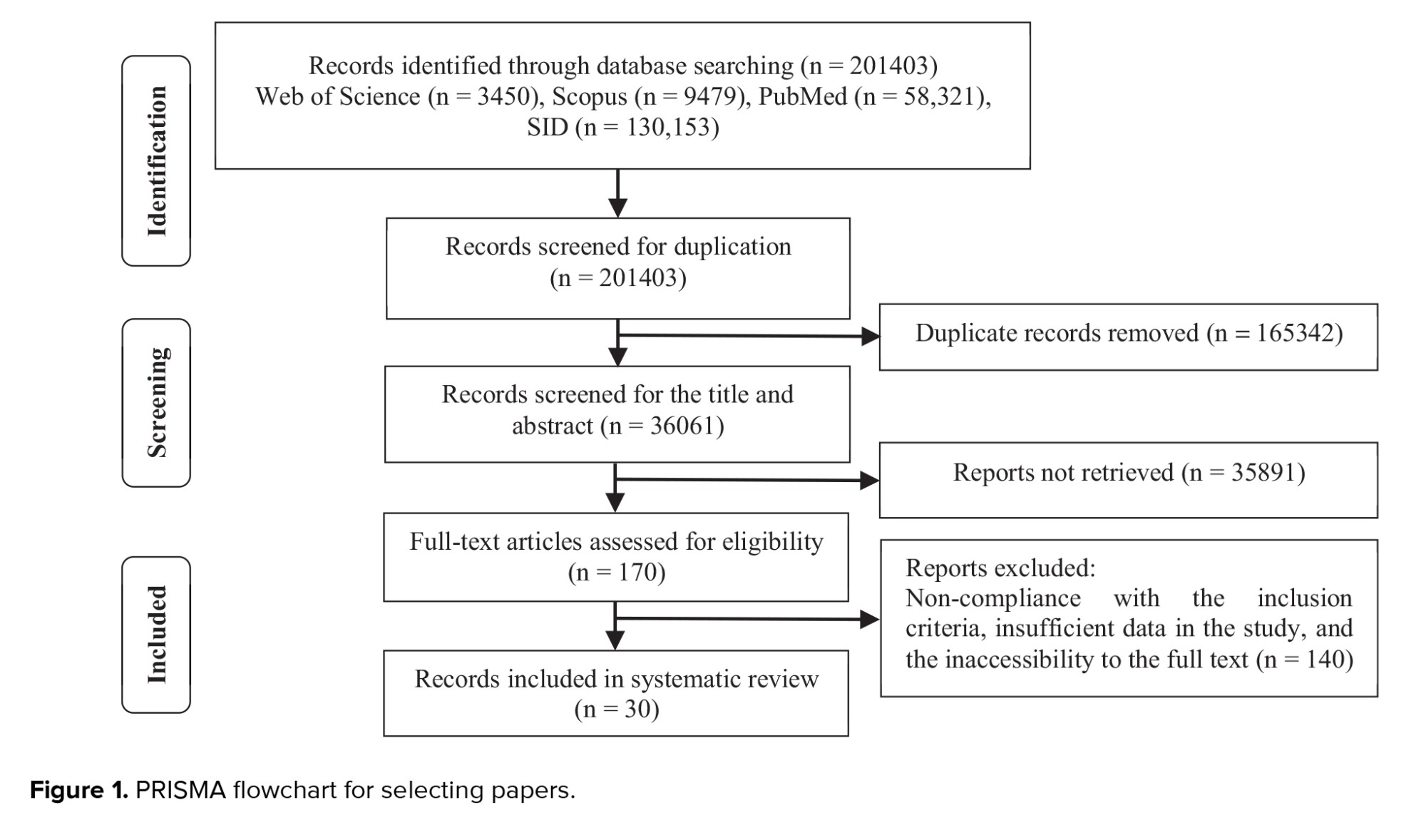
Out of 201,403 eligible articles identified, 165,342 were duplicates and were not included in the study. 2 independent reviewers evaluated the titles and abstracts of 36,061 studies. Moreover, 35,891 papers had unrelated reports and were excluded. Finally, 170 eligible papers were analyzed by both reviewers. Although some studies met the inclusion criteria, they were excluded because the full text of the article was not available. Of these papers, 140 were excluded due to insufficient data and lack of access to complete data. Thus, 30 papers were finally included in the study. The search and selection process are presented in figure 1 using the preferred reporting items for systematic reviews and meta-analyses flowchart.
3.1. First-time screenings for Down syndrome in post-ART pregnancies
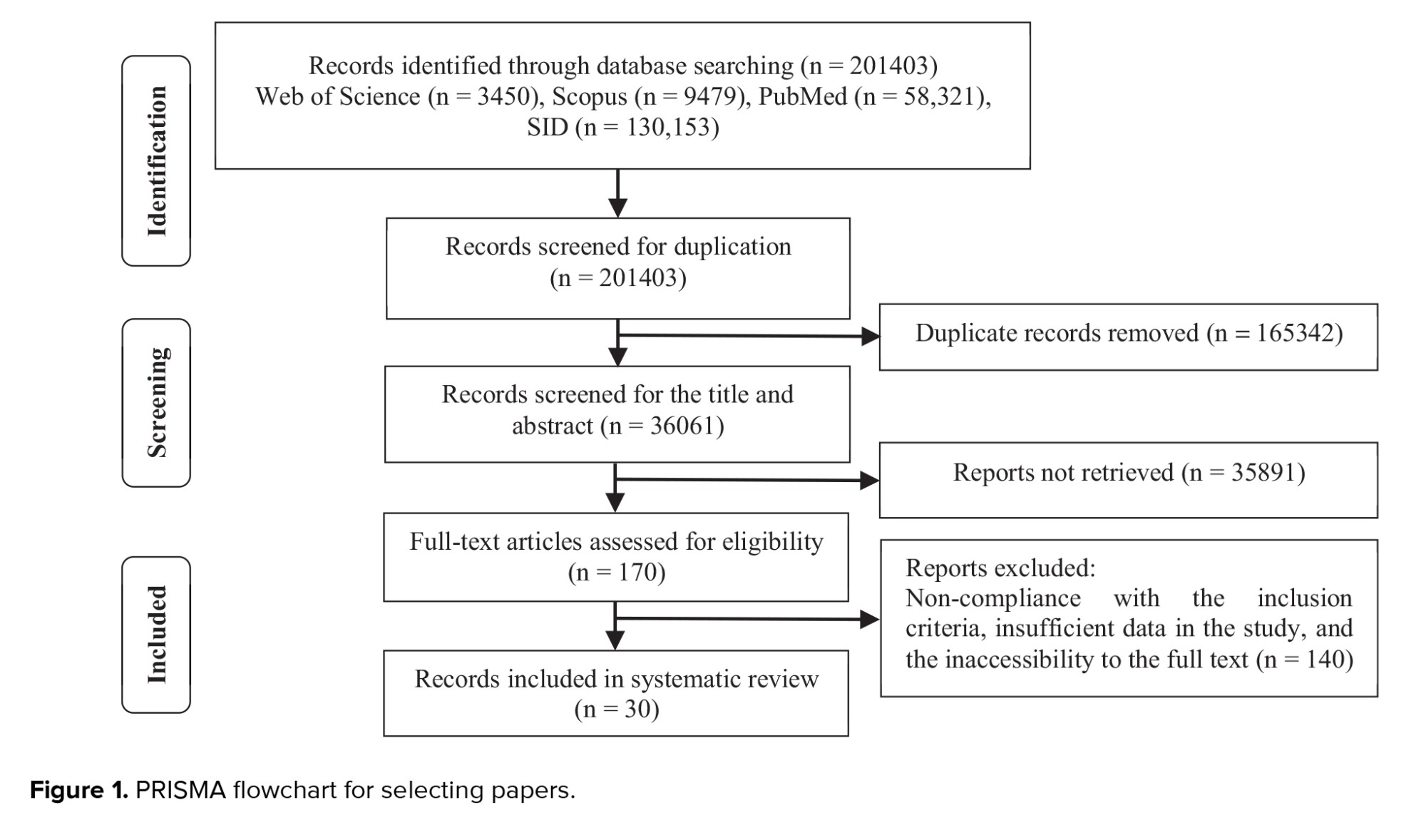
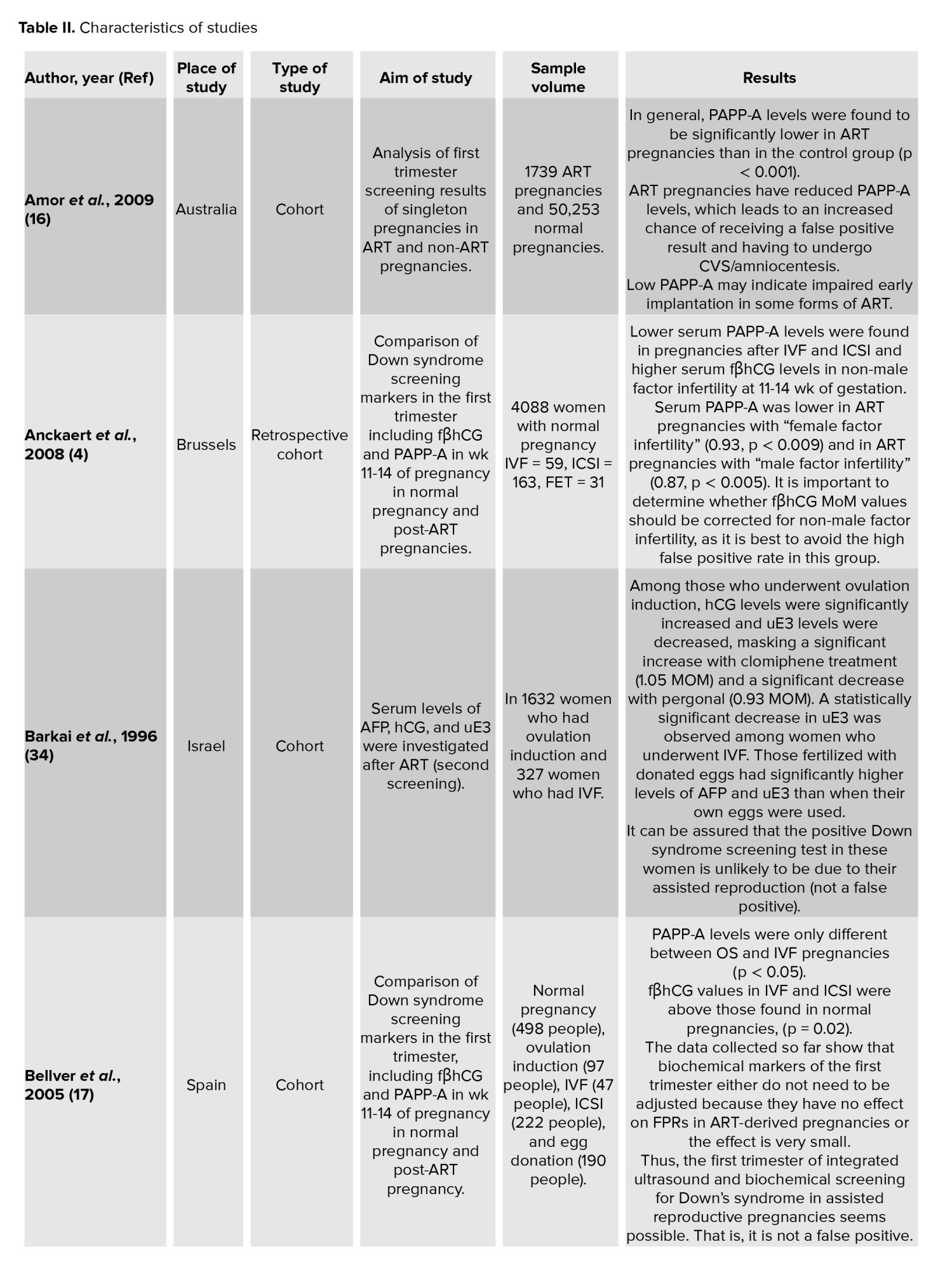
In the first screening test for Down syndrome, performed in the first trimester of gestation between 11th and 13th wk and 6 days, 2 types of measurements were used along with the mother's age to calculate the risk of Down syndrome (trisomy 21), trisomy 13 and 18. One of these measurements was through ultrasound and NT measurement, and the other was through the measurement of dual blood biomarkers, namely PAPP-A and fβhCG, while also considering the mother's age. In the past, there was another marker in the screening of the first trimester of Down syndrome, that is, the visibility of the nasal septum (nasal bone) in sonography, which is now excluded from the first screening protocol. In relation to the difference in biochemical markers between spontaneous pregnancies and post-ART pregnancies, we found that 16 studies showed statistically significant differences in reducing the PAPP-A index (abnormal values < 0.1 MOM) (4, 6, 16-29), 8 studies showed increased fβhCG index (abnormal values > 0.1 MOM) in most ART methods, especially in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) (4, 17, 18, 22, 25, 27, 28, 30) and 1 study showed an increase in the level of ADAM12-s (a disintegrin and metalloprotease) (abnormal values > 0.1 MOM) (29) in the first trimester screening; nonetheless, 5 studies rendered false-positive results as probable in the biochemical markers of the first trimester (4, 16, 21, 22, 31). An increased NT thickness (abnormal values of NT above 3 mm) was observed in 4 studies following some ART methods (6, 24, 30, 31). However, one study did not observe any difference in NT (25). These serum and ultrasound NT indicators revealed a positive screening in terms of Down syndrome. One study has recommended performing the cff DNA serum screening method (32) to reduce false-positive reports and thus prevent additional invasive tests, and one study has suggested non-invasive prenatal testing (NIPT), especially in twins (33).
3.2. Second round screenings for Down syndrome in post-ART pregnancies
The second screening test for Down syndrome was performed at the gestational age of 14 wk and 1 day to 20 wk by measuring 4 blood biomarkers (quad markers) including βhCG, uE3, inhibin A, and AFP. Regarding the difference in biochemical markers between spontaneous pregnancies and post-ART pregnancies, 4 studies reported an increase in βhCG (abnormal values > 0.1 MOM) (6, 21, 34, 35), 2 studies indicated a decrease in uE3 (abnormal values < 0.1 MOM) (21, 34), 2 studies reported a decrease in AFP (abnormal values < 0.1 MOM) (6, 19), and 2 studies indicated increased inhibin A (abnormal values > 0.1 MOM) (21, 26) in the second round of screening in post-ART pregnancies. Nevertheless, 3 studies considered false-positive results of the second screening biomarkers of Down syndrome as possible (21, 34, 35). Following these false positive results, 1 study performed a consecutive integrated test (36) and 10 studies suggested the correction of defined values for Down syndrome serum markers in ART pregnancies (4, 18, 21, 24, 25, 27, 29, 35-38). Yet, 5 studies did not consider the reported results to be false positives and did not see the need to adjust in serum markers; they did not report any difference in diagnostic screenings between spontaneous pregnancies and post-ART pregnancies (17, 34, 39-41). Even Hui stated in their study that couples undergoing ART should be counseled regarding the increased risk of adverse pregnancy outcomes and prenatal outcomes (6).

4. Discussion
3.1. First-time screenings for Down syndrome in post-ART pregnancies
In the first screening test for Down syndrome, performed in the first trimester of gestation between 11th and 13th wk and 6 days, 2 types of measurements were used along with the mother's age to calculate the risk of Down syndrome (trisomy 21), trisomy 13 and 18. One of these measurements was through ultrasound and NT measurement, and the other was through the measurement of dual blood biomarkers, namely PAPP-A and fβhCG, while also considering the mother's age. In the past, there was another marker in the screening of the first trimester of Down syndrome, that is, the visibility of the nasal septum (nasal bone) in sonography, which is now excluded from the first screening protocol. In relation to the difference in biochemical markers between spontaneous pregnancies and post-ART pregnancies, we found that 16 studies showed statistically significant differences in reducing the PAPP-A index (abnormal values < 0.1 MOM) (4, 6, 16-29), 8 studies showed increased fβhCG index (abnormal values > 0.1 MOM) in most ART methods, especially in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) (4, 17, 18, 22, 25, 27, 28, 30) and 1 study showed an increase in the level of ADAM12-s (a disintegrin and metalloprotease) (abnormal values > 0.1 MOM) (29) in the first trimester screening; nonetheless, 5 studies rendered false-positive results as probable in the biochemical markers of the first trimester (4, 16, 21, 22, 31). An increased NT thickness (abnormal values of NT above 3 mm) was observed in 4 studies following some ART methods (6, 24, 30, 31). However, one study did not observe any difference in NT (25). These serum and ultrasound NT indicators revealed a positive screening in terms of Down syndrome. One study has recommended performing the cff DNA serum screening method (32) to reduce false-positive reports and thus prevent additional invasive tests, and one study has suggested non-invasive prenatal testing (NIPT), especially in twins (33).
3.2. Second round screenings for Down syndrome in post-ART pregnancies
The second screening test for Down syndrome was performed at the gestational age of 14 wk and 1 day to 20 wk by measuring 4 blood biomarkers (quad markers) including βhCG, uE3, inhibin A, and AFP. Regarding the difference in biochemical markers between spontaneous pregnancies and post-ART pregnancies, 4 studies reported an increase in βhCG (abnormal values > 0.1 MOM) (6, 21, 34, 35), 2 studies indicated a decrease in uE3 (abnormal values < 0.1 MOM) (21, 34), 2 studies reported a decrease in AFP (abnormal values < 0.1 MOM) (6, 19), and 2 studies indicated increased inhibin A (abnormal values > 0.1 MOM) (21, 26) in the second round of screening in post-ART pregnancies. Nevertheless, 3 studies considered false-positive results of the second screening biomarkers of Down syndrome as possible (21, 34, 35). Following these false positive results, 1 study performed a consecutive integrated test (36) and 10 studies suggested the correction of defined values for Down syndrome serum markers in ART pregnancies (4, 18, 21, 24, 25, 27, 29, 35-38). Yet, 5 studies did not consider the reported results to be false positives and did not see the need to adjust in serum markers; they did not report any difference in diagnostic screenings between spontaneous pregnancies and post-ART pregnancies (17, 34, 39-41). Even Hui stated in their study that couples undergoing ART should be counseled regarding the increased risk of adverse pregnancy outcomes and prenatal outcomes (6).

4. Discussion
The present study systematically reviewed all types of prenatal imaging and serum screenings for the diagnosis of Down syndrome in ART pregnancies to know and correctly interpret the results of prenatal screenings in these pregnancies. In the quality assessment of the descriptive studies included in this review, all the studies were of excellent quality and their score was higher than 16; the studies with moderate and poor quality were excluded from this systematic review. Nonetheless, review papers with similar titles did not pay attention to the quality of the included papers (46, 47).
Based on the results of the studies, prenatal screenings for Down syndrome in ART pregnancies can be divided into 2 categories: "first round screening" and "second round screening."
In the first-round screening after most types of ART methods, PAPP-A was significantly lower than spontaneous pregnancies, while free βhCG was significantly higher, especially in IVF and ICSI methods. Some studies also indicated an increase in NT in ART pregnancies. Regarding the biochemical markers of the second-round screening of Down syndrome, an increase in inhibin A and a decrease in AFP and UE3 are evident in some studies. These markers, which cause the Down syndrome screening test to be positive, can be present in ART pregnancies due to the presence of exogenous ovulation-stimulating hormones, the presence of multiple corpora lutea, twins or multiplets, the type of IVF method, and changes in the egg cytoplasm in the ICSI method.
This imposes unnecessary adjunct invasive procedures on the mother. Some studies have suggested screening through NIPT, cell-free DNA, or an integrated screening test to solve this false positive. Some others have also recommended the modification and adjustment of serum markers in Down syndrome screening for these mothers. The American College of Medical Genetics and Genomics has recommended the NIPT method for the diagnosis of trisomy 21, 18, and 13 as an alternative to traditional biochemical screening tests (48).
Nevertheless, there are false positives in these 2 methods. The American College of Obstetricians and Gynecologists and the Gynecologists' Committee on Genetics (2012) acknowledge that since cell-free DNA originates from the placenta and in sporadic cases as when the mass of the placenta is larger for some reason after ART, its values may be reported as falsely higher (43).
Among significant issues in the interpretation of screening tests for chromosomal disorders is that patients who refer for ART are usually older than those who conceive spontaneously. Hence, it is more likely that the mother carries a fetus with chromosomal disorders (49, 50). Another point is that among the types of ART methods, the ICSI method has a higher risk of transmitting chromosomal abnormalities; this issue emphasizes the importance of genetic evaluation of men before performing this method, because paternal characteristics may be the main reason for these chromosomal abnormalities (42).
These complications, along with reporting false-positive results, can raise the level of stress and anxiety in patients and doctors. Yet, in many cases, everything is normal and due to placental and corpus luteum disorders or differences in the type of method used; the results have been falsely positive. Some studies suggest that high fβHCG and low PAPP-A in cases where there are pregnancy complications, such as pre-eclampsia and fetal growth restriction can evidently be a sign of an abnormal placenta and explain the reason for the false positive of the Down syndrome test (26, 30, 51, 52).
Adjustment of biochemical markers for conception type is already included in the aneuploidy risk assessment algorithm by FMF (www.fetalmedicine.org); however, to optimize the performance of the screening test, the concentration of free βhCG and PAPP-A should be adjusted differently for each ART method. Regarding IVF and ICSI, such settings may especially limit false positives due to increased free βhCG and decreased PAPP-A. This may diminish the use of additional invasive methods that may impose additional costs on the couple and even lead to the risk of miscarriage and abortion (4, 18, 21, 23-25, 27, 29, 35, 37, 38, 53).
Smith-Bindman et al. by reviewing the meta-analysis of 56 articles and 1930 fetuses regarding prenatal ultrasound examination of Down syndrome in fetuses in the population of pregnant women, they concluded that although NT examination can be effective in prenatal diagnosis of Down syndrome fetuses, the overall sensitivity of this finding for it is too low to be a practical screening test in cases where the fetus has no associated structural abnormalities for Down syndrome. The use of these markers as a basis for the decision to perform amniocentesis leads to more fetal losses than in cases of Down syndrome and leads to a decrease in the prenatal diagnosis of fetuses with Down syndrome (54). This study is similar to the present study in terms of prenatal sonographic markers of Down syndrome in fetuses, but our study considered both serum and imaging markers and limited it to the population of women whose pregnancy was the result of ART.
Also, Cavoretto et al. conducted a systematic review and meta-analysis on Down syndrome diagnosis markers including NT, free βhCG, and PAPP-A in IVF/ICSI pregnancies and reported similar results to the present study, that is, differences among the serum markers of prenatal diagnosis in ART pregnancies. They reported that free βhCG values were slightly higher in the ICSI group and PAPP-A values were slightly lower in the ICSI group, and also stated that these results may be due to changes in the placenta in ART pregnancies (55). The difference between the present study and this study is that we included a wider range of serum and imaging markers in both screening sessions in all types of ART methods in the study and we did a systematic review of the results of all of them and the need for different settings. We proposed the values of the markers mentioned in prenatal screenings for Down syndrome in pregnancies resulting from ART to reduce false-positive results and avoid the need for invasive diagnostic procedures. But due to the heterogeneity of the studies, it was only possible for the researchers to conduct a systematic review.
4.1. Strengths and limitations
One of the strengths of the present systematic review was that it was the first systematic review that evaluated both serum and sonographic markers in both screening rounds for prenatal diagnosis of Down syndrome in post-ART pregnancies. However, due to the limitation of the data of the studies included in the present review, it was not possible to conduct a meta-analysis.
It is suggested to carry out future research in the form of a meta-analysis review to investigate the definitive effect of each type of assisted reproduction method on serum and sonographic markers in the prenatal diagnosis of Down syndrome.
The knowledge translation of this study can be prepared in the form of an educational materials (educational pamphlet, video, and like these) for the awareness of service providers to enhance cautious interpretation and the method of transferring information about the results of the first and second trimester screenings for prenatal diagnosis of Down syndrome in ART pregnancies to couples as well as ART service customers.
5. Conclusion
Based on the results of the studies, prenatal screenings for Down syndrome in ART pregnancies can be divided into 2 categories: "first round screening" and "second round screening."
In the first-round screening after most types of ART methods, PAPP-A was significantly lower than spontaneous pregnancies, while free βhCG was significantly higher, especially in IVF and ICSI methods. Some studies also indicated an increase in NT in ART pregnancies. Regarding the biochemical markers of the second-round screening of Down syndrome, an increase in inhibin A and a decrease in AFP and UE3 are evident in some studies. These markers, which cause the Down syndrome screening test to be positive, can be present in ART pregnancies due to the presence of exogenous ovulation-stimulating hormones, the presence of multiple corpora lutea, twins or multiplets, the type of IVF method, and changes in the egg cytoplasm in the ICSI method.
This imposes unnecessary adjunct invasive procedures on the mother. Some studies have suggested screening through NIPT, cell-free DNA, or an integrated screening test to solve this false positive. Some others have also recommended the modification and adjustment of serum markers in Down syndrome screening for these mothers. The American College of Medical Genetics and Genomics has recommended the NIPT method for the diagnosis of trisomy 21, 18, and 13 as an alternative to traditional biochemical screening tests (48).
Nevertheless, there are false positives in these 2 methods. The American College of Obstetricians and Gynecologists and the Gynecologists' Committee on Genetics (2012) acknowledge that since cell-free DNA originates from the placenta and in sporadic cases as when the mass of the placenta is larger for some reason after ART, its values may be reported as falsely higher (43).
Among significant issues in the interpretation of screening tests for chromosomal disorders is that patients who refer for ART are usually older than those who conceive spontaneously. Hence, it is more likely that the mother carries a fetus with chromosomal disorders (49, 50). Another point is that among the types of ART methods, the ICSI method has a higher risk of transmitting chromosomal abnormalities; this issue emphasizes the importance of genetic evaluation of men before performing this method, because paternal characteristics may be the main reason for these chromosomal abnormalities (42).
These complications, along with reporting false-positive results, can raise the level of stress and anxiety in patients and doctors. Yet, in many cases, everything is normal and due to placental and corpus luteum disorders or differences in the type of method used; the results have been falsely positive. Some studies suggest that high fβHCG and low PAPP-A in cases where there are pregnancy complications, such as pre-eclampsia and fetal growth restriction can evidently be a sign of an abnormal placenta and explain the reason for the false positive of the Down syndrome test (26, 30, 51, 52).
Adjustment of biochemical markers for conception type is already included in the aneuploidy risk assessment algorithm by FMF (www.fetalmedicine.org); however, to optimize the performance of the screening test, the concentration of free βhCG and PAPP-A should be adjusted differently for each ART method. Regarding IVF and ICSI, such settings may especially limit false positives due to increased free βhCG and decreased PAPP-A. This may diminish the use of additional invasive methods that may impose additional costs on the couple and even lead to the risk of miscarriage and abortion (4, 18, 21, 23-25, 27, 29, 35, 37, 38, 53).
Smith-Bindman et al. by reviewing the meta-analysis of 56 articles and 1930 fetuses regarding prenatal ultrasound examination of Down syndrome in fetuses in the population of pregnant women, they concluded that although NT examination can be effective in prenatal diagnosis of Down syndrome fetuses, the overall sensitivity of this finding for it is too low to be a practical screening test in cases where the fetus has no associated structural abnormalities for Down syndrome. The use of these markers as a basis for the decision to perform amniocentesis leads to more fetal losses than in cases of Down syndrome and leads to a decrease in the prenatal diagnosis of fetuses with Down syndrome (54). This study is similar to the present study in terms of prenatal sonographic markers of Down syndrome in fetuses, but our study considered both serum and imaging markers and limited it to the population of women whose pregnancy was the result of ART.
Also, Cavoretto et al. conducted a systematic review and meta-analysis on Down syndrome diagnosis markers including NT, free βhCG, and PAPP-A in IVF/ICSI pregnancies and reported similar results to the present study, that is, differences among the serum markers of prenatal diagnosis in ART pregnancies. They reported that free βhCG values were slightly higher in the ICSI group and PAPP-A values were slightly lower in the ICSI group, and also stated that these results may be due to changes in the placenta in ART pregnancies (55). The difference between the present study and this study is that we included a wider range of serum and imaging markers in both screening sessions in all types of ART methods in the study and we did a systematic review of the results of all of them and the need for different settings. We proposed the values of the markers mentioned in prenatal screenings for Down syndrome in pregnancies resulting from ART to reduce false-positive results and avoid the need for invasive diagnostic procedures. But due to the heterogeneity of the studies, it was only possible for the researchers to conduct a systematic review.
4.1. Strengths and limitations
One of the strengths of the present systematic review was that it was the first systematic review that evaluated both serum and sonographic markers in both screening rounds for prenatal diagnosis of Down syndrome in post-ART pregnancies. However, due to the limitation of the data of the studies included in the present review, it was not possible to conduct a meta-analysis.
It is suggested to carry out future research in the form of a meta-analysis review to investigate the definitive effect of each type of assisted reproduction method on serum and sonographic markers in the prenatal diagnosis of Down syndrome.
The knowledge translation of this study can be prepared in the form of an educational materials (educational pamphlet, video, and like these) for the awareness of service providers to enhance cautious interpretation and the method of transferring information about the results of the first and second trimester screenings for prenatal diagnosis of Down syndrome in ART pregnancies to couples as well as ART service customers.
5. Conclusion
This systematic review found differences in the level of biochemical markers of Down syndrome screening and NT between ART pregnancies and spontaneous pregnancies, which can be due to various reasons such as placental disorders, corpus luteum multiplicity, and the type of ART method. Ultimately, these factors may cause false positive results, imposing aggressive procedures on these women for accurate diagnosis. Consequently, to optimize the performance of the screening test, the concentration of maternal serum markers such as free βhCG and PAPP-A, should be set differently for each ART method, especially between IVF and ICSI. However, more research is needed for strategies to reduce false positives in ART pregnancies.
Data Availability
Not applicable.
Author Contributions
FZ. Meamar: Searching in databases, writing proposals, writing the manuscript. M. Savabi-Esfahani: Searching in databases, writing the manuscript. T. Farajkhoda: Searching in databases, writing the proposal, and writing the manuscript.
Acknowledgments
In this research, artificial intelligence was not used in any of the stages of writing, translating, editing, checking grammar, etc. The authors would like to thank all the researchers whose papers were used in this systematic review.
Conflict of Interest
The authors declare that there is no conflict of interest.
Data Availability
Not applicable.
Author Contributions
FZ. Meamar: Searching in databases, writing proposals, writing the manuscript. M. Savabi-Esfahani: Searching in databases, writing the manuscript. T. Farajkhoda: Searching in databases, writing the proposal, and writing the manuscript.
Acknowledgments
In this research, artificial intelligence was not used in any of the stages of writing, translating, editing, checking grammar, etc. The authors would like to thank all the researchers whose papers were used in this systematic review.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Review Article |
Subject:
Fertility & Infertility
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |