Sun, Feb 1, 2026
[Archive]
Volume 23, Issue 8 (August 2025)
IJRM 2025, 23(8): 627-636 |
Back to browse issues page
Ethics code: R.UMSHA.REC.1402.541
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sanuie Farimani M, Amiri K, Anvari Aliabad R. Spontaneous pregnancy following intra-ovarian platelet-rich plasma administration in poor ovarian responders according to the POSEIDON criteria: A cross-sectional study. IJRM 2025; 23 (8) :627-636
URL: http://ijrm.ir/article-1-3478-en.html
URL: http://ijrm.ir/article-1-3478-en.html
1- Endometrium and Endometriosis Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
2- School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
3- Endometrium and Endometriosis Research Center, Hamadan University of Medical Sciences, Hamadan, Iran. ,anvar_anvari@yahoo.com; r.anvari@umsha.ac.ir
2- School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
3- Endometrium and Endometriosis Research Center, Hamadan University of Medical Sciences, Hamadan, Iran. ,
Full-Text [PDF 408 kb]
(500 Downloads)
| Abstract (HTML) (537 Views)
Full-Text: (67 Views)
1. Introduction
According to the World Health Organization, approximately 17.5% of the global adult population experiences infertility (1). This condition can be classified into primary and secondary infertility categories (2). Assisted reproductive technology (ART) has provided a solution for couples facing infertility. However, some individuals do not respond to ovarian stimulation (OS), a pre-ART procedure that uses stimulators such as gonadotropins (3-5). This has led to the progression of co-treatment methods (6). One of these co-treatments has been recently used to increase the pregnancy rate, especially in those with ovarian function issues (e.g., premature ovarian insufficiency [POI]) is platelet-rich plasma [PRP]), which administrates directly into the ovary (7).
PRP is an autologous product used to treat various pathological conditions, including the healing of chronic (8) and acute (9) wounds, osteoarthritis (10), tendinopathies (11), and musculoskeletal pathologies (12). The regenerative properties of PRP seem to be due to the growth factors mostly derived from the secretory granules. The regenerative properties of PRP appear to be due to growth factors, primarily derived from secretory granules (13). Considering the possible role of the aforementioned growth factors in the field of regenerative medicine (14) as well as the findings from systematic reviews and meta-analyses on PRP therapy for various pathologies (15-18), this treatment has been successfully tested in the field of infertility, particularly in ART (19). According to a recent systematic review and meta-analysis, PRP therapy significantly improved parameters related to the pregnancy success rate among individuals with ovarian reserve issues (20). In contrast, a question that remains is whether this intervention can be used as a standalone treatment for individuals with infertility due to ovarian dysfunction, and if so, which characteristics predict eligibility for this subpopulation.
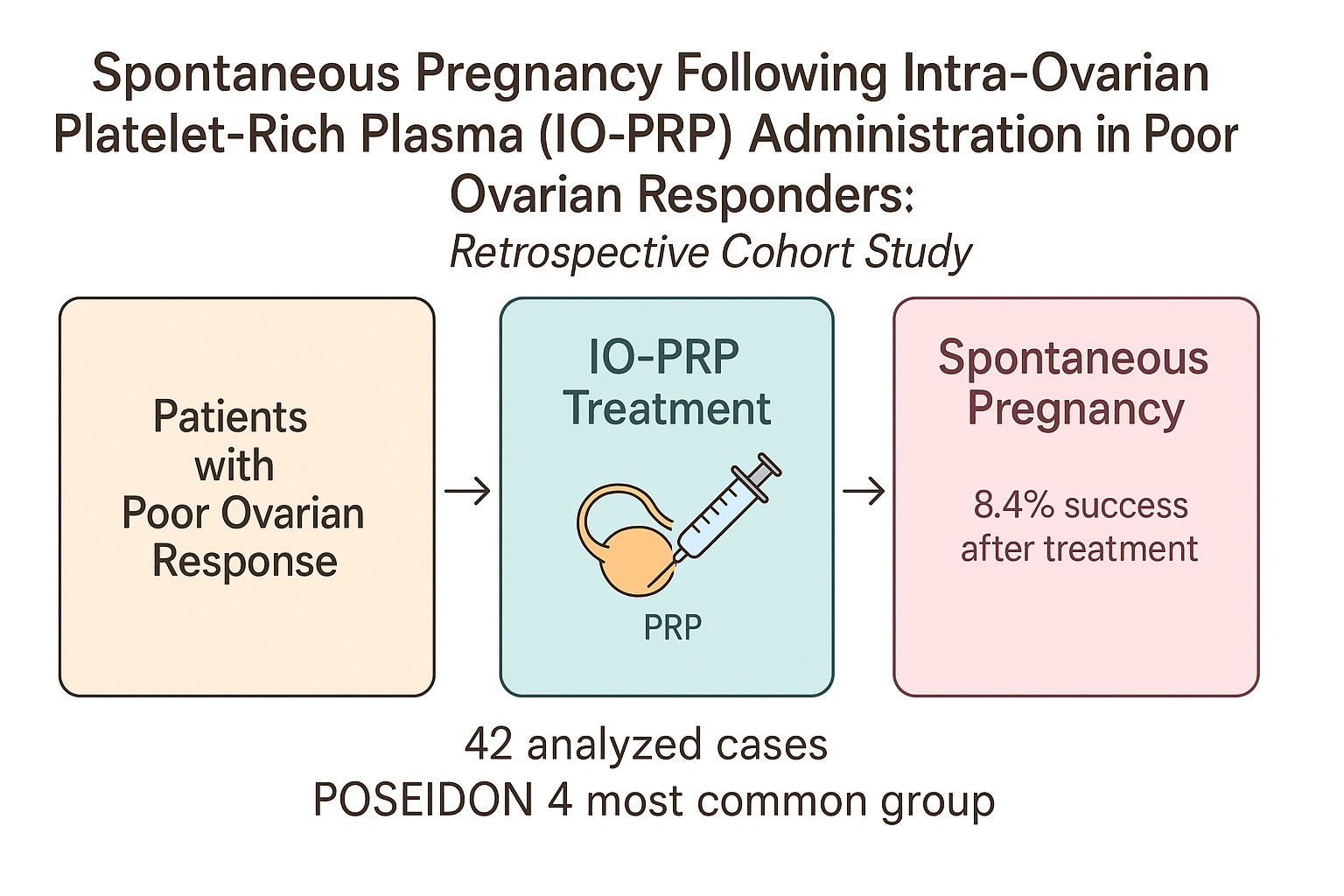
The aim of current study was to investigate the characteristics possibly associated with spontaneous pregnancy among individuals with poor ovarian response (POR) who underwent intra-ovarian PRP (IO-PRP) administration.
2. Materials and Methods
2.1. Study setting
For the current cross-sectional study, we followed all POR women according to the Bologna criteria who underwent IO-PRP injection, in Omid Infertility Clinic (Hamadan, Iran). According to defined Bologna criteria for a poor responder, at least 2 of the following 3 criteria were considered: 1) age > 40 yr; 2) POR in previous in vitro fertilization cycles (≤ 3 oocytes retrieved in a conventional stimulation protocol); and 3) abnormal ovarian reserve tests (21). The data used in this study covered the period between March 2018-2021, and only participants who completed their 2-yr follow-up (up to March 2023) were included. Since there is no solid evidence regarding the mechanistic pathways of the biological effects of PRP therapy in the ovary, and given the exploratory nature of this study aimed at generating findings to guide future investigations, a 2-yr follow-up was considered an appropriate timeline to capture the outcome. The dataset was reviewed to identify cases of spontaneous pregnancy following IO-PRP, and a total of 50 such women were initially found.
2.2. Inclusion and exclusion criteria
The inclusion criteria were: I) individuals diagnosed with infertility (defined as the inability to achieve a clinically recognized pregnancy after 12 months of unprotected sexual intercourse). II) diagnosed with POR according to the Bologna criteria (21). III) undergone IO-PRP administration. IV) laboratory-approved spontaneous pregnancy following PRP therapy. Moreover, exclusion criteria were defined as receiving any other medication/intervention affecting the pregnancy rate or being at any clinical trial with intervention(s) with unknown effect on fertility.
In regard to the PRP intervention, the exclusion criteria is defined as any underlying conditions such as severe anemia (e.g., sickle cell), renal failure, chronic respiratory conditions, neutropenia, sub-mucosal myoma, Asherman’s syndrome, untreated hypothyroidism, untreated hyperprolactinemia, any pathological condition in the fallopian tubes, polycystic ovary syndrome, a positive family history of ovarian cancer, or any contraindication(s) for pregnancy were excluded.
2.3. PRP preparation and administration
All individuals were screened for any contraindication for PRP preparation as previously outlined (9). PRP was then prepared according to our previously reported methods (22-24). Approximately 32 mL of whole blood was collected in 4 (8.5 mL) anticoagulated vacutainer tubes from BD Co. The samples were first subjected to a soft spin at 2500 rpm, after which the plasma and buffy coat layers were separated and transferred to sterile, empty tubes. A second centrifugation step allowed the platelet pellets to settle at the bottom, which were then re-suspended and transferred to another sterile tube, yielding approximately 5 mL of PRP. Platelet counts were measured in the whole blood using a cell counter, and the concentration of platelets in the PRP was confirmed to be > 3 times higher than that in whole blood. IO-PRP administration (2.5-3 ml per ovary) was performed after ovarian stimulation using the Shanghai method (25), as it was described in our previous study (6).
2.4. Study variables
Data related to women’s age, height, weight, body mass index (BMI), duration and causes of infertility, infertility treatment duration, number of PRP sessions, cycle day on which PRP was performed, number of follicles before puncture, number of oocytes after the last PRP session, and interval between the last IO-PRP administration and clinically confirmed pregnancy. In addition, blood levels of anti-Müllerian hormone (AMH), luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol, thyroid-stimulating hormone, and 25-hydroxy vitamin D (vitamin D) before PRP, and variables related to the spouse of these women including age, sperm count, sperm motility, and sperm morphology were extracted from the participants' files and compared in 4 groups based on POSEIDON criteria.
2.5. Ethical Considerations
To access and use the files and database of participated individuals, this study was approved by the Medical Ethics Committee of Hamdan University of Medical Sciences, Hamdan, Iran (Code: IR.UMSHA.REC.1402.541). All the authors adhered to the 1975 Declaration of Helsinki along with any further revisions, especially regarding the confidentiality of the data.
2.6. Statistical Analysis
Data from each participant was compiled in a Microsoft Excel sheet for final analysis. Given the sample size, the normality of data distribution was assessed using the Shapiro-Wilk test. Continuous variables with normal distribution were presented as mean ± standard deviation (SD), while those without normal distribution were reported as median with interquartile range. Categorical variables were described as N (%). To assess differences among POSEIDON groups for normally distributed variables, Levene’s test was first used to evaluate the homogeneity of variances. Based on the results, either one-way analysis of variance (ANOVA) or Welch’s ANOVA was applied. For non-normally distributed variables, the Kruskal-Wallis test was used. Post-hoc analyses were conducted to examine intergroup differences using Tukey’s honestly significant difference (HSD) for ANOVA, Games-Howell test for Welch’s ANOVA, and Dunn’s test for the Kruskal-Wallis test. A p < 0.05 was considered statistically significant.
3. Results
3.1. Biodemographic data
During a 3-yr period, 1,548 women with POR received IO-PRP. Among them, 596 women (38.50%) completed the 2-yr follow-up and were included in the current study, where 50 participants (8.39%) experienced spontaneous pregnancy following IO-PRP administration. However, due to missing data, only 42 women were included in the final statistical analysis.
According to table I, the most prevalent type of infertility was secondary, followed by primary infertility. The proportion of multigravida/primigravida was approximately twice as high as nulligravida. The majority of participants had no prior history of IO-PRP treatment and received the therapy only once; however, up to 4 IO-PRP sessions were recorded among some individuals. Additionally, only one-fifth of the participants (excluding those with missing data, n = 14) had no history of abortion, while up to 5 previous abortions were documented in the medical history of 2 individuals (Table I).
According to the data, the median age of the women who experienced spontaneous pregnancy following IO-PRP administration was 37.00 [32.00-40.00] yr. These participants had a history of infertility for a median of 3.00 [1.5-5.00] yr, followed by a treatment duration of 0.625 [0.25-1.00] yr. The mean BMI was 25.19 ± 3.75 kg/m2, categorized as overweight (26). Also, the pre-intervention laboratory results and pre-puncture follicle/oocyte count of individuals with spontaneous pregnancy following IO-PRP administration, as well as age and sperm analysis of their spouses, have been shown in table II.
3.2. Descriptive data according to the POSEIDON criteria
Based on the gathered data, all the participants with spontaneous pregnancy following IO-PRP administration were classified according to the POSEIDON criteria (4). Among the 42 women, groups 4 and 3 were the most prevalent groups according to the POSEIDON classification and groups 1 and 2 shared similar numbers of participants. The biodemographic characteristics of spontaneous pregnancy following IO-PRP administration according to POSEIDON group have been gathered in table III.
Significant differences were observed among the POSEIDON groups for several variables, including the age of treated individuals, age of their spouse, BMI, serum AMH level, and pre-intervention follicle/oocyte count following the latest IO-PRP. Additionally, the results of the post-hoc analysis, which identified differences between each pair of POSEIDON groups (1 vs. 2, 1 vs. 3, 1 vs. 4, 2 vs. 3, and 3 vs. 4), are shown in table IV.





4. Discussion
This study focused on the descriptive characteristics of individuals diagnosed with POR who experienced spontaneous pregnancy following IO-PRP. The results showed significant differences among the POSEIDON groups in terms of individual age, spouse’s age, BMI, serum AMH levels, and follicle/oocyte counts following the latest PRP treatment. Post hoc analysis further detailed the specific patterns of these differences.
Although POSEIDON group 4 was the most prevalent in this study, this does not imply that spontaneous pregnancy following IO-PRP administration is more likely to occur in this group. Another study performed using our database, focusing on another outcome but still classifying participants in accordance with the POSEIDON criteria, found that the POSEIDON group IV was the most prevalent (58.3%) (6). Therefore, higher number of spontaneous pregnancies in POSEIDON group IV is more likely due to this group representing higher population rather than higher susceptibility. As mentioned, age and AMH levels are key variables in the determination of the POSEIDON group (4). Given this, if POSEIDON group 4 were more susceptible to spontaneous pregnancy following IO-PRP administration, additional variables beyond age and AMH would be expected to differ in post hoc analysis.
In a study, the effects of IO-PRP on ovarian rejuvenation were investigated. 4 groups (each with 30 cases) of individuals with POI, POR, menopause, and perimenopause were included. According to their results, a notable improvement was observed in the hormonal profiles of the studied cases as well as in their ovarian reserve. Additionally, in the POI group, 3 spontaneous pregnancies were observed (27).
A study investigated the biodemographic variables of cases who underwent IO-PRP administration and evaluated these variables in 2 groups: those who experienced spontaneous pregnancy and those who conceived via in vitro fertilization. However, it seems that due to the low sample size in the spontaneous pregnancy group (n = 13), categorization according to the POSEIDON criteria was not performed. According to their results, the mean pre-intervention values for FSH and antral follicle count were 9.4 ± 5 IU/L and 5.7 ± 4.3, respectively. Unfortunately, data regarding age, BMI, LH, AMH, and other related variables were not presented for this group (28).
Another study reported spontaneous pregnancy following IO-PRP administration in infertile cases with POI. According to their results, out of 311 enrolled cases, 23 (7.4%) experienced spontaneous pregnancy. The mean age, infertility duration, pre-intervention FSH levels, pre-intervention AMH levels, and pre-intervention antral follicle count of these cases were 34.6 ± 4.0 yr, 5.6 ± 3.4 yr, 33.3 ± 8.9 mIU/mL, 0.09 ± 0.07 ng/mL, and 1.26 ± 0.8, respectively, which differ from our findings. However, since their data were presented as mean ± SD and most of our data were reported as median (interquartile range), an exact comparison was not possible. Nonetheless, the difference in AMH levels between their study (0.09 ± 0.07 ng/mL) and ours (0.9 [0.56-1.53] ng/mL) appears to be statistically significant (29). Similar to the reference (28), the already discussed study (29) did not categorize cases with spontaneous pregnancy following IO-PRP administration according to the POSEIDON criteria.
As with any study, this investigation has its strengths and limitations. Among the strengths, to the best of our knowledge, this is the first study to categorize and investigate cases with spontaneous pregnancy following IO-PRP administration according to the POSEIDON criteria. Additionally, compared to similar studies, a broader range of variables was investigated. In contrast, as a limitation, post-intervention laboratory values such as FSH, LH, and AMH were not assessed in this study due to a lack of follow-up once pregnancy was confirmed. Another limitation of this study is the small sample size (n = 42), although it is still larger than that of other similar studies (28, 29).
5. Conclusion
This study investigated the biodemographic characteristics of poor ovarian responders who experienced spontaneous pregnancy following intra-ovarian PRP administration. These results indicated that even with a follow-up duration of 2 yr, the rate of spontaneous pregnancy following IO-PRP was approximately 8.4%. This ratio seems not to be clinically significant to perform a wait-and-watch plan after IO-PRP instead of other infertility treatments. In regard to investigating any variable associated with higher rate of spontaneous pregnancy, variables including age of studied women, spouse’s age, serum AMH levels, BMI, and the pre-puncture follicle/oocyte count following the last PRP session showed statistically significant differences among the groups with and without spontaneous pregnancy. Thus, the authors suggest further prospective cohort studies to investigate their possible role in this regard.
Data Availability
Data would be available upon online request from the corresponding author.
Author Contributions
M. Sanuie Farimani and R. Anvari Aliabad had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: M. Sanuie Farimani and R. Anvari Aliabad. Acquisition, analysis, or interpretation of data K. Amiri and R. Anvari Aliabad. Drafting of the manuscript: K. Amiri and R. Anvari Aliabad. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: K. Amiri. Supervision: M. Sanuie Farimani and R. Anvari Aliabad.
Acknowledgments
The authors are thankful for the kind assistance of Omid Infertility Clinic, Hamadan, Iran. This study was funded by Hamadan University of Medical Sciences, Hamadan, Iran (grant number: 140208237153). This study used artificial intelligence (ChatGPT 4o) for grammar checking.
Conflict of Interest
The authors declare that there is no conflict of interest.
According to the World Health Organization, approximately 17.5% of the global adult population experiences infertility (1). This condition can be classified into primary and secondary infertility categories (2). Assisted reproductive technology (ART) has provided a solution for couples facing infertility. However, some individuals do not respond to ovarian stimulation (OS), a pre-ART procedure that uses stimulators such as gonadotropins (3-5). This has led to the progression of co-treatment methods (6). One of these co-treatments has been recently used to increase the pregnancy rate, especially in those with ovarian function issues (e.g., premature ovarian insufficiency [POI]) is platelet-rich plasma [PRP]), which administrates directly into the ovary (7).
PRP is an autologous product used to treat various pathological conditions, including the healing of chronic (8) and acute (9) wounds, osteoarthritis (10), tendinopathies (11), and musculoskeletal pathologies (12). The regenerative properties of PRP seem to be due to the growth factors mostly derived from the secretory granules. The regenerative properties of PRP appear to be due to growth factors, primarily derived from secretory granules (13). Considering the possible role of the aforementioned growth factors in the field of regenerative medicine (14) as well as the findings from systematic reviews and meta-analyses on PRP therapy for various pathologies (15-18), this treatment has been successfully tested in the field of infertility, particularly in ART (19). According to a recent systematic review and meta-analysis, PRP therapy significantly improved parameters related to the pregnancy success rate among individuals with ovarian reserve issues (20). In contrast, a question that remains is whether this intervention can be used as a standalone treatment for individuals with infertility due to ovarian dysfunction, and if so, which characteristics predict eligibility for this subpopulation.
The aim of current study was to investigate the characteristics possibly associated with spontaneous pregnancy among individuals with poor ovarian response (POR) who underwent intra-ovarian PRP (IO-PRP) administration.
2. Materials and Methods
2.1. Study setting
For the current cross-sectional study, we followed all POR women according to the Bologna criteria who underwent IO-PRP injection, in Omid Infertility Clinic (Hamadan, Iran). According to defined Bologna criteria for a poor responder, at least 2 of the following 3 criteria were considered: 1) age > 40 yr; 2) POR in previous in vitro fertilization cycles (≤ 3 oocytes retrieved in a conventional stimulation protocol); and 3) abnormal ovarian reserve tests (21). The data used in this study covered the period between March 2018-2021, and only participants who completed their 2-yr follow-up (up to March 2023) were included. Since there is no solid evidence regarding the mechanistic pathways of the biological effects of PRP therapy in the ovary, and given the exploratory nature of this study aimed at generating findings to guide future investigations, a 2-yr follow-up was considered an appropriate timeline to capture the outcome. The dataset was reviewed to identify cases of spontaneous pregnancy following IO-PRP, and a total of 50 such women were initially found.
2.2. Inclusion and exclusion criteria
The inclusion criteria were: I) individuals diagnosed with infertility (defined as the inability to achieve a clinically recognized pregnancy after 12 months of unprotected sexual intercourse). II) diagnosed with POR according to the Bologna criteria (21). III) undergone IO-PRP administration. IV) laboratory-approved spontaneous pregnancy following PRP therapy. Moreover, exclusion criteria were defined as receiving any other medication/intervention affecting the pregnancy rate or being at any clinical trial with intervention(s) with unknown effect on fertility.
In regard to the PRP intervention, the exclusion criteria is defined as any underlying conditions such as severe anemia (e.g., sickle cell), renal failure, chronic respiratory conditions, neutropenia, sub-mucosal myoma, Asherman’s syndrome, untreated hypothyroidism, untreated hyperprolactinemia, any pathological condition in the fallopian tubes, polycystic ovary syndrome, a positive family history of ovarian cancer, or any contraindication(s) for pregnancy were excluded.
2.3. PRP preparation and administration
All individuals were screened for any contraindication for PRP preparation as previously outlined (9). PRP was then prepared according to our previously reported methods (22-24). Approximately 32 mL of whole blood was collected in 4 (8.5 mL) anticoagulated vacutainer tubes from BD Co. The samples were first subjected to a soft spin at 2500 rpm, after which the plasma and buffy coat layers were separated and transferred to sterile, empty tubes. A second centrifugation step allowed the platelet pellets to settle at the bottom, which were then re-suspended and transferred to another sterile tube, yielding approximately 5 mL of PRP. Platelet counts were measured in the whole blood using a cell counter, and the concentration of platelets in the PRP was confirmed to be > 3 times higher than that in whole blood. IO-PRP administration (2.5-3 ml per ovary) was performed after ovarian stimulation using the Shanghai method (25), as it was described in our previous study (6).
2.4. Study variables
Data related to women’s age, height, weight, body mass index (BMI), duration and causes of infertility, infertility treatment duration, number of PRP sessions, cycle day on which PRP was performed, number of follicles before puncture, number of oocytes after the last PRP session, and interval between the last IO-PRP administration and clinically confirmed pregnancy. In addition, blood levels of anti-Müllerian hormone (AMH), luteinizing hormone (LH), follicle-stimulating hormone (FSH), estradiol, thyroid-stimulating hormone, and 25-hydroxy vitamin D (vitamin D) before PRP, and variables related to the spouse of these women including age, sperm count, sperm motility, and sperm morphology were extracted from the participants' files and compared in 4 groups based on POSEIDON criteria.
2.5. Ethical Considerations
To access and use the files and database of participated individuals, this study was approved by the Medical Ethics Committee of Hamdan University of Medical Sciences, Hamdan, Iran (Code: IR.UMSHA.REC.1402.541). All the authors adhered to the 1975 Declaration of Helsinki along with any further revisions, especially regarding the confidentiality of the data.
2.6. Statistical Analysis
Data from each participant was compiled in a Microsoft Excel sheet for final analysis. Given the sample size, the normality of data distribution was assessed using the Shapiro-Wilk test. Continuous variables with normal distribution were presented as mean ± standard deviation (SD), while those without normal distribution were reported as median with interquartile range. Categorical variables were described as N (%). To assess differences among POSEIDON groups for normally distributed variables, Levene’s test was first used to evaluate the homogeneity of variances. Based on the results, either one-way analysis of variance (ANOVA) or Welch’s ANOVA was applied. For non-normally distributed variables, the Kruskal-Wallis test was used. Post-hoc analyses were conducted to examine intergroup differences using Tukey’s honestly significant difference (HSD) for ANOVA, Games-Howell test for Welch’s ANOVA, and Dunn’s test for the Kruskal-Wallis test. A p < 0.05 was considered statistically significant.
3. Results
3.1. Biodemographic data
During a 3-yr period, 1,548 women with POR received IO-PRP. Among them, 596 women (38.50%) completed the 2-yr follow-up and were included in the current study, where 50 participants (8.39%) experienced spontaneous pregnancy following IO-PRP administration. However, due to missing data, only 42 women were included in the final statistical analysis.
According to table I, the most prevalent type of infertility was secondary, followed by primary infertility. The proportion of multigravida/primigravida was approximately twice as high as nulligravida. The majority of participants had no prior history of IO-PRP treatment and received the therapy only once; however, up to 4 IO-PRP sessions were recorded among some individuals. Additionally, only one-fifth of the participants (excluding those with missing data, n = 14) had no history of abortion, while up to 5 previous abortions were documented in the medical history of 2 individuals (Table I).
According to the data, the median age of the women who experienced spontaneous pregnancy following IO-PRP administration was 37.00 [32.00-40.00] yr. These participants had a history of infertility for a median of 3.00 [1.5-5.00] yr, followed by a treatment duration of 0.625 [0.25-1.00] yr. The mean BMI was 25.19 ± 3.75 kg/m2, categorized as overweight (26). Also, the pre-intervention laboratory results and pre-puncture follicle/oocyte count of individuals with spontaneous pregnancy following IO-PRP administration, as well as age and sperm analysis of their spouses, have been shown in table II.
3.2. Descriptive data according to the POSEIDON criteria
Based on the gathered data, all the participants with spontaneous pregnancy following IO-PRP administration were classified according to the POSEIDON criteria (4). Among the 42 women, groups 4 and 3 were the most prevalent groups according to the POSEIDON classification and groups 1 and 2 shared similar numbers of participants. The biodemographic characteristics of spontaneous pregnancy following IO-PRP administration according to POSEIDON group have been gathered in table III.
Significant differences were observed among the POSEIDON groups for several variables, including the age of treated individuals, age of their spouse, BMI, serum AMH level, and pre-intervention follicle/oocyte count following the latest IO-PRP. Additionally, the results of the post-hoc analysis, which identified differences between each pair of POSEIDON groups (1 vs. 2, 1 vs. 3, 1 vs. 4, 2 vs. 3, and 3 vs. 4), are shown in table IV.





4. Discussion
This study focused on the descriptive characteristics of individuals diagnosed with POR who experienced spontaneous pregnancy following IO-PRP. The results showed significant differences among the POSEIDON groups in terms of individual age, spouse’s age, BMI, serum AMH levels, and follicle/oocyte counts following the latest PRP treatment. Post hoc analysis further detailed the specific patterns of these differences.
Although POSEIDON group 4 was the most prevalent in this study, this does not imply that spontaneous pregnancy following IO-PRP administration is more likely to occur in this group. Another study performed using our database, focusing on another outcome but still classifying participants in accordance with the POSEIDON criteria, found that the POSEIDON group IV was the most prevalent (58.3%) (6). Therefore, higher number of spontaneous pregnancies in POSEIDON group IV is more likely due to this group representing higher population rather than higher susceptibility. As mentioned, age and AMH levels are key variables in the determination of the POSEIDON group (4). Given this, if POSEIDON group 4 were more susceptible to spontaneous pregnancy following IO-PRP administration, additional variables beyond age and AMH would be expected to differ in post hoc analysis.
In a study, the effects of IO-PRP on ovarian rejuvenation were investigated. 4 groups (each with 30 cases) of individuals with POI, POR, menopause, and perimenopause were included. According to their results, a notable improvement was observed in the hormonal profiles of the studied cases as well as in their ovarian reserve. Additionally, in the POI group, 3 spontaneous pregnancies were observed (27).
A study investigated the biodemographic variables of cases who underwent IO-PRP administration and evaluated these variables in 2 groups: those who experienced spontaneous pregnancy and those who conceived via in vitro fertilization. However, it seems that due to the low sample size in the spontaneous pregnancy group (n = 13), categorization according to the POSEIDON criteria was not performed. According to their results, the mean pre-intervention values for FSH and antral follicle count were 9.4 ± 5 IU/L and 5.7 ± 4.3, respectively. Unfortunately, data regarding age, BMI, LH, AMH, and other related variables were not presented for this group (28).
Another study reported spontaneous pregnancy following IO-PRP administration in infertile cases with POI. According to their results, out of 311 enrolled cases, 23 (7.4%) experienced spontaneous pregnancy. The mean age, infertility duration, pre-intervention FSH levels, pre-intervention AMH levels, and pre-intervention antral follicle count of these cases were 34.6 ± 4.0 yr, 5.6 ± 3.4 yr, 33.3 ± 8.9 mIU/mL, 0.09 ± 0.07 ng/mL, and 1.26 ± 0.8, respectively, which differ from our findings. However, since their data were presented as mean ± SD and most of our data were reported as median (interquartile range), an exact comparison was not possible. Nonetheless, the difference in AMH levels between their study (0.09 ± 0.07 ng/mL) and ours (0.9 [0.56-1.53] ng/mL) appears to be statistically significant (29). Similar to the reference (28), the already discussed study (29) did not categorize cases with spontaneous pregnancy following IO-PRP administration according to the POSEIDON criteria.
As with any study, this investigation has its strengths and limitations. Among the strengths, to the best of our knowledge, this is the first study to categorize and investigate cases with spontaneous pregnancy following IO-PRP administration according to the POSEIDON criteria. Additionally, compared to similar studies, a broader range of variables was investigated. In contrast, as a limitation, post-intervention laboratory values such as FSH, LH, and AMH were not assessed in this study due to a lack of follow-up once pregnancy was confirmed. Another limitation of this study is the small sample size (n = 42), although it is still larger than that of other similar studies (28, 29).
5. Conclusion
This study investigated the biodemographic characteristics of poor ovarian responders who experienced spontaneous pregnancy following intra-ovarian PRP administration. These results indicated that even with a follow-up duration of 2 yr, the rate of spontaneous pregnancy following IO-PRP was approximately 8.4%. This ratio seems not to be clinically significant to perform a wait-and-watch plan after IO-PRP instead of other infertility treatments. In regard to investigating any variable associated with higher rate of spontaneous pregnancy, variables including age of studied women, spouse’s age, serum AMH levels, BMI, and the pre-puncture follicle/oocyte count following the last PRP session showed statistically significant differences among the groups with and without spontaneous pregnancy. Thus, the authors suggest further prospective cohort studies to investigate their possible role in this regard.
Data Availability
Data would be available upon online request from the corresponding author.
Author Contributions
M. Sanuie Farimani and R. Anvari Aliabad had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: M. Sanuie Farimani and R. Anvari Aliabad. Acquisition, analysis, or interpretation of data K. Amiri and R. Anvari Aliabad. Drafting of the manuscript: K. Amiri and R. Anvari Aliabad. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: K. Amiri. Supervision: M. Sanuie Farimani and R. Anvari Aliabad.
Acknowledgments
The authors are thankful for the kind assistance of Omid Infertility Clinic, Hamadan, Iran. This study was funded by Hamadan University of Medical Sciences, Hamadan, Iran (grant number: 140208237153). This study used artificial intelligence (ChatGPT 4o) for grammar checking.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Fertility & Infertility
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |