Sat, Jan 31, 2026
[Archive]
Volume 23, Issue 6 (June 2025)
IJRM 2025, 23(6): 459-474 |
Back to browse issues page
Ethics code: IR.MAZUMS.REC.1403.436
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zamaniyan M, Peivandi S, Pashazadeh M, Safarloo F. Efficacy of intraovarian injection of autologous platelet-rich plasma on outcome of in vitro fertilization in women with poor ovarian response: A systematic review. IJRM 2025; 23 (6) :459-474
URL: http://ijrm.ir/article-1-3530-en.html
URL: http://ijrm.ir/article-1-3530-en.html
1- Diabetes Research Center, Mazandaran University of Medical Sciences, Sari, Iran. & Department of Obstetrics and Gynecology, IVF Ward, Faculty of Medicine, Sexual and Reproductive Health Research Center, Diabetes Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Obstetrics and Gynecology, IVF Ward, Faculty of Medicine, Sexual and Reproductive Health Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
3- Islamic Azad University, Ardabil Branch, Ardabil, Iran.
4- IVF ward, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran. ,safarloo203@gmail.com
2- Department of Obstetrics and Gynecology, IVF Ward, Faculty of Medicine, Sexual and Reproductive Health Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
3- Islamic Azad University, Ardabil Branch, Ardabil, Iran.
4- IVF ward, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran. ,
Full-Text [PDF 458 kb]
(469 Downloads)
| Abstract (HTML) (501 Views)
Full-Text: (110 Views)
1. Introduction
An inadequate ovarian response to gonadotropin injections is a key characteristic of poor ovarian response (POR) (1). In women with POR, ovarian stimulation during assisted reproductive technologies (ART), often results in a reduced number of retrieved oocytes, leading to lower pregnancy rates (2). Research indicates that the prevalence of POR ranges from 9-24% (3). Currently, egg donation is the primary treatment option for women with POR who exhibit an insufficient response to ovarian stimulation (4).
While the number of patients requiring egg donation is increasing, many women reject this approach due to cultural and ideological reasons (5). A significant proportion of women struggle with the idea of having a child using genetic material from another person (6). Additionally, ethical and religious concerns have led some countries to impose restrictions on the use of donor eggs, forcing women to seek alternative treatments, such as ovarian rejuvenation and methods aimed at enhancing ovarian response (7).
Platelet-rich plasma (PRP) has demonstrated beneficial effects on tissue regeneration, angiogenesis, inflammation regulation, and anabolism across various medical disciplines (8). However, its efficacy in the field of infertility, particularly regarding ovarian insufficiency, remains inconclusive (9).
Platelets are small cytoplasmic fragments derived from megakaryocytes in the bone marrow, measuring approximately 2 μm in diameter (10). The activation of alpha granules within platelets is a crucial step that determines the availability of bioactive molecules and, consequently, the quality of PRP (11).
In infertility-related discussions, PRP may enhance ovarian response in patients with POR through several mechanisms. One of the primary effects of PRP is the stimulation of blood flow to the ovaries (12). The growth factors in PRP can promote the expansion of blood vessels in the ovaries, increasing blood circulation, which in turn improves the nourishment and oxygen supply to ovarian cells (13). This can help enhance oocyte quality and follicular development. Additionally, PRP reduces inflammation and oxidative stress in the ovaries, creating a favorable environment for the repair and regeneration of ovarian tissue (14).
In addition to its blood circulation and anti-inflammatory effects, PRP can stimulate the proliferation and differentiation of granulosa cells and ovarian follicles (15). The growth factors in PRP assist in activating repair signaling pathways that play a key role in the regeneration and improvement of ovarian tissues. These processes may lead to an increase in the number of growing follicles and enhancement of oocyte quality (16). Therefore, by stimulating repair and regenerative processes in the ovaries, PRP may improve the chances of pregnancy in patients with POR.
Although further research is needed to confirm these mechanisms and its efficacy because a detailed study of this effect, especially in the long term, has not yet been conducted (17). The long-term effects of PRP have not been thoroughly investigated in these studies (18). Therefore, we aimed to conduct a study titled "Efficacy of intra-ovarian injection of autologous platelet-rich plasma on the outcome of in vitro fertilization in patients with poor ovarian response: A systematic review".
2. Materials and Methods
This systematic review was conducted according to the PRISMA guidelines (19). The search strategy was based on the PICO (P: population or participants; I: intervention; C: comparison; O: outcome) or PECO (P: population or participants; E: exposure; C: comparison; O: outcome) criteria for either observational studies or clinical trials. In these studies, the "population" was women undergoing infertility treatment. The "intervention or exposure" was ovarian PRP. The "control or comparator group" consisted of those who did not receive ovarian PRP. The "outcome" was miscarriage, implantation, clinical pregnancy, and live birth.
2.1. Literature search
This study is a systematic review conducted following the JBI methodology guidelines (20). The research community comprised all scientific articles related to ovarian PRP and its success in infertility treatment worldwide, indexed in at least one database. The first and second researchers conducted a comprehensive search in international databases, including PubMed, ScienceDirect, Scopus, Web of Science, Embase, Cochrane, and the Google Scholar search engine. In the process of searching for relevant articles related to the research topic, in addition to using well-known and established databases, articles were identified through manual searching and other sources. All articles were reviewed at every stage of the search and quality assessment by 2 independent researchers, and in case of any disagreement, a third author was consulted.
2.2. Search strategy
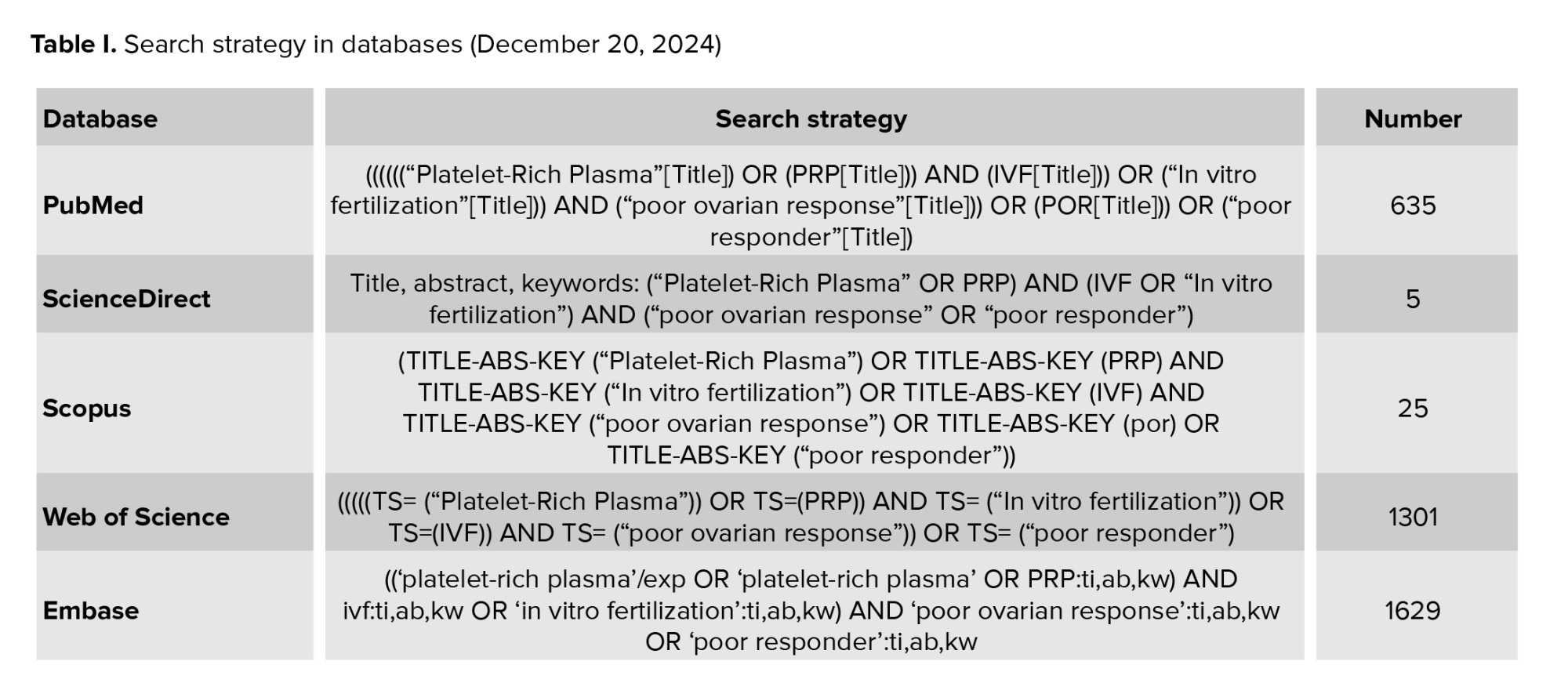
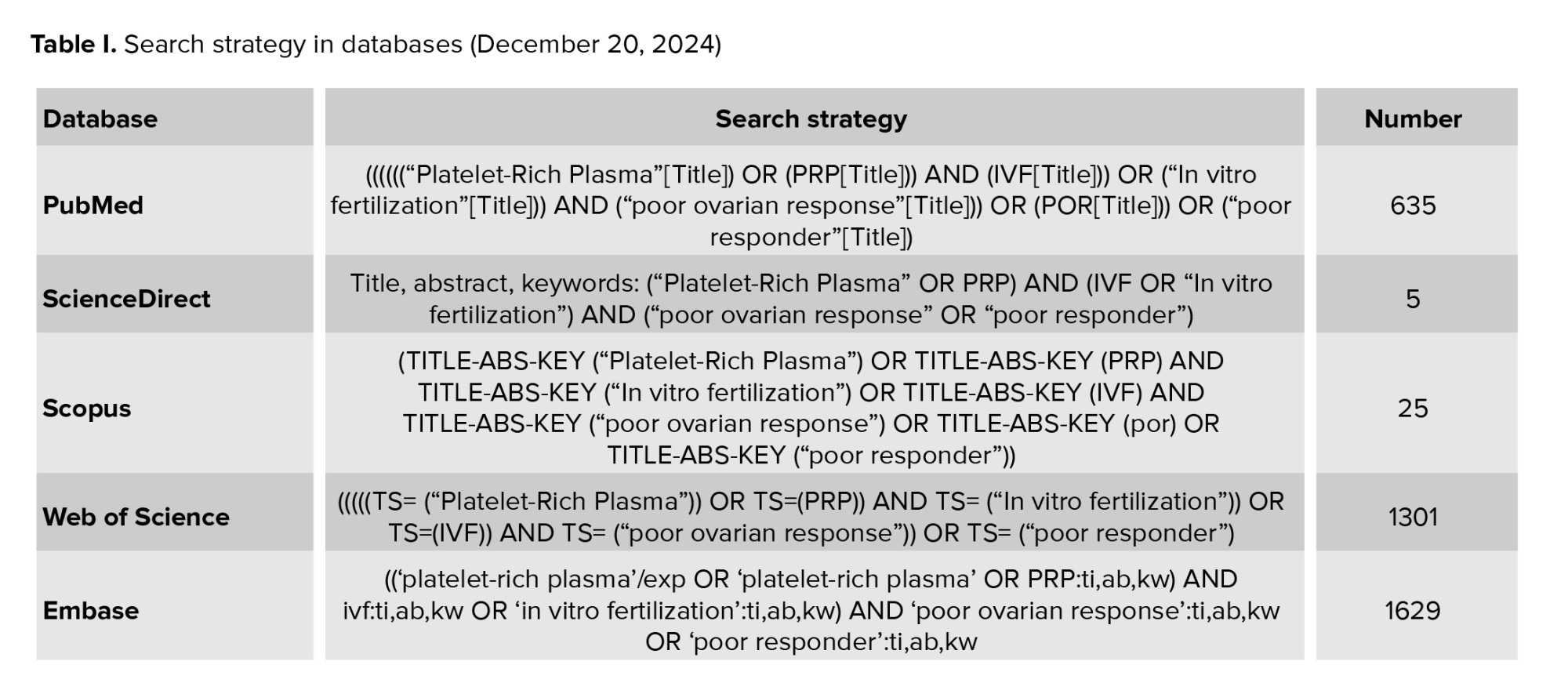
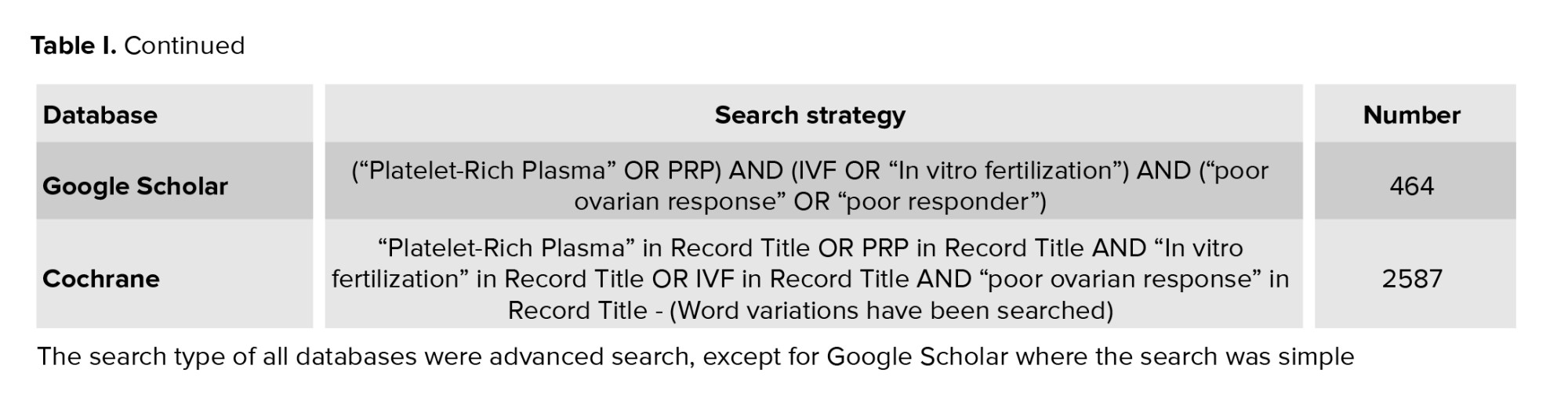
In order to find related articles in English-language databases, keywords were selected based on Mesh and included the combination of the words ("Platelet-Rich Plasma") OR (PRP) AND (IVF) OR ("In vitro fertilization") AND ("poor ovarian response") OR (POR) OR ("poor responder") in the plural and with the operators "OR" and "AND" were combined. To ensure that all relevant data were retained, a time frame was set and all published articles without time limits up to December 20, 2024 were included in the evaluation. To achieve the most comprehensive search possible, all final articles related to the topic were manually reviewed, allowing for the identification of any additional potential sources (Table I).
2.3. Inclusion and exclusion criteria
2.3.1. Search phase
Scientific articles published in PubMed, ScienceDirect, Scopus, Web of Science, Embase, and Cochrane databases. Articles published within a specified time period and those that were relevant to the main research topic (according to PICO or PECO as mentioned earlier). The following studies were considered eligible for inclusion in this scope study: observational studies (including cross-sectional, prospective, and retrospective cohort and case-control designs) and interventional studies (such as clinical trials, experimental trials, and quasi-experimental trials). The studies included were those that investigated the use of PRP therapy for ovarian treatment in the context of IVF globally. Articles in languages other than the target languages (e.g., English or Persian). Articles that do not fully provide the desired information in the research context.
2.3.2. Title and abstract screening stage
Inclusion criteria: research-related articles that refer to the main concepts of the research in the title and abstract. Articles that are aligned with your research based on keywords and PICO/PECO concepts.
Exclusion criteria: do not refer to the main concepts in the research.
2.3.3. Full review stage of articles
Eligibility criteria required participants to be women aged between 18 and 55 yr diagnosed with diminished ovarian reserve (DOR), premature ovarian failure, or premature ovarian insufficiency. Studies were included if they assessed participants both before and after intra-ovarian PRP injection. A participant was classified as having DOR if at least 1 of the following criteria was met: basal follicle-stimulating hormone > 15 IU/L, basal anti-Müllerian hormone < 1 ng/ml, antral follicle count < 5, meeting the Bologna criteria for DOR, meeting POSEIDON criteria groups 3 or 4, associated with low prognosis in ART outcomes.
Both randomized and non-randomized studies were eligible for inclusion. Studies that did not contain original research data, such as letters to the editor, correspondence pieces, or reviews, were excluded from the analysis.
The intervention under investigation was intra-ovarian PRP injection, regardless of the number of administrations, the volume of PRP injected, or the method of PRP preparation and administration. Studies using self-controlled designs, where outcomes before the intervention served as the basis for comparison, were included.
In the reviewed studies, the primary outcome measured was the biochemical pregnancy rate, defined as a positive pregnancy test or elevated β-human chorionic gonadotropin levels 2 wk after embryo transfer. Secondary outcomes included the rate of spontaneous pregnancies, live birth rates, implantation, clinical pregnancy, abortion, and ongoing pregnancy.
This approach ensures a comprehensive assessment of PRP’s efficacy and its impact on reproductive outcomes in women with compromised ovarian function. It should be noted that in studies where participants had male infertility factors or the participants in the study used methods of ART other than IVF, they were excluded from the analysis.
2.4. Data collection and extraction
2 authors (F. Safarloo, M. Zamaniyan) independently reviewed the collected articles and extracted the data using a uniform, standardized data collection form. If a study was deemed relevant, its full text was reviewed for further assessment. Any discrepancies were resolved through discussion with a third author (S. Peivandi) during the search and screening procedure. The variables extracted from the articles included the year of study and author's name, place of study, study design, purpose of the study, sample size and statistical population, variables investigated in the study, tools used in the study, and study results.
2.5. Methodological quality assessment (risk of bias assessment)
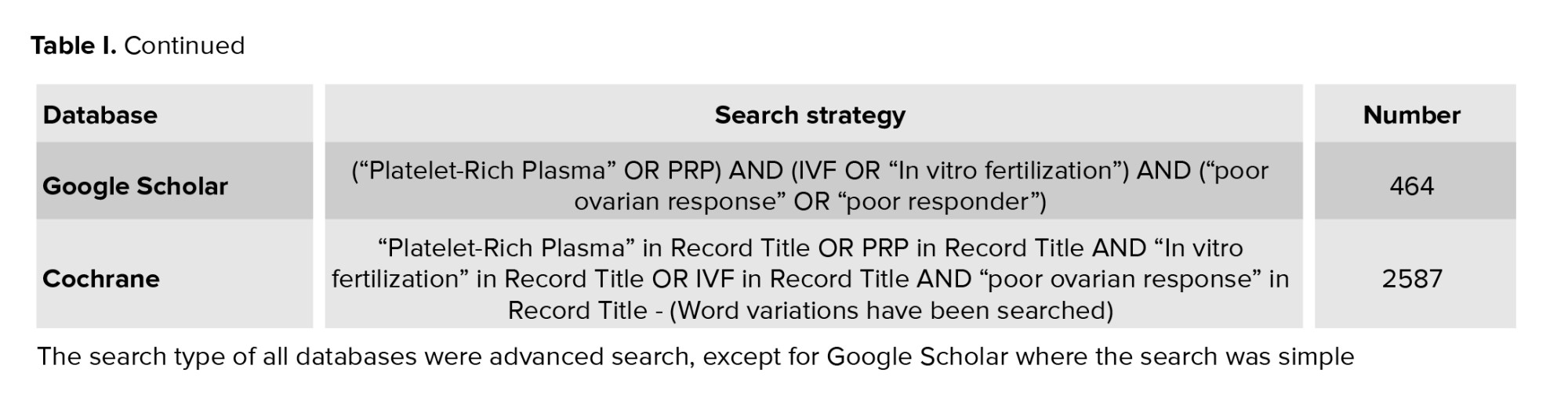
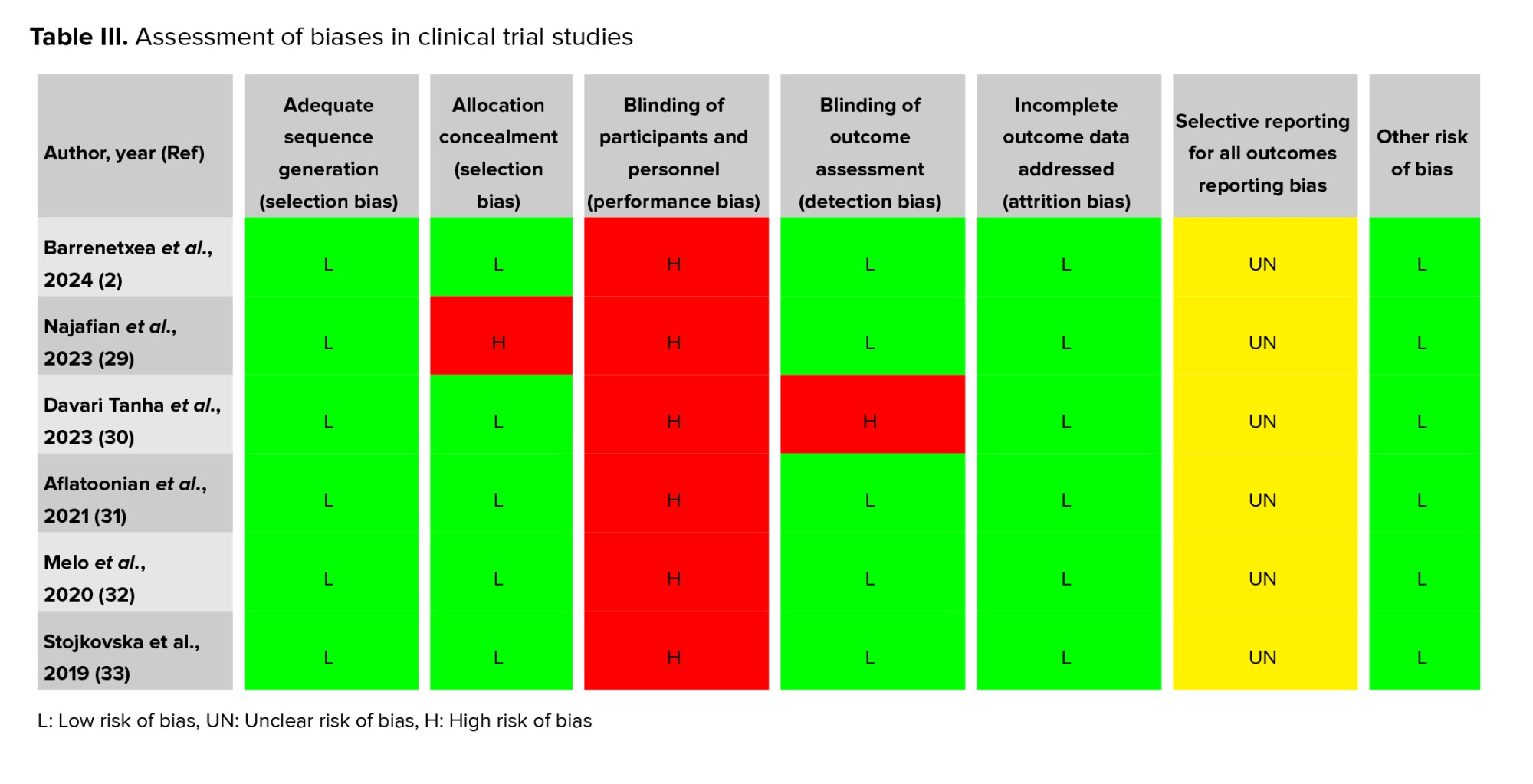
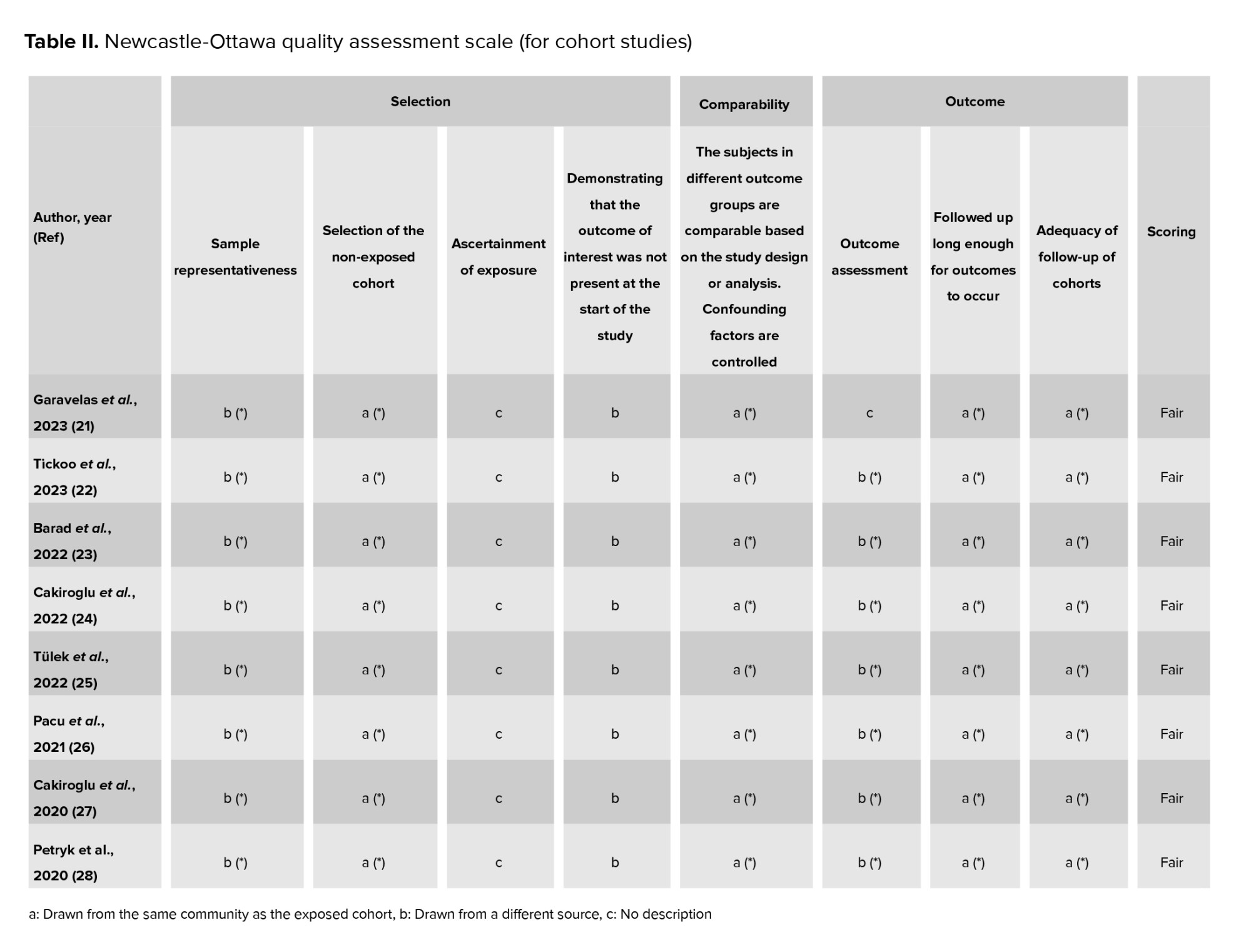
The Newcastle-Ottawa scale (NOS) for cohort studies table II is a widely recognized tool for assessing the quality and potential risk of bias in observational research (18, 19). The NOS evaluates 3 main domains: selection, comparability, and outcome. These domains are further divided into 9 specific items, with slight variations in the scoring system for cohort, cross-sectional, and case-control studies. For cohort studies, quality is classified as follows:
Good quality: 3 or 4 stars in the selection domain, 1 or 2 stars in the comparability domain, and 2 or 3 stars in the outcome/exposure domain.
Fair quality: 2 stars in the selection domain, 1 or 2 stars in the comparability domain, and 2 or 3 stars in the outcome/exposure domain (18, 19).
Poor quality: 0 or 1 star in the selection domain, 0 stars in the comparability domain, or 0 or 1 star in the outcome/exposure domain.
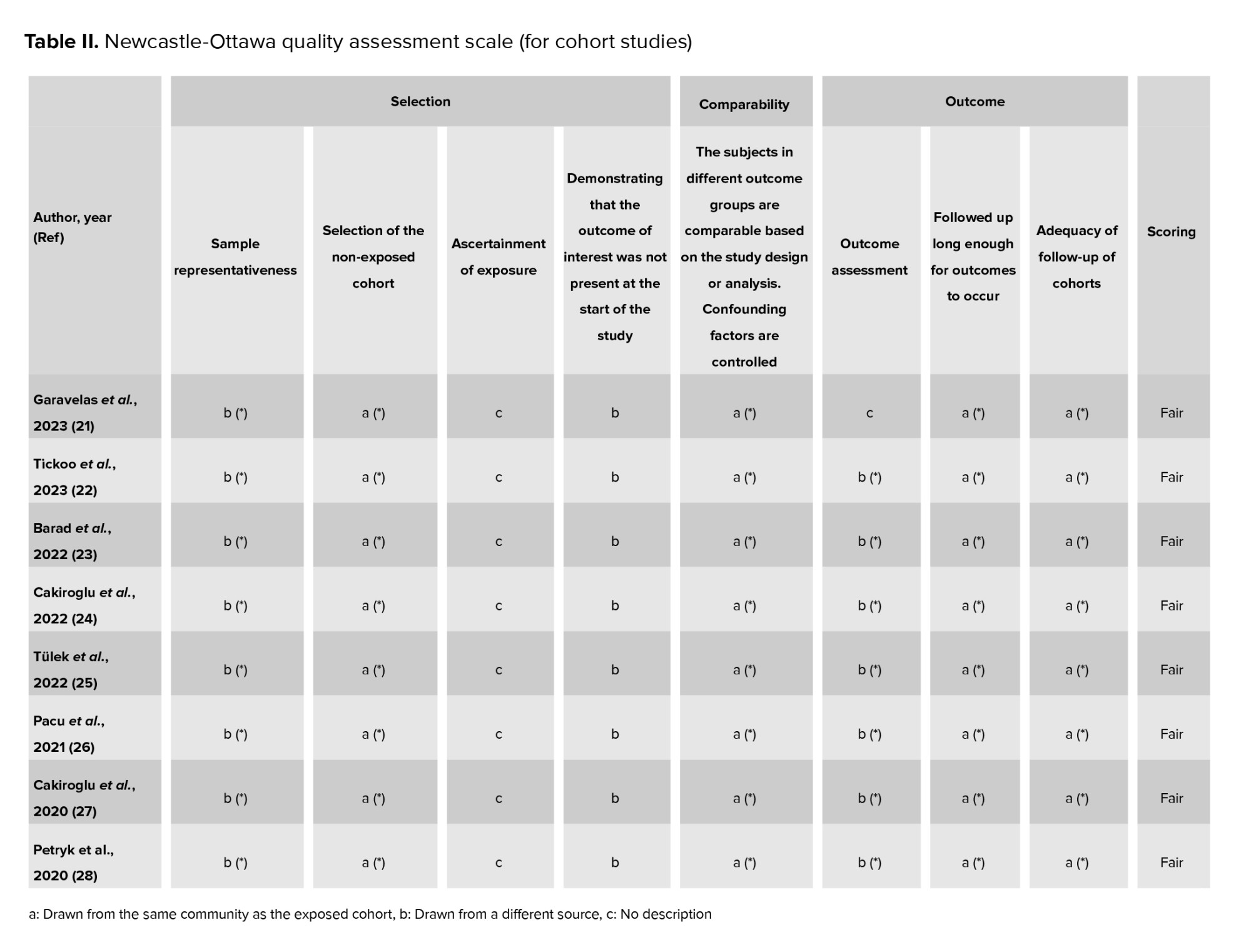
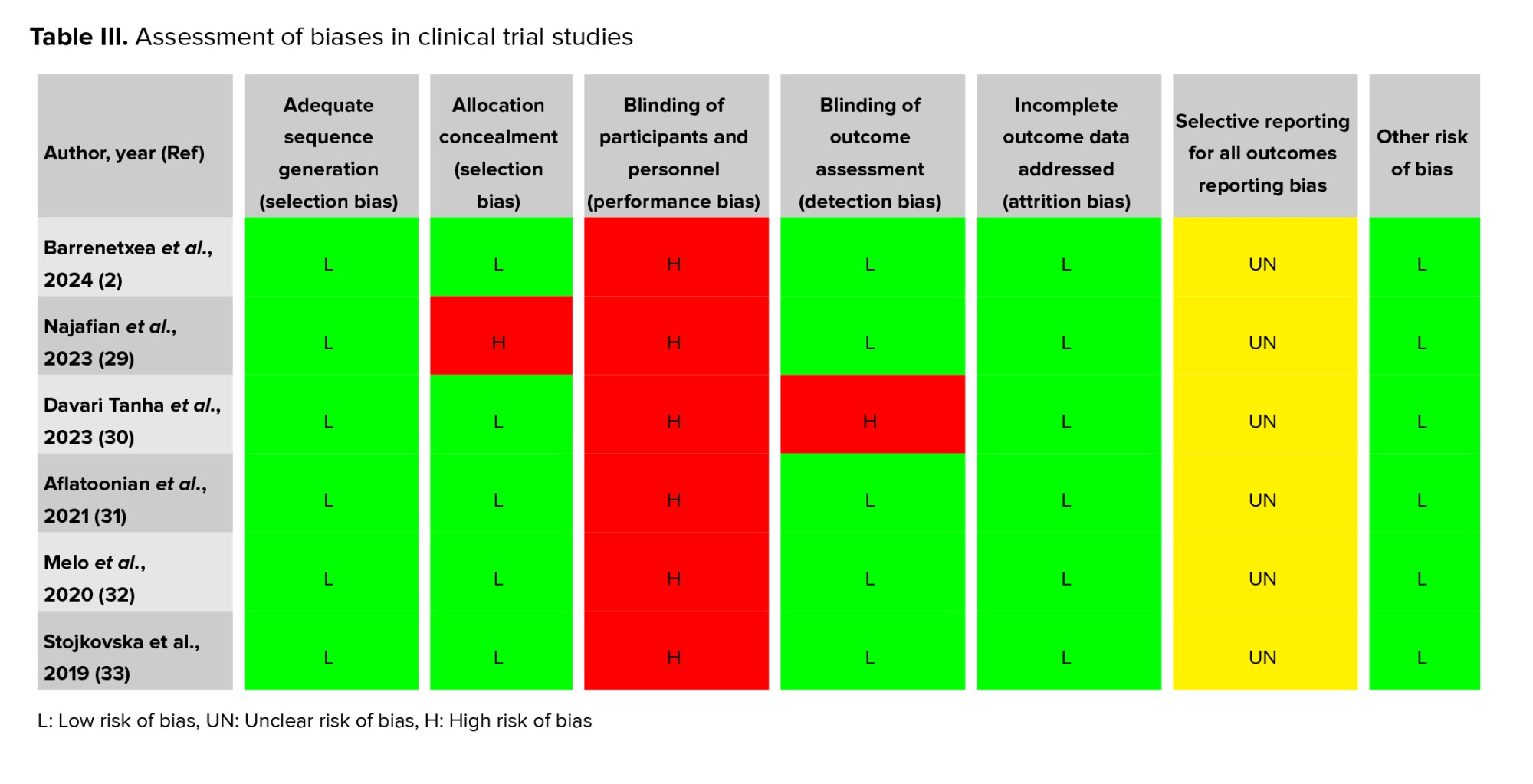
To assess the quality of the studies included in this systematic review, various types of bias were examined, including selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and assessors), detection bias (blinding of the statistical analyst), attrition bias (post-randomization exclusions), selective reporting bias, and other potential sources of bias. The Cochrane risk of bias tool was used for this evaluation. Based on this tool, studies were classified into 3 categories: high, low, and unclear risk of bias. Table III provides an overview of the quality ratings of the included studies.
2.6. Ethical Considerations
The Ethics Committee at Mazandaran University of Medical Sciences, Sari, Iran approved this study on January 5, 2025 (Code: IR.MAZUMS.REC.1403.436). The review was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO) with the unique number CRD42024576970.
3. Results
3.1. Search results
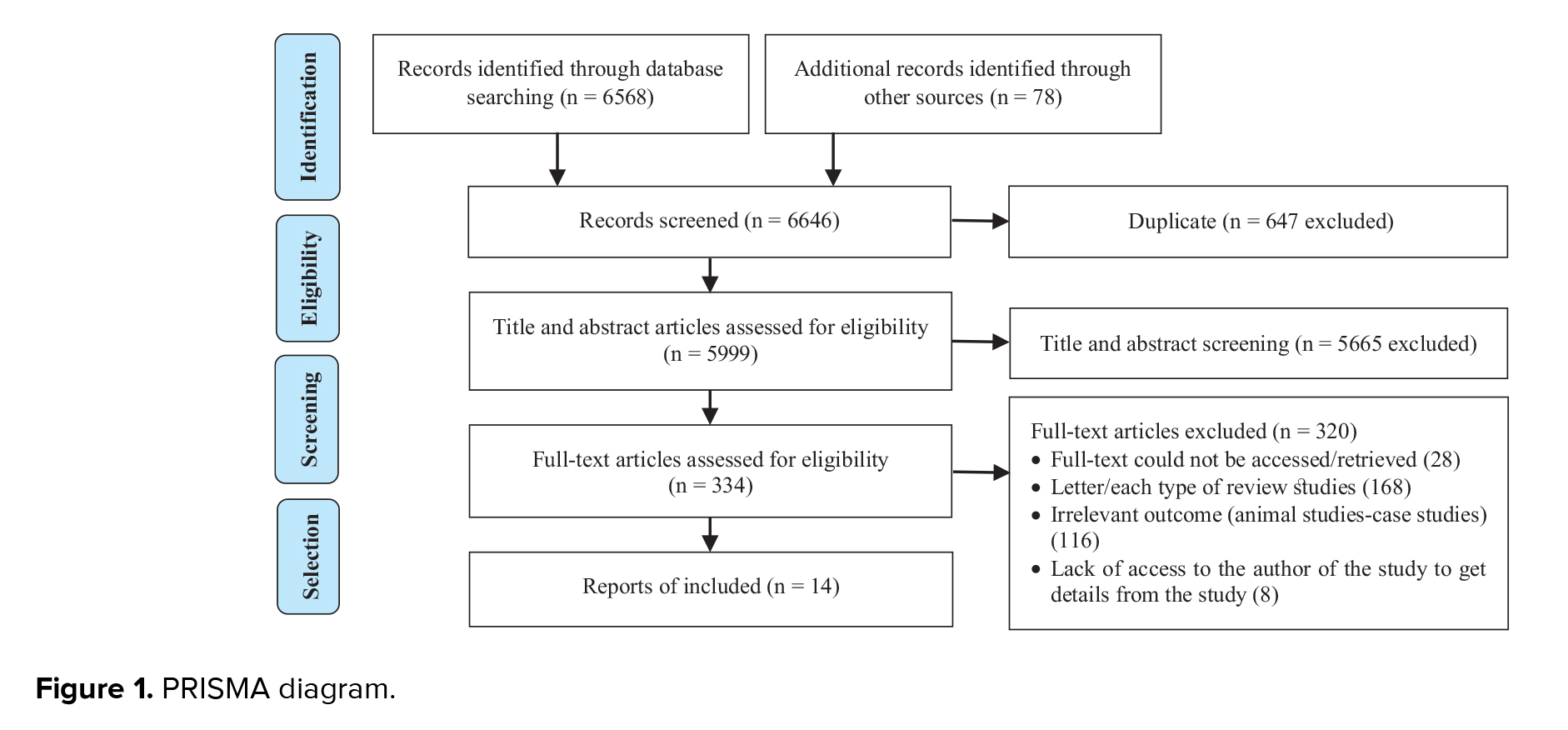
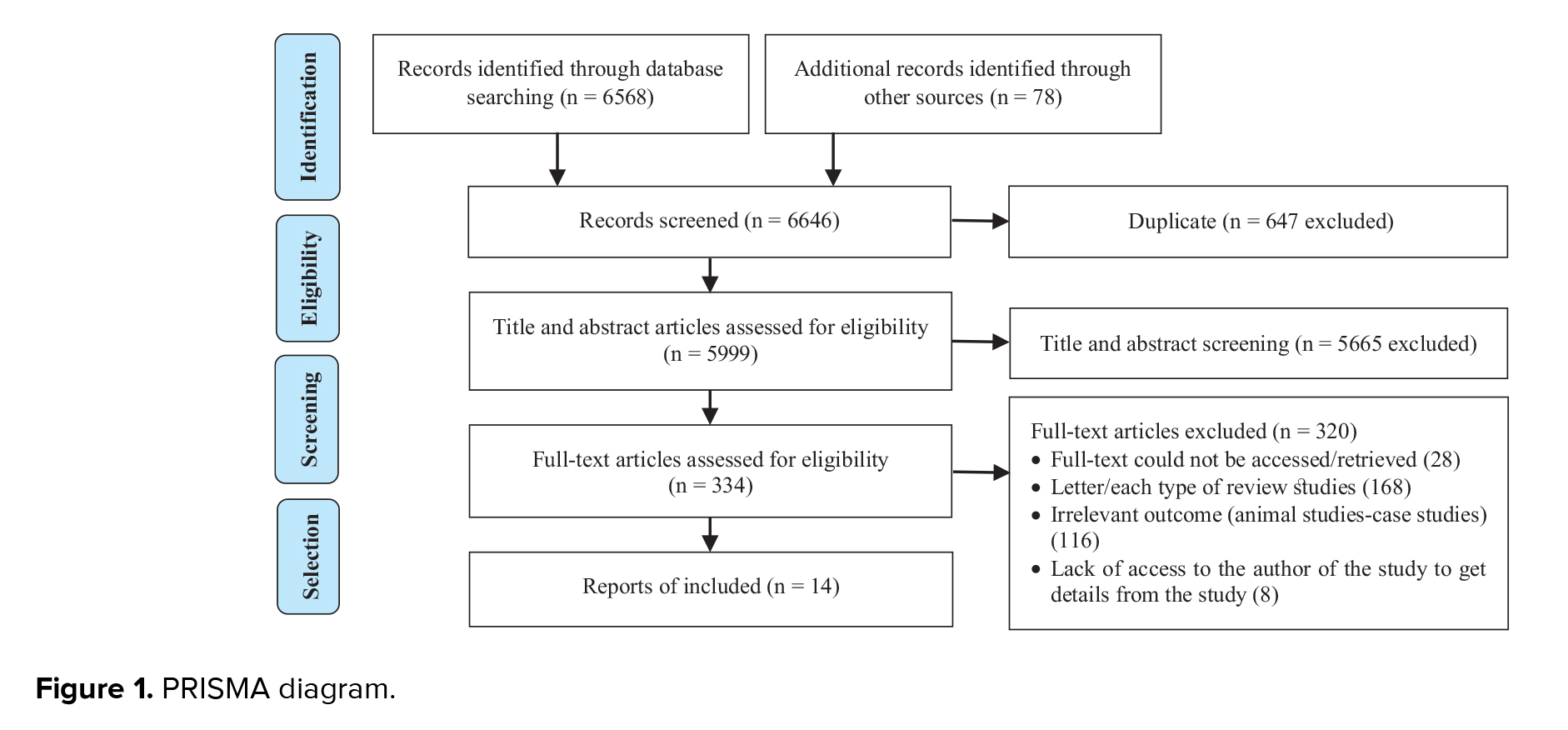
The researchers found 6646 articles, 6568 articles from the search, and 78 from other databases. In the process of searching for relevant articles related to the research topic, in addition to using well-known and established databases, 78 articles were identified through manual searching and other sources. These sources included articles referenced in other studies, unpublished reports, and research presented at conferences and scientific seminars that may not be indexed in official databases. The manual search of these articles contributed to enhancing the comprehensiveness and accuracy of the results, ensuring that the present study covers all important aspects.
After removing 647 duplicate records and excluding 5665 articles based on title and abstract evaluation, 334 articles underwent a comprehensive full-text assessment. During this process, 320 studies were excluded for various reasons, including full-text could not be accessed/retrieved (28), letter/each type of review studies (168), irrelevant outcome (animal studies-case studies) (116), lack of access to the author of the study to get details from the study (8). Finally, 14 articles were included in the study (Figure 1).
3.2. Participant information
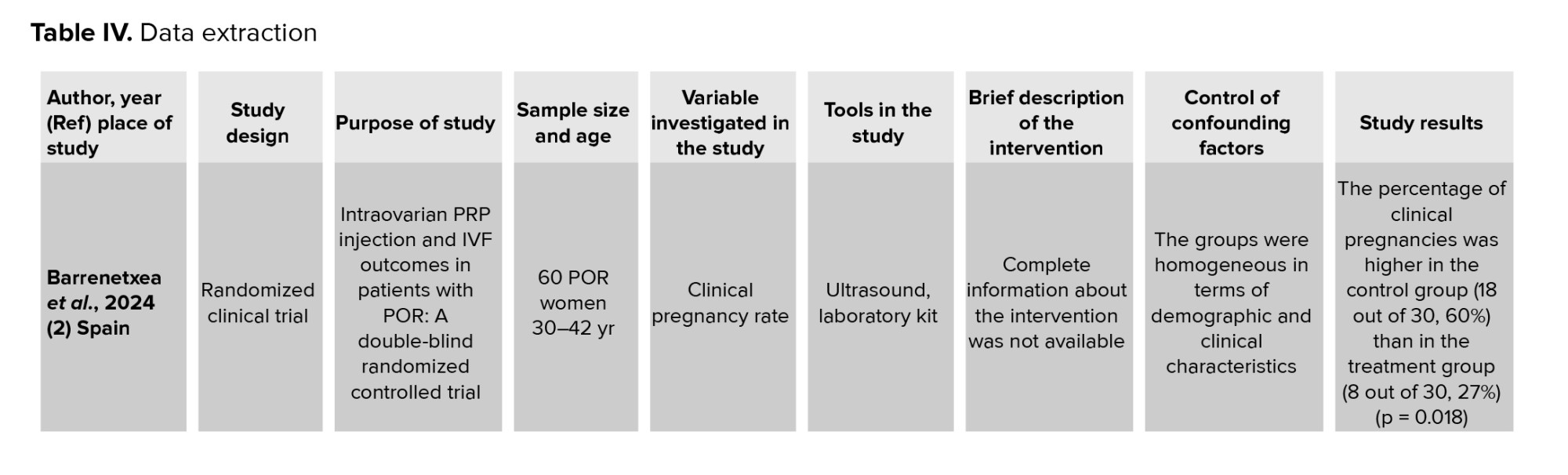
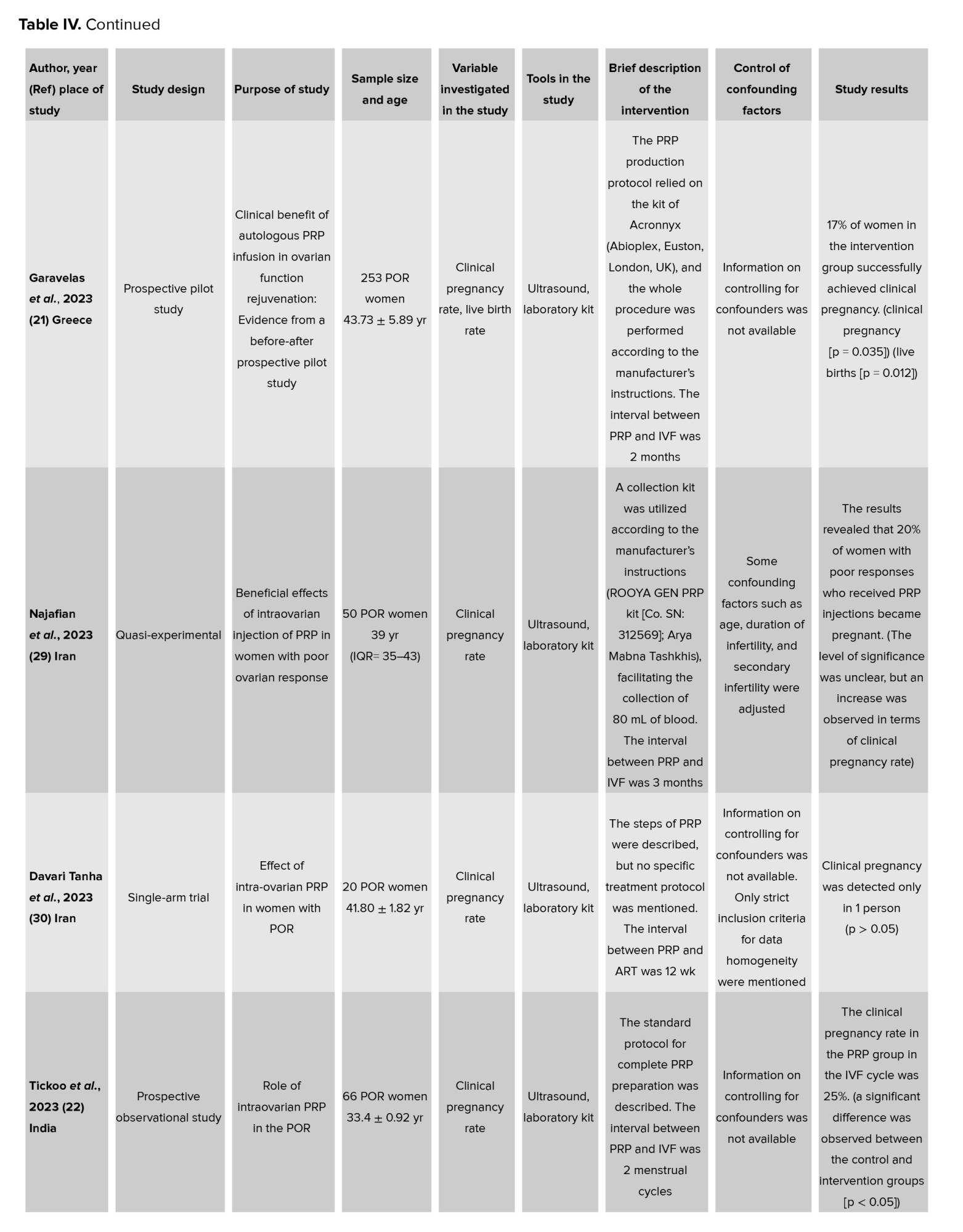
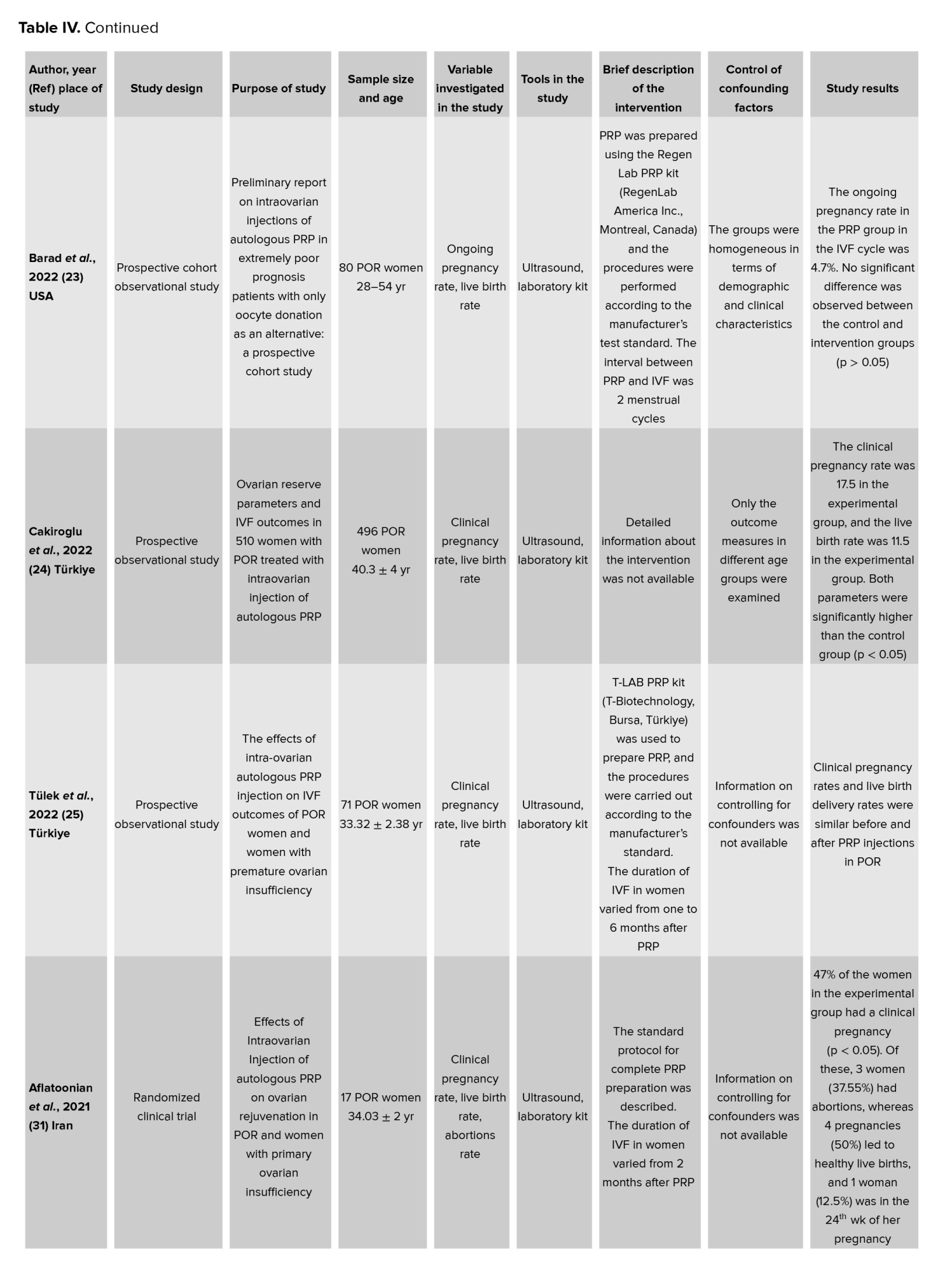
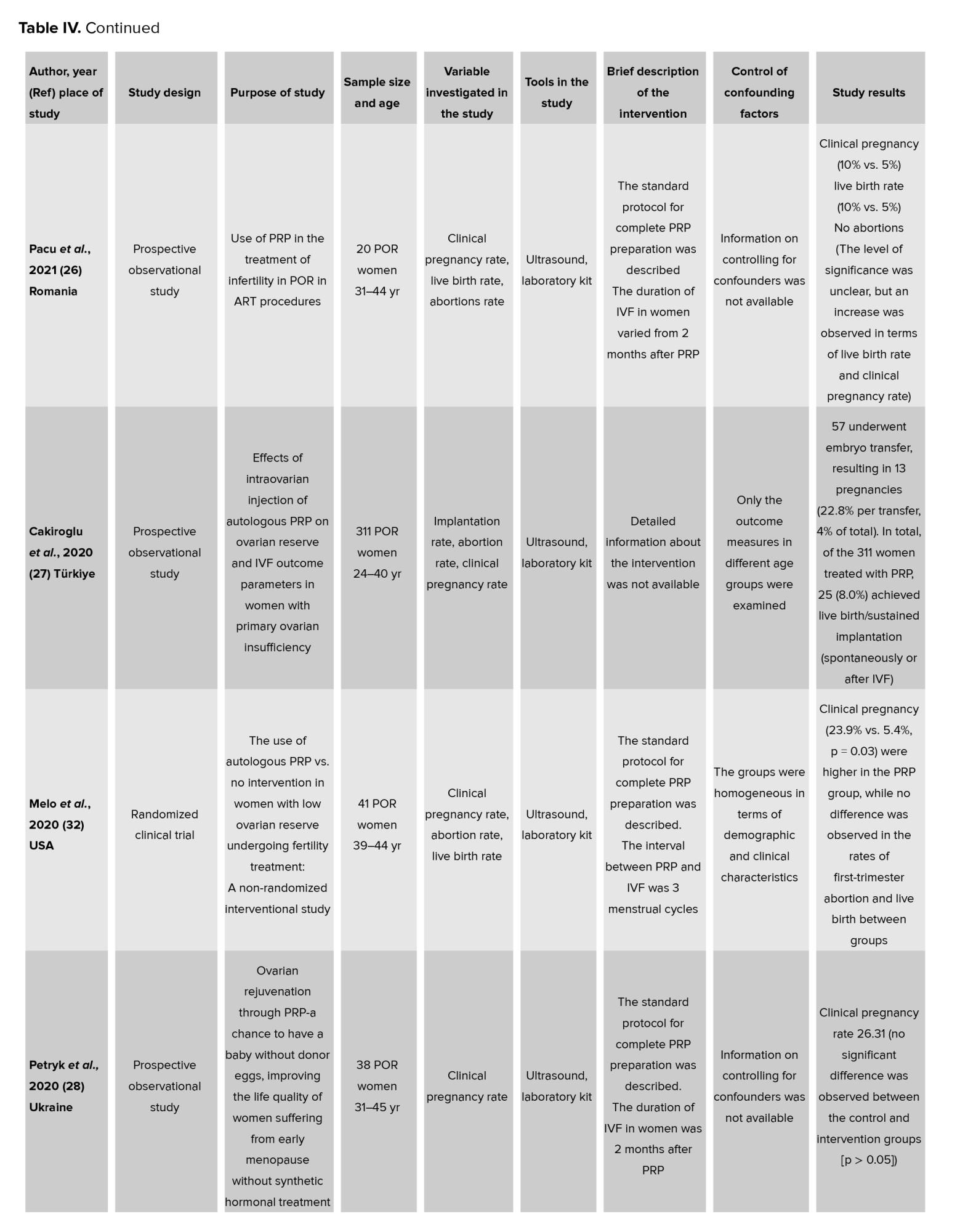
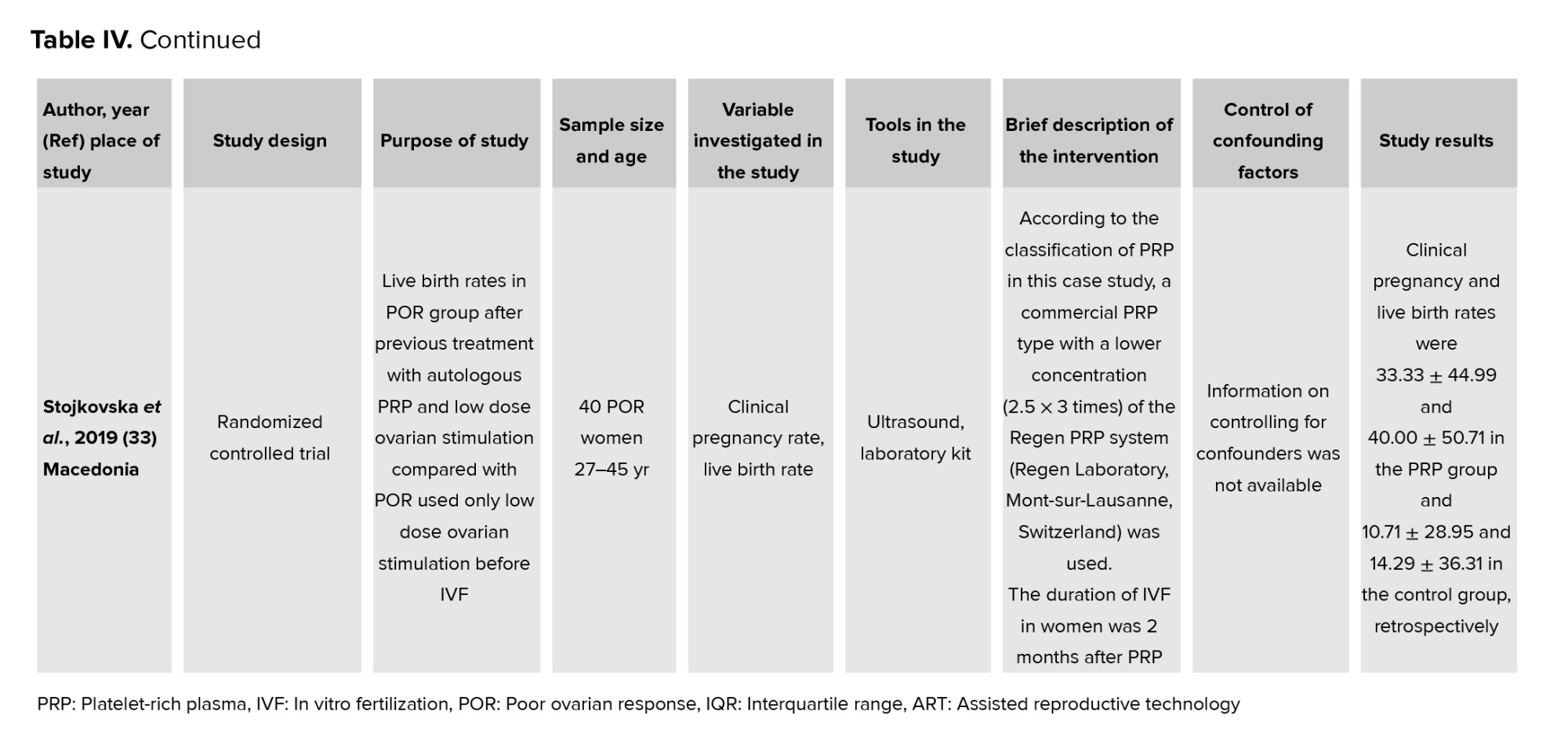
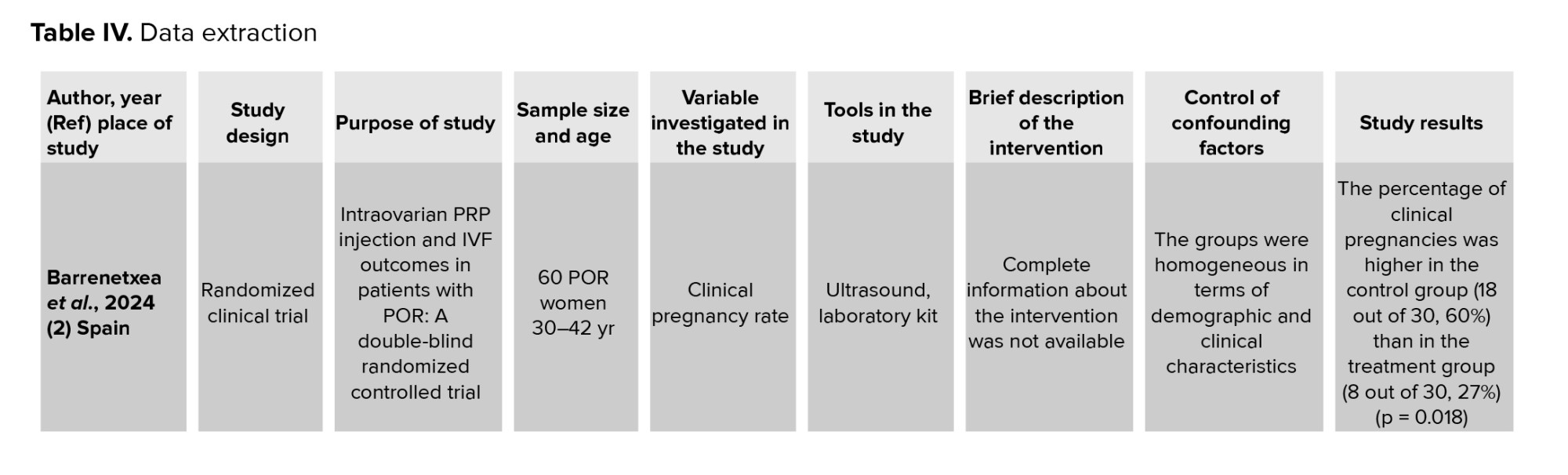
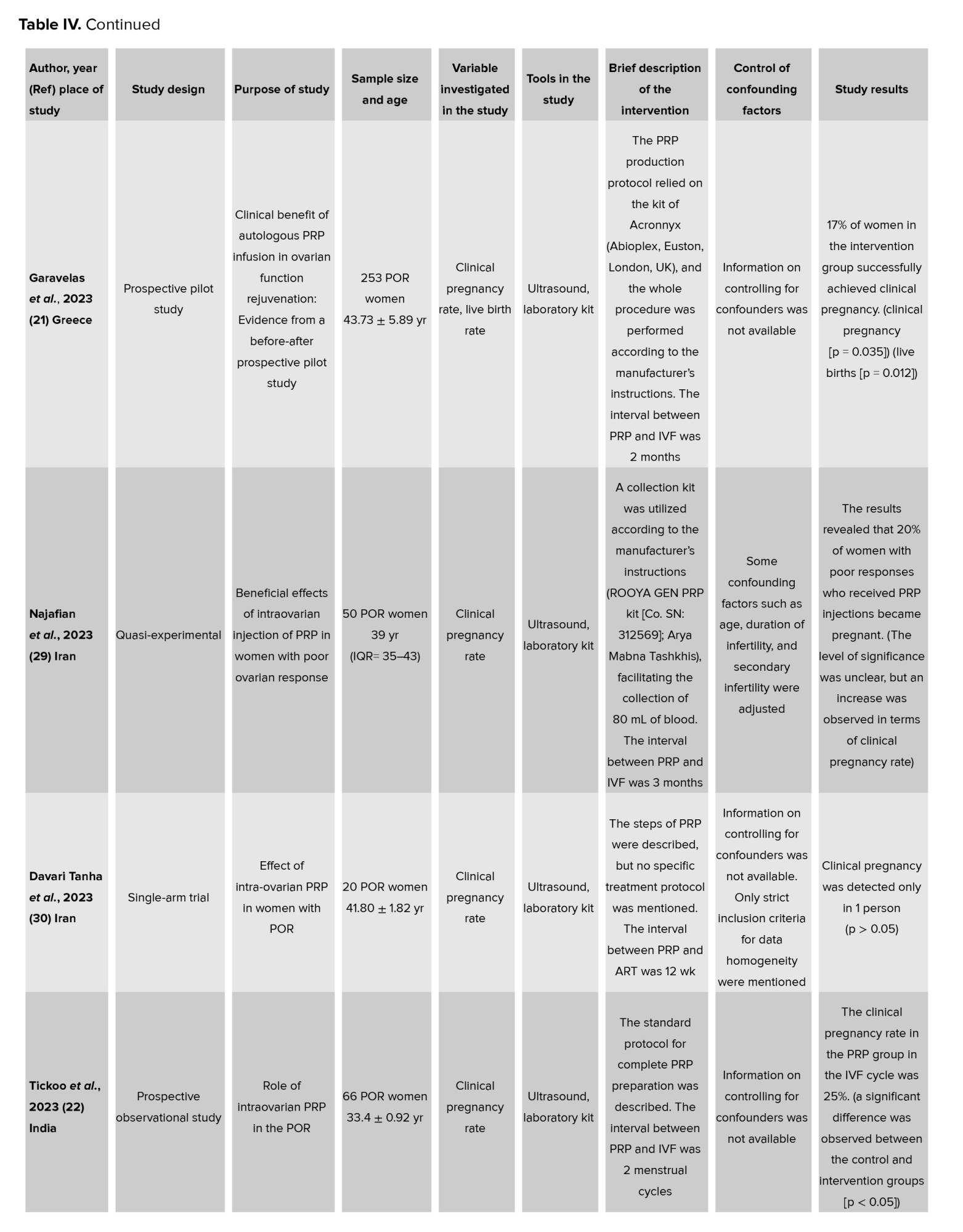
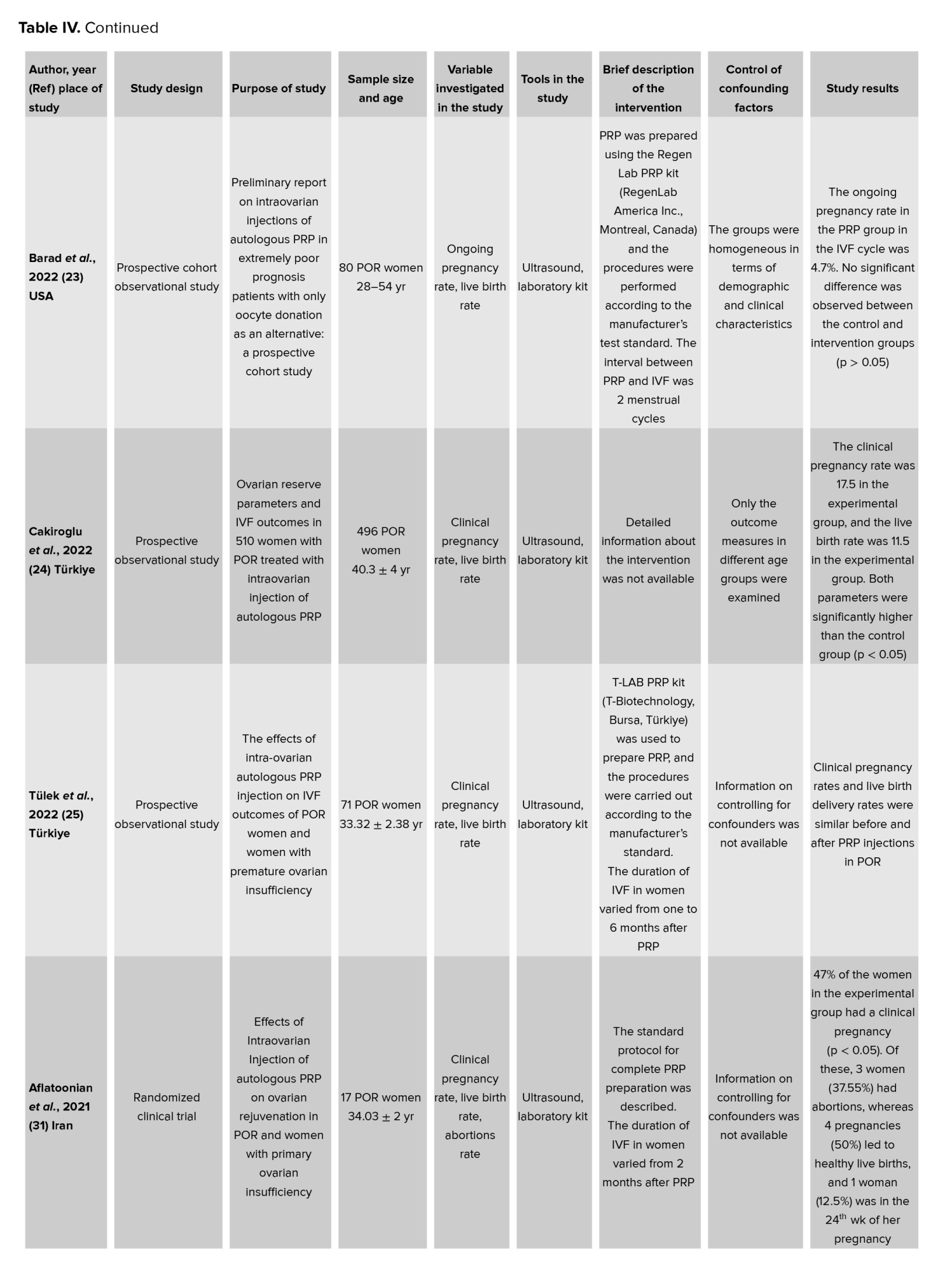
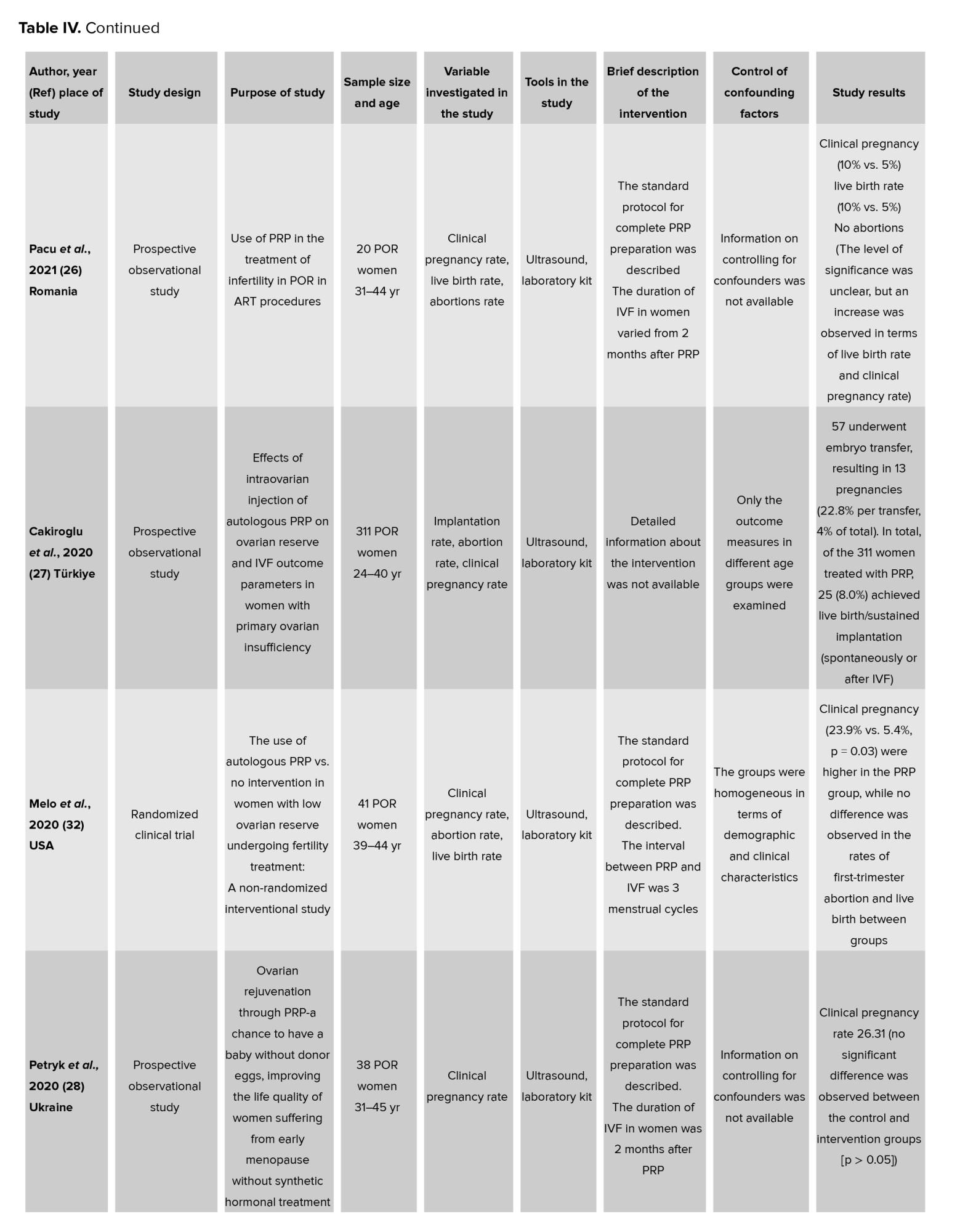
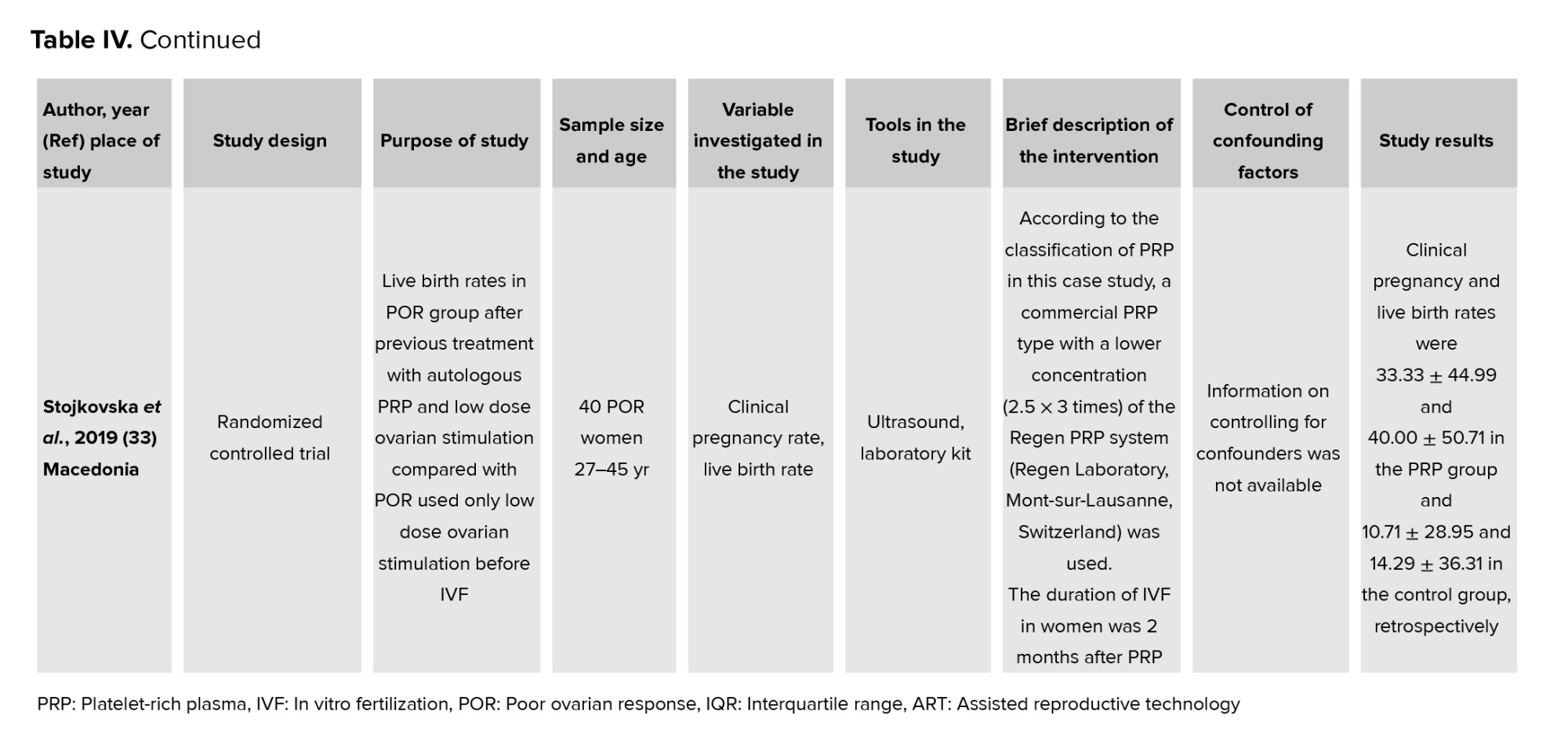
This study included women with ovarian PRP. All women were between the ages of 25 and 45. The total number of participants were 101,266 women undergoing infertility treatment. All studies compared the effectiveness of PRP (Table IV).
3.3. Abortion
The effect of ovarian PRP on the abortion rate in different studies has brought diverse and sometimes ambiguous results. In 3 studies, the procedure failed to show a clear and significant effect, and researchers also did not reach any definitive conclusions about its effectiveness or ineffectiveness (31, 27, 32). In another study, however, the results were different. In this study, an obvious difference was observed between the intervention group and the control group, so none of the participants in the intervention group had an abortion. This finding not only draws special attention to the possible role of PRP but also highlights the need for more detailed and extensive research to better understand this treatment method (26). However, these results may be influenced by the study design, type of intervention, and limited sample size, which could affect the overall outcome.
3.4. Clinical pregnancy
The effect of PRP on increasing the chances of clinical pregnancy success with IVF in women who have experienced repeated implantation failure is a controversial topic and of interest to researchers. Promising results were obtained in all the 6 studies, and PRP was able to significantly increase the probability of clinical pregnancy success, so this method was proposed as a promising approach and brought new hopes for this group of women (21, 22, 24, 31, 32, 33).
However, in contrast, 5 other studies reported opposite results, and the effect of PRP was considered statistically insignificant and negligible, which raised doubts about the actual effectiveness of this method (2, 30, 25, 27, 28). At the same time, 2 other studies presented inconclusive results, reporting neither a positive effect nor a clear lack of effect, which reflects the complexity of this area of research (29, 26). These diverse and sometimes contradictory findings provide a multifaceted picture of the effect of PRP on fertility and emphasize the need for more in-depth and rigorous research in this area. The variation in results is likely due to differences in patient selection criteria (such as the number of implantation failures) or PRP administration methods
3.5. Live birth
The effect of PRP on increasing the probability of live birth in IVF pregnancies in women with recurrent implantation failure has been a subject of mixed results in studies. In 5 studies, the procedure was able to significantly increase the probability of live birth and is presented as an effective treatment option for this group of women (21, 24, 31, 32, 33). These findings have illuminated glimmers of hope for the use of PRP in improving the outcomes of infertility treatments.
However, in 3 other studies, evidence showed no significant effect of this procedure, and conflicting results were reported, raising doubts about the actual effectiveness of PRP (23, 25, 27). Additionally, the results in 2 studies were presented inconclusively, and the effect of PRP in these studies was not clearly established (26). These inconsistencies highlight the complexity of PRP's effects on pregnancy success and live birth and emphasize the importance of conducting more comprehensive and rigorous studies to clarify the role of this procedure. A better understanding of this issue could help clarify the place of PRP in infertility treatments and provide more effective strategies. The live birth rate may be influenced by external factors such as embryo quality, IVF laboratory techniques, or the combination of PRP with other treatments.
3.6. Other parameters
Other outcomes studied in this study included implantation and ongoing pregnancy. One study indicated that the ongoing pregnancy rate in the PRP group in the IVF cycle was 4.7%. A significant difference was observed between the control and intervention groups (p < 0.05) (23). 2 studies also showed that PRP can increase the probability of implantation in infertile women (27, 33). But given other contradictory results, we cannot be certain about this.
4. Discussion
The present study was designed to investigate the effectiveness of intraovarian injection of autologous PRP on IVF outcomes in women with POR. The overall results of the study showed that, in 3 studies, no significant effect was observed on abortion rates. Still, in 1 study, no abortions were reported in the intervention group, raising concerns about the possible role of this procedure. In 5 studies, PRP significantly increased pregnancy success with IVF. In contrast, 6 studies found this effect to be non-significant, and 2 reported inconclusive results. In terms of live birth, 5 studies showed a positive effect of PRP, but 3 studies reported non-significant results, and 2 studies reported inconclusive results. One study showed an increase in ongoing pregnancy rates in the PRP group, and 2 studies showed an increase in implantation.
PRP is 1 of the new and interesting methods in the treatment of infertility, especially in women with recurrent implantation failure. The study of the effects of this method on important outcomes such as abortion rate, pregnancy success, and live births in different studies has yielded contradictory results, which require deeper analysis. These results not only help to understand the actual function of PRP but also reveal the limitations of this method. Regarding the effect of PRP on the abortion rate, 3 studies reported no clear and significant effect. This lack of significance could be due to several factors (31, 27, 32). One of these factors may be related to the study population and its characteristics. In studies that included women with more complex problems, such as severe endometrial damage or immune disorders, PRP alone may not be able to produce a significant effect. Also, study design and small sample sizes can affect the interpretability of results. Results are often ambiguous, especially in studies that are not well randomized and control for confounding variables.
In contrast, 1 study reported mixed results, showing that none of the women in the intervention group experienced an abortion (26). This finding suggests that PRP may have a beneficial effect in certain cases. Possible mechanisms for this effect include improving endometrial quality by increasing blood flow, stimulating tissue regeneration, and reducing inflammation. Reproductive loss in women is often caused by poor embryo quality and endometrial insufficiency. Ovarian PRP helps stimulate ovarian cell regeneration and improve mitochondrial function by using growth factors such as platelet-derived growth factor and insulin-like growth factor. These processes increase the quality of eggs and produce healthier embryos, which play a key role in successful implantation and prevention of abortion. It is worth noting that ovarian PRP reduces the risk of abortion by improving egg quality and, consequently, increasing the health of the embryo. High-quality embryos are less likely to have genetic or metabolic disorders, which are one of the main causes of abortion in the early stages of pregnancy. By enhancing ovarian function and improving egg quality, the embryos resulting from these eggs will be better in terms of stability and development, which reduces the risk of abortion. However, such a difference in study results suggests that the response to PRP may depend heavily on women's characteristics and clinical conditions.
Regarding clinical pregnancy success with IVF, 6 studies reported positive results, showing a significant increase in the probability of pregnancy in women who used PRP (21, 22, 24, 31, 32, 33). These findings suggest that PRP may play a vital role in improving embryo implantation. Healthier, higher-quality embryos send stronger biochemical signals that can stimulate endometrial co-receptors, increase the chance of successful implantation, and lead to clinical pregnancy. In other words, when the eggs are of better quality, the resulting embryos have a greater potential to interact with the endometrium, which can secondarily affect the endometrial environment. Ovarian PRP can also help improve hormonal balance, including increasing estrogen and progesterone levels. These hormones play a critical role in preparing the endometrium for more successful implantation and clinical pregnancy. Increased ovarian hormone production by PRP may help to enhance endometrial thickness and receptors. However, this effect is indirect and should be used in conjunction with uterine PRP to directly affect the endometrium. However, 5 other studies (2, 30, 25, 27, 28) found mixed results, and the effect of PRP on clinical pregnancy success was not statistically significant. These inconsistencies could be related to several factors. Differences in PRP preparation methods, including platelet concentration, timing of injections, and number of interventions, could influence the results. In addition, characteristics of the study population, such as older women, decreased ovarian reserve, or the presence of other comorbidities could reduce the effectiveness of PRP. Studies on live births have also yielded mixed results.
5 studies showed that PRP increased the likelihood of live birth (21, 24, 31, 32, 33). These results suggest that the positive effects of PRP on the endometrium and implantation process may lead to more successful and ongoing pregnancies. On the other hand, 3 studies reported no significant results on the effect of PRP on live birth (23, 25, 27). These differences may be related to similar reasons, such as study design, population characteristics, and differences in implementation protocols. Overall, the conflicting results of these studies suggest that although PRP can be effective in some situations, this effect is highly dependent on the individual women conditions, the implementation method, and study characteristics. Factors such as differences in the degree of inflammation, the quality of the eggs and embryos, and the condition of the endometrium may influence the final results. Also, the lack of specific standards for the preparation and injection of PRP makes the results of different studies difficult to compare. To gain a better understanding of the true effects of PRP, randomized, multicenter studies with larger sample sizes are essential. Such studies should help clarify the place of PRP in infertility treatment by carefully controlling confounding variables, providing standardized protocols, and analyzing the relevant biological mechanisms. Only with this approach can clinical decisions based on valid evidence and reliable results be provided to women.
Studies on the effects of PRP in women with POR have highlighted its potential to improve IVF outcomes. One study reported a 4.7% ongoing pregnancy rate in the PRP group, showing a statistically significant difference compared to the control group (p < 0.05) (23). This suggests that PRP may positively impact critical reproductive parameters, making it a potential option for women who have previously faced poor outcomes in IVF cycles. Additionally, 2 other studies found that PRP increases the likelihood of implantation in infertile women, emphasizing its role in improving embryo receptivity and implantation rates (27, 33). These findings underscore the growing interest in PRP as a therapeutic option in reproductive medicine. The significant differences between intervention and control groups in these studies indicate that PRP could be an effective adjunct in IVF protocols, especially for challenging cases like POR. However, despite the promising results, the overall pregnancy rate remains modest, suggesting the need for further investigations to understand its benefits and limitations. This evidence calls for larger, more comprehensive studies to confirm these outcomes and establish standardized protocols for PRP use in fertility treatments.
4.1. Strengths and limitations
The present study is the first comprehensive study on the effect of ovarian PRP in women with POR on post-IVF transfer parameters. In other words, this study investigated the long-term effect of ovarian PRP on the success of infertility treatment. Lack of access to the full text of some articles, and the inclusion of studies in Farsi and English were the limitations of this study. The existence of heterogeneity caused by the different instruments and results of the studies did not allow meta-analysis.
5. Conclusion
The findings on the impact of ovarian PRP in infertility treatments present a complex and multifaceted picture. While several studies provide strong evidence supporting its efficacy in reducing abortion rates and improving pregnancy and live birth outcomes, others report inconclusive or statistically insignificant effects. A few studies have also indicated continued pregnancy and successful implantation. These discrepancies suggest that the effectiveness of PRP may depend on a range of factors, including the characteristics of the study population, specific clinical conditions of the women, the protocols used for PRP preparation and administration, and the overall design of the studies.
Nevertheless, the promising results in studies demonstrating increased pregnancy success and live birth rates highlight PRP as a potentially innovative and effective treatment option for women experiencing recurrent implantation failure. However, the inconclusive or contradictory outcomes underscore the necessity of further comprehensive research with rigorously designed methodologies and control of influencing variables to reach definitive and scientifically robust conclusions. In summary, a deeper understanding of the mechanisms and effects of ovarian PRP, along with standardized protocols for its application, could pave the way for more effective and optimized infertility treatments. This approach holds the potential to enhance clinical outcomes and sustain hope for improved success rates in women struggling with recurrent implantation failure.
It should be noted that the overall results of this study are influenced by certain limitations present in the reviewed studies. While some studies accounted for important confounding factors, others did not consider these aspects. The duration of the intervention, in terms of frequency or time of effect, varied across the studies, which affects the overall findings. Moreover, the type of included studies also differed, impacting the strength of the results in each study.
Data Availability
All data generated during this study are included in this published article, and the additional files are available from the corresponding author. The datasets for this study can be found in the humanitas repository. Due to our internal policy, no raw data are available for external use. The datasets generated for this study are available upon request from the corresponding author.
Author Contributions
F. Safarloo, M. Zamaniyan, and S. Peivandi searched the literature, independently reviewed the articles for eligibility, collected the data, and drafted the manuscript. M. Pashazadeh and F. Safarloo contributed to the conception of the work, study design, writing the protocol, identifying the studies, and editing of the manuscript. All authors have read and approved the final manuscript.
Acknowledgments
We would like to thank all the embryologists and gynecologists working at the Kosar Humanitas Fertility Center, Sari, Iran. Artificial intelligence was not used to draft this article.
Conflict of Interest
The authors declare that there is no conflict of interest.
An inadequate ovarian response to gonadotropin injections is a key characteristic of poor ovarian response (POR) (1). In women with POR, ovarian stimulation during assisted reproductive technologies (ART), often results in a reduced number of retrieved oocytes, leading to lower pregnancy rates (2). Research indicates that the prevalence of POR ranges from 9-24% (3). Currently, egg donation is the primary treatment option for women with POR who exhibit an insufficient response to ovarian stimulation (4).
While the number of patients requiring egg donation is increasing, many women reject this approach due to cultural and ideological reasons (5). A significant proportion of women struggle with the idea of having a child using genetic material from another person (6). Additionally, ethical and religious concerns have led some countries to impose restrictions on the use of donor eggs, forcing women to seek alternative treatments, such as ovarian rejuvenation and methods aimed at enhancing ovarian response (7).
Platelet-rich plasma (PRP) has demonstrated beneficial effects on tissue regeneration, angiogenesis, inflammation regulation, and anabolism across various medical disciplines (8). However, its efficacy in the field of infertility, particularly regarding ovarian insufficiency, remains inconclusive (9).
Platelets are small cytoplasmic fragments derived from megakaryocytes in the bone marrow, measuring approximately 2 μm in diameter (10). The activation of alpha granules within platelets is a crucial step that determines the availability of bioactive molecules and, consequently, the quality of PRP (11).
In infertility-related discussions, PRP may enhance ovarian response in patients with POR through several mechanisms. One of the primary effects of PRP is the stimulation of blood flow to the ovaries (12). The growth factors in PRP can promote the expansion of blood vessels in the ovaries, increasing blood circulation, which in turn improves the nourishment and oxygen supply to ovarian cells (13). This can help enhance oocyte quality and follicular development. Additionally, PRP reduces inflammation and oxidative stress in the ovaries, creating a favorable environment for the repair and regeneration of ovarian tissue (14).
In addition to its blood circulation and anti-inflammatory effects, PRP can stimulate the proliferation and differentiation of granulosa cells and ovarian follicles (15). The growth factors in PRP assist in activating repair signaling pathways that play a key role in the regeneration and improvement of ovarian tissues. These processes may lead to an increase in the number of growing follicles and enhancement of oocyte quality (16). Therefore, by stimulating repair and regenerative processes in the ovaries, PRP may improve the chances of pregnancy in patients with POR.
Although further research is needed to confirm these mechanisms and its efficacy because a detailed study of this effect, especially in the long term, has not yet been conducted (17). The long-term effects of PRP have not been thoroughly investigated in these studies (18). Therefore, we aimed to conduct a study titled "Efficacy of intra-ovarian injection of autologous platelet-rich plasma on the outcome of in vitro fertilization in patients with poor ovarian response: A systematic review".
2. Materials and Methods
This systematic review was conducted according to the PRISMA guidelines (19). The search strategy was based on the PICO (P: population or participants; I: intervention; C: comparison; O: outcome) or PECO (P: population or participants; E: exposure; C: comparison; O: outcome) criteria for either observational studies or clinical trials. In these studies, the "population" was women undergoing infertility treatment. The "intervention or exposure" was ovarian PRP. The "control or comparator group" consisted of those who did not receive ovarian PRP. The "outcome" was miscarriage, implantation, clinical pregnancy, and live birth.
2.1. Literature search
This study is a systematic review conducted following the JBI methodology guidelines (20). The research community comprised all scientific articles related to ovarian PRP and its success in infertility treatment worldwide, indexed in at least one database. The first and second researchers conducted a comprehensive search in international databases, including PubMed, ScienceDirect, Scopus, Web of Science, Embase, Cochrane, and the Google Scholar search engine. In the process of searching for relevant articles related to the research topic, in addition to using well-known and established databases, articles were identified through manual searching and other sources. All articles were reviewed at every stage of the search and quality assessment by 2 independent researchers, and in case of any disagreement, a third author was consulted.
2.2. Search strategy
In order to find related articles in English-language databases, keywords were selected based on Mesh and included the combination of the words ("Platelet-Rich Plasma") OR (PRP) AND (IVF) OR ("In vitro fertilization") AND ("poor ovarian response") OR (POR) OR ("poor responder") in the plural and with the operators "OR" and "AND" were combined. To ensure that all relevant data were retained, a time frame was set and all published articles without time limits up to December 20, 2024 were included in the evaluation. To achieve the most comprehensive search possible, all final articles related to the topic were manually reviewed, allowing for the identification of any additional potential sources (Table I).
2.3. Inclusion and exclusion criteria
2.3.1. Search phase
Scientific articles published in PubMed, ScienceDirect, Scopus, Web of Science, Embase, and Cochrane databases. Articles published within a specified time period and those that were relevant to the main research topic (according to PICO or PECO as mentioned earlier). The following studies were considered eligible for inclusion in this scope study: observational studies (including cross-sectional, prospective, and retrospective cohort and case-control designs) and interventional studies (such as clinical trials, experimental trials, and quasi-experimental trials). The studies included were those that investigated the use of PRP therapy for ovarian treatment in the context of IVF globally. Articles in languages other than the target languages (e.g., English or Persian). Articles that do not fully provide the desired information in the research context.
2.3.2. Title and abstract screening stage
Inclusion criteria: research-related articles that refer to the main concepts of the research in the title and abstract. Articles that are aligned with your research based on keywords and PICO/PECO concepts.
Exclusion criteria: do not refer to the main concepts in the research.
2.3.3. Full review stage of articles
Eligibility criteria required participants to be women aged between 18 and 55 yr diagnosed with diminished ovarian reserve (DOR), premature ovarian failure, or premature ovarian insufficiency. Studies were included if they assessed participants both before and after intra-ovarian PRP injection. A participant was classified as having DOR if at least 1 of the following criteria was met: basal follicle-stimulating hormone > 15 IU/L, basal anti-Müllerian hormone < 1 ng/ml, antral follicle count < 5, meeting the Bologna criteria for DOR, meeting POSEIDON criteria groups 3 or 4, associated with low prognosis in ART outcomes.
Both randomized and non-randomized studies were eligible for inclusion. Studies that did not contain original research data, such as letters to the editor, correspondence pieces, or reviews, were excluded from the analysis.
The intervention under investigation was intra-ovarian PRP injection, regardless of the number of administrations, the volume of PRP injected, or the method of PRP preparation and administration. Studies using self-controlled designs, where outcomes before the intervention served as the basis for comparison, were included.
In the reviewed studies, the primary outcome measured was the biochemical pregnancy rate, defined as a positive pregnancy test or elevated β-human chorionic gonadotropin levels 2 wk after embryo transfer. Secondary outcomes included the rate of spontaneous pregnancies, live birth rates, implantation, clinical pregnancy, abortion, and ongoing pregnancy.
This approach ensures a comprehensive assessment of PRP’s efficacy and its impact on reproductive outcomes in women with compromised ovarian function. It should be noted that in studies where participants had male infertility factors or the participants in the study used methods of ART other than IVF, they were excluded from the analysis.
2.4. Data collection and extraction
2 authors (F. Safarloo, M. Zamaniyan) independently reviewed the collected articles and extracted the data using a uniform, standardized data collection form. If a study was deemed relevant, its full text was reviewed for further assessment. Any discrepancies were resolved through discussion with a third author (S. Peivandi) during the search and screening procedure. The variables extracted from the articles included the year of study and author's name, place of study, study design, purpose of the study, sample size and statistical population, variables investigated in the study, tools used in the study, and study results.
2.5. Methodological quality assessment (risk of bias assessment)
The Newcastle-Ottawa scale (NOS) for cohort studies table II is a widely recognized tool for assessing the quality and potential risk of bias in observational research (18, 19). The NOS evaluates 3 main domains: selection, comparability, and outcome. These domains are further divided into 9 specific items, with slight variations in the scoring system for cohort, cross-sectional, and case-control studies. For cohort studies, quality is classified as follows:
Good quality: 3 or 4 stars in the selection domain, 1 or 2 stars in the comparability domain, and 2 or 3 stars in the outcome/exposure domain.
Fair quality: 2 stars in the selection domain, 1 or 2 stars in the comparability domain, and 2 or 3 stars in the outcome/exposure domain (18, 19).
Poor quality: 0 or 1 star in the selection domain, 0 stars in the comparability domain, or 0 or 1 star in the outcome/exposure domain.
To assess the quality of the studies included in this systematic review, various types of bias were examined, including selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and assessors), detection bias (blinding of the statistical analyst), attrition bias (post-randomization exclusions), selective reporting bias, and other potential sources of bias. The Cochrane risk of bias tool was used for this evaluation. Based on this tool, studies were classified into 3 categories: high, low, and unclear risk of bias. Table III provides an overview of the quality ratings of the included studies.
2.6. Ethical Considerations
The Ethics Committee at Mazandaran University of Medical Sciences, Sari, Iran approved this study on January 5, 2025 (Code: IR.MAZUMS.REC.1403.436). The review was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO) with the unique number CRD42024576970.
3. Results
3.1. Search results
The researchers found 6646 articles, 6568 articles from the search, and 78 from other databases. In the process of searching for relevant articles related to the research topic, in addition to using well-known and established databases, 78 articles were identified through manual searching and other sources. These sources included articles referenced in other studies, unpublished reports, and research presented at conferences and scientific seminars that may not be indexed in official databases. The manual search of these articles contributed to enhancing the comprehensiveness and accuracy of the results, ensuring that the present study covers all important aspects.
After removing 647 duplicate records and excluding 5665 articles based on title and abstract evaluation, 334 articles underwent a comprehensive full-text assessment. During this process, 320 studies were excluded for various reasons, including full-text could not be accessed/retrieved (28), letter/each type of review studies (168), irrelevant outcome (animal studies-case studies) (116), lack of access to the author of the study to get details from the study (8). Finally, 14 articles were included in the study (Figure 1).
3.2. Participant information
This study included women with ovarian PRP. All women were between the ages of 25 and 45. The total number of participants were 101,266 women undergoing infertility treatment. All studies compared the effectiveness of PRP (Table IV).
3.3. Abortion
The effect of ovarian PRP on the abortion rate in different studies has brought diverse and sometimes ambiguous results. In 3 studies, the procedure failed to show a clear and significant effect, and researchers also did not reach any definitive conclusions about its effectiveness or ineffectiveness (31, 27, 32). In another study, however, the results were different. In this study, an obvious difference was observed between the intervention group and the control group, so none of the participants in the intervention group had an abortion. This finding not only draws special attention to the possible role of PRP but also highlights the need for more detailed and extensive research to better understand this treatment method (26). However, these results may be influenced by the study design, type of intervention, and limited sample size, which could affect the overall outcome.
3.4. Clinical pregnancy
The effect of PRP on increasing the chances of clinical pregnancy success with IVF in women who have experienced repeated implantation failure is a controversial topic and of interest to researchers. Promising results were obtained in all the 6 studies, and PRP was able to significantly increase the probability of clinical pregnancy success, so this method was proposed as a promising approach and brought new hopes for this group of women (21, 22, 24, 31, 32, 33).
However, in contrast, 5 other studies reported opposite results, and the effect of PRP was considered statistically insignificant and negligible, which raised doubts about the actual effectiveness of this method (2, 30, 25, 27, 28). At the same time, 2 other studies presented inconclusive results, reporting neither a positive effect nor a clear lack of effect, which reflects the complexity of this area of research (29, 26). These diverse and sometimes contradictory findings provide a multifaceted picture of the effect of PRP on fertility and emphasize the need for more in-depth and rigorous research in this area. The variation in results is likely due to differences in patient selection criteria (such as the number of implantation failures) or PRP administration methods
3.5. Live birth
The effect of PRP on increasing the probability of live birth in IVF pregnancies in women with recurrent implantation failure has been a subject of mixed results in studies. In 5 studies, the procedure was able to significantly increase the probability of live birth and is presented as an effective treatment option for this group of women (21, 24, 31, 32, 33). These findings have illuminated glimmers of hope for the use of PRP in improving the outcomes of infertility treatments.
However, in 3 other studies, evidence showed no significant effect of this procedure, and conflicting results were reported, raising doubts about the actual effectiveness of PRP (23, 25, 27). Additionally, the results in 2 studies were presented inconclusively, and the effect of PRP in these studies was not clearly established (26). These inconsistencies highlight the complexity of PRP's effects on pregnancy success and live birth and emphasize the importance of conducting more comprehensive and rigorous studies to clarify the role of this procedure. A better understanding of this issue could help clarify the place of PRP in infertility treatments and provide more effective strategies. The live birth rate may be influenced by external factors such as embryo quality, IVF laboratory techniques, or the combination of PRP with other treatments.
3.6. Other parameters
Other outcomes studied in this study included implantation and ongoing pregnancy. One study indicated that the ongoing pregnancy rate in the PRP group in the IVF cycle was 4.7%. A significant difference was observed between the control and intervention groups (p < 0.05) (23). 2 studies also showed that PRP can increase the probability of implantation in infertile women (27, 33). But given other contradictory results, we cannot be certain about this.
4. Discussion
The present study was designed to investigate the effectiveness of intraovarian injection of autologous PRP on IVF outcomes in women with POR. The overall results of the study showed that, in 3 studies, no significant effect was observed on abortion rates. Still, in 1 study, no abortions were reported in the intervention group, raising concerns about the possible role of this procedure. In 5 studies, PRP significantly increased pregnancy success with IVF. In contrast, 6 studies found this effect to be non-significant, and 2 reported inconclusive results. In terms of live birth, 5 studies showed a positive effect of PRP, but 3 studies reported non-significant results, and 2 studies reported inconclusive results. One study showed an increase in ongoing pregnancy rates in the PRP group, and 2 studies showed an increase in implantation.
PRP is 1 of the new and interesting methods in the treatment of infertility, especially in women with recurrent implantation failure. The study of the effects of this method on important outcomes such as abortion rate, pregnancy success, and live births in different studies has yielded contradictory results, which require deeper analysis. These results not only help to understand the actual function of PRP but also reveal the limitations of this method. Regarding the effect of PRP on the abortion rate, 3 studies reported no clear and significant effect. This lack of significance could be due to several factors (31, 27, 32). One of these factors may be related to the study population and its characteristics. In studies that included women with more complex problems, such as severe endometrial damage or immune disorders, PRP alone may not be able to produce a significant effect. Also, study design and small sample sizes can affect the interpretability of results. Results are often ambiguous, especially in studies that are not well randomized and control for confounding variables.
In contrast, 1 study reported mixed results, showing that none of the women in the intervention group experienced an abortion (26). This finding suggests that PRP may have a beneficial effect in certain cases. Possible mechanisms for this effect include improving endometrial quality by increasing blood flow, stimulating tissue regeneration, and reducing inflammation. Reproductive loss in women is often caused by poor embryo quality and endometrial insufficiency. Ovarian PRP helps stimulate ovarian cell regeneration and improve mitochondrial function by using growth factors such as platelet-derived growth factor and insulin-like growth factor. These processes increase the quality of eggs and produce healthier embryos, which play a key role in successful implantation and prevention of abortion. It is worth noting that ovarian PRP reduces the risk of abortion by improving egg quality and, consequently, increasing the health of the embryo. High-quality embryos are less likely to have genetic or metabolic disorders, which are one of the main causes of abortion in the early stages of pregnancy. By enhancing ovarian function and improving egg quality, the embryos resulting from these eggs will be better in terms of stability and development, which reduces the risk of abortion. However, such a difference in study results suggests that the response to PRP may depend heavily on women's characteristics and clinical conditions.
Regarding clinical pregnancy success with IVF, 6 studies reported positive results, showing a significant increase in the probability of pregnancy in women who used PRP (21, 22, 24, 31, 32, 33). These findings suggest that PRP may play a vital role in improving embryo implantation. Healthier, higher-quality embryos send stronger biochemical signals that can stimulate endometrial co-receptors, increase the chance of successful implantation, and lead to clinical pregnancy. In other words, when the eggs are of better quality, the resulting embryos have a greater potential to interact with the endometrium, which can secondarily affect the endometrial environment. Ovarian PRP can also help improve hormonal balance, including increasing estrogen and progesterone levels. These hormones play a critical role in preparing the endometrium for more successful implantation and clinical pregnancy. Increased ovarian hormone production by PRP may help to enhance endometrial thickness and receptors. However, this effect is indirect and should be used in conjunction with uterine PRP to directly affect the endometrium. However, 5 other studies (2, 30, 25, 27, 28) found mixed results, and the effect of PRP on clinical pregnancy success was not statistically significant. These inconsistencies could be related to several factors. Differences in PRP preparation methods, including platelet concentration, timing of injections, and number of interventions, could influence the results. In addition, characteristics of the study population, such as older women, decreased ovarian reserve, or the presence of other comorbidities could reduce the effectiveness of PRP. Studies on live births have also yielded mixed results.
5 studies showed that PRP increased the likelihood of live birth (21, 24, 31, 32, 33). These results suggest that the positive effects of PRP on the endometrium and implantation process may lead to more successful and ongoing pregnancies. On the other hand, 3 studies reported no significant results on the effect of PRP on live birth (23, 25, 27). These differences may be related to similar reasons, such as study design, population characteristics, and differences in implementation protocols. Overall, the conflicting results of these studies suggest that although PRP can be effective in some situations, this effect is highly dependent on the individual women conditions, the implementation method, and study characteristics. Factors such as differences in the degree of inflammation, the quality of the eggs and embryos, and the condition of the endometrium may influence the final results. Also, the lack of specific standards for the preparation and injection of PRP makes the results of different studies difficult to compare. To gain a better understanding of the true effects of PRP, randomized, multicenter studies with larger sample sizes are essential. Such studies should help clarify the place of PRP in infertility treatment by carefully controlling confounding variables, providing standardized protocols, and analyzing the relevant biological mechanisms. Only with this approach can clinical decisions based on valid evidence and reliable results be provided to women.
Studies on the effects of PRP in women with POR have highlighted its potential to improve IVF outcomes. One study reported a 4.7% ongoing pregnancy rate in the PRP group, showing a statistically significant difference compared to the control group (p < 0.05) (23). This suggests that PRP may positively impact critical reproductive parameters, making it a potential option for women who have previously faced poor outcomes in IVF cycles. Additionally, 2 other studies found that PRP increases the likelihood of implantation in infertile women, emphasizing its role in improving embryo receptivity and implantation rates (27, 33). These findings underscore the growing interest in PRP as a therapeutic option in reproductive medicine. The significant differences between intervention and control groups in these studies indicate that PRP could be an effective adjunct in IVF protocols, especially for challenging cases like POR. However, despite the promising results, the overall pregnancy rate remains modest, suggesting the need for further investigations to understand its benefits and limitations. This evidence calls for larger, more comprehensive studies to confirm these outcomes and establish standardized protocols for PRP use in fertility treatments.
4.1. Strengths and limitations
The present study is the first comprehensive study on the effect of ovarian PRP in women with POR on post-IVF transfer parameters. In other words, this study investigated the long-term effect of ovarian PRP on the success of infertility treatment. Lack of access to the full text of some articles, and the inclusion of studies in Farsi and English were the limitations of this study. The existence of heterogeneity caused by the different instruments and results of the studies did not allow meta-analysis.
5. Conclusion
The findings on the impact of ovarian PRP in infertility treatments present a complex and multifaceted picture. While several studies provide strong evidence supporting its efficacy in reducing abortion rates and improving pregnancy and live birth outcomes, others report inconclusive or statistically insignificant effects. A few studies have also indicated continued pregnancy and successful implantation. These discrepancies suggest that the effectiveness of PRP may depend on a range of factors, including the characteristics of the study population, specific clinical conditions of the women, the protocols used for PRP preparation and administration, and the overall design of the studies.
Nevertheless, the promising results in studies demonstrating increased pregnancy success and live birth rates highlight PRP as a potentially innovative and effective treatment option for women experiencing recurrent implantation failure. However, the inconclusive or contradictory outcomes underscore the necessity of further comprehensive research with rigorously designed methodologies and control of influencing variables to reach definitive and scientifically robust conclusions. In summary, a deeper understanding of the mechanisms and effects of ovarian PRP, along with standardized protocols for its application, could pave the way for more effective and optimized infertility treatments. This approach holds the potential to enhance clinical outcomes and sustain hope for improved success rates in women struggling with recurrent implantation failure.
It should be noted that the overall results of this study are influenced by certain limitations present in the reviewed studies. While some studies accounted for important confounding factors, others did not consider these aspects. The duration of the intervention, in terms of frequency or time of effect, varied across the studies, which affects the overall findings. Moreover, the type of included studies also differed, impacting the strength of the results in each study.
Data Availability
All data generated during this study are included in this published article, and the additional files are available from the corresponding author. The datasets for this study can be found in the humanitas repository. Due to our internal policy, no raw data are available for external use. The datasets generated for this study are available upon request from the corresponding author.
Author Contributions
F. Safarloo, M. Zamaniyan, and S. Peivandi searched the literature, independently reviewed the articles for eligibility, collected the data, and drafted the manuscript. M. Pashazadeh and F. Safarloo contributed to the conception of the work, study design, writing the protocol, identifying the studies, and editing of the manuscript. All authors have read and approved the final manuscript.
Acknowledgments
We would like to thank all the embryologists and gynecologists working at the Kosar Humanitas Fertility Center, Sari, Iran. Artificial intelligence was not used to draft this article.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Review Article |
Subject:
Reproductive Biology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |








