Tue, Jan 27, 2026
[Archive]
Volume 23, Issue 10 (October 2025)
IJRM 2025, 23(10): 853-858 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Radi V, Mohammadi N. Fetus-in-fetu, a rare congenital anomaly: A case report. IJRM 2025; 23 (10) :853-858
URL: http://ijrm.ir/article-1-3611-en.html
URL: http://ijrm.ir/article-1-3611-en.html
1- Department of Gynecology and Obstetrics, Bentolhoda Hospital, North Khorasan University of Medical Sciences, Bojnord, Iran. , drvidaradi@mums.ac.ir
2- Department of Gynecology and Obstetrics, Bentolhoda Hospital, North Khorasan University of Medical Sciences, Bojnord, Iran.
2- Department of Gynecology and Obstetrics, Bentolhoda Hospital, North Khorasan University of Medical Sciences, Bojnord, Iran.
Full-Text [PDF 832 kb]
(351 Downloads)
| Abstract (HTML) (265 Views)
Full-Text: (1 Views)
1. Introduction
Fetus-in-fetu (FIF) is a rare congenital anomaly characterized by the presence of a malformed, parasitic twin enclosed within its normally developing counterpart. It results from abnormal embryogenesis during early twinning, typically in monochorionic diamniotic pregnancies. FIF is an exceptionally uncommon condition, with an estimated incidence of approximately 1 in 500,000 live births and fewer than 200 reported cases worldwide (1, 2).
Clinically, FIF most often presents as an abdominal mass detected in infancy, usually located in the retroperitoneal space, although other sites have been described. Early and accurate diagnosis is essential, as FIF must be differentiated from teratomas, which have different management strategies and malignant potential. Recognizing the distinguishing features of FIF facilitates appropriate treatment and improves patient outcomes.
2. Case Presentation
A 21-yr-old pregnant woman, in her second pregnancy, presented at 35 + 1/7 wk of gestation. This rare case was observed in Bentolhoda hospital, Bojnord, Iran. She had previously delivered a healthy full-term baby girl via vaginal delivery 2 yr earlier. We confirm that the pregnancy occurred spontaneously without assisted reproductive technologies. The pregnancy had been uneventful until the third trimester, at which point the case was referred for a routine ultrasound. During this examination, a fetal abdominal mass was incidentally detected. The relatively late diagnosis at 33 wk was primarily due to delayed referral to specialist care and limited access to detailed prenatal imaging earlier in pregnancy. Magnetic resonance imaging (MRI) was not performed in this case; prenatal diagnosis and surgical planning relied on detailed ultrasound imaging.
The mother reported no significant medical history, and the father also had no history of significant illness. Both parents are first cousins with blood type A+. There is no known family history of genetic disorders or hereditary diseases. The case had been following a routine prenatal care regimen, including folic acid supplementation from the start of the pregnancy. Additionally, she had received a single dose of the COVID-19 vaccine. She did not receive specialized obstetric care such as high-risk pregnancy monitoring, genetic counseling, or frequent prenatal ultrasounds, and instead attended routine prenatal check-ups at a local health center. The case had previously undergone an uncomplicated vaginal delivery. No history of genetic testing or nuchal translucency screening was observed due to a late referral.
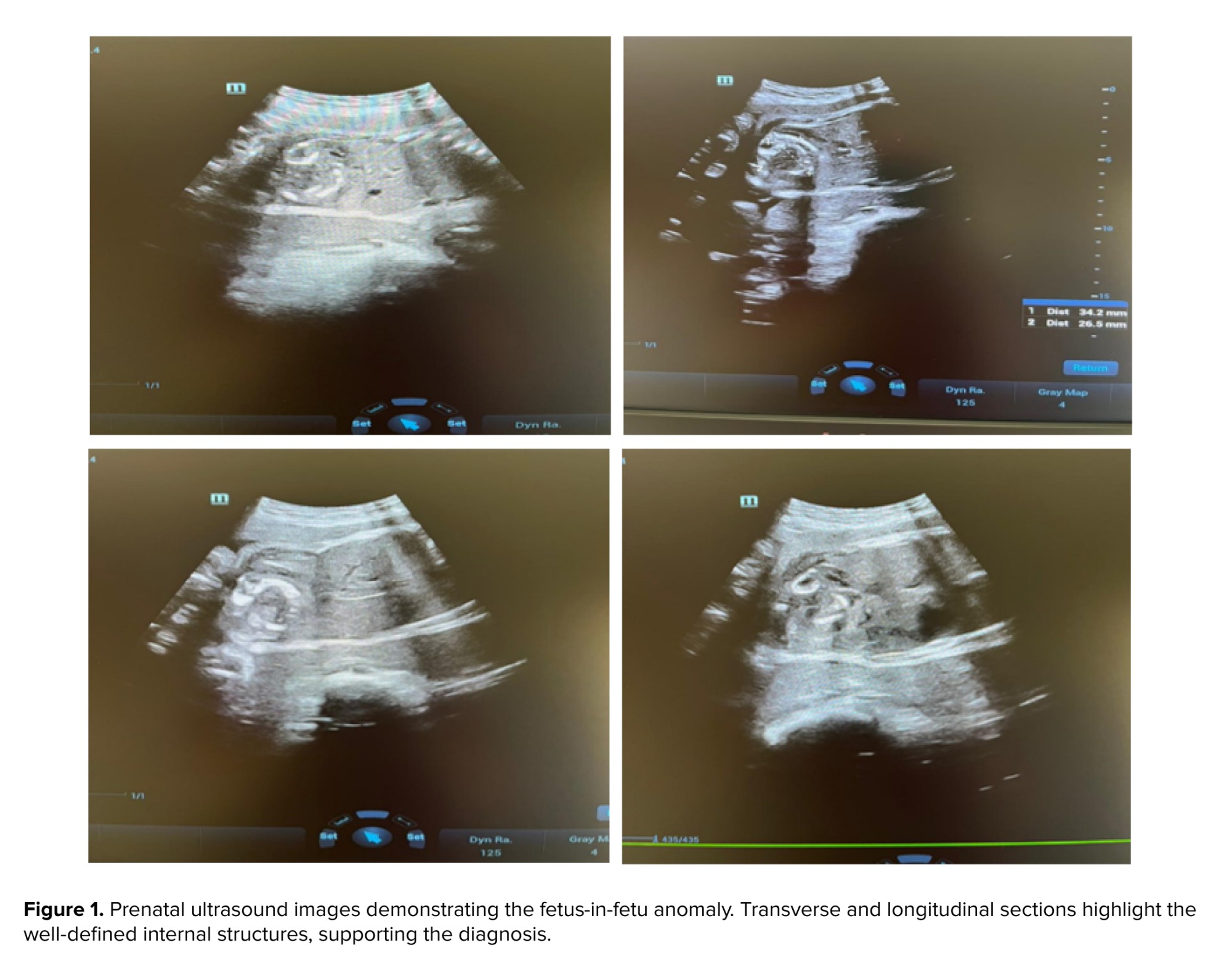
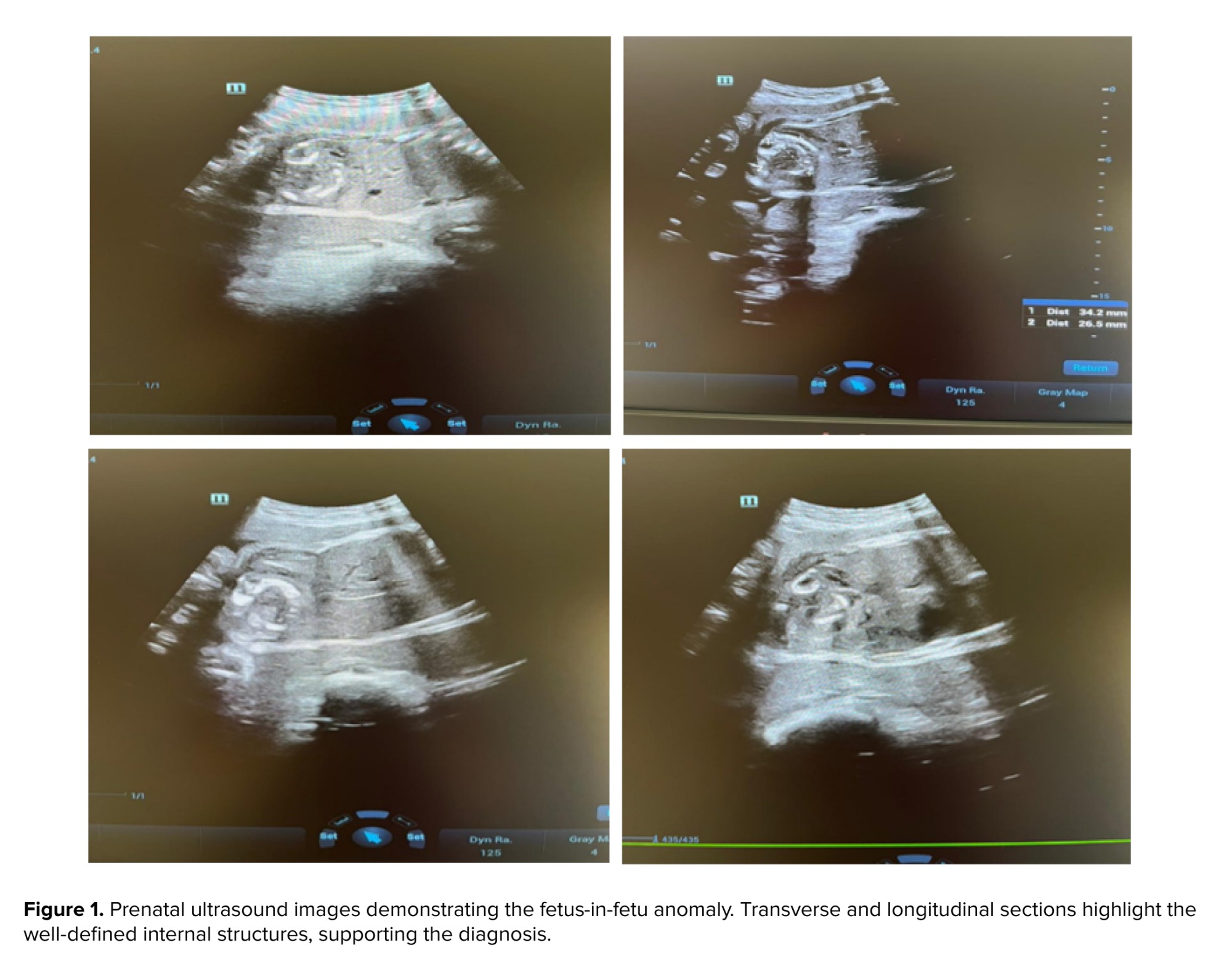
At 33rd wk of gestation, a routine ultrasound revealed a well-formed fetus with an estimated weight of 2200 gr and a normal amniotic fluid index (12.5 cm). However, a solid intra-abdominal mass, measuring 43 × 37 mm, was detected on the right side of the fetal abdomen, raising suspicion of FIF (Figure 1). Routine laboratory tests were within normal limits, with hemoglobin at 11.4 g/dL, hematocrit at 33.9%, creatinine at 0.61 mg/dL, and thyroid-stimulating hormone at 2.6 μIU/mL.
Fetus-in-fetu (FIF) is a rare congenital anomaly characterized by the presence of a malformed, parasitic twin enclosed within its normally developing counterpart. It results from abnormal embryogenesis during early twinning, typically in monochorionic diamniotic pregnancies. FIF is an exceptionally uncommon condition, with an estimated incidence of approximately 1 in 500,000 live births and fewer than 200 reported cases worldwide (1, 2).
Clinically, FIF most often presents as an abdominal mass detected in infancy, usually located in the retroperitoneal space, although other sites have been described. Early and accurate diagnosis is essential, as FIF must be differentiated from teratomas, which have different management strategies and malignant potential. Recognizing the distinguishing features of FIF facilitates appropriate treatment and improves patient outcomes.
2. Case Presentation
A 21-yr-old pregnant woman, in her second pregnancy, presented at 35 + 1/7 wk of gestation. This rare case was observed in Bentolhoda hospital, Bojnord, Iran. She had previously delivered a healthy full-term baby girl via vaginal delivery 2 yr earlier. We confirm that the pregnancy occurred spontaneously without assisted reproductive technologies. The pregnancy had been uneventful until the third trimester, at which point the case was referred for a routine ultrasound. During this examination, a fetal abdominal mass was incidentally detected. The relatively late diagnosis at 33 wk was primarily due to delayed referral to specialist care and limited access to detailed prenatal imaging earlier in pregnancy. Magnetic resonance imaging (MRI) was not performed in this case; prenatal diagnosis and surgical planning relied on detailed ultrasound imaging.
The mother reported no significant medical history, and the father also had no history of significant illness. Both parents are first cousins with blood type A+. There is no known family history of genetic disorders or hereditary diseases. The case had been following a routine prenatal care regimen, including folic acid supplementation from the start of the pregnancy. Additionally, she had received a single dose of the COVID-19 vaccine. She did not receive specialized obstetric care such as high-risk pregnancy monitoring, genetic counseling, or frequent prenatal ultrasounds, and instead attended routine prenatal check-ups at a local health center. The case had previously undergone an uncomplicated vaginal delivery. No history of genetic testing or nuchal translucency screening was observed due to a late referral.
At 33rd wk of gestation, a routine ultrasound revealed a well-formed fetus with an estimated weight of 2200 gr and a normal amniotic fluid index (12.5 cm). However, a solid intra-abdominal mass, measuring 43 × 37 mm, was detected on the right side of the fetal abdomen, raising suspicion of FIF (Figure 1). Routine laboratory tests were within normal limits, with hemoglobin at 11.4 g/dL, hematocrit at 33.9%, creatinine at 0.61 mg/dL, and thyroid-stimulating hormone at 2.6 μIU/mL.
- The timeline of events is as follows:
- October 14, 2024: first specialist consultation and ultrasound performed
- 33rd wk: mass detected via ultrasound, suspected to be FIF
- 35th wk: referred for further evaluation and surgical planning
The diagnosis of FIF was suspected to be based on prenatal ultrasound findings, which revealed a well-defined intra-abdominal mass (Figure 1). The mass showed features suggestive of internal organ development, including the possibility of a vertebral column. Differentiating FIF from teratoma was critical due to the potential malignancy associated with teratomas. The diagnosis was further confirmed through postnatal imaging and surgical findings. Serum alpha-fetoprotein (AFP) testing was not performed due to unavailability during prenatal care. The presence of vertebral structures, the organized arrangement of tissues, and the encapsulated nature of the mass strongly supported the diagnosis of FIF rather than a teratoma. Following complete surgical excision, the prognosis was favorable, with low recurrence rates and no malignant potential.
Surgical excision was performed to remove the intra-abdominal mass. The infant underwent surgery shortly after birth, and the intra-abdominal mass was completely excised without complications. No changes were required in the intervention, as surgical excision was the definitive management approach.
Postoperative recovery was uneventful, and no complications were observed. Follow-up monitoring revealed no abnormalities. Postoperative follow-up lasted 6 months, during which no complications or recurrence were observed. Histopathological examination confirmed the presence of a well-organized structure with vertebral elements, consistent with FIF. The surgical intervention was well tolerated, and no complications or recurrences were observed during the follow-up period. No adverse or unanticipated events were reported.
The symptoms associated with FIF primarily arise from mass effects, which can lead to abdominal distension, difficulty feeding, vomiting, jaundice, urinary retention, and compression of the abdominal viscera by the mass. Diagnosis often involves imaging techniques such as ultrasound, CT scans, or MRI, which help differentiate FIF from teratomas-tumors that can also appear as abdominal masses but have malignant potential.
2.1. Ethical Considerations
Written informed consent for the publication of this case report and accompanying images were obtained from the case’s legal guardians. All identifying information has been anonymized to maintain case confidentiality.
3. Discussion
In this case, a well-formed intra-abdominal mass consistent with FIF was identified prenatally at 33 wk gestation via routine ultrasound. Postnatal surgical excision confirmed the diagnosis by revealing a vertebral column and organized tissue structures, which clearly differentiated it from teratoma. These hallmark features align with previous reports describing FIF’s characteristic axial skeleton and organ-like development (3-4). Unlike teratomas, which possess malignant potential, FIF is generally benign, and complete surgical removal offers a favorable prognosis. However, accurate diagnosis remains challenging, particularly in prenatal settings.
The clinical decision-making process requires careful differentiation between FIF and teratoma due to differences in management and prognosis. Prenatal imaging, mainly ultrasound, plays a vital role in detection, though limited access to advanced imaging modalities like MRI may complicate diagnosis (5). Radiologically, FIF is distinguished by organized axial development, whereas teratomas lack such structure and may demonstrate malignant features. Serum AFP levels, often elevated in teratomas, are typically normal or only mildly increased in FIF, although AFP testing was not performed in this case due to unavailability (6).
According to Willis’s criteria, the presence of an axial skeleton is key for diagnosing FIF (7). In our case, pathological examination confirmed the vertebral column, supporting the diagnosis. Nevertheless, some literature reports (approximately 9%) describe cases without identifiable axial skeletons, prompting alternative definitions emphasizing advanced organogenesis (8-11).
This case of FIF highlights the critical role of early and accurate prenatal imaging and a multidisciplinary approach in achieving a favorable outcome. However, our study was limited by the absence of MRI and AFP testing, along with a relatively short follow-up period of 6 months. Future cases would benefit from comprehensive diagnostic assessments, including advanced imaging and tumor markers, and extended follow-up to monitor for potential long-term complications or recurrence.
3.1. Strengths and Limitations
This report highlights key clinical lessons: the necessity for heightened clinical suspicion of FIF in cases of fetal abdominal masses, the pivotal role of detailed prenatal imaging, and the value of prompt surgical intervention. Despite its rarity, recognizing FIF ensures appropriate treatment and avoids misdiagnosis with malignant teratomas. Awareness of diagnostic challenges and limitations can guide clinicians toward better patient care.
4. Conclusion
FIF is a rare congenital condition that typically presents as an abdominal mass in early infancy. Prenatal detection is possible through imaging, and surgical removal is curative. It must be distinguished from teratomas due to their potential for malignancy. Prompt diagnosis and surgical intervention are essential to ensure a favorable outcome.
Data Availability
The data supporting the findings of this case report are available from the corresponding author upon reasonable request. All relevant data are included in the manuscript and figures. No additional datasets were generated or analyzed during the current study.
Author Contributions
V. Radi developed the study concept and design. N. Mohammadi and V. Radi wrote the first draft of the manuscript. All authors contributed to the intellectual content, manuscript editing, and read and approved the final manuscript.
Acknowledgments
The authors would like to thank all participants in the study. This research did not receive any grant from funding agencies from the public, commercial, or non-profit sectors. The authors declare that no artificial intelligence tools were used in any part of this work, including translation, revision, or grammar checking.
Conflict of Interest
The authors declare that there is no conflict of interest.
Surgical excision was performed to remove the intra-abdominal mass. The infant underwent surgery shortly after birth, and the intra-abdominal mass was completely excised without complications. No changes were required in the intervention, as surgical excision was the definitive management approach.
Postoperative recovery was uneventful, and no complications were observed. Follow-up monitoring revealed no abnormalities. Postoperative follow-up lasted 6 months, during which no complications or recurrence were observed. Histopathological examination confirmed the presence of a well-organized structure with vertebral elements, consistent with FIF. The surgical intervention was well tolerated, and no complications or recurrences were observed during the follow-up period. No adverse or unanticipated events were reported.
The symptoms associated with FIF primarily arise from mass effects, which can lead to abdominal distension, difficulty feeding, vomiting, jaundice, urinary retention, and compression of the abdominal viscera by the mass. Diagnosis often involves imaging techniques such as ultrasound, CT scans, or MRI, which help differentiate FIF from teratomas-tumors that can also appear as abdominal masses but have malignant potential.
2.1. Ethical Considerations
Written informed consent for the publication of this case report and accompanying images were obtained from the case’s legal guardians. All identifying information has been anonymized to maintain case confidentiality.
3. Discussion
In this case, a well-formed intra-abdominal mass consistent with FIF was identified prenatally at 33 wk gestation via routine ultrasound. Postnatal surgical excision confirmed the diagnosis by revealing a vertebral column and organized tissue structures, which clearly differentiated it from teratoma. These hallmark features align with previous reports describing FIF’s characteristic axial skeleton and organ-like development (3-4). Unlike teratomas, which possess malignant potential, FIF is generally benign, and complete surgical removal offers a favorable prognosis. However, accurate diagnosis remains challenging, particularly in prenatal settings.
The clinical decision-making process requires careful differentiation between FIF and teratoma due to differences in management and prognosis. Prenatal imaging, mainly ultrasound, plays a vital role in detection, though limited access to advanced imaging modalities like MRI may complicate diagnosis (5). Radiologically, FIF is distinguished by organized axial development, whereas teratomas lack such structure and may demonstrate malignant features. Serum AFP levels, often elevated in teratomas, are typically normal or only mildly increased in FIF, although AFP testing was not performed in this case due to unavailability (6).
According to Willis’s criteria, the presence of an axial skeleton is key for diagnosing FIF (7). In our case, pathological examination confirmed the vertebral column, supporting the diagnosis. Nevertheless, some literature reports (approximately 9%) describe cases without identifiable axial skeletons, prompting alternative definitions emphasizing advanced organogenesis (8-11).
This case of FIF highlights the critical role of early and accurate prenatal imaging and a multidisciplinary approach in achieving a favorable outcome. However, our study was limited by the absence of MRI and AFP testing, along with a relatively short follow-up period of 6 months. Future cases would benefit from comprehensive diagnostic assessments, including advanced imaging and tumor markers, and extended follow-up to monitor for potential long-term complications or recurrence.
3.1. Strengths and Limitations
This report highlights key clinical lessons: the necessity for heightened clinical suspicion of FIF in cases of fetal abdominal masses, the pivotal role of detailed prenatal imaging, and the value of prompt surgical intervention. Despite its rarity, recognizing FIF ensures appropriate treatment and avoids misdiagnosis with malignant teratomas. Awareness of diagnostic challenges and limitations can guide clinicians toward better patient care.
4. Conclusion
FIF is a rare congenital condition that typically presents as an abdominal mass in early infancy. Prenatal detection is possible through imaging, and surgical removal is curative. It must be distinguished from teratomas due to their potential for malignancy. Prompt diagnosis and surgical intervention are essential to ensure a favorable outcome.
Data Availability
The data supporting the findings of this case report are available from the corresponding author upon reasonable request. All relevant data are included in the manuscript and figures. No additional datasets were generated or analyzed during the current study.
Author Contributions
V. Radi developed the study concept and design. N. Mohammadi and V. Radi wrote the first draft of the manuscript. All authors contributed to the intellectual content, manuscript editing, and read and approved the final manuscript.
Acknowledgments
The authors would like to thank all participants in the study. This research did not receive any grant from funding agencies from the public, commercial, or non-profit sectors. The authors declare that no artificial intelligence tools were used in any part of this work, including translation, revision, or grammar checking.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Case Report |
Subject:
Embryology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |