Sat, Feb 21, 2026
[Archive]
Volume 23, Issue 11 (November 2025)
IJRM 2025, 23(11): 953-960 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hasani S, Gholizadeh R, Rajabi Khamesi S, Ebrahim Kalantari M, Salimi M. Fimbria torsion as a rare cause of lower abdominal pain: A case report and literature review. IJRM 2025; 23 (11) :953-960
URL: http://ijrm.ir/article-1-3706-en.html
URL: http://ijrm.ir/article-1-3706-en.html
Solmaz Hasani1 

 , Roya Gholizadeh2
, Roya Gholizadeh2 

 , Sima Rajabi Khamesi2
, Sima Rajabi Khamesi2 

 , Mohammad Ebrahim Kalantari3
, Mohammad Ebrahim Kalantari3 

 , Mostafa Salimi *4
, Mostafa Salimi *4 




 , Roya Gholizadeh2
, Roya Gholizadeh2 

 , Sima Rajabi Khamesi2
, Sima Rajabi Khamesi2 

 , Mohammad Ebrahim Kalantari3
, Mohammad Ebrahim Kalantari3 

 , Mostafa Salimi *4
, Mostafa Salimi *4 


1- Endocrine Research Center, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran.
2- Student Research Committee, Faculty of Medicine, Mashhad Medical Sciences, Islamic Azad University, Mashhad, Iran.
3- Surgical Oncology Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Student Research Committee, Faculty of Medicine, Mashhad Medical Sciences, Islamic Azad University, Mashhad, Iran. ,salimi.mostafa@iaumshms.ac.ir
2- Student Research Committee, Faculty of Medicine, Mashhad Medical Sciences, Islamic Azad University, Mashhad, Iran.
3- Surgical Oncology Research Center, Mashhad University of Medical Sciences, Mashhad, Iran.
4- Student Research Committee, Faculty of Medicine, Mashhad Medical Sciences, Islamic Azad University, Mashhad, Iran. ,
Full-Text [PDF 1555 kb]
(242 Downloads)
| Abstract (HTML) (194 Views)
Full-Text: (12 Views)
1. Introduction
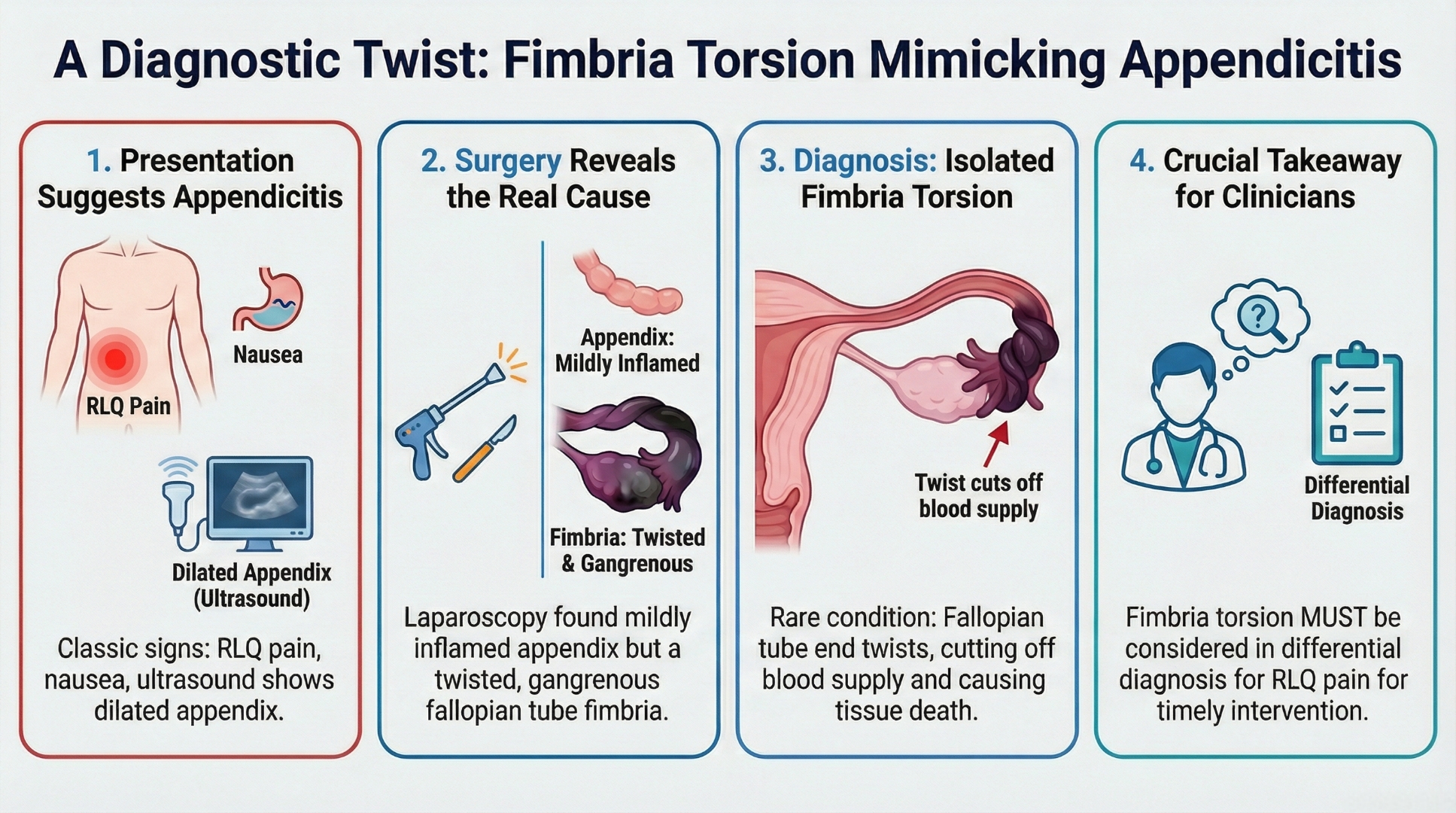
Acute pelvic pain is a common presentation in the emergency department and poses a significant diagnostic challenge, as it encompasses a wide spectrum of gynecological and non-gynecological etiologies. Among these, adnexal torsion, the twisting of the ovary and/or fallopian tube on its vascular pedicle, is the 5th most common gynecological emergency, accounting for approximately 2.7% of such cases (1, 2). However, a less common and often overlooked variant is the torsion of the fimbrial end of the fallopian tube. This condition, known as fimbrial torsion, is a rare but significant gynecological emergency. It occurs when the fimbriae, those delicate, finger-like projections at the terminal ends of the fallopian tubes, become twisted (3). If untreated, this condition obstructs venous outflow and subsequently arterial inflow, leading to edema, ischemia, and necrosis (4). Although it is an infrequent occurrence, fimbria torsion should be an important consideration when evaluating acute pelvic pain, particularly in women of reproductive age (5).
The etiology of fimbrial torsion remains unclear, though it is often associated with intrinsic tubal abnormalities such as paratubal cysts or adhesions (6). The clinical presentation is notoriously nonspecific, typically involving the sudden onset of lower abdominal or pelvic pain, often associated with nausea and vomiting (1, 7, 8). This symptomatic overlap creates a diagnostic challenge, as right lower quadrant (RLQ) pain necessitates a differential diagnosis that includes appendicitis, ovarian cysts, ectopic pregnancy, and other adnexal pathologies (9, 10).
Because acute appendicitis is the most common cause of RLQ pain requiring surgery, it is often the leading presumptive diagnosis (11). This clinical mimicry can delay the diagnosis of fimbrial torsion, thereby jeopardizing tubal viability. Therefore, maintaining a high index of clinical suspicion is crucial for timely surgical intervention.
This article presents a case involving a woman admitted to the emergency department with RLQ abdominal pain, who was subsequently diagnosed with fimbrial torsion intraoperatively. This report will detail her clinical presentation, diagnostic workup, and surgical management. Furthermore, provide a brief review of the literature to underscore the key features that can aid in the preoperative identification of this rare condition.
2. Case Presentation
The etiology of fimbrial torsion remains unclear, though it is often associated with intrinsic tubal abnormalities such as paratubal cysts or adhesions (6). The clinical presentation is notoriously nonspecific, typically involving the sudden onset of lower abdominal or pelvic pain, often associated with nausea and vomiting (1, 7, 8). This symptomatic overlap creates a diagnostic challenge, as right lower quadrant (RLQ) pain necessitates a differential diagnosis that includes appendicitis, ovarian cysts, ectopic pregnancy, and other adnexal pathologies (9, 10).
Because acute appendicitis is the most common cause of RLQ pain requiring surgery, it is often the leading presumptive diagnosis (11). This clinical mimicry can delay the diagnosis of fimbrial torsion, thereby jeopardizing tubal viability. Therefore, maintaining a high index of clinical suspicion is crucial for timely surgical intervention.
This article presents a case involving a woman admitted to the emergency department with RLQ abdominal pain, who was subsequently diagnosed with fimbrial torsion intraoperatively. This report will detail her clinical presentation, diagnostic workup, and surgical management. Furthermore, provide a brief review of the literature to underscore the key features that can aid in the preoperative identification of this rare condition.
2. Case Presentation
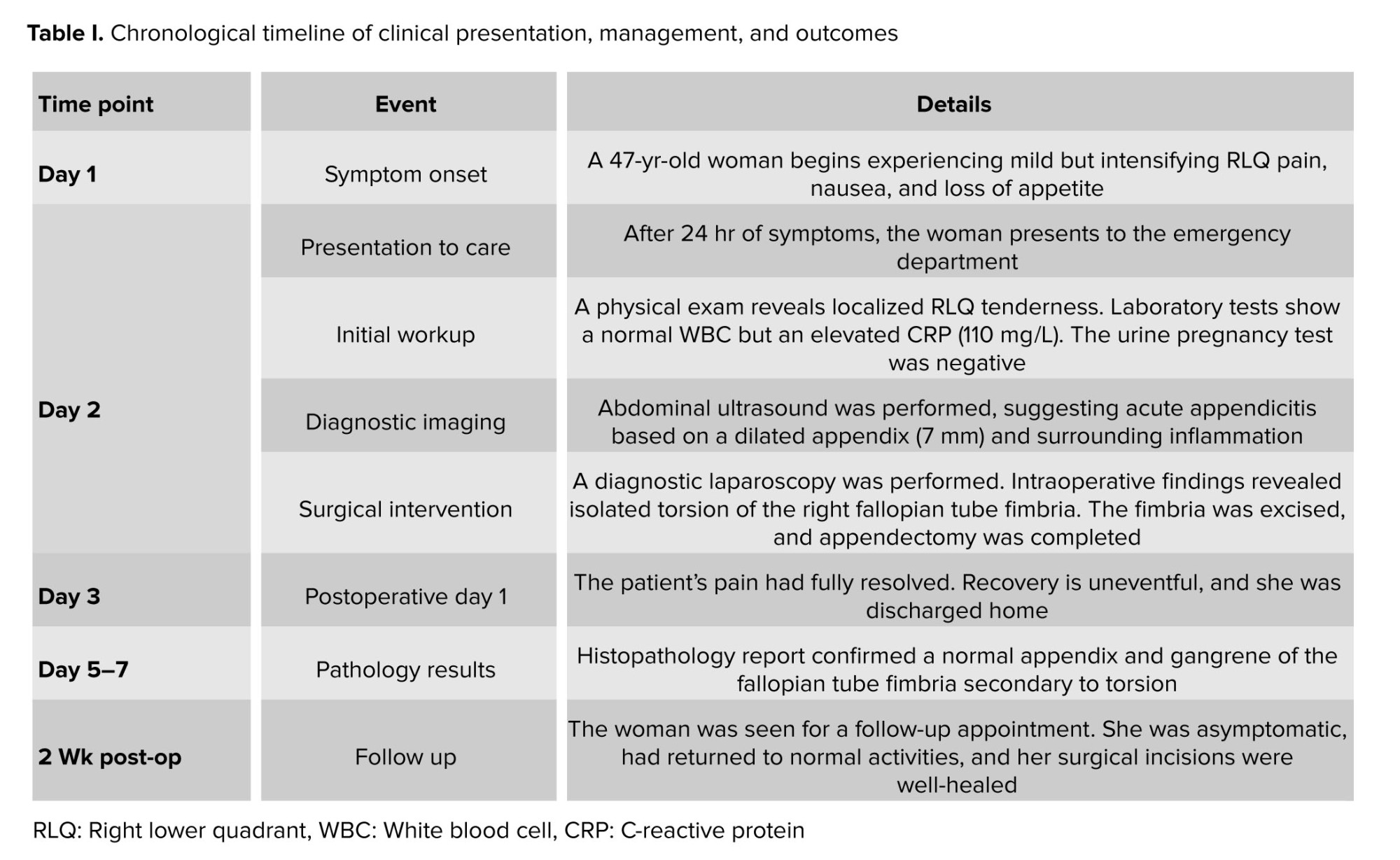
A 47-yr-old, gravida 2, para 2 woman presented to the emergency department with a 24-hr history of progressively intensifying RLQ abdominal pain, accompanied by nausea and anorexia. She had no significant past medical, surgical, or family history, specifically denying any prior abdominal surgeries or known gynecological conditions. Her menstrual cycle was regular, with her last period occurring 2 wk prior.
2.1. Clinical findings and diagnostic assessment
2.1. Clinical findings and diagnostic assessment
Upon physical examination, she was afebrile with stable vital signs. Abdominal examination revealed localized tenderness and guarding in the RLQ. Laboratory tests revealed an elevated C-reactive protein (CRP) level of 110 mg/L (reference range < 5 mg/L) but a normal white blood cell count. The urine pregnancy test was negative. An abdominal ultrasound was performed, revealing a non-compressible, dilated appendix measuring 7 mm in diameter with surrounding inflamed fatty tissue. A presumptive diagnosis of acute appendicitis was made, with ovarian torsion and pelvic inflammatory disease considered as differential diagnoses.
2.2. Therapeutic intervention and surgical findings
2.2. Therapeutic intervention and surgical findings
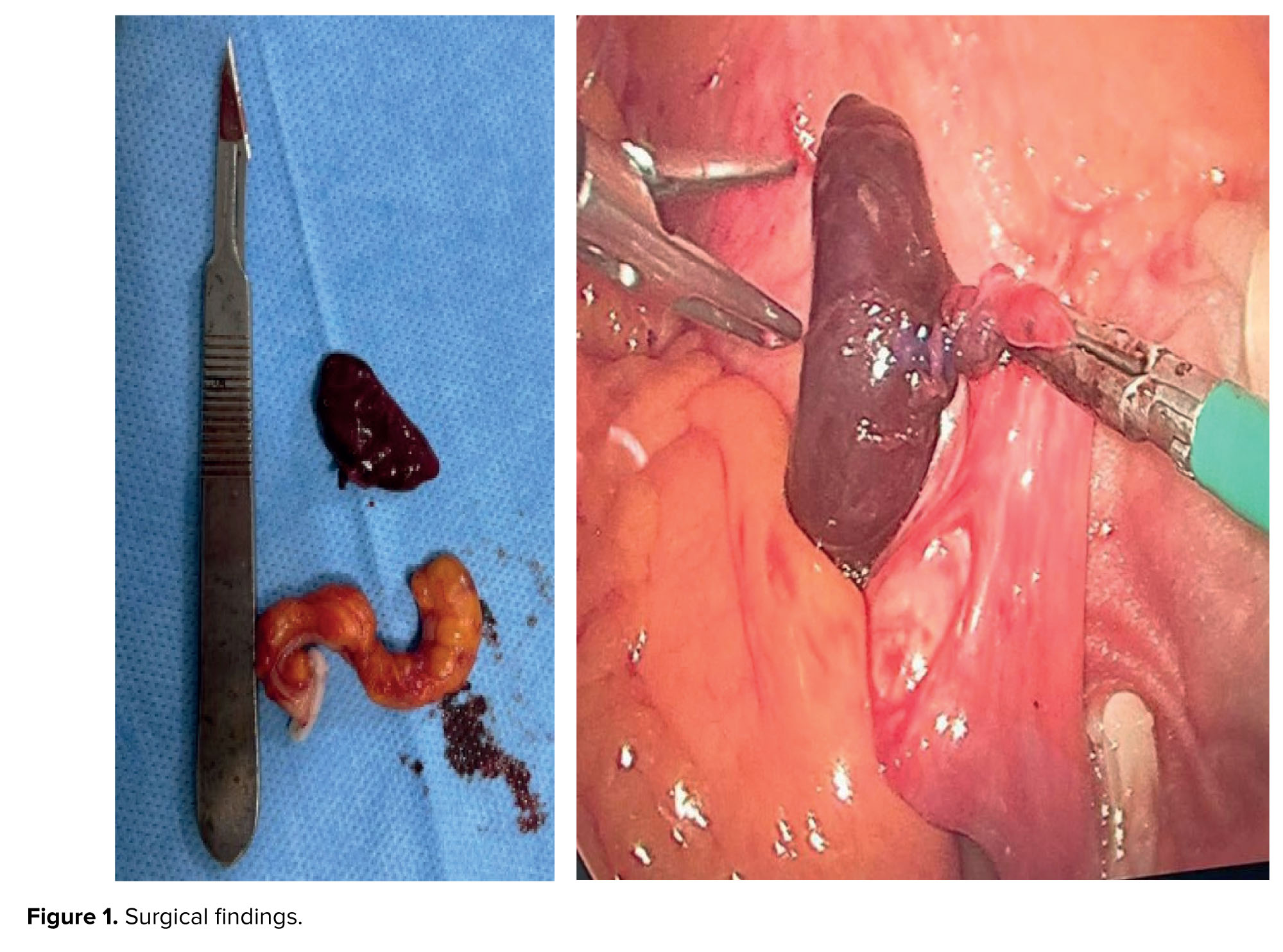
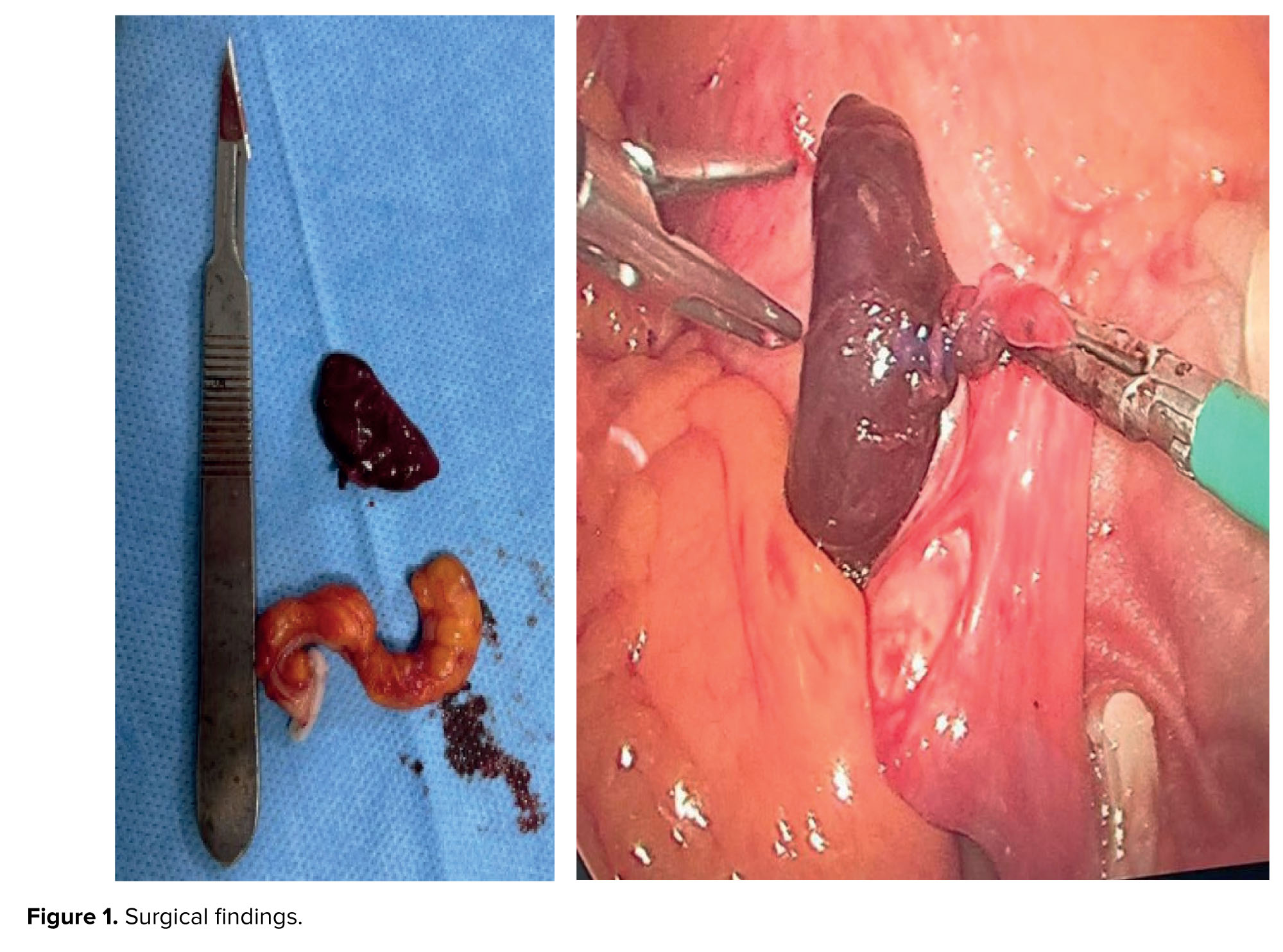
Given the strong clinical suspicion for acute appendicitis, she underwent a diagnostic laparoscopy. Intraoperatively, the appendix appeared only mildly inflamed. However, a systematic evaluation of the pelvic organs revealed isolated torsion of the right fimbria, which was edematous, hemorrhagic, and gangrenous (Figure 1).
No torsion of the ovary or the remainder of the fallopian tube was observed. The necrotic fimbrial end was excised, and a laparoscopic appendectomy was performed.
2.3. Follow-up and outcomes
No torsion of the ovary or the remainder of the fallopian tube was observed. The necrotic fimbrial end was excised, and a laparoscopic appendectomy was performed.
2.3. Follow-up and outcomes
The patient’s postoperative recovery was uneventful. Her pain resolved completely within 24 hr, and she was discharged on the first postoperative day. At a 2-wk follow-up appointment, she was asymptomatic and had returned to her normal activities with her incisions well-healed.
2.4. Pathology report
2.4. Pathology report
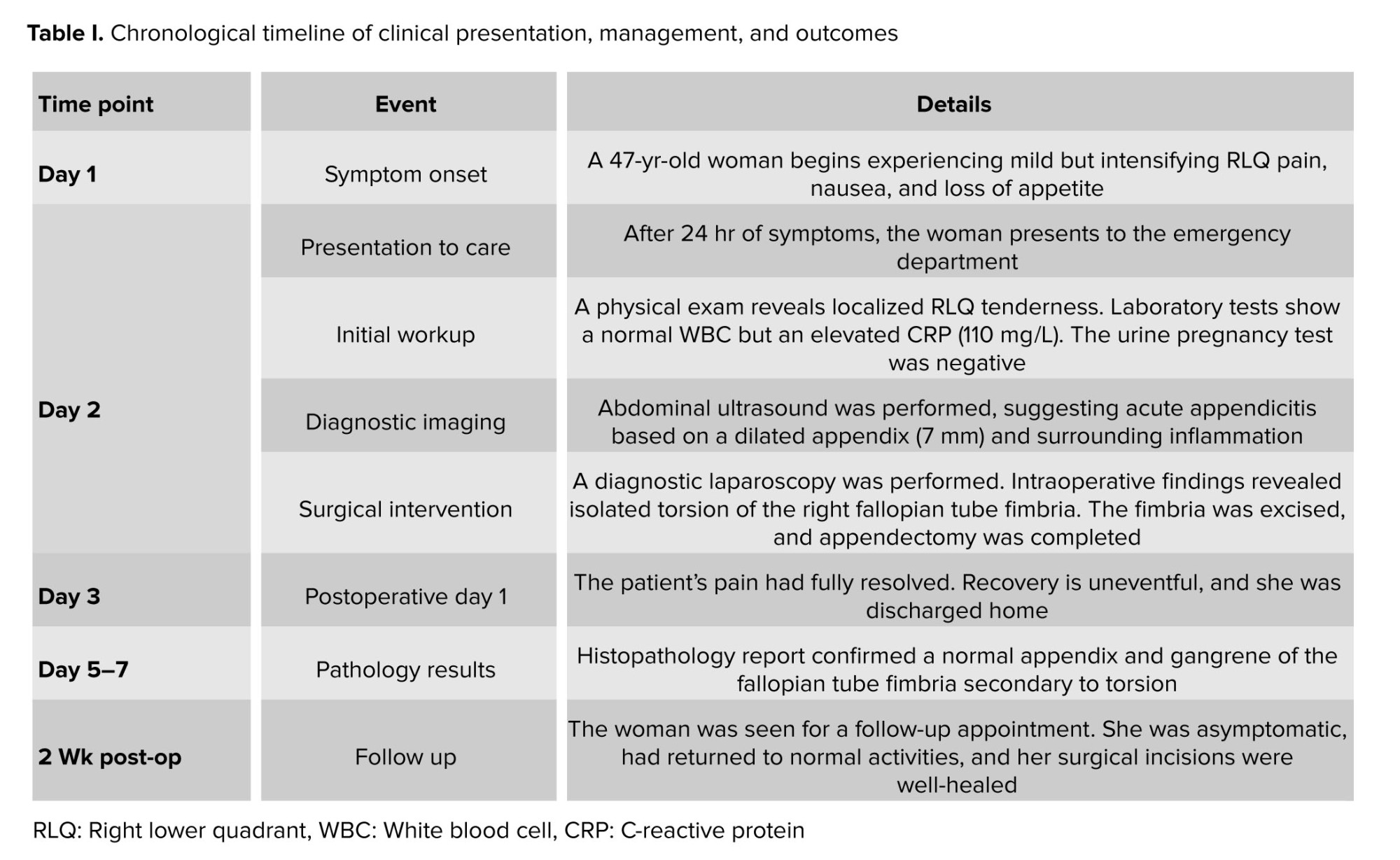
Histopathological examination revealed no acute inflammation in the appendix. In contrast, the fallopian tube specimen showed extensive hemorrhage, edema, and necrosis, confirming gangrene secondary to torsion. The chronological progression is outlined in table I.
2.5. Ethical Considerations
2.5. Ethical Considerations
Informed written consent was obtained from the case for future publication of this case report.
3. Discussion
3. Discussion
This case demonstrates a significant diagnostic challenge, as a 47-yr-old woman whose clinical presentation and imaging were highly suggestive of acute appendicitis, which was ultimately diagnosed intraoperatively with isolated fimbrial torsion. This outcome highlights that fimbrial torsion, while rare, is a critical differential diagnosis in women with acute abdominal pain because it can precisely mimic more common conditions. The localized RLQ pain and elevated inflammatory markers justifiably led to an initial diagnosis of appendicitis, illustrating the deceptive clinical overlap between these conditions. As noted in the literature, the true incidence of isolated fallopian tube torsion is likely under-reported due to its rarity and nonspecific presentation (12). In our case, the ultrasound findings of inflammatory changes in the RLQ contributed to the initial misdiagnosis. While imaging is invaluable in emergency settings, this demonstrates its limitations in definitively identifying rare adnexal pathologies, especially when they mimic appendicitis. Furthermore, our finding that the torsion occurred on the right side was consistent with previous reports, which suggest a higher prevalence of right-sided torsion (13).
Timely surgical intervention is critical in preventing long-term consequences such as infertility and chronic pelvic pain (14). The laparoscopic identification and management in this case underscore the importance of a comprehensive intraoperative survey, particularly when the suspected pathology does not appear severe enough to explain the woman’s clinical presentation. Her uneventful postoperative recovery aligns with literature indicating that prompt surgical management leads to favorable outcomes and reduces complications (15).
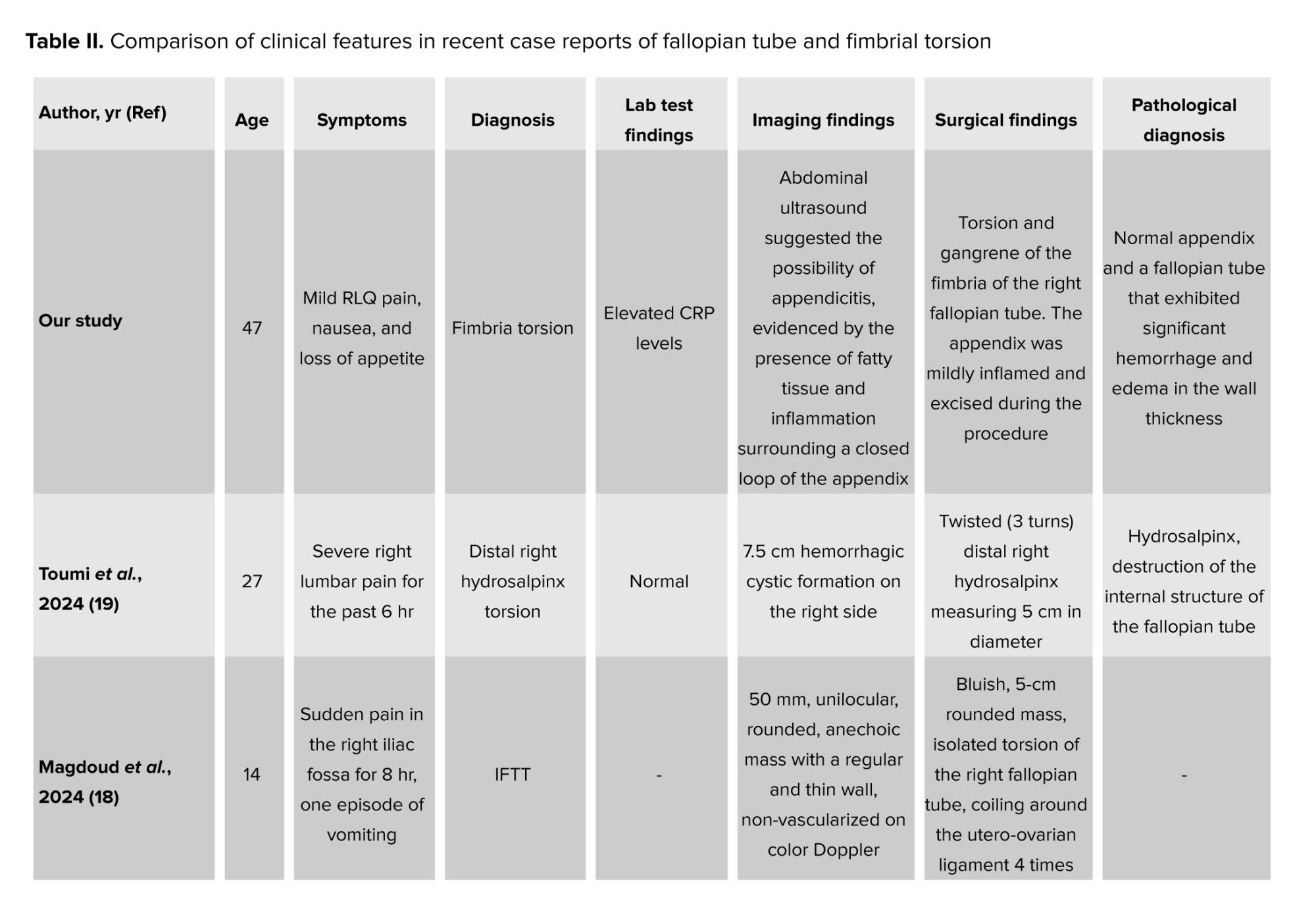
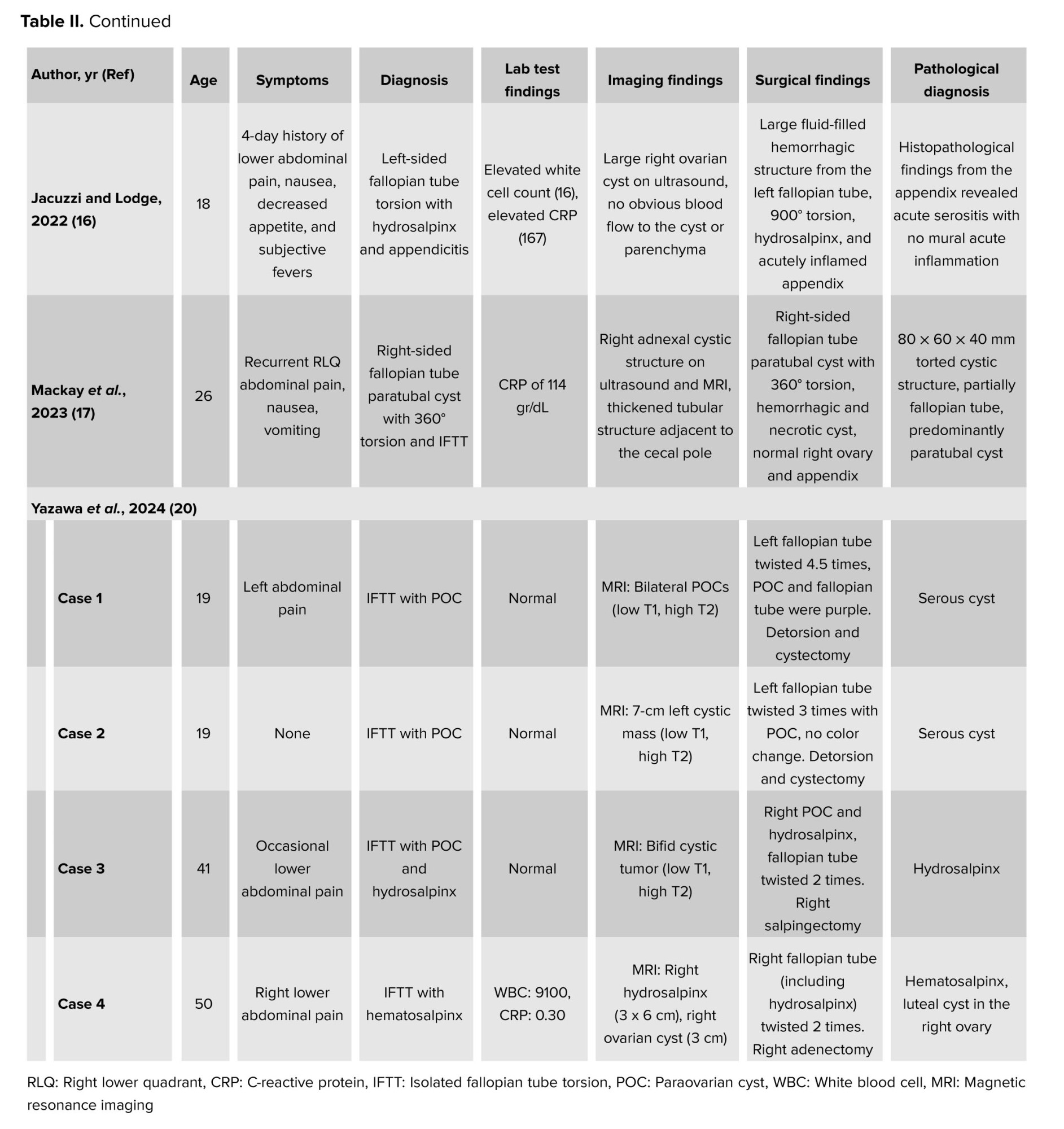
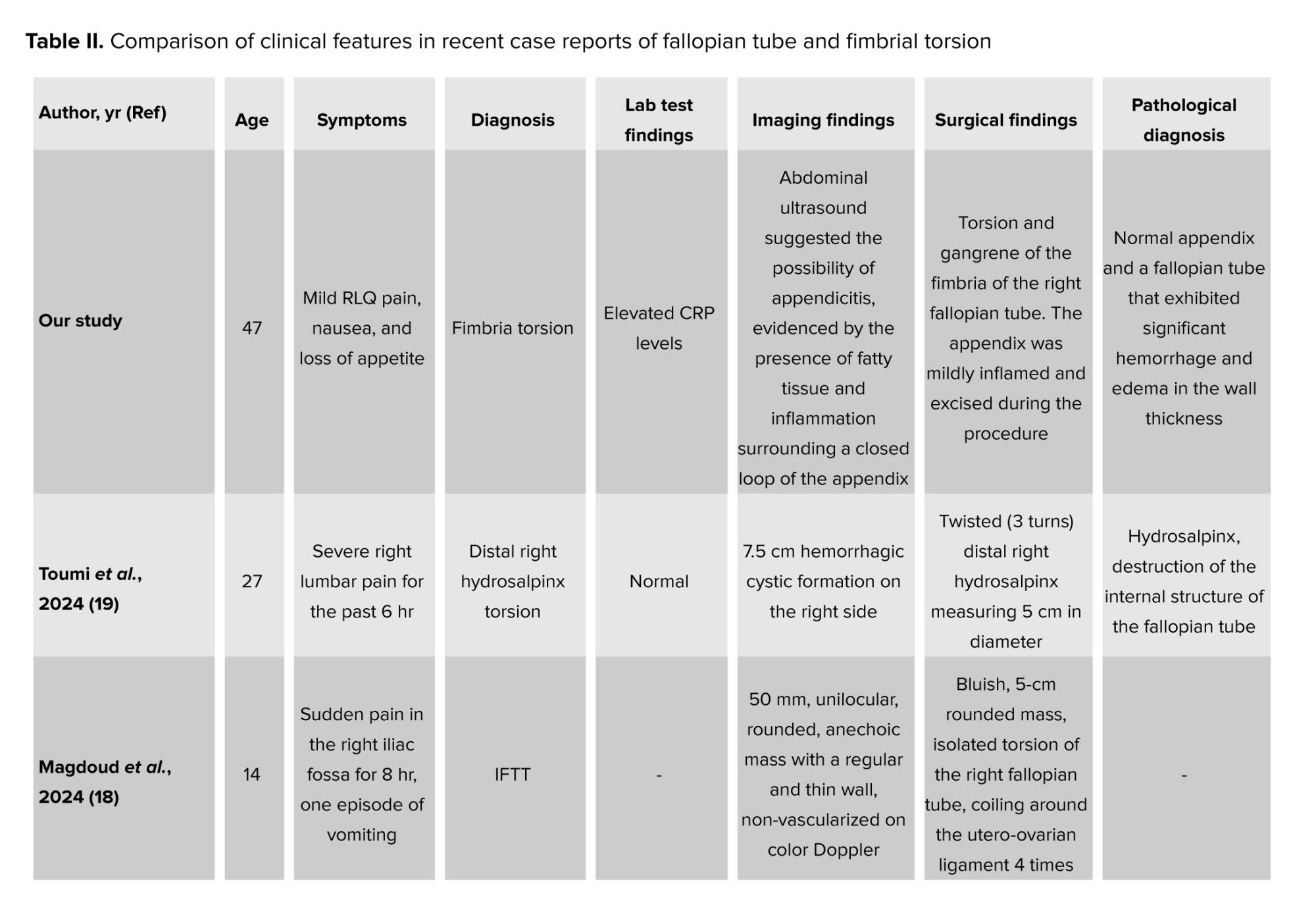
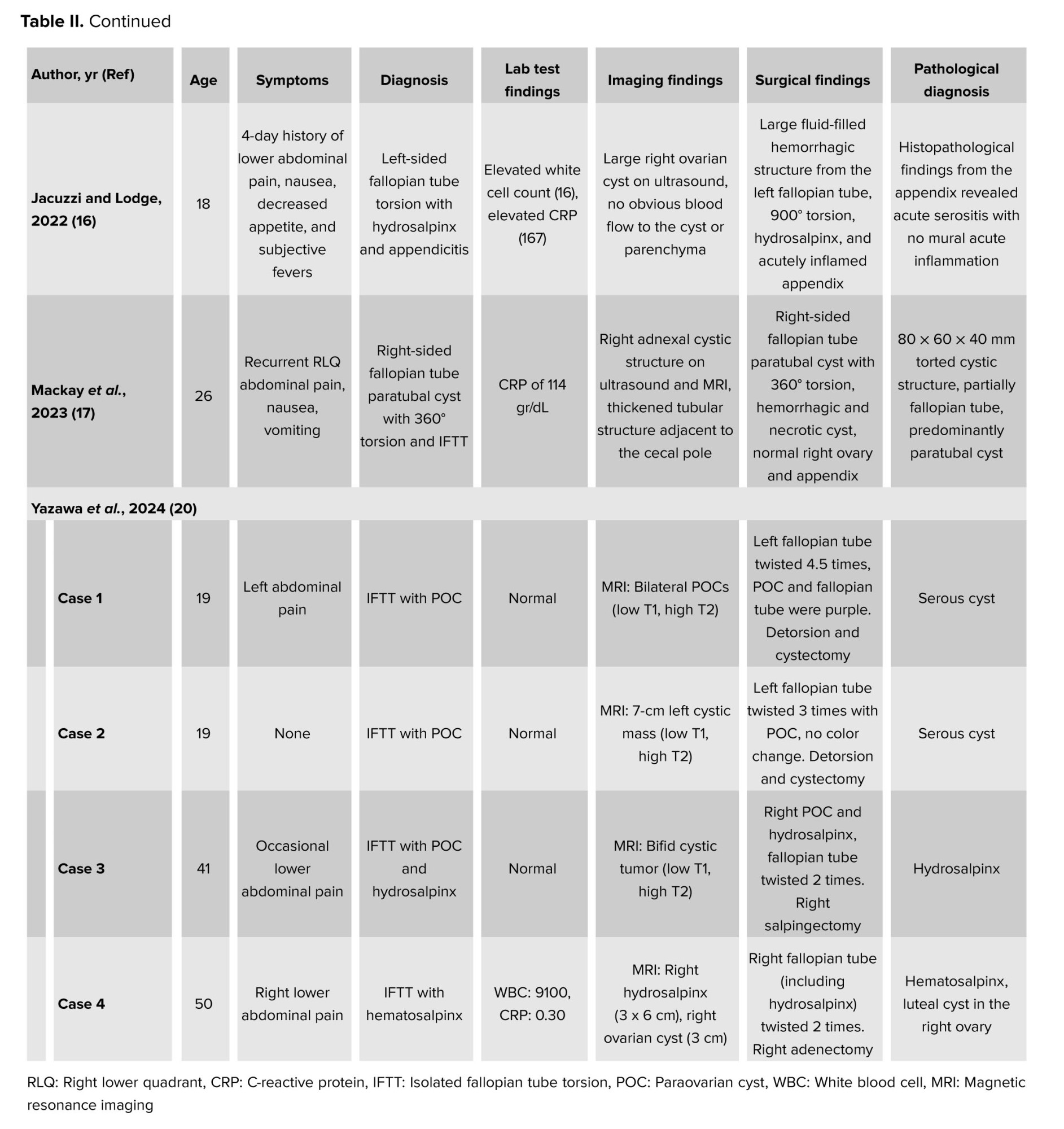
Our literature review emphasizes the articles on this condition in medical literature and underscores the importance of sharing clinical experiences to expand the knowledge base (Table II).
Comparison with recent literature reveals both similarities and distinctions. Our case patient (47 yr old) is older than the typical demographic for torsion; however, this finding aligns with other cases reported in perimenopausal women. The clinical presentation, characterized by RLQ pain that mimics acute appendicitis, was consistent with findings from another report, thus emphasizing this common diagnostic challenge. A notable differentiating factor in many reviewed cases was the presence of associated adnexal pathology, such as a paratubal cyst or hydrosalpinx, which was believed to act as a precipitating factor for torsion. This case was significant because it describes isolated fimbrial torsion in the absence of predisposing anatomical factors, such as a paratubal cyst. This comparison highlights that, while clinical demographics and underlying pathologies may differ, the risk of fimbrial and tubal torsion presenting as a more common acute surgical abdomen remains a critical diagnostic pitfall (16-20).
4. Conclusion
This case exemplifies the need for a heightened index of suspicion for fimbrial torsion in women presenting with RLQ pain. While appendicitis remains the most common cause of such presentations, the potential occurrence of less common conditions like fimbria torsion must be considered. Improved understanding and recognition of fimbria torsion could lead to more timely diagnoses, appropriate interventions, and ultimately better patient outcomes. Further reporting is warranted to better elucidate the clinical presentations, risk factors, and optimal management strategies for this rare gynecological emergency.
Author Contributions
S. Hasani: Provided critical feedback, interpretation of clinical data, and critical revision of the manuscript. R. Gholizadeh: Acquisition of data and drafted the manuscript. S. Rajabi Khamesi: Performed the literature review and drafted the manuscript. M.E. Kalantari: Surgical management of the case and provided technical insights for the manuscript. M. Salimi: Supervised the study, drafted and finalized the manuscript for submission, and was responsible for the integrity of the work. All authors have read and approved the final manuscript.
Acknowledgments
This study was not financially supported. The authors would like to express their gratitude to the journal editors and reviewers for their insightful comments and constructive feedback, which significantly improved the case report. The Grammarly online tool was used to improve the grammar and accuracy of the text.
Conflict of Interest
The authors declare that there is no conflict of interest.
Timely surgical intervention is critical in preventing long-term consequences such as infertility and chronic pelvic pain (14). The laparoscopic identification and management in this case underscore the importance of a comprehensive intraoperative survey, particularly when the suspected pathology does not appear severe enough to explain the woman’s clinical presentation. Her uneventful postoperative recovery aligns with literature indicating that prompt surgical management leads to favorable outcomes and reduces complications (15).
Our literature review emphasizes the articles on this condition in medical literature and underscores the importance of sharing clinical experiences to expand the knowledge base (Table II).
Comparison with recent literature reveals both similarities and distinctions. Our case patient (47 yr old) is older than the typical demographic for torsion; however, this finding aligns with other cases reported in perimenopausal women. The clinical presentation, characterized by RLQ pain that mimics acute appendicitis, was consistent with findings from another report, thus emphasizing this common diagnostic challenge. A notable differentiating factor in many reviewed cases was the presence of associated adnexal pathology, such as a paratubal cyst or hydrosalpinx, which was believed to act as a precipitating factor for torsion. This case was significant because it describes isolated fimbrial torsion in the absence of predisposing anatomical factors, such as a paratubal cyst. This comparison highlights that, while clinical demographics and underlying pathologies may differ, the risk of fimbrial and tubal torsion presenting as a more common acute surgical abdomen remains a critical diagnostic pitfall (16-20).
4. Conclusion
This case exemplifies the need for a heightened index of suspicion for fimbrial torsion in women presenting with RLQ pain. While appendicitis remains the most common cause of such presentations, the potential occurrence of less common conditions like fimbria torsion must be considered. Improved understanding and recognition of fimbria torsion could lead to more timely diagnoses, appropriate interventions, and ultimately better patient outcomes. Further reporting is warranted to better elucidate the clinical presentations, risk factors, and optimal management strategies for this rare gynecological emergency.
Author Contributions
S. Hasani: Provided critical feedback, interpretation of clinical data, and critical revision of the manuscript. R. Gholizadeh: Acquisition of data and drafted the manuscript. S. Rajabi Khamesi: Performed the literature review and drafted the manuscript. M.E. Kalantari: Surgical management of the case and provided technical insights for the manuscript. M. Salimi: Supervised the study, drafted and finalized the manuscript for submission, and was responsible for the integrity of the work. All authors have read and approved the final manuscript.
Acknowledgments
This study was not financially supported. The authors would like to express their gratitude to the journal editors and reviewers for their insightful comments and constructive feedback, which significantly improved the case report. The Grammarly online tool was used to improve the grammar and accuracy of the text.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Case Report |
Subject:
Reproductive Surgery
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |