Thu, Apr 25, 2024
[Archive]
Volume 4, Issue 1 (7-2006)
IJRM 2006, 4(1): 23-28 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khademi A, Alleyassin A, Agha-hosseini M, Dadras N, Asghari Roodsari A, Tabatabaeefar L et al . Psychometric properties of Sexual Function Questionnaire: evaluation of an Iranian sample. IJRM 2006; 4 (1) :23-28
URL: http://ijrm.ir/article-1-48-en.html
URL: http://ijrm.ir/article-1-48-en.html
Afsaneh Khademi * 
 1, Ashraf Alleyassin2
1, Ashraf Alleyassin2 
 , Marzieh Agha-hosseini2
, Marzieh Agha-hosseini2 
 , Nasrin Dadras2
, Nasrin Dadras2 
 , Allaleh Asghari Roodsari3
, Allaleh Asghari Roodsari3 
 , Leila Tabatabaeefar3
, Leila Tabatabaeefar3 
 , Mehrnoosh Amini2
, Mehrnoosh Amini2 


 1, Ashraf Alleyassin2
1, Ashraf Alleyassin2 
 , Marzieh Agha-hosseini2
, Marzieh Agha-hosseini2 
 , Nasrin Dadras2
, Nasrin Dadras2 
 , Allaleh Asghari Roodsari3
, Allaleh Asghari Roodsari3 
 , Leila Tabatabaeefar3
, Leila Tabatabaeefar3 
 , Mehrnoosh Amini2
, Mehrnoosh Amini2 

1- Infertility Ward, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran , afkhademi@sina.tums.ac.ir
2- Infertility Ward, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran
3- Faculty of Medicine, Tehran University of Medical Sciences, Tehran, Iran
2- Infertility Ward, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran
3- Faculty of Medicine, Tehran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 115 kb]
(797 Downloads)
| Abstract (HTML) (2717 Views)
Introduction
Female sexual dysfunction (FSD) is a real problem that affects a significant number of populations. Increased awareness of this problem in the medical community will lead to further research in female sexual dysfunction, and improved treatment (1). FSD is highly prevalent, occurring in 25–63% of women (2). A meta-analysis estimated prevalence of orgasmic disorders to be 7–10% (3).
Although the best method of screening and diagnosis of FSD is structured interview by several designed questionnaires. Some of these tests are designed to address one specific aspect of FSD such as ease in arousal or level of sexual desire (4-5). The Sexual Activity Questionnaire was designed to assess the impact of cancer treatments on sexual function (6). The Sexual Interaction Survey and the Sexual Interaction System Scale have a dyadic focus (7-8). More multidimensional measures include the Derogatis Sexual Function Inventory (DSFI), a collection survey of sexual attitude, experience, and satisfaction, and the Brief Index of Sexual Functioning for Women (9-10).
The more recently developed Female Sexual Function Index has already been used in several clinical trials (11). Now there are newer questionnaires in relation to sexual dysfunction. The Sexual Quality of Life-Female (SQOL-F) questionnaire has been developed to assess the impact of female sexual dysfunction (FSD) on a woman's sexual quality of life. SQOL-F items were developed through interviews with 82 women. The SQOL-F showed good psychometric properties: convergent validity, discriminate validity, and test-retest reliability. However, the SQOL-F sensitivity should be confirmed (12). Sexual Function Questionnaire (SFQ) is a self- reported outcomes measure of female sexual function (13). The SFQ addresses all aspects of the sexual response cycle and pain, incorporating the more recently developed classifications (14).
In our knowledge, there is no valid Persian version of sexual inventory. The aim of this study was to translate SFQ in Persian (Iranian language) and test the reliability and validity of Persian version of SFQ.
Materials and Methods
From March to October 2005, in total 547 women participated in a cross-sectional study. The participants included 73 pregnant subjects, 167 infertile patients, 258 normal subjects (university students or subjects visited the contraception clinic) and 49 patients visited for gynecological problems. The study was approved by the Ethical Committee of Tehran Medical Sciences University. Institutional Review Board approval was obtained before commencing the trial as well. All patients and their husbands gave their written permission.
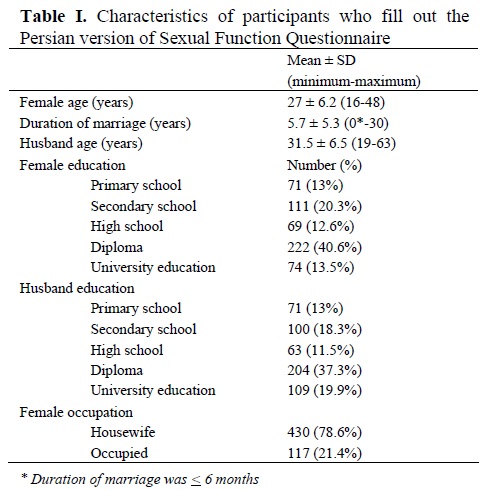
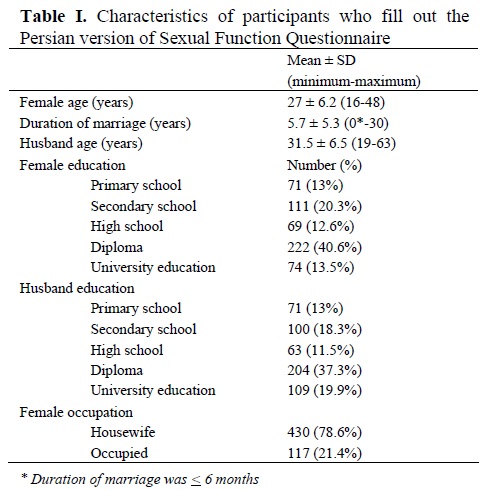
The main characteristics of the studied population are described in Table I. A questionnaire asked about female and her partner age, duration of marriage, level of education of female and her partner, and female occupation. All patients were initially evaluated for satisfaction of sexual function by asking a single question: ‘How much is your satisfaction rate from your sexual function?’ The answer estimated by a self-rating scale, which was shown in the demographic questionnaire.
Self-rating scale was scored 0 to 10 in a positive regression. Due to rules of ethics, patients with score <5 were offered sexologist visit for confirmation of diagnosis and treatment if needed. We put the open question about FSD on demographic questionnaire to compare the scores obtained by the main questionnaire of sexual dysfunction in patients complained from FSD with normal subjects.
Questionnaire
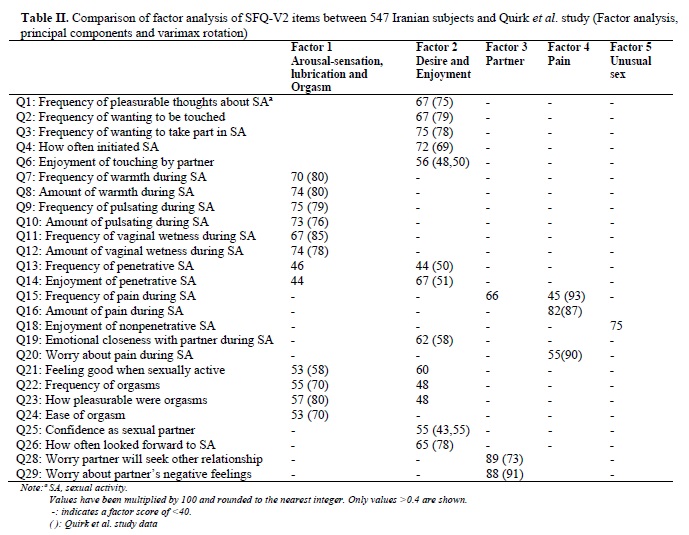
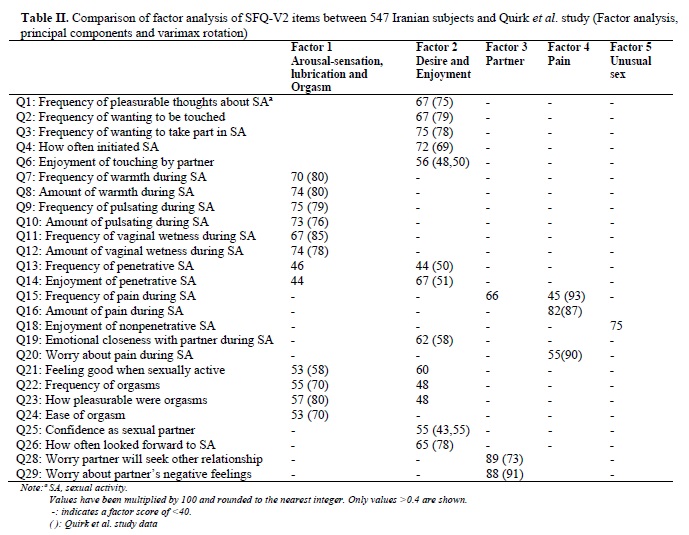
A questionnaire named Sexual Function Questionnaire-version 2 (SFQ-V2) with 7 domains and 26 items was used. The 7 domains of SFQ are consisting of 26 items. These 7 domains included: desire (Q1–4, 13, 26; score range 5–31), arousal-sensation (Q7–10; score range 4–20), arousal-lubrication (Q11–12; score range 2–10), orgasm (Q22–24; score range 3–15), enjoyment (Q6, 14, 18, 19, 21, 25; score range 6–30), pain (Q15, 16, 20; score range 2–15), and partner relationship (Q28, 29; score range 2–10). (Table II) (13).
The standard "forward-backward" procedure was applied to translate the questionnaire from English into Persian. Two independent English experts translated the items, two others translated the response categories, and a provisional version was provided. Careful cultural adaptation of the final version was provided. Subsequently it was back translated into English and checked by another two English experts to confirm the similarity of the translated items to the original questionnaire.
Factor analysis
Factor analysis attempts to identify underlying variables, or factors, which explains the pattern of correlation within a set of observed variables. Factor analysis is often used in data reduction to identify a small number of factors that explain most of the variance observed in a much larger number of manifest variables. In this study, factor structure of the questionnaire was done. Criteria for identification of domains and items to be retained on factor analysis were factors with eigenvalues >1.0 and items with factor loading >0.4, and Pearson’s correlation coefficient R value < 0.3. If the Cronbach's alpha (α) value was acceptable (above 0.6 to 0.7) and could not be improved by the removal of items, this was acknowledged as a domain (15).
Internal consistency
Internal consistency of the questionnaire was assessed by Cronbach's alpha coefficient and values equal to or greater than 0.70 was considered satisfactory (16). Internal consistency, a correlational determination of the goodness of fit of the items within a domain, is measured on a scale of 0–1. In our study, we watched 49 couples who had undergone treatment with Sildenafil citrate (Viagra; Pfizer, India) for FSD. Forty-four normal subjects fill the questionnaire at baseline and 4-8 weeks later. We used data of whole sample and the data of before-after treatment of these two groups to find out internal consistency.
Reliability
To determine test-retest reliability, Pearson’s correlations were used. Data of 44 normal participants were used to determine test-retest reliability.
Validity
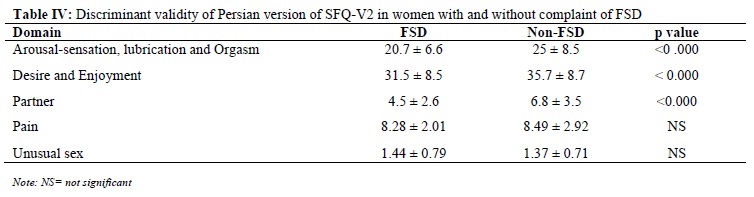
To determine validity of the questionnaire discriminant validity was assessed. Discriminant validity refers to the ability of items to show clear, statistically significant differences between populations known to differ on aspects of function. In the studies used other questionnaires, there was a significant difference between the baseline mean SFQ domain scores of patients with FSD compared with those of women without FSD (13, 17-20). In our study, mean values of domains were compared between patients complained from FSD and normal participants.
Results are presented as means ± SD or percentile. Statistical analysis was conducted using factor analysis, reliability analysis, and Student’s t-test as appropriate. The significant level was set at p-value less than 0.05. Data analysis was carried out using Statistical Package for Social Science (SPSS 11.0; Chicago, IL).
Results
The study was carried out on 547 subjects. Their characteristics are shown in Table 1. A total of 227 (42%) participants had a FSD score of <5, found out by self-rating scale. Principal components analysis with varimax rotation was conducted in order to identify possible new domains (Table II). This method was used by authors who introduced the questionnaire (13). By this way, Quirk et al (13) found seven domains. To compare their domains with our study, the factor scores of Quirk et al study are included in parentheses in Table II. We found five domains in our analysis.
Questions entered in first domain were similar to questions located in arousal-lubrication, arousal-sensation, and orgasm domains of Quirk et al study (13). Therefore, this domain was named arousal-orgasm domain. Items located in second domain were as items of enjoyment and desire domains of Quirk et al study. The exception was question 18: Over the last 4 weeks, in general, how much did you enjoy sexual activity without penetration (e.g., masturbation and oral sex)?
Enjoyment-desire was the suitable name for this domain. In total 72.2% of patients responded to question 18 with negative slant. They answered “Not enjoyable” to this question.
Pain and partner domains were as same as original article. The last domain consisted question 18. Because of concept of this question, we named it as unusual sex domain. Five-factor structure accounted for 63% of the variance.
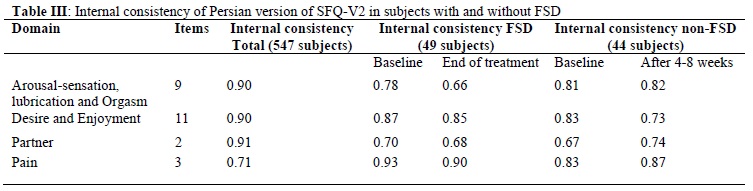
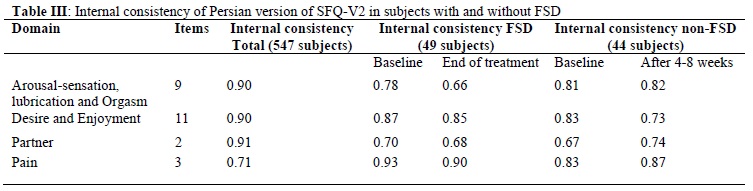
Internal consistency of Persian version of SFQ ranged from 0.71 to 0.91 in total sample. Values were similar between the patients complained from FSD and normal samples. Baseline values were comparable with values obtained from second questionnaire administered after treatment or after 4-8 weeks (Table III).
The item test-retest reliability showed fair scaling results for the normal samples. R values for Pearson’s correlation coefficient for individual domains were as follows; 0.9 for arousal-orgasm domain, 0.85 for enjoyment-desire domain, 0.81 for pain domain, 0.96 for partner domain, and 0.91 for unusual sex domain.
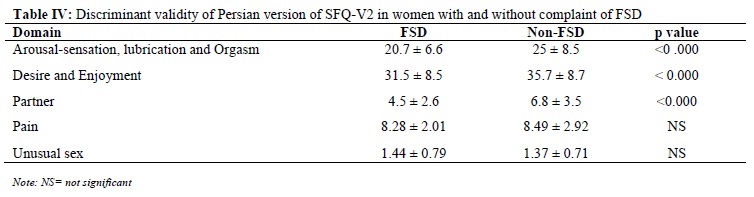
There was a significant difference between the baseline mean SFQ domain scores of patients with FSD complaint compared with those of women without FSD complaint (except for pain and unusual sex) (p < 0.000) (Table IV).
Discussion
The original version of SFQ is a sexual questionnaire with excellent internal consistency, moderate to good reliability, excellent discriminant validity, longitudinal validity, and construct validity (13).
In factor analysis of Persian version of SFQ we found five domains. These domains included arousal-orgasm (Q7–12, Q22–24; score range 9–45), enjoyment-desire Q1–4, 6, 13-14,19,21, 25-26; score range 10–56), pain (Q15, 16, 20; score range 2–15), partner relationship (Q28, 29; score range 2–10), and unusual sex (Q18; score range 1-5).
All items and domains had reasonable correlation with their own dimension. However, as only one item of enjoyment domain produced a significantly different correlation, the results were considered satisfactory (20). Cronbach’s alpha values being above the 0.70 threshold for all domains indicated excellent internal consistency reliability. R values for Pearson’s correlation coefficient of 0.81 to 0.91 for individual items is a reasonable result.
In comparison of patients with FSD complaint and normal subjects, mean score of all domains except pain and unusual sex domain were significantly higher in patients with problem. Other studies compared definitely diagnosed FSD with normal subjects, found out the significantly higher scores in women with FSD (11, 17-20). Samples of Quirk et al (13) study displayed some type of sexual dysfunction conditions for at least 6 months prior to the study. In contrast, the majority of our samples were recruited from normal population. It seems that concept of organic disease was matched more than FSD to pain symptom. Participants with pain in their sexual function did not point it out as FSD. So, the mean score of pain domain did not significantly differed between the two groups.
The response to item unusual sex domain was negative in 72.2% of participants. This makes the result of comparing means to be unreliable (Table IV).
In Persian version of SFQ, the items of arousal-sensation, arousal lubrication, and orgasm domain in original version were categorized in one factor. As the original domains figured out separate items in sexual dysfunction, it is reasonable to assume the original domains. The domain named enjoyment-desire was similar to two domains of enjoyment and desire domain of the original version. Question 18 [Over the last 4 weeks, in general, how much did you enjoy sexual activity without penetration? (e.g., masturbation and oral sex)] had different results. The results of question 18 should discuss with caution in Iranian population. This is due to different cultural insight in eastern countries. Question 18 can be analyzed separately as unusual sex factor.
It seems that with exception of results of question 18, Persian version of SFQ has reasonable validity and reliability to use for Iranian population. Results of question 18 should interpret separately. The score ranges of Quirk et al study were based on their database of subjects. One study emphasized that the scores may be subject to alteration as the database increases (21). In using Quirk et al scores, only score of domain enjoyment should be adjusted in the Persian version. By subtracting question 18 from the list of questions in this item we can calculate the scores again with five questions. Maximum score of this item change from 30 to 25 in Persian version. Therefore, the 15% decrease in total score can be manipulated to all scores in this domain. Scores 6-16 indicates high probability of FSD in enjoyment domain. This score will change to 5-13 in Persian version. Score of borderline probability of normal sexual function, which was 17-22 in original version, will change to 14-18. Score of 23-30, which is indicative of high probability of normal sexual dysfunction, will change to 19-25 in Persian version of SFQ. Future studies on Iranian samples can disclose the scores more correctly.
Conclusion
We emphasize that there are a number of meaningful relationships between sexual function and socio-cultural variables, which were not mentioned here. Thus, in future studies, other questions in relation to socio-cultural variables should be included and evaluated specifically for Iranian subjects.
Acknowledgements
We gratefully acknowledge the participation of the infertility ward staff of Shariati Hospital: Nahid Abbassi Moaff, Sedeegheh Amrollahi and Zahra Rezaian Movahed. This study was supported by Vali-e-Asr Reproductive Health Research Center, Tehran University of Medical Sciences.
Full-Text: (1087 Views)
Introduction
Female sexual dysfunction (FSD) is a real problem that affects a significant number of populations. Increased awareness of this problem in the medical community will lead to further research in female sexual dysfunction, and improved treatment (1). FSD is highly prevalent, occurring in 25–63% of women (2). A meta-analysis estimated prevalence of orgasmic disorders to be 7–10% (3).
Although the best method of screening and diagnosis of FSD is structured interview by several designed questionnaires. Some of these tests are designed to address one specific aspect of FSD such as ease in arousal or level of sexual desire (4-5). The Sexual Activity Questionnaire was designed to assess the impact of cancer treatments on sexual function (6). The Sexual Interaction Survey and the Sexual Interaction System Scale have a dyadic focus (7-8). More multidimensional measures include the Derogatis Sexual Function Inventory (DSFI), a collection survey of sexual attitude, experience, and satisfaction, and the Brief Index of Sexual Functioning for Women (9-10).
The more recently developed Female Sexual Function Index has already been used in several clinical trials (11). Now there are newer questionnaires in relation to sexual dysfunction. The Sexual Quality of Life-Female (SQOL-F) questionnaire has been developed to assess the impact of female sexual dysfunction (FSD) on a woman's sexual quality of life. SQOL-F items were developed through interviews with 82 women. The SQOL-F showed good psychometric properties: convergent validity, discriminate validity, and test-retest reliability. However, the SQOL-F sensitivity should be confirmed (12). Sexual Function Questionnaire (SFQ) is a self- reported outcomes measure of female sexual function (13). The SFQ addresses all aspects of the sexual response cycle and pain, incorporating the more recently developed classifications (14).
In our knowledge, there is no valid Persian version of sexual inventory. The aim of this study was to translate SFQ in Persian (Iranian language) and test the reliability and validity of Persian version of SFQ.
Materials and Methods
From March to October 2005, in total 547 women participated in a cross-sectional study. The participants included 73 pregnant subjects, 167 infertile patients, 258 normal subjects (university students or subjects visited the contraception clinic) and 49 patients visited for gynecological problems. The study was approved by the Ethical Committee of Tehran Medical Sciences University. Institutional Review Board approval was obtained before commencing the trial as well. All patients and their husbands gave their written permission.
The main characteristics of the studied population are described in Table I. A questionnaire asked about female and her partner age, duration of marriage, level of education of female and her partner, and female occupation. All patients were initially evaluated for satisfaction of sexual function by asking a single question: ‘How much is your satisfaction rate from your sexual function?’ The answer estimated by a self-rating scale, which was shown in the demographic questionnaire.
Self-rating scale was scored 0 to 10 in a positive regression. Due to rules of ethics, patients with score <5 were offered sexologist visit for confirmation of diagnosis and treatment if needed. We put the open question about FSD on demographic questionnaire to compare the scores obtained by the main questionnaire of sexual dysfunction in patients complained from FSD with normal subjects.
Questionnaire
A questionnaire named Sexual Function Questionnaire-version 2 (SFQ-V2) with 7 domains and 26 items was used. The 7 domains of SFQ are consisting of 26 items. These 7 domains included: desire (Q1–4, 13, 26; score range 5–31), arousal-sensation (Q7–10; score range 4–20), arousal-lubrication (Q11–12; score range 2–10), orgasm (Q22–24; score range 3–15), enjoyment (Q6, 14, 18, 19, 21, 25; score range 6–30), pain (Q15, 16, 20; score range 2–15), and partner relationship (Q28, 29; score range 2–10). (Table II) (13).
The standard "forward-backward" procedure was applied to translate the questionnaire from English into Persian. Two independent English experts translated the items, two others translated the response categories, and a provisional version was provided. Careful cultural adaptation of the final version was provided. Subsequently it was back translated into English and checked by another two English experts to confirm the similarity of the translated items to the original questionnaire.
Factor analysis
Factor analysis attempts to identify underlying variables, or factors, which explains the pattern of correlation within a set of observed variables. Factor analysis is often used in data reduction to identify a small number of factors that explain most of the variance observed in a much larger number of manifest variables. In this study, factor structure of the questionnaire was done. Criteria for identification of domains and items to be retained on factor analysis were factors with eigenvalues >1.0 and items with factor loading >0.4, and Pearson’s correlation coefficient R value < 0.3. If the Cronbach's alpha (α) value was acceptable (above 0.6 to 0.7) and could not be improved by the removal of items, this was acknowledged as a domain (15).
Internal consistency
Internal consistency of the questionnaire was assessed by Cronbach's alpha coefficient and values equal to or greater than 0.70 was considered satisfactory (16). Internal consistency, a correlational determination of the goodness of fit of the items within a domain, is measured on a scale of 0–1. In our study, we watched 49 couples who had undergone treatment with Sildenafil citrate (Viagra; Pfizer, India) for FSD. Forty-four normal subjects fill the questionnaire at baseline and 4-8 weeks later. We used data of whole sample and the data of before-after treatment of these two groups to find out internal consistency.
Reliability
To determine test-retest reliability, Pearson’s correlations were used. Data of 44 normal participants were used to determine test-retest reliability.
Validity
To determine validity of the questionnaire discriminant validity was assessed. Discriminant validity refers to the ability of items to show clear, statistically significant differences between populations known to differ on aspects of function. In the studies used other questionnaires, there was a significant difference between the baseline mean SFQ domain scores of patients with FSD compared with those of women without FSD (13, 17-20). In our study, mean values of domains were compared between patients complained from FSD and normal participants.
Results are presented as means ± SD or percentile. Statistical analysis was conducted using factor analysis, reliability analysis, and Student’s t-test as appropriate. The significant level was set at p-value less than 0.05. Data analysis was carried out using Statistical Package for Social Science (SPSS 11.0; Chicago, IL).
Results
The study was carried out on 547 subjects. Their characteristics are shown in Table 1. A total of 227 (42%) participants had a FSD score of <5, found out by self-rating scale. Principal components analysis with varimax rotation was conducted in order to identify possible new domains (Table II). This method was used by authors who introduced the questionnaire (13). By this way, Quirk et al (13) found seven domains. To compare their domains with our study, the factor scores of Quirk et al study are included in parentheses in Table II. We found five domains in our analysis.
Questions entered in first domain were similar to questions located in arousal-lubrication, arousal-sensation, and orgasm domains of Quirk et al study (13). Therefore, this domain was named arousal-orgasm domain. Items located in second domain were as items of enjoyment and desire domains of Quirk et al study. The exception was question 18: Over the last 4 weeks, in general, how much did you enjoy sexual activity without penetration (e.g., masturbation and oral sex)?
Enjoyment-desire was the suitable name for this domain. In total 72.2% of patients responded to question 18 with negative slant. They answered “Not enjoyable” to this question.
Pain and partner domains were as same as original article. The last domain consisted question 18. Because of concept of this question, we named it as unusual sex domain. Five-factor structure accounted for 63% of the variance.
Internal consistency of Persian version of SFQ ranged from 0.71 to 0.91 in total sample. Values were similar between the patients complained from FSD and normal samples. Baseline values were comparable with values obtained from second questionnaire administered after treatment or after 4-8 weeks (Table III).
The item test-retest reliability showed fair scaling results for the normal samples. R values for Pearson’s correlation coefficient for individual domains were as follows; 0.9 for arousal-orgasm domain, 0.85 for enjoyment-desire domain, 0.81 for pain domain, 0.96 for partner domain, and 0.91 for unusual sex domain.
There was a significant difference between the baseline mean SFQ domain scores of patients with FSD complaint compared with those of women without FSD complaint (except for pain and unusual sex) (p < 0.000) (Table IV).
Discussion
The original version of SFQ is a sexual questionnaire with excellent internal consistency, moderate to good reliability, excellent discriminant validity, longitudinal validity, and construct validity (13).
In factor analysis of Persian version of SFQ we found five domains. These domains included arousal-orgasm (Q7–12, Q22–24; score range 9–45), enjoyment-desire Q1–4, 6, 13-14,19,21, 25-26; score range 10–56), pain (Q15, 16, 20; score range 2–15), partner relationship (Q28, 29; score range 2–10), and unusual sex (Q18; score range 1-5).
All items and domains had reasonable correlation with their own dimension. However, as only one item of enjoyment domain produced a significantly different correlation, the results were considered satisfactory (20). Cronbach’s alpha values being above the 0.70 threshold for all domains indicated excellent internal consistency reliability. R values for Pearson’s correlation coefficient of 0.81 to 0.91 for individual items is a reasonable result.
In comparison of patients with FSD complaint and normal subjects, mean score of all domains except pain and unusual sex domain were significantly higher in patients with problem. Other studies compared definitely diagnosed FSD with normal subjects, found out the significantly higher scores in women with FSD (11, 17-20). Samples of Quirk et al (13) study displayed some type of sexual dysfunction conditions for at least 6 months prior to the study. In contrast, the majority of our samples were recruited from normal population. It seems that concept of organic disease was matched more than FSD to pain symptom. Participants with pain in their sexual function did not point it out as FSD. So, the mean score of pain domain did not significantly differed between the two groups.
The response to item unusual sex domain was negative in 72.2% of participants. This makes the result of comparing means to be unreliable (Table IV).
In Persian version of SFQ, the items of arousal-sensation, arousal lubrication, and orgasm domain in original version were categorized in one factor. As the original domains figured out separate items in sexual dysfunction, it is reasonable to assume the original domains. The domain named enjoyment-desire was similar to two domains of enjoyment and desire domain of the original version. Question 18 [Over the last 4 weeks, in general, how much did you enjoy sexual activity without penetration? (e.g., masturbation and oral sex)] had different results. The results of question 18 should discuss with caution in Iranian population. This is due to different cultural insight in eastern countries. Question 18 can be analyzed separately as unusual sex factor.
It seems that with exception of results of question 18, Persian version of SFQ has reasonable validity and reliability to use for Iranian population. Results of question 18 should interpret separately. The score ranges of Quirk et al study were based on their database of subjects. One study emphasized that the scores may be subject to alteration as the database increases (21). In using Quirk et al scores, only score of domain enjoyment should be adjusted in the Persian version. By subtracting question 18 from the list of questions in this item we can calculate the scores again with five questions. Maximum score of this item change from 30 to 25 in Persian version. Therefore, the 15% decrease in total score can be manipulated to all scores in this domain. Scores 6-16 indicates high probability of FSD in enjoyment domain. This score will change to 5-13 in Persian version. Score of borderline probability of normal sexual function, which was 17-22 in original version, will change to 14-18. Score of 23-30, which is indicative of high probability of normal sexual dysfunction, will change to 19-25 in Persian version of SFQ. Future studies on Iranian samples can disclose the scores more correctly.
Conclusion
We emphasize that there are a number of meaningful relationships between sexual function and socio-cultural variables, which were not mentioned here. Thus, in future studies, other questions in relation to socio-cultural variables should be included and evaluated specifically for Iranian subjects.
Acknowledgements
We gratefully acknowledge the participation of the infertility ward staff of Shariati Hospital: Nahid Abbassi Moaff, Sedeegheh Amrollahi and Zahra Rezaian Movahed. This study was supported by Vali-e-Asr Reproductive Health Research Center, Tehran University of Medical Sciences.
Type of Study: Original Article |
References
1. DeUgarte CM, Berman L, Berman J. Female Sexual Dysfunction-from Diagnosis to Treatment. Sexuality, Reproduction & Menopause 2004;2:139-145. [DOI:10.1016/j.sram.2004.07.002]
2. Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44. [DOI:10.1001/jama.281.6.537]
3. Simons JS, Carey MP. Prevalence of sexual dysfunctions: results from a decade of research. Arch Sex Behav 2001;30:177-219. [DOI:10.1023/A:1002729318254]
4. Hoon EF, Joon PW, Wincze JP. An inventory for the measurement of female sexual arousability: The SAI. Arch Sex Behav 1976;5:269-274. [DOI:10.1007/BF01542081]
5. Spector IP, Carey MP, Steinberg L. The sexual desire inventory: development, factor structure, and evidence of reliability. J Sex Marital Ther 1996;22:175-190. [DOI:10.1080/00926239608414655]
6. Thirlaway K, Fallowfield L, Cuzick J. The Sexual Activity Questionnaire: a measure of women's sexual functioning. Qual Life Res 1996;5:81-90. [DOI:10.1007/BF00435972]
7. LoPiccolo J, Steger JC. The sexual interaction inventory: a new instrument for assessment of sexual dysfunction. Arch Sex Behav 1974;3:585-595. [DOI:10.1007/BF01541141]
8. Woody JD, D'Souza HJ. The Sexual Interaction System Scale: a new inventory for assessing sexual dysfunction and sexual distress. J Sex Marital Ther 1994;20:210-228. [DOI:10.1080/00926239408403431]
9. Derogatis LR, Melisaratos N. The DSFI: a multidimensional measure of sexual functioning. J Sex Marital Ther 1979;5:244-81. [DOI:10.1080/00926237908403732]
10. Mazer NA, Leiblum SR, Rosen RC. The brief index of sexual functioning for women (BISF-W): a new scoring algorithm and comparison of normative and surgically menopausal population. Menopause 2000;5:350-363. [DOI:10.1097/00042192-200007050-00009]
11. Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, et al. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 2000; 26:191-208. [DOI:10.1080/009262300278597]
12. Symonds T, Boolell M, Quirk F. Development of a questionnaire on sexual quality of life in women. J Sex Marital Ther 2005;31:385-397. [DOI:10.1080/00926230591006502]
13. Quirk FH, Heiman JH, Rosen RC, Laan E, Smith MD, Boolell M. Development of a Sexual Function Questionnaire for Clinical Trials of Female Sexual Dysfunction. J Womens Health Gend based Med 2002; 11:277-289 [DOI:10.1089/152460902753668475]
14. Basson R, Berman J, Burnett A, Derogatis L, Ferguson D, Fourcroy J, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol 2000;163:888-893. [DOI:10.1016/S0022-5347(05)67828-7]
15. Bullinger M, Power MJ, Aaronson NK, Cella DF, Anderson RT. Creating and Evaluating Cross-Cultural Instruments. in: Quality of Life and Pharmacoeconomics in Clinical Trials. Edited by Spilker B. Philadelphia: Lippincott-Raven; 1996;659-668.
16. Nunnally JC, Bernstien IH. Psychometric Theory. 3rd edition. New York:McGraw-Hill ;1994.
17. Wiegel M, Meston C, Rosen R. The female sexual function index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 2005;31:1-20. [DOI:10.1080/00926230590475206]
18. Matzaroglou C, Assimakopoulos K, Panagiotopoulos E, Kasimatis G, Dimakopoulos P, Lambiris E. Sexual function in females with severe cervical spinal cord injuries: a controlled study with the Female Sexual Function Index. Int J Rehabil Res 2005;28:375-377. [DOI:10.1097/00004356-200512000-00014]
19. Meston CM. Validation of the Female Sexual Function Index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther 2003;29:39-46. [DOI:10.1080/713847100]
20. Derogatis L, Rust J, Golombok S, Bouchard C, Nachtigall L, Rodenberg C, et al. Validation of the profile of female sexual function (PFSF) in surgically and naturally menopausal women. J Sex Marital Ther 2004;30:25-36. [DOI:10.1080/00926230490247183]
21. De la Loge C, Sullivan K, Pinkney R, Marquis P, Roux C, Meunier PJ. Cross-cultural validation and analysis of responsiveness of the QUALIOST: QUAlity of Life questionnaire In OSTeoporosis. Health Qual Life Outcomes 2005; 3:69. [DOI:10.1186/1477-7525-3-69]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |