Tue, Feb 3, 2026
[Archive]
Volume 4, Issue 2 (7-2006)
IJRM 2006, 4(2): 81-83 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ilkhanizadeh B, Taghizadieh M, Mahzad-Sadaghiani M, Noroozinia F, Jahandideh B. Extragonadal germ cell tumor and male infertility. IJRM 2006; 4 (2) :81-83
URL: http://ijrm.ir/article-1-51-en.html
URL: http://ijrm.ir/article-1-51-en.html
Behrouz Ilkhanizadeh * 
 , Mohammad Taghizadieh
, Mohammad Taghizadieh 
 , Mehrzad Mahzad-Sadaghiani
, Mehrzad Mahzad-Sadaghiani 
 , Farahnaz Noroozinia
, Farahnaz Noroozinia 
 , Bahman Jahandideh
, Bahman Jahandideh 


 , Mohammad Taghizadieh
, Mohammad Taghizadieh 
 , Mehrzad Mahzad-Sadaghiani
, Mehrzad Mahzad-Sadaghiani 
 , Farahnaz Noroozinia
, Farahnaz Noroozinia 
 , Bahman Jahandideh
, Bahman Jahandideh 

Full-Text [PDF 197 kb]
(730 Downloads)
| Abstract (HTML) (3153 Views)
Full-Text: (488 Views)
Introduction
Germ cell tumors are the most common malignant tumors in young men between 25 and 29 years of age. Extragonadal germ cell tumors (EGCT) occurring in the sacrococcygeum, retroperitoneum, mediastinum and CNS. It was reported that testicular cancers has been increasing in many populations over the past decades (1), and there is some evidence to suggest that sperm quality has decreased in the same period (2-6). Definite comparison between testicular tumors and sperm quality in Iranian patients was not done and is limited to few case reports (3). Carroll et al reported eight patients with EGCT who had undergone testicular biopsy or orchiectomy and were retrospectively analyzed for primary testicular abnormalities, subfertility and abnormal sex hormone levels. It has been hypothesized that common etiological factors may exist for testicular cancer and for male subfertility (7).
Case report
A 30 years old man with history of infertility for 3 years ago, referred to our clinic with chief complaint of scrotal mass. Spermogram revealed azoospermia and ultrasound examination showed an extratesticular intrascrotal mass. Surgical exploration trough a Right inguinal approach showed only atrophic testes and isolated intrascrotal mass which was excised. Testis biopsy also was taken.
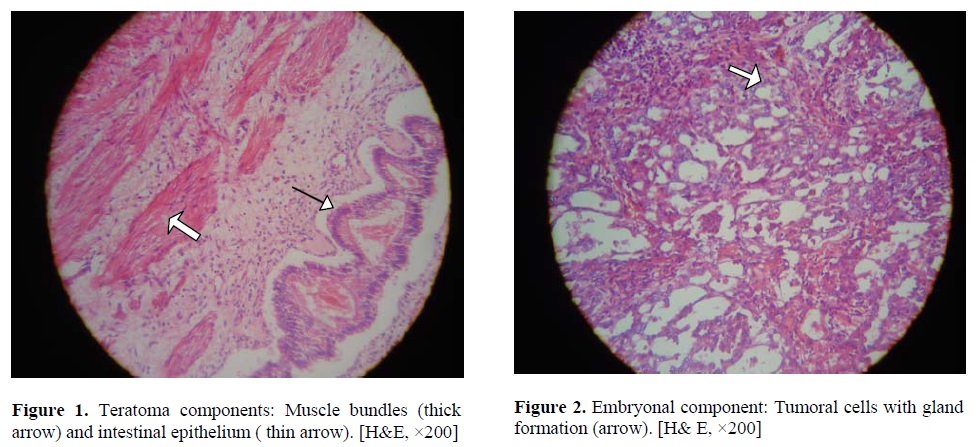
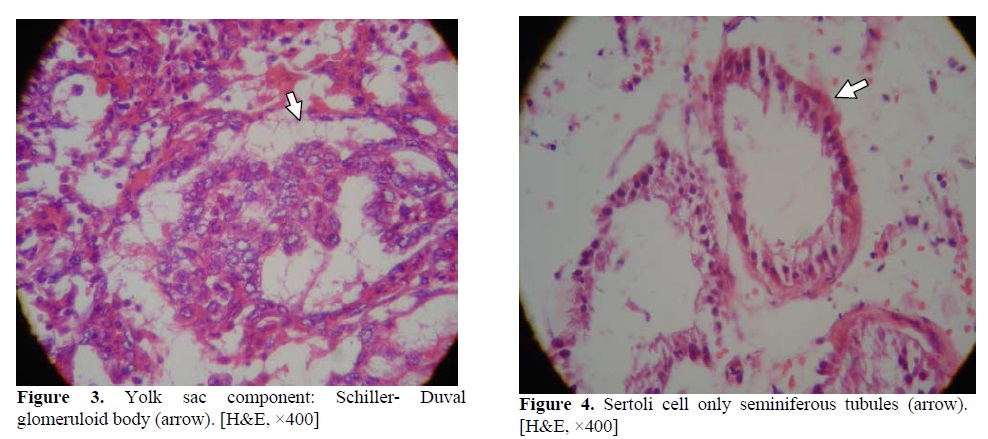
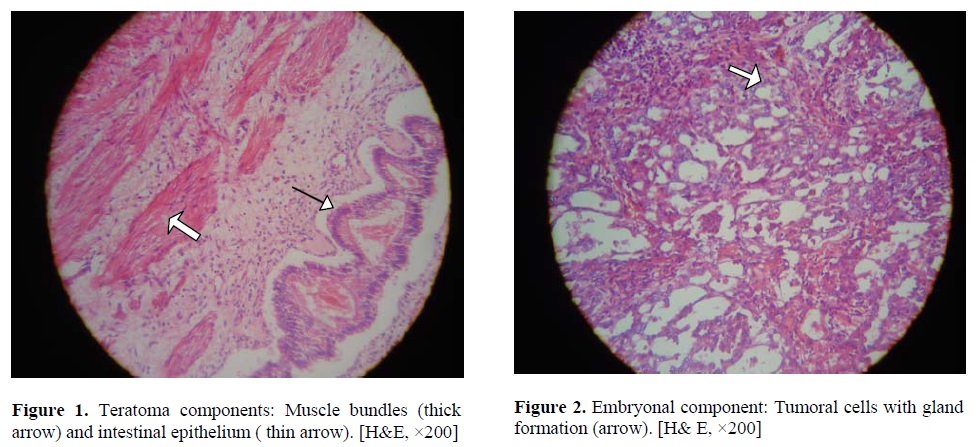
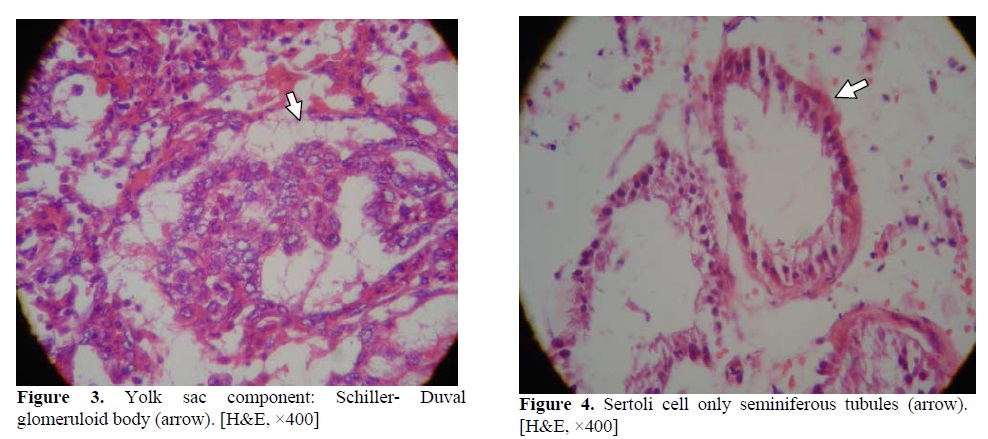
The gross examination revealed a multicystic mass measuring 9×6×5cm with bosselated external surface. Cut surfaces showed multiple variable sized cycts containing mucoid material, as well as solid areas. The microscopic examination showed mixed germ cell tumor containing teratoma, embryonal and yolk sac components (Figures1,2,3). Bilateral testicular biopsy showed only sertoli cells on microscopic examination (Figure 4). According to pathologic report of mixed germ cell tumor, patient’s treatment followed by left radical orchiectomy for definite histopathologic evaluation that showed only sertoli cells without evidence of any tumoral tissue. Abdominal CT-scan showed large retroperitoneal lymph nodes and retroperitoneal lymph nodes dissection (RPLND) was done for him. Tumor markers showed increased LDH, α-FP and β-HCG serum levels. Hormonal level of LH, FSH and testosterone were within normal limit. Patient was treated by adjuvant chemotherapy. Follow up after 5 months showed retroperitoneal multicystic mass located over the left renal vein in the CT scan. Second operation for mass excision was done. Histopathologic examination showed same previous tumor histology.
Discussion
Primary tumors of extragonadal origin are rare, fewer than 1000 cases described in the literature. Although the exact incidence of EGCTs is unknown, clinical data suggest that roughly 3% to 5% of all GCTs are of extragonadal origin (8,9).
The most common sites of origin, in decreasing order of frequency are mediastinum, retroperitoneum, sacrococcygeal region and pineal gland, although many unusual sites have also been reported (8).
The possible pathogensis of the origin of these neoplasms are including; 1- Displacement of primitive germ cells during early embryonic migration from the yolk sac, and 2- Persistence of pluripotential cells in sequestered primitive rests during early somatic development (9).
Males are predominantly affected, although a female predominance has been also noted with advanced local disease and distant metastasis. These tumors most commonly spread to regional lymph nodes, lung, liver and bone. EGCTs may reach a large size with no or relatively few symptoms. Clinical signs and symptoms of EGCT are related to its anatomic site of origin.
Some studies confirmed the association between subfertility in men and the subsequent risk of testicular cancer, the association is similar for seminoma and non-seminoma, and it persists when several potentially confounding factors are taken into account (10). One study showed that testicular cancer occurs more commonly in men who had fathered no or only few children when the age of the man is taken into account (11). These data support the hypothesis that male subfertility is associated with a high risk of testicular cancer. The most plausible explanation for this association is the existence of causal factors that are common to both subfertility and testicular cancer. The epidemiology of testicular cancer suggest that such common causes may act prenatally. There are also some case reports about coincidence of testicular tumors and azoospermia with Klinefeler syndrome (3). In this case report, we presented a case of EGCT of scrotal sac anatomic site in an infertile man with sertoli cell only.
We suggest Cohort studies to evaluate the multifactorial causes of coincidence of infertility and testicular tumors. In addition, a precise work up is suggested in patients with infertility and azoospermia (3).
Germ cell tumors are the most common malignant tumors in young men between 25 and 29 years of age. Extragonadal germ cell tumors (EGCT) occurring in the sacrococcygeum, retroperitoneum, mediastinum and CNS. It was reported that testicular cancers has been increasing in many populations over the past decades (1), and there is some evidence to suggest that sperm quality has decreased in the same period (2-6). Definite comparison between testicular tumors and sperm quality in Iranian patients was not done and is limited to few case reports (3). Carroll et al reported eight patients with EGCT who had undergone testicular biopsy or orchiectomy and were retrospectively analyzed for primary testicular abnormalities, subfertility and abnormal sex hormone levels. It has been hypothesized that common etiological factors may exist for testicular cancer and for male subfertility (7).
Case report
A 30 years old man with history of infertility for 3 years ago, referred to our clinic with chief complaint of scrotal mass. Spermogram revealed azoospermia and ultrasound examination showed an extratesticular intrascrotal mass. Surgical exploration trough a Right inguinal approach showed only atrophic testes and isolated intrascrotal mass which was excised. Testis biopsy also was taken.
The gross examination revealed a multicystic mass measuring 9×6×5cm with bosselated external surface. Cut surfaces showed multiple variable sized cycts containing mucoid material, as well as solid areas. The microscopic examination showed mixed germ cell tumor containing teratoma, embryonal and yolk sac components (Figures1,2,3). Bilateral testicular biopsy showed only sertoli cells on microscopic examination (Figure 4). According to pathologic report of mixed germ cell tumor, patient’s treatment followed by left radical orchiectomy for definite histopathologic evaluation that showed only sertoli cells without evidence of any tumoral tissue. Abdominal CT-scan showed large retroperitoneal lymph nodes and retroperitoneal lymph nodes dissection (RPLND) was done for him. Tumor markers showed increased LDH, α-FP and β-HCG serum levels. Hormonal level of LH, FSH and testosterone were within normal limit. Patient was treated by adjuvant chemotherapy. Follow up after 5 months showed retroperitoneal multicystic mass located over the left renal vein in the CT scan. Second operation for mass excision was done. Histopathologic examination showed same previous tumor histology.
Discussion
Primary tumors of extragonadal origin are rare, fewer than 1000 cases described in the literature. Although the exact incidence of EGCTs is unknown, clinical data suggest that roughly 3% to 5% of all GCTs are of extragonadal origin (8,9).
The most common sites of origin, in decreasing order of frequency are mediastinum, retroperitoneum, sacrococcygeal region and pineal gland, although many unusual sites have also been reported (8).
The possible pathogensis of the origin of these neoplasms are including; 1- Displacement of primitive germ cells during early embryonic migration from the yolk sac, and 2- Persistence of pluripotential cells in sequestered primitive rests during early somatic development (9).
Males are predominantly affected, although a female predominance has been also noted with advanced local disease and distant metastasis. These tumors most commonly spread to regional lymph nodes, lung, liver and bone. EGCTs may reach a large size with no or relatively few symptoms. Clinical signs and symptoms of EGCT are related to its anatomic site of origin.
Some studies confirmed the association between subfertility in men and the subsequent risk of testicular cancer, the association is similar for seminoma and non-seminoma, and it persists when several potentially confounding factors are taken into account (10). One study showed that testicular cancer occurs more commonly in men who had fathered no or only few children when the age of the man is taken into account (11). These data support the hypothesis that male subfertility is associated with a high risk of testicular cancer. The most plausible explanation for this association is the existence of causal factors that are common to both subfertility and testicular cancer. The epidemiology of testicular cancer suggest that such common causes may act prenatally. There are also some case reports about coincidence of testicular tumors and azoospermia with Klinefeler syndrome (3). In this case report, we presented a case of EGCT of scrotal sac anatomic site in an infertile man with sertoli cell only.
We suggest Cohort studies to evaluate the multifactorial causes of coincidence of infertility and testicular tumors. In addition, a precise work up is suggested in patients with infertility and azoospermia (3).
Type of Study: Original Article |
References
1. Adami HO, Bergstrom R, Mohner M, Zatosky W, Storm H, Ekbom A, et al. Testicular cancer in nine northern European countries. Int J Cancer 1994;59:33-38. [DOI:10.1002/ijc.2910590108] [PMID]
2. Bostofte E, Serup J, Rebbe H. Has the fertility of Danish men decline through the years in terms of semen quality? A comparison of semen qualities between 1952 and 1972. Int J Fertil 1983;28:91-95.
3. Okada H, Fujioka H, Tatsumi N. Klinefelter syndrome in the male infertility clinic. Hum rerpod 1991; 14: 946-952. [DOI:10.1093/humrep/14.4.946] [PMID]
4. Carlsen E, Giwercman A, Keiding N, Skakkebak NE. Evidence for decreasing quality of semen during past 50 years. BMJ 1992;305:609-613. [DOI:10.1136/bmj.305.6854.609] [PMID] [PMCID]
5. Auger J, Kunstmann JM, Czyglik F, Jouannet P. Decline in semen quality amogfertile men in paris during the past 20 years. N Engl J Med 1995;332:281-285. [DOI:10.1056/NEJM199502023320501] [PMID]
6. Irvine S, Cawood E, Richardson D, MacDonald E, Aitken J. Evidence of deteriorating semen quality in the United Kingdom: birth cohort study in 577 men in Scotland over 11 years. BMJ 1996;312:467-471. [DOI:10.1136/bmj.312.7029.467] [PMID] [PMCID]
7. Carroll PR, Withmore WF Jr, Herr HW, Morse MJ, Sogni PC, Bajorunas D, et al. Endocrine and exocrine profiles of men with testicular tumors before orchiectomy. J Urol 1987;137:420-423. [DOI:10.1016/S0022-5347(17)44054-7]
8. Luna MA, Valenzuela-Tamariz J. Germ cell tumors of the mediastinum: Postmortem findings. Am J Clin Pathol 1976;65:450. [DOI:10.1093/ajcp/65.4.450] [PMID]
9. Recondo J, Libshitz HI. Mediastinal extrgonadal germ cell tumors. Urology 1978;11:369. [DOI:10.1016/0090-4295(78)90234-0]
10. Moller H, Skakkebeak NE. Risk of testicular cancer in subfertile men: case-control study. BMJ 1999;318:559-62. [DOI:10.1136/bmj.318.7183.559] [PMID] [PMCID]
11. Berthelsen JG, Skakkebeak NE. Gonadal function in men with testis cancer. Fertil Steril 1983;39:68-75. [DOI:10.1016/S0015-0282(16)46760-9]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


