BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijrm.ir/article-1-54-en.html
Introduction
Infertility is usually defined as not being able to get pregnant despite trying for more than one year. A broader view of infertility includes not being able to carry a pregnancy. It is a stressful event in life and psychological symptoms that infertile women experience are similar to patients with other medical disorders such as, cancer, hypertension, and cardiac rehabilitation (1). Although the relationship between emotional stress and infertility has been widely accepted, this knowledge is still not widely used in the infertile couple’s care. Emotional tensions can directly affect fertility by altering hypothalamic–pituitary pathways or by causing tubal spasm, and indirectly by contributing to vaginismus, dyspareunia, frigidity, and to some extent, decrease in male libido. Equally important to the concept that emotional stress can affect fertility is the concept that infertility can result in emotional stress, thus initiating a vicious cycle (2). Even diagnosis of infertility can cause stress (3).
The psychological problems which have been most commonly investigated are anxiety and depression; anxiety because of the stressful nature of the treatment procedures and fear of treatment failure, depression because of the inability to conceive. Infertile women showed higher scores on the depression and anxiety scales (4,5). It was shown that anxiety was the major difficulty facing patients during infertility (6).
A study in Kuwait shows infertile women exhibited a significant higher psychopathology in the form of tension, hostility, anxiety, depression, self-blame and suicidal ideation. Childlessness result in social stigmatization for infertile women and put them at risk of serious social and emotional consequences (7).
Considering various studies and importance of relation between infertility and psychological state of women we have design this study to investigate the psychological disturbances in infertile Iranian women.
Materials and methods
A cross-sectional study was carried out by introducing a PHQ questionnaire to 198 patients who visited our obstetric and gynecologic clinic (affiliated to Fasa University of Medical Sciences) for psychiatric assessments. Overall 100 infertile patients with minimum of 3 and maximum of 8 yrs of infertility and average age of (24.2±4.5 years old) and 98 fertile women with average age of (25.3±4.3) were participated in this study. Exclusion criteria were probable other causes of psychiatric problems such as socio economic status, poverty, family problem and age. In order to detect emotional status, the subjects were evaluated, using PHQ questionnaire which is a useful instrument for the assessment of mental disorders, functional impairment and recent psychosocial stresses (8). The PHQ evaluates the 5 most common groups of mental health disorders (depression, anxiety, panic, somatoform, and eating disorders). PHQ diagnoses are based on diagnostic criteria contained in the American psychiatric association's diagnostic and statistical manual of mental disorders (DSM-IV), 4th edition (8).
The subjects were informed about the study and those were interested to joine were referred to sign a formal consent prior to the study.
Statistical analysis
The data were analyzed using chi-Square statistical analysis and p<0.05 was considered to be significant.
Results
Hundred and ninety–eight women at reproductive age took part in this cross-sectional study. Among them hundred were infertile and ninety–eight were fertile. The results of PHQ showed that twenty infertile women and eleven normal women have depression (table I). Depression group were subdivided into mild, moderate and severe cases.
Among the infertile patients, 40% of the patients have Major Depressive Disorder (MDD) in which 60% had sever type of MDD and 40% suffered from mild to moderate depression.
Among normal patients (n=98) 18% had MDD in which 27.3% had sever type of MDD and 72.7% suffered from mild to moderate depression.
Same analysis for the prevalence of anxiety and somatoform and panic disorder were done in all of the women. Forty six percent of infertile patients and 18.4 percent of normal women have anxiety disorders. The difference was significant (p<0.01).
Thirty out of 100 infertile women (30%) and twenty out of 98 fertile women (20.4%) have somatoform disorder which shows no significant difference.
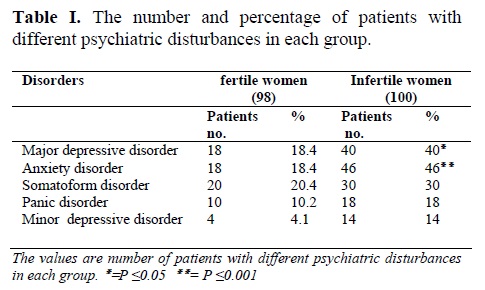
Eighteen out of hundred infertile patients (18%) and ten out of ninety eight fertile women (10.2%) have panic disorder (p=0.3).
Finally fourteen percent of infertile patients have minor depression which was not significantly different from this rate in fertile women.
Discussion
The purpose of this study was to find the relation between infertility and psychiatric disorders, using PHQ. This study was valuable because using a self-reported inventory which is different from psychiatric structured interview both in cost and time consumption, is reasonably valid and reliable. (8).
Women may develop depression, during different phases of the reproductive cycle (premenstrual dysphoric disorder, depression during pregnancy, postpartum depressive conditions, and menopausal depression). Other reproductive events such as miscarriage, oral contraceptives, and hormone replacement treatment have been reported to cause depression in women (9).
The prevalence of psychiatric morbidity especially depression and/or anxiety in infertile patients have been assessed in several countries. For example, anxiety was investigated in 130 infertile women in China. The results showed that different levels of mental pressure were found in 83.8% of infertile women (10). In our study the prevalence of MDD in infertile women was significantly high as compared with normal patients (40% vs. 18%). With regard to anxiety disorders, 46 of 100 infertile patients and 18 of 98 fertile women have other anxiety disorders which showed significant difference (p<0.01). These results are consistence with previous studies (6, 9,10).
One study indicated that infertile men showed more somatic complaints than a group of healthy male volunteers (11), to the best of our knowledge there is no such study about the relation between somatoform disorder and women infertility. Though, there is a report that showed diagnostic overlap between somatoform, depressive, and anxiety disorders in 79.6% of the patients (12).
In our study, infertile women have higher prevalence of somatoform disorder when compared with normal women but this difference was not significant. The results of the present study showed that infertile women were psychologically disturbed, specially in regard to depression and anxiety disorders, in which many factor are involved such as poverty, low socioeconomic status, low educational level, social pressure, lack of husband support, etc. Our finding is compatible with other studies .For example anxiety in childless Japanese women was significantly associated with lack of husband’s support (13). In addition, another study about Iranian infertile women showed that the level of education, low coping ability and being housewife has close relationship to anxiety level (14). On the other hand, sometimes childlessness results in social stigmatization that increases the risk of serious emotional consequences which in turn show the role of social support in management of infertile women (7,14).
Conclusion
It is suggested that in relation to higher prevalence of depression, the implementation of psychological interventions would help to reduce depressive symptoms especially for women with a definitive diagnosis and for those with durations of more than 2 years of infertility (1). For this purpose, it is necessary that the physician dealings with the infertile couple be aware of: 1) the role of primary emotional factors in the problem of infertility, and vice versa. 2) the additional emotional tensions may add to the problem after unsuccessful treatment. Considering the small sample size, the results of this study are limited, however further research about the cause of these psychological problems is suggested.
Acknowledgement
This work was supported by Fasa University of Medical Sciences.
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |