Sat, Dec 27, 2025
[Archive]
Volume 5, Issue 3 (7-2007)
IJRM 2007, 5(3): 77-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ragab Shalaby A M. Fallopian tube endometrioid carcinoma. IJRM 2007; 5 (3) :77-0
URL: http://ijrm.ir/article-1-67-en.html
URL: http://ijrm.ir/article-1-67-en.html
Oncologic Pathology Department, Damanhour National Medical Institute, El-Behera, Egypt , ahmad_shalaby20@yahoo.com
Full-Text [PDF 253 kb]
(723 Downloads)
| Abstract (HTML) (2502 Views)
Full-Text: (486 Views)
Introduction
Carcinoma of the fallopian tube is extremely uncommon neoplasm, accounting for only 0.3% of gynecologic cancer(1), but this figure may be low because carcinomas of uncertain origin involving both the ovary and the tube are generally classified as ovarian in view of their much higher overall frequency. In support of a higher frequency of tubal carcinoma than the figure just cited is a screening study using CA-125 assays that detected one tubal carcinoma for every six ovarian carcinomas (2-4).
Case Report
A 17-year-old female patient presented with clinical symptoms of right side deep pelvic pain and recurrent attacks of lower abdominal colic with a history of intermittent, profuse, watery, and biochemical investigations were performed for her but the results were within the normal limits. Ultrasound examination reveals right adenxal mass with breakdown suggesting neoplastic lesion or tubo-ovarian abscess. She was diagnosed clinically as tubo-ovarian mass for histopathological verification of its nature and prepared for surgery. The surprise was in that, the ovary was completely free from any pathological lesion but there was a large soft tissue lesion arising in the middle of the right fallopian tube. The tube was excised and sent for the pathology department. The patient was discharged on the next week. The pathology results revealed a large fusiform swelling which measured 12x9x7 cm in dimensions arising from middle third of the fallopian tube; leaving both the fimbrial and the uterine ends unaffected grossly (Figure I). On cut section, we found the lesion completely obstructing the lumen of the tube and appearing as a single solid mass distending and infiltrating the wall at the affected part of the tube. The tumor tissue varied in color from tan to yellow to white in cut section and firm in consistency; in general. The external surface was smooth; glistening and not penetrated the serosal surface of the tube but shows many congested blood vessels.
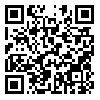
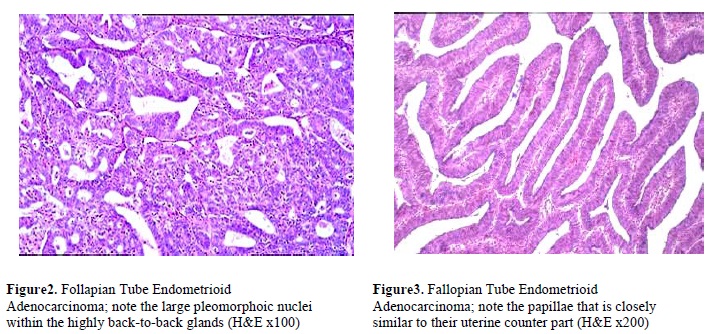
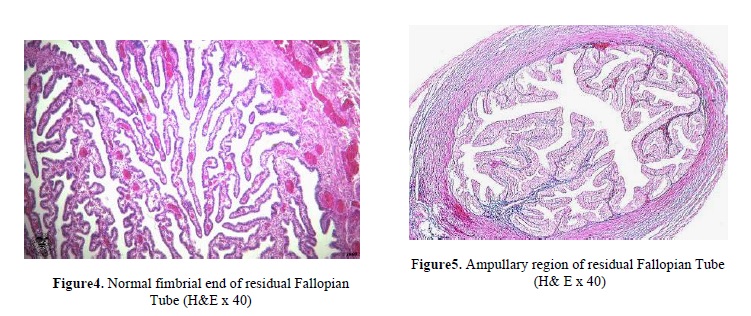
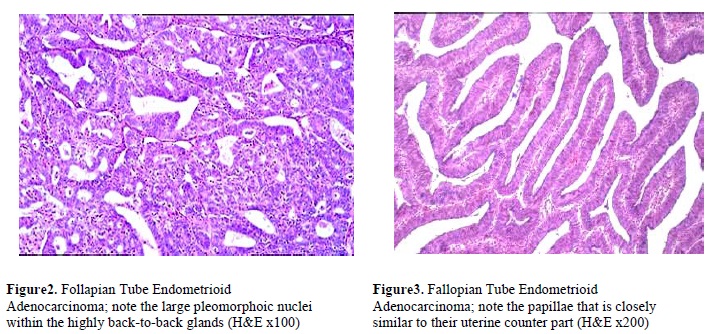
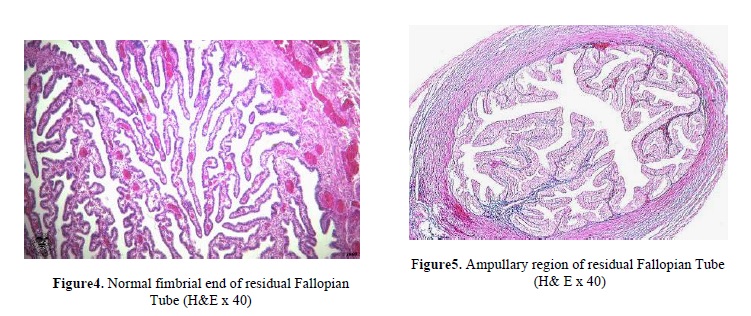
Histopathological analysis of the specimen revealed neoplastic growth formed of malignant glands and acini of endometrioid pattern (Figure 2) similar to the uterine counter part in slides prepared from the tumor area. The tumor also showed other morphological patterns as it contained solid areas and papillary foci (Figure 3) in other places, but no necrosis could be detected although serial sectioning of the specimen was achieved. The fimbrial end (Figure 4), ampullary region (Figure 5) and the uterine end were completely free from tumor invasion.

Discussion
The classic complaint of intermittent, profuse, watery, clear to turbid yellow vaginal discharge accompanied by colicky abdominal pain and followed by decrease in the size of the abdominal mass (hydrops tubae profluens) is encountered in only a minority of the cases (less than 10%).The diagnosis is usually unsuspected preoperatively (5,6). A rare case of carcinoma in situ of fallopian tube has been reported after tamoxafen therapy (5). On the bases of the cases reported in the literature, about 50% of tubal carcinomas are serous, about one-quarter endometrioid, one-fifth transitional or undifferentiated and the remainders are other epithelial types (6,7). Endometrioid carcinoma which is the second commonest subtype of tubal carcinoma is important to recognize because it carries the best prognosis of tubal cancers (6, 7).
Most tubal endometrioid carcinomas resemble the endometrial counterpart histologically and it may be associated with endometriosis, squamous metaplasia or prominent spindle epithelial cell component but this should not lead to mis-diagnosis as carcinosarcoma (7, 8). Involvement of tubal serosa, of the ovary or corpus uteri or other pelvic and abdominal structures indicates a poor prognosis (8- 10).
Acknowledgements
We thank Professor Nayera Anwar AbdAl-Hameid, Professor Nadia Mahmoud Mokhtar and Professor Magda Murad (Professors of Oncologic Pathology in National Cancer Institute, Cairo University) for their great help and advise that make this work possible.
Carcinoma of the fallopian tube is extremely uncommon neoplasm, accounting for only 0.3% of gynecologic cancer(1), but this figure may be low because carcinomas of uncertain origin involving both the ovary and the tube are generally classified as ovarian in view of their much higher overall frequency. In support of a higher frequency of tubal carcinoma than the figure just cited is a screening study using CA-125 assays that detected one tubal carcinoma for every six ovarian carcinomas (2-4).
Case Report
A 17-year-old female patient presented with clinical symptoms of right side deep pelvic pain and recurrent attacks of lower abdominal colic with a history of intermittent, profuse, watery, and biochemical investigations were performed for her but the results were within the normal limits. Ultrasound examination reveals right adenxal mass with breakdown suggesting neoplastic lesion or tubo-ovarian abscess. She was diagnosed clinically as tubo-ovarian mass for histopathological verification of its nature and prepared for surgery. The surprise was in that, the ovary was completely free from any pathological lesion but there was a large soft tissue lesion arising in the middle of the right fallopian tube. The tube was excised and sent for the pathology department. The patient was discharged on the next week. The pathology results revealed a large fusiform swelling which measured 12x9x7 cm in dimensions arising from middle third of the fallopian tube; leaving both the fimbrial and the uterine ends unaffected grossly (Figure I). On cut section, we found the lesion completely obstructing the lumen of the tube and appearing as a single solid mass distending and infiltrating the wall at the affected part of the tube. The tumor tissue varied in color from tan to yellow to white in cut section and firm in consistency; in general. The external surface was smooth; glistening and not penetrated the serosal surface of the tube but shows many congested blood vessels.
Histopathological analysis of the specimen revealed neoplastic growth formed of malignant glands and acini of endometrioid pattern (Figure 2) similar to the uterine counter part in slides prepared from the tumor area. The tumor also showed other morphological patterns as it contained solid areas and papillary foci (Figure 3) in other places, but no necrosis could be detected although serial sectioning of the specimen was achieved. The fimbrial end (Figure 4), ampullary region (Figure 5) and the uterine end were completely free from tumor invasion.

Discussion
The classic complaint of intermittent, profuse, watery, clear to turbid yellow vaginal discharge accompanied by colicky abdominal pain and followed by decrease in the size of the abdominal mass (hydrops tubae profluens) is encountered in only a minority of the cases (less than 10%).The diagnosis is usually unsuspected preoperatively (5,6). A rare case of carcinoma in situ of fallopian tube has been reported after tamoxafen therapy (5). On the bases of the cases reported in the literature, about 50% of tubal carcinomas are serous, about one-quarter endometrioid, one-fifth transitional or undifferentiated and the remainders are other epithelial types (6,7). Endometrioid carcinoma which is the second commonest subtype of tubal carcinoma is important to recognize because it carries the best prognosis of tubal cancers (6, 7).
Most tubal endometrioid carcinomas resemble the endometrial counterpart histologically and it may be associated with endometriosis, squamous metaplasia or prominent spindle epithelial cell component but this should not lead to mis-diagnosis as carcinosarcoma (7, 8). Involvement of tubal serosa, of the ovary or corpus uteri or other pelvic and abdominal structures indicates a poor prognosis (8- 10).
Acknowledgements
We thank Professor Nayera Anwar AbdAl-Hameid, Professor Nadia Mahmoud Mokhtar and Professor Magda Murad (Professors of Oncologic Pathology in National Cancer Institute, Cairo University) for their great help and advise that make this work possible.
Type of Study: Original Article |
References
1. Get persistent links for your reference list or bibliography.
Copy and paste the list, we’ll match with our metadata and return the links.
Members may also deposit reference lists here too.
1. Benedet JL, White GW. Malignant tumor fallopian tube. In: Coppleson M, ed. Gynecologic Oncology, Fundamental principles and clinical practice.Edinburgh:Churchil Livinstone, 1981:621-629.
2. Woolas R, Jacob I. What is the true incidence of primary fallopian tube carcinoma? Int J Gynecol Cancer 199; 4:384-388. [DOI:10.1046/j.1525-1438.1994.04060384.x]
3. Goldman JA, Gans B, Eckerling B. Hydrops tubae profluens- a symptom in tubal carcinoma. Obstet Gynecol 1961; 18:631-634.
4. Sedlis A. Primary carcinoma of the fallopian tube. Obstet Gynecol Surv 1961; 16:209-226. [DOI:10.1097/00006254-196104000-00022]
5. Sonnendecker HE, Cooper K, Kalian KN. Primary fallopian tube adenocarcinoma in situ associated with adjuvant tamoxifen therapy for breast carcinoma. Gynecol Oncol 1994; 52:402-407. [DOI:10.1006/gyno.1994.1069]
6. Gaffney EF, Cornog J. Endometrioid carcinoma of the fallopian tube arising in endometrioisis. Obstet Gynecol 1978; 52:34s-36s.
7. Daya D, Young RH, Scully RE. Endometrioid carcinoma of the fallopian tube resembling an adenxal tumor of probable wolffian origin. A report of six cases. Int J Gynecol Pathol 1992; 11:122-130. [DOI:10.1097/00004347-199204000-00006]
8. Hirai Y, Kaku S, Hamada T. Clinical study of primary carcinoma of the fallopian tube. Experience with 15 cases. Gynecol Oncol 1989;34:20-26. [DOI:10.1016/0090-8258(89)90098-X]
9. Schiller HM, Silverberg SG. Staging and prognosis in primary carcinoma of the fallopian tube. Cancer 1971;28:383-395.
https://doi.org/10.1002/1097-0142(197108)28:2<389::AID-CNCR2820280219>3.0.CO;2-2 [DOI:10.1002/1097-0142(197108)28:23.0.CO;2-2]
10. Talamato S, Bender BL, Ellis LD, Scioscia EA. Adenocarcinoma of the fallopian tube. An ultrastuctural study. Virchows Arch [A] 1982; 397:363-368. [DOI:10.1007/BF00496577]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |