Fri, Jul 11, 2025
[Archive]
Volume 5, Issue 4 (7-2007)
IJRM 2007, 5(4): 95-98 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
davar R, Ghandi S, Tayebi N. Does transabdominal ultrasound-guided embryo transfer improve pregnancy rates in ART cycles?. IJRM 2007; 5 (4) :95-98
URL: http://ijrm.ir/article-1-83-en.html
URL: http://ijrm.ir/article-1-83-en.html
1- Research and Clinical Center for Infertility, Shahid Sadoughi University of Medical Sciences, Yazd, Iran , r_davar@yahoo.com
2- Research and Clinical Center for Infertility, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
2- Research and Clinical Center for Infertility, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Full-Text [PDF 32 kb]
(571 Downloads)
| Abstract (HTML) (2838 Views)
Full-Text: (440 Views)
Introduction
Despite great developments in assisted reproduction, the clinical pregnancy rate (CPR) in in-vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) remains low. It has been estimated that up to 85 % of the embryos replaced into the uterine cavity fail to implant (1). This failure may be due to poor embryo quality, lack of uterine receptivity, or the technique of embryo transfer (ET).
Although ET is the vital step in ART cycle, ET technique had received little attention (2).
The use of ultrasound guidance during the transfer procedure helps to verify accurate embryo placement and to improve pregnancy outcomes (3).
For example, some studies showed that ultrasound-guided embryo transfer increased clinical pregnancy rate compared to the clinical touch technique (4-6).While other studies found no significant difference between ultrasound-guided and clinical touch uterine embryo transfers (7-9).
The aim of this prospective randomized study was to compare the effect of transabdominal ultrasound-guided embryo transfer and clinical touch on the clinical pregnancy rate after IVF or ICSI.
Materials and methods
Patients
A total of 180 infertile patients (20-39 years old) undergoing treatment with IVF-ET and ICSI from Research and Clinical Center for Infertility, Yazd, Iran were recruited into the study between September 2005 and August 2006. Written consent was obtained from patients prior to participation in the study. The study protocol was approved by the Ethics Committee, Faculty of Medicine, University of Shahid Sadoughi. Fresh embryos were transferred in all the patients. They were randomized prospectively by computer-generated random table on the day of embryo transfer into two groups: 1) Transabdominal Ultrasound-guided embryo transfer; 2) Clinical touch embryo transfer. The randomization table was made and kept by a nurse who was not involved in the recruitment of subjects. One of the skilled gynecologists was responsible for conducting embryo transfer in two groups.
Ovarian stimulation protocol
The patients were all treated with a long protocol for ovarian stimulation. In the long protocol, pituitary down-regulation was achieved by administrating buserelin acetate (suprefact; Hoechst AG, Germany) (0.5mg S.C.) per day starting from day 21 of menstrual cycle and the dose was decreased to 0.25cc per day when the menstrual bleeding happened. Then, stimulation was commenced using Human Menopausal Gonadotrophin ( HMG ) (Menogon, Ferring, Germany) from the second day of their menstrual cycle with a dose of 150-300 IU per day. Monitoring was carried out by transvaginal ultrasound (HS-4000 JAPAN) on day 7 of HMG stimulation. After more than three follicles larger than 18mm in diameter were observed, 10000 IU of human chorionic gonadotrophin (hCG) (Pregnyl®5000, Organon) was administered intramuscularly, and 36 hours later, oocytes were retrieved under general anesthesia by transvaginal ultrasound-guided aspiration. Mature oocytes were retrieved from follicular fluid and placed in G-fert (version 3; vitrolife, Goteborg, Sweden) and after fertilization; 2PN zygote was transferred to G-1 media (G-1 TM version 3; vitrolife, Goteborg, Sweden). All embryo transfers were performed 48h after oocyte retrieval. Before the transfer, the embryos were evaluated microscopically and the best-quality embryos were selected for the transfer. A maximum of three embryos were transferred.
The luteal phase was supported with Progesterone in oil, intramuscularly, per day administered by starting on the puncture day.
Technique of embryo transfer
Patients were admitted on the morning of embryo transfer and were randomized into two groups: embryo transfer under transabdominal ultrasound-guided (Hitachi, Japan, 2000, EZU-PC3A, 220 V and 3.5MHz) and clinical touch method. Those patients randomized to the ultrasound-guided group were asked to keep a full bladder before the transfer to assist visualization during the procedure. The patients in the clinical touch were allowed to pass urine according to their need and this was the usual practice of our center.
Preparation prior to the transfer was the same in both groups. The patient was placed in the dorsolithotomy position and a sterile speculum was inserted into the vagina. When the speculum was adequately positioned to visualize the cervix, the cervix was washed with a sponge soaked with transfer media, and cervix mucus was aspirated from the external os by means pipette pump. Embryos were prepared in the laboratory by lab technician prior to the transfer. When ultrasound was used, the position of the uterus and cervix was ascertained before placement of the transfer catheter. A ultrasoft catheter (Laboratoire CCD, Paris, France) was used in all patients of both groups.
In case group where ultrasound guidance was used, the catheter was advanced so that the tip was approximately 1.5cm from the uterine fundus and the embryo(s) were slowly released. In control group where the clinical touch method was used, the catheter was inserted through the cervical canal and the embryos were released according to the clinician's feeling as to the position of the catheter.
In both groups, the catheter was carefully removed after a period of 10s. Then it was checked under a stereomicroscope to ensure that all embryos had been transferred. After transfer, the patient was transferred to the recovery room and allowed to rest in the supine position with her legs slightly elevated for 30min following the procedure.
The difficulty of the replacement was determined by the following criteria:1)easy, for embryos were placed without effort using a catheter 2)difficult, transfers performed using a catheter but requiring the use of a tenaculum and cervical dilators.
Clinical pregnancy was defined as the presence of at least one gestational sac by ultrasound examination. An ongoing pregnancy was defined as the presence of at least one fetus with positive heart pulsations seen with ultrasound examination beyond the first trimester of pregnancy. Implantation rate was determined as the total number of gestational sacs with fetal heart beat seen on ultrasound examination in relation to the total number of embryos transferred. Also, the incidence of miscarriage was noted.
Statistical analysis
SPSS 13 for Windows Statistical Package was used for statistical analysis. Continuous variables were compared by Student's t-test if they were normally distributed. The Mann-Whitney U-test was used where the data were skewed. Differences in proportions were analyzed with X2-test or Fisher's exact test as appropriate. p<0.05 was considered statistically significant.
Results
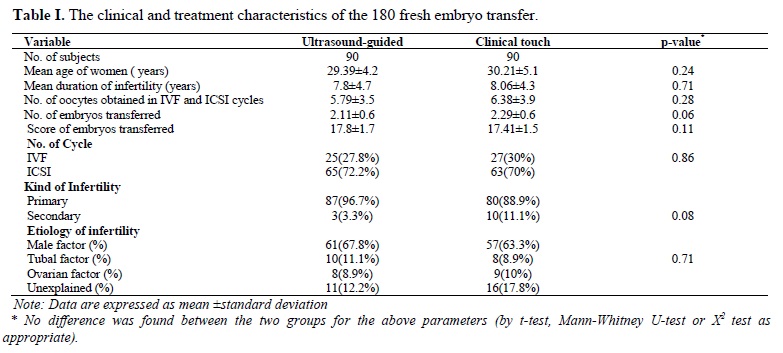
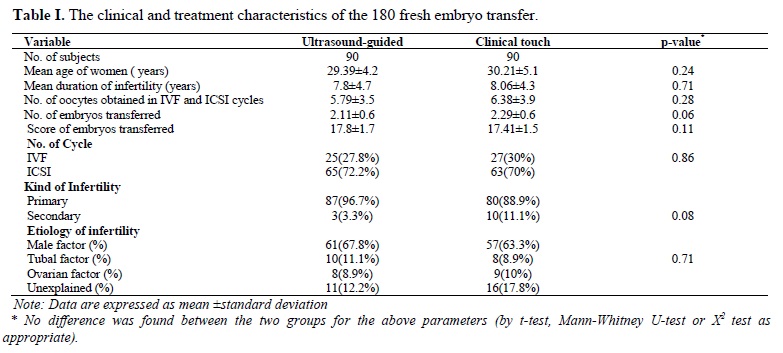
A total of 180 women who underwent embryo transfer in our Center were recruited into the study. All of them had fresh embryo transfer. The characteristics of the women are summarized in Table I. There were no differences in the age, duration and etiology of infertility and the number of embryo transferred between the Ultrasound-guided and clinical touch groups. The percentages of IVF and ICSI were similar in both groups.
Table II shows the pregnancy outcomes of the 180 cycles. The Clinical pregnancy rate was 21.1 % in the ultrasound-guided group and 15.5 % in the clinical touch group. The difference was not statistically significant. The ongoing pregnancy rate was 18.9% in the ultrasound and 12.2% in the clinical group and again the difference was not statistically significant. The implantation rate in the ultrasound guided group was 11.1% while this was 7.2% in the clinical group and there was no significant difference. In addition, all of the embryos were singleton and no significant differences were observed between two groups in terms of miscarriage rate.
The difference of percentage of difficult embryo transfers was not significant in groups. This was 8.9% in the ultrasound-guided group and 13.3% in the clinical touch group (p-value=0.47).

Discussion
Since the introduction of ultrasound-guided embryo transfer during the mid-1980s, this technique has evolved into a more routine part of ART practices around the world (10, 11). Although studies have suggested that a significant improvement in pregnancy and implantation rates has been observed following the use of
transabdominal guidance during embryo transfer
(12-14), other studies have refused these observations (15, 16).
In our research, 180 patients have been recruited into the study: 90 in ultrasound-guided embryo transfer group and 90 in clinical touch group. The characteristics of the comparison groups were similar with respect to the age of the patients, the etiology of infertility, the number and quality of embryos transferred. Also, the number of oocytes was obtained from IVF or ICSI cycles were the same. Failure to demonstrate a significant difference in our implantation and clinical pregnancy rates may be a consequence of the small size of our population.
Some studies have showed that keeping an appropriate distance between the tip of the internal catheter and the fundus of the uterus is an important point for a successful embryo transfer (17, 18).Kojima et al (2001) reported that the distance of 1.5cm was more suitable than 1cm and significantly improved the clinical pregnancy rate (17); whereas Rosenlund et al (1996) have found no relationship between the site of embryo deposition in the uterus and pregnancy outcome (19).In our study, although the tip of the catheter was positioned with the use of ultrasound at 1.5 cm from the fundus of the uterine cavity, there was no significant increase in pregnancy or implantation rate.The use of ultrasound guidance has been shown to decrease the incidence of difficult transfers (6, 20), but this finding is not consistent in all prospective studies (12).
Our results were in agreement with other studies that ET using ultrasound not only improved pregnancy outcome but also the use of ultrasound has been associated with easy transfers (7- 9, 21).
Conclusion
While more recent studies have been encouraging regarding the use of ultrasound-assisted embryo transfer, the value of experience in the clinical touch method can not be discounted. A large prospective study in our population would be necessary for definitive ascertainment of the value of routine simultaneous ultrasound monitoring during embryo transfer.
Despite great developments in assisted reproduction, the clinical pregnancy rate (CPR) in in-vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) remains low. It has been estimated that up to 85 % of the embryos replaced into the uterine cavity fail to implant (1). This failure may be due to poor embryo quality, lack of uterine receptivity, or the technique of embryo transfer (ET).
Although ET is the vital step in ART cycle, ET technique had received little attention (2).
The use of ultrasound guidance during the transfer procedure helps to verify accurate embryo placement and to improve pregnancy outcomes (3).
For example, some studies showed that ultrasound-guided embryo transfer increased clinical pregnancy rate compared to the clinical touch technique (4-6).While other studies found no significant difference between ultrasound-guided and clinical touch uterine embryo transfers (7-9).
The aim of this prospective randomized study was to compare the effect of transabdominal ultrasound-guided embryo transfer and clinical touch on the clinical pregnancy rate after IVF or ICSI.
Materials and methods
Patients
A total of 180 infertile patients (20-39 years old) undergoing treatment with IVF-ET and ICSI from Research and Clinical Center for Infertility, Yazd, Iran were recruited into the study between September 2005 and August 2006. Written consent was obtained from patients prior to participation in the study. The study protocol was approved by the Ethics Committee, Faculty of Medicine, University of Shahid Sadoughi. Fresh embryos were transferred in all the patients. They were randomized prospectively by computer-generated random table on the day of embryo transfer into two groups: 1) Transabdominal Ultrasound-guided embryo transfer; 2) Clinical touch embryo transfer. The randomization table was made and kept by a nurse who was not involved in the recruitment of subjects. One of the skilled gynecologists was responsible for conducting embryo transfer in two groups.
Ovarian stimulation protocol
The patients were all treated with a long protocol for ovarian stimulation. In the long protocol, pituitary down-regulation was achieved by administrating buserelin acetate (suprefact; Hoechst AG, Germany) (0.5mg S.C.) per day starting from day 21 of menstrual cycle and the dose was decreased to 0.25cc per day when the menstrual bleeding happened. Then, stimulation was commenced using Human Menopausal Gonadotrophin ( HMG ) (Menogon, Ferring, Germany) from the second day of their menstrual cycle with a dose of 150-300 IU per day. Monitoring was carried out by transvaginal ultrasound (HS-4000 JAPAN) on day 7 of HMG stimulation. After more than three follicles larger than 18mm in diameter were observed, 10000 IU of human chorionic gonadotrophin (hCG) (Pregnyl®5000, Organon) was administered intramuscularly, and 36 hours later, oocytes were retrieved under general anesthesia by transvaginal ultrasound-guided aspiration. Mature oocytes were retrieved from follicular fluid and placed in G-fert (version 3; vitrolife, Goteborg, Sweden) and after fertilization; 2PN zygote was transferred to G-1 media (G-1 TM version 3; vitrolife, Goteborg, Sweden). All embryo transfers were performed 48h after oocyte retrieval. Before the transfer, the embryos were evaluated microscopically and the best-quality embryos were selected for the transfer. A maximum of three embryos were transferred.
The luteal phase was supported with Progesterone in oil, intramuscularly, per day administered by starting on the puncture day.
Technique of embryo transfer
Patients were admitted on the morning of embryo transfer and were randomized into two groups: embryo transfer under transabdominal ultrasound-guided (Hitachi, Japan, 2000, EZU-PC3A, 220 V and 3.5MHz) and clinical touch method. Those patients randomized to the ultrasound-guided group were asked to keep a full bladder before the transfer to assist visualization during the procedure. The patients in the clinical touch were allowed to pass urine according to their need and this was the usual practice of our center.
Preparation prior to the transfer was the same in both groups. The patient was placed in the dorsolithotomy position and a sterile speculum was inserted into the vagina. When the speculum was adequately positioned to visualize the cervix, the cervix was washed with a sponge soaked with transfer media, and cervix mucus was aspirated from the external os by means pipette pump. Embryos were prepared in the laboratory by lab technician prior to the transfer. When ultrasound was used, the position of the uterus and cervix was ascertained before placement of the transfer catheter. A ultrasoft catheter (Laboratoire CCD, Paris, France) was used in all patients of both groups.
In case group where ultrasound guidance was used, the catheter was advanced so that the tip was approximately 1.5cm from the uterine fundus and the embryo(s) were slowly released. In control group where the clinical touch method was used, the catheter was inserted through the cervical canal and the embryos were released according to the clinician's feeling as to the position of the catheter.
In both groups, the catheter was carefully removed after a period of 10s. Then it was checked under a stereomicroscope to ensure that all embryos had been transferred. After transfer, the patient was transferred to the recovery room and allowed to rest in the supine position with her legs slightly elevated for 30min following the procedure.
The difficulty of the replacement was determined by the following criteria:1)easy, for embryos were placed without effort using a catheter 2)difficult, transfers performed using a catheter but requiring the use of a tenaculum and cervical dilators.
Clinical pregnancy was defined as the presence of at least one gestational sac by ultrasound examination. An ongoing pregnancy was defined as the presence of at least one fetus with positive heart pulsations seen with ultrasound examination beyond the first trimester of pregnancy. Implantation rate was determined as the total number of gestational sacs with fetal heart beat seen on ultrasound examination in relation to the total number of embryos transferred. Also, the incidence of miscarriage was noted.
Statistical analysis
SPSS 13 for Windows Statistical Package was used for statistical analysis. Continuous variables were compared by Student's t-test if they were normally distributed. The Mann-Whitney U-test was used where the data were skewed. Differences in proportions were analyzed with X2-test or Fisher's exact test as appropriate. p<0.05 was considered statistically significant.
Results
A total of 180 women who underwent embryo transfer in our Center were recruited into the study. All of them had fresh embryo transfer. The characteristics of the women are summarized in Table I. There were no differences in the age, duration and etiology of infertility and the number of embryo transferred between the Ultrasound-guided and clinical touch groups. The percentages of IVF and ICSI were similar in both groups.
Table II shows the pregnancy outcomes of the 180 cycles. The Clinical pregnancy rate was 21.1 % in the ultrasound-guided group and 15.5 % in the clinical touch group. The difference was not statistically significant. The ongoing pregnancy rate was 18.9% in the ultrasound and 12.2% in the clinical group and again the difference was not statistically significant. The implantation rate in the ultrasound guided group was 11.1% while this was 7.2% in the clinical group and there was no significant difference. In addition, all of the embryos were singleton and no significant differences were observed between two groups in terms of miscarriage rate.
The difference of percentage of difficult embryo transfers was not significant in groups. This was 8.9% in the ultrasound-guided group and 13.3% in the clinical touch group (p-value=0.47).

Discussion
Since the introduction of ultrasound-guided embryo transfer during the mid-1980s, this technique has evolved into a more routine part of ART practices around the world (10, 11). Although studies have suggested that a significant improvement in pregnancy and implantation rates has been observed following the use of
transabdominal guidance during embryo transfer
(12-14), other studies have refused these observations (15, 16).
In our research, 180 patients have been recruited into the study: 90 in ultrasound-guided embryo transfer group and 90 in clinical touch group. The characteristics of the comparison groups were similar with respect to the age of the patients, the etiology of infertility, the number and quality of embryos transferred. Also, the number of oocytes was obtained from IVF or ICSI cycles were the same. Failure to demonstrate a significant difference in our implantation and clinical pregnancy rates may be a consequence of the small size of our population.
Some studies have showed that keeping an appropriate distance between the tip of the internal catheter and the fundus of the uterus is an important point for a successful embryo transfer (17, 18).Kojima et al (2001) reported that the distance of 1.5cm was more suitable than 1cm and significantly improved the clinical pregnancy rate (17); whereas Rosenlund et al (1996) have found no relationship between the site of embryo deposition in the uterus and pregnancy outcome (19).In our study, although the tip of the catheter was positioned with the use of ultrasound at 1.5 cm from the fundus of the uterine cavity, there was no significant increase in pregnancy or implantation rate.The use of ultrasound guidance has been shown to decrease the incidence of difficult transfers (6, 20), but this finding is not consistent in all prospective studies (12).
Our results were in agreement with other studies that ET using ultrasound not only improved pregnancy outcome but also the use of ultrasound has been associated with easy transfers (7- 9, 21).
Conclusion
While more recent studies have been encouraging regarding the use of ultrasound-assisted embryo transfer, the value of experience in the clinical touch method can not be discounted. A large prospective study in our population would be necessary for definitive ascertainment of the value of routine simultaneous ultrasound monitoring during embryo transfer.
Type of Study: Original Article |
References
1. Edwards RG. Clinical approaches to increasing uterine receptivity during human implantation. Human Reprod 1995; 10:60-66. [DOI:10.1093/humrep/10.suppl_2.60]
2. Al-Shawaf T, Dave R, Harper J, Linehan D, Riley P, Craft I. Transfer of embryos into the uterus: How much do technical factors affect pregnancy rates? J Assist Reprod Genet 1993; 10:31-36. [DOI:10.1007/BF01204437]
3. Woolcott R, Stanger J. Potentially important variables identified by transvaginal ultrasound-guided embryo transfer. Hum Reprod 1997; 12:963-636. [DOI:10.1093/humrep/12.5.963]
4. Coroleu B, Carreras O, Veiga A, Martell A, Martinez F, Belil I, et al. Embryo transfer under ultrasound guidance improves pregnancy rates in in-vitro fertilization. Hum Reprod 2000; 15:616-620.Coroleu B, Barri PN, Carreras O, Martínez F, Parriego M, Hereter L, et al. The influence of the depth of embryo replacement into the uterine cavity on implantation rates after IVF: a controlled, ultrasound-guided study. Hum Reprod 2002; 17:341-346. [DOI:10.1093/humrep/17.2.341]
5. Matorras R, Urquijo E, Mendoza R, Corcostegui B, Exposito A, Rodriguez-Escudero FJ. Ultrasound-guided embryo transfer improved pregnancy rates and increases the frequency of easy transfer. Hum Reprod 2002; 17:1762-1766. [DOI:10.1093/humrep/17.7.1762]
6. Kan AKS, Abdalla HI, Gafar AH, Nappi L, Ogunyemi BO, Thomas A, et al. Embryo transfer: Ultrasound-guided versus clinical touch. Hum Reprod 1999; 14:1259-1261. [DOI:10.1093/humrep/14.5.1259]
7. Coroleu B, Barri PN, Carreras O, Martinez F, Veiga A, Balasch J. The usefulness of ultrasound guidance in frozen-thawed embryo transfer: A prospective randomized clinical trial. Hum Reprod 2002; 17:2885-2890. [DOI:10.1093/humrep/17.11.2885]
8. Garcia-Velasco JA, Isaza Vv, Martinez-Salazar J, Landazabal A, Requena A, Remhoi J et al. Transabdominal ultrasound-guided embryo transfer does not increase pregnancy rate in oocyte recipients. Fertili Steril.2002; 78:534-539. [DOI:10.1016/S0015-0282(02)03249-1]
9. Strickler RC, Christianson C, Crane JP, Curato A, Knight AB, Yang V. Ultrasound guidance for human embryo transfer. Fertil Steril 1985; 43:54-61. [DOI:10.1016/S0015-0282(16)48317-2]
10. Leong M, Leung C, Tucker M, Wong C, Chan H. Ultrasound-assisted embryo transfer. J In vitro Fert Emb Tranf 1986; 3:383-385. [DOI:10.1007/BF01133254]
11. Tang OS, Ng EH, So WW, Ho PC. Ultrasound-guided embryo transfer: a prospective randomized controlled trial. Hum Reprod 2001; 16:2310-2315. [DOI:10.1093/humrep/16.11.2310]
12. Li R, Lu L, Hao G, Zhong k, Cai Z, Wang W. Abdominal ultrasound-guided embryo transfer improves clinical pregnancy rates after in vitro fertilization: experiences from 330 clinical investigations. J Assist Reprod Genet 2005; 22:3-8. [DOI:10.1007/s10815-005-0813-0]
13. Li R, Zhuang GL, Cai Zm, Wang H, Zhong K, Zhou WY. Clinical analysis of ultrasound-guided embryo transfer after in vitro fertilization. Zhonghua Fu Chan Ke Za Zhi 2004; 39:180-183.
14. de Camargo Martins AM, Baruffi RL, Mauri AL, Peterson C, Oliveira JB, Contart P, et al. Ultrasound guidance is not necessary during easy embryo transfers. J Assist Reprod Genet 2004; 21:421-425. [DOI:10.1007/s10815-004-8757-3]
15. Chen SC, Lai TH, Lee FK. The influence of abdominal ultrasound-guided embryo transfer on pregnancy rate: a preliminary report. Fertil Steril 2007; 87:1235-1237. [DOI:10.1016/j.fertnstert.2006.11.026]
16. Kojima K, Nomiyama M, Kumamoto T, Matsumoto Y, Iwasaka T. Transvaginal ultrasound-guided embryo transfer improves pregnancy and implantation rates after IVF. Hum Reprod 2001; 16:2578-2582. [DOI:10.1093/humrep/16.12.2578]
17. Shamonki MI, Spandorfer SD, Roberts JE, Rosenwaks Z. Ultrasound-guided embryo transfer: does it improve IVF success? Fertil Steril. 2003; 80:S127-128. [DOI:10.1016/S0015-0282(03)01212-3]
18. Rosenlund B, Sjoblom P, Hillensjo T. Pregnancy outcome related to the site of embryo deposition in the uterus. J Assist Reorod Genet 1996; 13:511-513. [DOI:10.1007/BF02066534]
19. Mirkin S, Jones EL, Mayer JF, Stadtmauer L, Gibbons WE, Oehninger S. Impact of transabdominal ultrasound guidance on performance and outcome of transcervical uterine embryo transfer. J Assist Reprod Genet 2003; 20:318-322. [DOI:10.1023/A:1024809607966]
20. Flisser E, Grifo JA, Kery LC, Noyes N. Transabdominal ultrasound-assisted embryo transfer and pregnancy outcome. Fertil Steril 2006; 85:353-357. [DOI:10.1016/j.fertnstert.2005.08.015]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




