Sat, Feb 21, 2026
[Archive]
Volume 5, Issue 5 (7-2007)
IJRM 2007, 5(5): 191-194 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aali B S, Abdollahi H, Nakhaee N, Davazdahemami Z, Mehdizadeh A. The association of preterm labor with vaginal colonization of group B streptococci. IJRM 2007; 5 (5) :191-194
URL: http://ijrm.ir/article-1-86-en.html
URL: http://ijrm.ir/article-1-86-en.html
Bibi Shahnaz Aali *1 
 , Hamid Abdollahi2
, Hamid Abdollahi2 
 , Nouzar Nakhaee3
, Nouzar Nakhaee3 
 , Zohreh Davazdahemami3
, Zohreh Davazdahemami3 
 , Anahita Mehdizadeh4
, Anahita Mehdizadeh4 


 , Hamid Abdollahi2
, Hamid Abdollahi2 
 , Nouzar Nakhaee3
, Nouzar Nakhaee3 
 , Zohreh Davazdahemami3
, Zohreh Davazdahemami3 
 , Anahita Mehdizadeh4
, Anahita Mehdizadeh4 

1- Departmentn of Obstetrics and Gynecology, Physiology Research Center, Kerman University of Medical Sciences, kerman, Iran , shahnaz.aali@gmail.com
2- Department of Microbiology, Kerman University of Medical sciences
3- Kerman University of Medical sciences, Kerman, Iran
4- Departmant of Genetics, Isfahan University, Isfahan, Iran
2- Department of Microbiology, Kerman University of Medical sciences
3- Kerman University of Medical sciences, Kerman, Iran
4- Departmant of Genetics, Isfahan University, Isfahan, Iran
Full-Text [PDF 92 kb]
(842 Downloads)
| Abstract (HTML) (2884 Views)
Full-Text: (419 Views)
Introduction
Preterm delivery is a relatively common condition in obstetrics. It comprises 7% of all deliveries, but accounts for more than 80% of perinatal morbidity (1). Recently, the association of maternal GBS colonization with preterm labor has become a subject of controversy. In 1996, the Centers for Disease Control and Prevention, accounted preterm delivery as a risk factor for group B streptococcal sepsis and recommended
the use of prophylactic antibiotic in preterm labor (2) . Regan et al (1996) found that women heavily colonized with GBS at the time of
delivery were more likely to deliver prematurely (3). Feikin et al (2001) study also indicated an association between GBS colonization at delivery and preterm birth (4). On the contrary, other investigators reported no association between preterm labor and cervicovaginal GBS colonization (5, 6). The prevalence of maternal colonization varies in countries owing to socioeconomic and ethnic differences (3-6). As the contribution of GBS to preterm labor may also be influenced by ethnicity and geographic variations, we performed the present study to assess the association between preterm labor and GBS vaginal colonization in women attending Afzalipour Maternity Center, Kerman, Iran. This center is the main referral maternity center of Kerman Medical University and admits patients from all over the province of Kerman, which is located in southeast of Iran with a hot and dry climate.
Materials and methods
During a year from April 2005 to May 2006, 101 women with preterm labor and 105 patients randomly admitted for delivery at a gestational age of 38-40 weeks entered this case- control study. Preterm labor was considered as the occurrence of four uterine contractions in a 20 minutes time period plus cervical dilatation greater than 1 cm and cervical effacement of 80% or more before 37 weeks of gestational age based on the last menstrual period or ultrasonographic report in the first half of pregnancy. Multifetal pregnancy, previous preterm delivery, underlying disease, uterine anomaly, placenta previa, current antibiotic usage, rupture of membranes ≥ 6 hours were excluded. Demographic and obstetric data was gathered for each patient. All participants gave written informed consent. Samples were collected from the upper thirds of vagina and cultured on blood and chocolate agar plates (Merck, Germany), and then incubated in 5- 10% carbon dioxide at 37ºC for 24 hours.
The small round bacterial colonies with almost flat surface (discoid like) on blood agar were regarded as β hemolytic and group B streptococcus at first stage. Further differential tests including Gram stain, Bacitracin, SXT, VP, CAMP and hipurate hydrolysis were performed on each isolate. Additional confirmation was carried out by using a specific test for GBS, MASTSTREP (agglutination tests from Mast Company, UK). Data were analyzed using SPSS software (version 15). Student`s t test, Chi square test were used to compare continuous and categorical data between cases and controls. Using multivariate logistic regression the associations between selected characteristics and preterm labor were analyzed. The Hosmer–Lemeshow test was used to assess model fit. P-values<0.05 were considered as significant.
Results
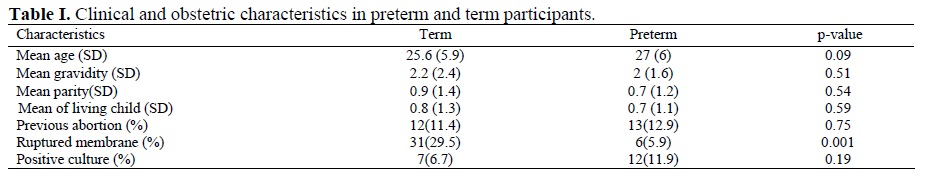
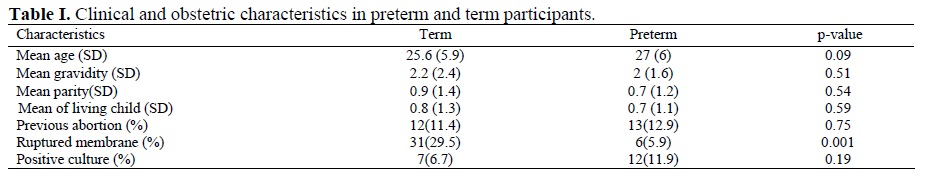
The majority of women in both groups were young (mean age: 26.3 years) and had low parity (mean: 0.8). The groups were comparable regarding age, gravidity and other obstetric parameters (Table I). No difference in socioeconomic and ethnic status was expected, as all patients attended a public center.
The frequency of positive cultures was calculated to be 9.2% in the entire study population. Although a greater number of preterm patients (11.9%) in comparison to the term group (6.7%) revealed positive culture for GBS, the difference was not statistically significant (Table I). Age revealed a significant association with preterm labor (Table II). Besides, as it is shown in Table 2 the odds of preterm labor was roughly associated with GBS culture positivity (OR: 2.96, 95%CI: 0.96-9.17). No case of neonatal sepsis was developed during the study period.
Discussion
Researchers have shown that the risk of early onset sepsis in colonized neonates is increased in case of prolonged membrane rupture, maternal signs of infection, amnionitis, intrapartum fetal monitoring, or if the baby has a low birth weight or is born preterm (8). As intrapartum fetal monitoring is not used in our center and cases with prolonged membrane rupture were excluded, lack of neonatal sepsis was not a surprising finding.
In the present study older women were more at risk of preterm labor. This can be due to more frequent conditions for contamination
these women experience over time. On the other hand, gravidity and parity showed no significant association with preterm labor while Tsolia et al (1998) indicated that multiparity was associated with a lower colonization rate (5). This inconsistency is related to the socioeconomic differences in the population studied.
Preterm delivery is a relatively common condition in obstetrics. It comprises 7% of all deliveries, but accounts for more than 80% of perinatal morbidity (1). Recently, the association of maternal GBS colonization with preterm labor has become a subject of controversy. In 1996, the Centers for Disease Control and Prevention, accounted preterm delivery as a risk factor for group B streptococcal sepsis and recommended
the use of prophylactic antibiotic in preterm labor (2) . Regan et al (1996) found that women heavily colonized with GBS at the time of
delivery were more likely to deliver prematurely (3). Feikin et al (2001) study also indicated an association between GBS colonization at delivery and preterm birth (4). On the contrary, other investigators reported no association between preterm labor and cervicovaginal GBS colonization (5, 6). The prevalence of maternal colonization varies in countries owing to socioeconomic and ethnic differences (3-6). As the contribution of GBS to preterm labor may also be influenced by ethnicity and geographic variations, we performed the present study to assess the association between preterm labor and GBS vaginal colonization in women attending Afzalipour Maternity Center, Kerman, Iran. This center is the main referral maternity center of Kerman Medical University and admits patients from all over the province of Kerman, which is located in southeast of Iran with a hot and dry climate.
Materials and methods
During a year from April 2005 to May 2006, 101 women with preterm labor and 105 patients randomly admitted for delivery at a gestational age of 38-40 weeks entered this case- control study. Preterm labor was considered as the occurrence of four uterine contractions in a 20 minutes time period plus cervical dilatation greater than 1 cm and cervical effacement of 80% or more before 37 weeks of gestational age based on the last menstrual period or ultrasonographic report in the first half of pregnancy. Multifetal pregnancy, previous preterm delivery, underlying disease, uterine anomaly, placenta previa, current antibiotic usage, rupture of membranes ≥ 6 hours were excluded. Demographic and obstetric data was gathered for each patient. All participants gave written informed consent. Samples were collected from the upper thirds of vagina and cultured on blood and chocolate agar plates (Merck, Germany), and then incubated in 5- 10% carbon dioxide at 37ºC for 24 hours.
The small round bacterial colonies with almost flat surface (discoid like) on blood agar were regarded as β hemolytic and group B streptococcus at first stage. Further differential tests including Gram stain, Bacitracin, SXT, VP, CAMP and hipurate hydrolysis were performed on each isolate. Additional confirmation was carried out by using a specific test for GBS, MASTSTREP (agglutination tests from Mast Company, UK). Data were analyzed using SPSS software (version 15). Student`s t test, Chi square test were used to compare continuous and categorical data between cases and controls. Using multivariate logistic regression the associations between selected characteristics and preterm labor were analyzed. The Hosmer–Lemeshow test was used to assess model fit. P-values<0.05 were considered as significant.
Results
The majority of women in both groups were young (mean age: 26.3 years) and had low parity (mean: 0.8). The groups were comparable regarding age, gravidity and other obstetric parameters (Table I). No difference in socioeconomic and ethnic status was expected, as all patients attended a public center.
The frequency of positive cultures was calculated to be 9.2% in the entire study population. Although a greater number of preterm patients (11.9%) in comparison to the term group (6.7%) revealed positive culture for GBS, the difference was not statistically significant (Table I). Age revealed a significant association with preterm labor (Table II). Besides, as it is shown in Table 2 the odds of preterm labor was roughly associated with GBS culture positivity (OR: 2.96, 95%CI: 0.96-9.17). No case of neonatal sepsis was developed during the study period.
Discussion
Maternal colonization rate was calculated to be 9.2% in our study. Reported GBS colonization rates in the world are quite variable, but generally range from 6 to 30% (5,7,8). The differences in colonization rates depend on the particular population and especially on the laboratory methods used to identify GBS (9). The additional tests performed in our study may account for the lower frequency of colonization in our population in comparison to other developing countries (10).
In Nomura et al (2006) study, Colonization rate for women with preterm premature rupture of membranes was 30% (9). However, 21.1% of our study population who presented with ruptured membrane revealed positive culture for GBS. This difference can best be explained by the geographical variation of GBS colonization. No significant difference was found in colonization between term and preterm patients on admission in our study that corroborates Kubota's findings (6). However, based on multivariate logistic regression, GBS positive women were nearly three times more likely to suffer from preterm labor than negative ones which is consistent with other studies (3, 4). The p-value for this odds ratio was almost significant, and worth considering. In contrast, Tsolia et al (2003) found no association between prematurity and GBS colonization (5).Researchers have shown that the risk of early onset sepsis in colonized neonates is increased in case of prolonged membrane rupture, maternal signs of infection, amnionitis, intrapartum fetal monitoring, or if the baby has a low birth weight or is born preterm (8). As intrapartum fetal monitoring is not used in our center and cases with prolonged membrane rupture were excluded, lack of neonatal sepsis was not a surprising finding.
In the present study older women were more at risk of preterm labor. This can be due to more frequent conditions for contamination
these women experience over time. On the other hand, gravidity and parity showed no significant association with preterm labor while Tsolia et al (1998) indicated that multiparity was associated with a lower colonization rate (5). This inconsistency is related to the socioeconomic differences in the population studied.
Although the colonization rate of GBS is relatively low in our center, it can be regarded as a risk factor for preterm labor. Therefore, Prophylactic antibiotic therapy should be considered in these patients. Older women are more susceptible to be colonized with this microorganism. More investigations are required to confirm the association of age and colonization rate.

This project was funded by Research Council of Kerman University of Medical Sciences. Authors extend their gratitude to the council members for their valuable advice.

Acknowledgement
This project was funded by Research Council of Kerman University of Medical Sciences. Authors extend their gratitude to the council members for their valuable advice.
Type of Study: Original Article |
References
1. Holst E, Goffeng AR, Andersch B. Bacterial vaginosis and vaginal microorganisms in idiopathic premature labor and association with pregnancy outcome. Clin Microbiol 1994; 32:176-186.
2. Centers for Disease Control and Prevention: Prevention of perinatal group B streptococci disease. Revised guidelines from the CDC. MMWR 51(RR-11):1, 2002d.
3. Regan JA, Klebanoff MA, Nugent RP, Eschenbach DA, Blachwelder WC, Lou Y, et al . Colonization with group B streptococci in pregnancy and adverse outcome. Am J Obstet Gynecol 1996; 174:1354-1360. [DOI:10.1016/S0002-9378(96)70684-1]
4. Feikin DR, Thorsen P, Zywicki S, Arpi M, Westergaard JG, Schuchat A. Association between colonization with group B streptococci during pregnancy and preterm delivery among Danish women. Am J Obstet Gynecol 2001; 184:427-433. [DOI:10.1067/mob.2001.109936]
5. Tsolia M, Psoma M, Gavrili S, Petrochilou V, Michalas S, Legakis N, et al. Group B streptococcus colonization of Greek pregnant women and neonates:prevalence, risk factors and serotypes. Clin Microbiol Infect 2003; 9:832-838. [DOI:10.1046/j.1469-0691.2003.00662.x]
6. Kubota T. Relationship between maternal group B streptococcal colonization and pregnancy outcome. Obstet Gynecol 1998; 92:926-930. [DOI:10.1016/S0029-7844(98)00309-3]
7. Amin A, Abdulrazzaq YM, Uduman S. Group B streptococcal serotype distribution of isolates from colonized pregnant women at the time of delivery in United Arab Emirates. J Infect 2002; 45:42-46. [DOI:10.1053/jinf.2001.0990]
8. Benitz WE, Gould JB, Druzin ML. Risk factors for early-onset group B streptococcal sepsis: estimation of odds ratios by critical literature review. Pediatrics 1999; 103:77. [DOI:10.1542/peds.103.6.e77]
9. Nomura ML, Passini Júnior R, Oliveira UM. Selective versus non - selective culture medium for group B streptococcus detection in pregnancies complicated by preterm labor or preterm-premature rupture of memberance. Braz J Infect Dis 2006; 10:247-250. [DOI:10.1590/S1413-86702006000400006]
10. Stoll BJ, Schuchat A. Maternal carriage of group B streptococci in developing countries. Pediatr Infect Dis 1998;17:499-503. [DOI:10.1097/00006454-199806000-00013]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


