Sat, Apr 20, 2024
[Archive]
Volume 5, Issue 5 (7-2007)
IJRM 2007, 5(5): 183-186 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hosseini M –, Gharehkhani P, Sadeghi M. Association of inherited thrombophilia and antiphospholipid syndrome with severe preeclampsia. IJRM 2007; 5 (5) :183-186
URL: http://ijrm.ir/article-1-89-en.html
URL: http://ijrm.ir/article-1-89-en.html
1- Department of Gynecology and Obstetrics, Shaheed Beheshti University of Medical Sciences, Tehran, Iran , hoseiny339@yahoo.com
2- Department of Gynecology and Obstetrics, Shaheed Beheshti University of Medical Sciences, Tehran, Iran
2- Department of Gynecology and Obstetrics, Shaheed Beheshti University of Medical Sciences, Tehran, Iran
Keywords: Severe preeclampsia, Factor V leiden, Protein C, Protein S, Antithrombin III, Lupus anticoagulant antibody, Anticardiolipin IgG and IgM.
Full-Text [PDF 98 kb]
(539 Downloads)
| Abstract (HTML) (2766 Views)
Full-Text: (343 Views)
Introduction
Despite many advances achieved in obstetrics and gynecology during the recent decades, severe preeclampsia remains one the most common concerns that complicates approximately 5% of all pregnancies. It is often distressing for the patient and frustrating for the physician (1). Although its etiology has been a matter of continuing debate, vascular endothelial inflammation and dysfunction have been proposed as the main etiologic factors (1).
Unfortunately, severe preeclampsia is not a preventable illness and delivery is the only definitive treatment (1-3). Severe preeclampsia is frequently associated with preterm delivery and its subsequent complications; however, it could cause seizure, blindness, renal ischemia, hepatic rupture, or even death in mother (1-3). Therefore, determining the etiologic factors of severe preeclampsia is one of the most important priorities of gynecologists. Inherited disorders of hemostasis and antiphospholipid syndrome have been postulated by prior investigators as common causes (4-6), however, controversies have aroused about their actual mechanisms. Some have demonstrated a significant association between severe preeclampsia and antiphospholipid syndrome (7,8), while others failed to show any association (9,10). The present study was designed to evaluate the association between severe preeclampsia and inherited disorders of hemostasis and antiphospholipid syndrome in a group of Iranian patients referring to a referral center for Gynecology and Obstetrics in Tehran.
Materials and methods
For this case-control study from April 2002 to March 2003, 26 females with severe preeclampsia were matched with 26 healthy parturients as controls. Severe preeclampsia was defined as diastolic blood pressure ≥110mmHg, severe proteinuria (+2) as well as other signs and symptoms including headache, blurred vision, epigastric pain, oliguria, thrombocytopenia, elevated liver enzymes, intrauterine growth retardation, and pulmonary edema (1). Parturients referring to the same hospital (similar socioeconomic status) who did not meet the diagnostic criteria of severe preeclampsia were matched according to the age, gestational age, parity, and previous history of abortion with the cases. A similar questionnaire was completed for all subjects.
Meanwhile, 10cc peripheral blood samples were obtained and indices of inherited disorders of hemostasis such as factor V Leiden, protein C, protein S, and antithrombin III (AT III) as well as antiphospholipid syndrome ie, lupus anticoagulant antibody, and anticardiolipin antibody (IgM and IgG) were determined. The normal range of the abovementioned indices were considered as follow: factor V Leiden: >120pg/l, anticardiolipin IgM<7pg/l and IgG<10pg/l, protein C: 70-130pg/l, protein S: 65-140pg/l, and AT III: 80-120pg/l. Lupus anticoagulant antibody was considered either positive or negative. All subjects were requested to fill an informed consent. T-test, Mann-Whitney U-test, chi square, and Fisher's exact test were used for data analysis, when appropriate.
In case of significant association, odd's ratio of index with severe preeclampsia was calculated with 95% confidence interval. A p-value of less than 0.05 was considered to be statistically significant.
Results
The study population included 26 cases with the mean (± standard deviation) age of 27.6±7.6 years, mean gestational age of 33.9±5.4 months, and mean parity of 1.8±1.3 as well as 26 controls with mean age, gestational age and parity of 24.5±4.7, 36.8±3.5 and 1.4±1.2, respectively. There was no significant difference (NS) between the two groups in any of the aforementioned variables.The mean value of factor V Leiden in the control group was 137.3±20.0pg/l as compared to 138.8±22.7pg/l in the severe preeclamptic patients (NS). Table 1 outlines the frequency of positive subjects in different indices of inherited disorders of hemostasis. As shown, factor V Leiden was found abnormally high just in one parturient with severe preeclampsia.
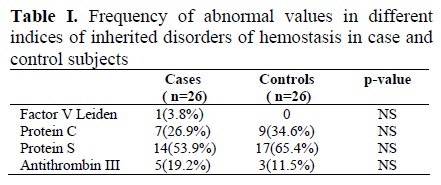
Fisher's exact test did not reveal a significant association between factor V Leiden and severe preeclampsia. The mean value of protein C and S were 107.6±32.6 and 60.6±14.5pg/l in preeclamptic patients, while these values were 118.8±26.1 and 58.0±17.1pg/l in controls, respectively, and t-test revealed insignificant differences between the two groups. Of 26 cases, 7(26.9%) and 14(53.9%) had abnormal values of protein C and S, respectively, however, the differences with the control subjects (34.6% and 65.4%) were not statistically significant (table 1). Similarly, the antithrombin III level did not differ between case and control subjects (97.4±16 vs. 99.0±11.7pg/l). The mean of anticardiolipin-IgM value was 4.48±2.69pg/l in severe preeclamptic parturients as compared to 3.27±2.0pg/l in controls (p<0.001). IgM>4pg/l was found in 2 (7.7%) non-preeclamptic (controls) and 7(27.9%) severe preeclamptic parturients that showed a statistical significant difference (p<0.05). Indeed, severe preeclamptic parturients were 4.4 times more likely to develop elevated levels of IgM (OR=4.4, 95%CI=1.9-10). The mean of anticardiolipin-IgG value was 6.04±9.6pg/l in cases and 4.88±2.8pg/l in controls (NS). Abnormally elevated IgG level was reported in one severe preeclamptic female (3.8%) as compared with 4 (15.4%) controls (NS). Finally, lupus anticoagulant antibody was similarly detected in one case and one control. Figure 1 represents the distribution of anticardiolipin-IgM in severe preeclamptic and non-preeclamptic subjects. As shown, controls are more likely to have low IgM levels.

Discussion
Results have revealed that indices of inherited disorders of hemostasis including factor V Leiden, antithrombin III, protein C, and protein S as well as anticardiolipin-IgG and lupus anticoagulant antibody were not associated with severe preeclampsia, however, anticardiolipin-IgM was found more frequently in severe preeclamptic subjects. Although anticardiolipin-IgM was reported within the normal range in both groups (<7pg/l), preeclamptic parturients were more frequently found to have IgM>4pg/l than non- preeclamptic subjects, thus, preeclamptic patients are more likely to develop elevated level of IgM. Decreased Antithrombin III, inherited as autosomal dominant traits, is associated with a 70-90% increased risk of thrombosis (11, 12), however, several studies failed to address its role in severe preeclampsia (13-15).
Deficiency of protein C has been documented in approximately 0.2% of the general population and may be manifested as decreased antigenic factors or dysfunctional proteins. Deficiency of protein S has similar prevalence but could also produce symptoms because of decreased free protein level (16, 17). Dekker and colleagues (1995) have reported deficiencies of protein C and S in less than 1% and 25% of severe early-onset preeclamptic parturients, respectively (14), however, this association was not supported in other studies (13, 18). Similarly, there are some controversies around the role of factor V Leiden in preeclampsia. Dizon-Townson et al (1996) reported predisposition to severe preeclampsia in females with mutation in factor V Leiden, whereas others disagreed these findings (19, 20). Prior investigators have also demonstrated an increased risk of preeclampsia in the presence of antiphospholipid syndrome and anticardiolipin-IgM and -IgG antibodies (19, 21-23). They have reported an odd's ratio of 6.2 in their studies, whereas, more recent studies failed to show this association (24, 25). These controversies in different studies could be explained in part by different methodological approaches or the fact that preeclampsia is a multifactorial disorder. Nevertheless, sample size imparts an important role in interpretation of the results.
Our study has some potential weaknesses. Like previous studies of the same design, there was a risk of a selection bias and recall bias as well. Our sample size was quite small; however, we may address matched controls, similar socioeconomic status and our study protocol as the strong points of this study. In conclusion, the present case control study reveals a modest association between anticardiolipin-IgM antibody and development of severe preeclampsia; however, routine screening tests for indices of inherited disorders of hemostasis are not recommended due to the high expenses and shortness of their association with preeclampsia. Finally, we believe cohort studies may shed further insight into the mechanisms of preeclampsia.
Despite many advances achieved in obstetrics and gynecology during the recent decades, severe preeclampsia remains one the most common concerns that complicates approximately 5% of all pregnancies. It is often distressing for the patient and frustrating for the physician (1). Although its etiology has been a matter of continuing debate, vascular endothelial inflammation and dysfunction have been proposed as the main etiologic factors (1).
Unfortunately, severe preeclampsia is not a preventable illness and delivery is the only definitive treatment (1-3). Severe preeclampsia is frequently associated with preterm delivery and its subsequent complications; however, it could cause seizure, blindness, renal ischemia, hepatic rupture, or even death in mother (1-3). Therefore, determining the etiologic factors of severe preeclampsia is one of the most important priorities of gynecologists. Inherited disorders of hemostasis and antiphospholipid syndrome have been postulated by prior investigators as common causes (4-6), however, controversies have aroused about their actual mechanisms. Some have demonstrated a significant association between severe preeclampsia and antiphospholipid syndrome (7,8), while others failed to show any association (9,10). The present study was designed to evaluate the association between severe preeclampsia and inherited disorders of hemostasis and antiphospholipid syndrome in a group of Iranian patients referring to a referral center for Gynecology and Obstetrics in Tehran.
Materials and methods
For this case-control study from April 2002 to March 2003, 26 females with severe preeclampsia were matched with 26 healthy parturients as controls. Severe preeclampsia was defined as diastolic blood pressure ≥110mmHg, severe proteinuria (+2) as well as other signs and symptoms including headache, blurred vision, epigastric pain, oliguria, thrombocytopenia, elevated liver enzymes, intrauterine growth retardation, and pulmonary edema (1). Parturients referring to the same hospital (similar socioeconomic status) who did not meet the diagnostic criteria of severe preeclampsia were matched according to the age, gestational age, parity, and previous history of abortion with the cases. A similar questionnaire was completed for all subjects.
Meanwhile, 10cc peripheral blood samples were obtained and indices of inherited disorders of hemostasis such as factor V Leiden, protein C, protein S, and antithrombin III (AT III) as well as antiphospholipid syndrome ie, lupus anticoagulant antibody, and anticardiolipin antibody (IgM and IgG) were determined. The normal range of the abovementioned indices were considered as follow: factor V Leiden: >120pg/l, anticardiolipin IgM<7pg/l and IgG<10pg/l, protein C: 70-130pg/l, protein S: 65-140pg/l, and AT III: 80-120pg/l. Lupus anticoagulant antibody was considered either positive or negative. All subjects were requested to fill an informed consent. T-test, Mann-Whitney U-test, chi square, and Fisher's exact test were used for data analysis, when appropriate.
In case of significant association, odd's ratio of index with severe preeclampsia was calculated with 95% confidence interval. A p-value of less than 0.05 was considered to be statistically significant.
Results
The study population included 26 cases with the mean (± standard deviation) age of 27.6±7.6 years, mean gestational age of 33.9±5.4 months, and mean parity of 1.8±1.3 as well as 26 controls with mean age, gestational age and parity of 24.5±4.7, 36.8±3.5 and 1.4±1.2, respectively. There was no significant difference (NS) between the two groups in any of the aforementioned variables.The mean value of factor V Leiden in the control group was 137.3±20.0pg/l as compared to 138.8±22.7pg/l in the severe preeclamptic patients (NS). Table 1 outlines the frequency of positive subjects in different indices of inherited disorders of hemostasis. As shown, factor V Leiden was found abnormally high just in one parturient with severe preeclampsia.
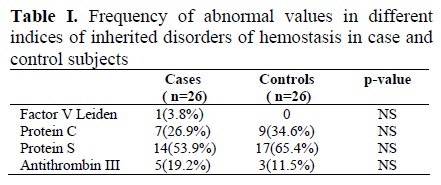
Fisher's exact test did not reveal a significant association between factor V Leiden and severe preeclampsia. The mean value of protein C and S were 107.6±32.6 and 60.6±14.5pg/l in preeclamptic patients, while these values were 118.8±26.1 and 58.0±17.1pg/l in controls, respectively, and t-test revealed insignificant differences between the two groups. Of 26 cases, 7(26.9%) and 14(53.9%) had abnormal values of protein C and S, respectively, however, the differences with the control subjects (34.6% and 65.4%) were not statistically significant (table 1). Similarly, the antithrombin III level did not differ between case and control subjects (97.4±16 vs. 99.0±11.7pg/l). The mean of anticardiolipin-IgM value was 4.48±2.69pg/l in severe preeclamptic parturients as compared to 3.27±2.0pg/l in controls (p<0.001). IgM>4pg/l was found in 2 (7.7%) non-preeclamptic (controls) and 7(27.9%) severe preeclamptic parturients that showed a statistical significant difference (p<0.05). Indeed, severe preeclamptic parturients were 4.4 times more likely to develop elevated levels of IgM (OR=4.4, 95%CI=1.9-10). The mean of anticardiolipin-IgG value was 6.04±9.6pg/l in cases and 4.88±2.8pg/l in controls (NS). Abnormally elevated IgG level was reported in one severe preeclamptic female (3.8%) as compared with 4 (15.4%) controls (NS). Finally, lupus anticoagulant antibody was similarly detected in one case and one control. Figure 1 represents the distribution of anticardiolipin-IgM in severe preeclamptic and non-preeclamptic subjects. As shown, controls are more likely to have low IgM levels.

Discussion
Results have revealed that indices of inherited disorders of hemostasis including factor V Leiden, antithrombin III, protein C, and protein S as well as anticardiolipin-IgG and lupus anticoagulant antibody were not associated with severe preeclampsia, however, anticardiolipin-IgM was found more frequently in severe preeclamptic subjects. Although anticardiolipin-IgM was reported within the normal range in both groups (<7pg/l), preeclamptic parturients were more frequently found to have IgM>4pg/l than non- preeclamptic subjects, thus, preeclamptic patients are more likely to develop elevated level of IgM. Decreased Antithrombin III, inherited as autosomal dominant traits, is associated with a 70-90% increased risk of thrombosis (11, 12), however, several studies failed to address its role in severe preeclampsia (13-15).
Deficiency of protein C has been documented in approximately 0.2% of the general population and may be manifested as decreased antigenic factors or dysfunctional proteins. Deficiency of protein S has similar prevalence but could also produce symptoms because of decreased free protein level (16, 17). Dekker and colleagues (1995) have reported deficiencies of protein C and S in less than 1% and 25% of severe early-onset preeclamptic parturients, respectively (14), however, this association was not supported in other studies (13, 18). Similarly, there are some controversies around the role of factor V Leiden in preeclampsia. Dizon-Townson et al (1996) reported predisposition to severe preeclampsia in females with mutation in factor V Leiden, whereas others disagreed these findings (19, 20). Prior investigators have also demonstrated an increased risk of preeclampsia in the presence of antiphospholipid syndrome and anticardiolipin-IgM and -IgG antibodies (19, 21-23). They have reported an odd's ratio of 6.2 in their studies, whereas, more recent studies failed to show this association (24, 25). These controversies in different studies could be explained in part by different methodological approaches or the fact that preeclampsia is a multifactorial disorder. Nevertheless, sample size imparts an important role in interpretation of the results.
Our study has some potential weaknesses. Like previous studies of the same design, there was a risk of a selection bias and recall bias as well. Our sample size was quite small; however, we may address matched controls, similar socioeconomic status and our study protocol as the strong points of this study. In conclusion, the present case control study reveals a modest association between anticardiolipin-IgM antibody and development of severe preeclampsia; however, routine screening tests for indices of inherited disorders of hemostasis are not recommended due to the high expenses and shortness of their association with preeclampsia. Finally, we believe cohort studies may shed further insight into the mechanisms of preeclampsia.
Type of Study: Original Article |
References
1. Cunninghum F, Gray, Gart Norman F, Leveno, Kenneth. J.Williams obstetrics. 21 ed. MCGRAW-HIL; 2002: 568-588.
2. Cherry and Merkatz's. Complication of pregnancy.5th Ed wayne R.Cohen; 2000: 208-210.
3. Abramovici Dorl, Sibai Baham. High Risk pregnancy 4th Edition. Joho.T.Queenan; 1999: 369-375.
4. Branch DW, Andres R, Digre KB, Rote NS, Scott JR. The association of antiphospholipid antibodies with severe pre-eclampsia. Obstet Gynecol 1989; 73: 541-545.
5. Allen JY, Tapia-Santiago C, Kutteh WH. Antiphospholipid antibodies in patients with pre-eclampsia. Am J Reprod Immunol 1996; 36: 81-85. [DOI:10.1111/j.1600-0897.1996.tb00143.x]
6. Alsulyman OM, Castro MA, Zuckerman E, MC Gehee W, Gooedwin TM. Preeclampsia and liver infarction in early pregnancy associated with the antiphospholipid syndrome. Obstet Gyncol 1996; 88(4 pt2): 644-646. [DOI:10.1016/0029-7844(96)00098-1]
7. Cetin M, Gucer S, Serin IS, Eser B, Toyyar M, Una LA. Activated protein C resistance in Turkish women with severe pre-eclampsia. Gynecol Obstet Invest 2001; 52:168-172. [DOI:10.1159/000052967]
8. Benedettoc, Marziol, salton L, Maula V, ChieppaG, Massobrio M. Factor V Leiden and factor II G 20210 A in preeclamspia and Hellp syndrome. Acta Obstect Gynecol Scand 2002; 81: 1095-1100. [DOI:10.1034/j.1600-0412.2002.811201.x]
9. Riyazi N, Leeda M, Devries JT, Huijgens PC, Van Geijn HP, Dekker GA. Low-molecular-weigh heparin in pregnant women with thrombophilia and a history of pre-eclampia or fetal growth restriction, a preliminary study. Obstect Gynaecol 2001; 97: 44-48.
10. Bernard N, Giguere Y. Genetics of pre-eclampsia: What are the challengens? Obstect Gynaecol 2003; 25: 578-585. [DOI:10.1016/S1701-2163(16)31017-9]
11. Girling J, de Swiet M. Inherited thrombophilia and pregnancy. Curr Opin Obtect Gynocol 1998; 10:135-144. [DOI:10.1097/00001703-199804000-00010]
12. Cavenagh JD, Colurin BT, Guide lines for the management of thrombophilia. Postgrde Med J 1996; 72:87-94. [DOI:10.1136/pgmj.72.844.87]
13. Kup ferminc MJ, Eldor A, steinman N, Many A, Bar-AM, Jaffa A, et al. Increased frequency of genetic thrombophilia in woman with complications of pregnancy. N EngL Med 1999; 340: 9-13. [DOI:10.1056/NEJM199901073400102]
14. Dekker GA, de Vires JI, Doelitezsch PM, Huijgens PC, Von Blomberg BM, Jacobs C, et al. underlying disorders associated with severe early-onset pre-eclapsia. AMJ Obstet Gynecol 1995; 173:1042-1048. [DOI:10.1016/0002-9378(95)91324-6]
15. Simmonds RE, Zoller B, Ireland H, Thompson E, de Frustos PG, Dahlback B. Genetic and phenotypic analysis of a large (122-member) protein S-deficient kindred proides an explanation for the familial coexistence of type I and type III plasma phenotypes. Blood 1997; 89:4364-4370.
16. Zoller B, Garcia de Frutos P, Dahlback B. Evaluation of the relationship between protein S and C 4b-binding protein isoforms in hereditary protein S deficiency demonstrating type I and type III deficiencies to be phenotypic variants of the same genetic disease. Blood 1995; 85:3524-3531.
17. Arais F, Romereo R, Joist H, Kravs FT. Thrombophilia a mechanism of disease in women with adverse pregnancy outcome and thrombotic lesions in placenta, Matern Fetal Med 1998; 7:277-286. [DOI:10.3109/14767059809020459]
18. De Vries JI, Dekker GA, Huijgens PC, Jakobs C, Blombers BM, Van Geijn HP. Hyperhomocysteinemia and protein S deficiency in- Complicated pregnancies. Br J Obstet Gynaecol 1997; 104:1248-1254. [DOI:10.1111/j.1471-0528.1997.tb10970.x]
19. Van Pampus MG, Dekker GA, Wolf H, Huijgens PC, Koopman MM, Von Blomberg BM, et al, High prevalence of hemostatic abnormalities in women with a history of severe preeclampsia. Am J Obstet Gynecol 1999; 180:1146-1150. [DOI:10.1016/S0002-9378(99)70608-3]
20. Dizon-Townson DS, Nelson LM, Easton K, Ward K. The facto V Leiden mutation may predispose women to severe preeclampsia. Am J Obstet Gnecol 1996; 175:902-905. [DOI:10.1016/S0002-9378(96)80022-6]
21. Oshiro BT, Silver RM, Scott JR, Yu H, Branch DW. Antiphospholipid antibodies and fetal death. Obstet Gnecol 1996; 87:489-493. [DOI:10.1016/0029-7844(95)00498-X]
22. Rai RS, Clifford K, Cohen H, Regan L. High prospective fetal loss rate in untreated pregnancies of women with recurrent miscarriage and antiphospholipid antiobodies. Hum Reprod 1995; 10-3301-3304. [DOI:10.1093/oxfordjournals.humrep.a135907]
23. Allen JY, Tapia-Santiago C, Kutteh WH. Annti-phospholipid antibodies in patients with preeclampsia. Am J Reprod Immuno 1996; 36:81-85. [DOI:10.1111/j.1600-0897.1996.tb00143.x]
24. Schei B,Ostensen M, Moen T, Jacobsen G, Bakketeig LS. Can maternal antiphospholipid antibodies predict the birth of a small-for-gestational age child? Acta Obs Gyn Scand 1995; 74:425-428. [DOI:10.3109/00016349509024403]
25. D'anna R, Scilipoti A, Leonardi J, Scuderi M, Jasonni VM, leonardi R. Anticardiolipin antibodies in preeclamsia and intrauterine growth restriction. Clin Exp Obstet Gynecol 1997; 24: 135-137.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




