Fri, Apr 26, 2024
[Archive]
Volume 6, Issue 2 (7-2008)
IJRM 2008, 6(2): 25-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hoque M, Hoque E, Kader S B. Pregnancy complications of grandmultiparity at a rural setting of South Africa. IJRM 2008; 6 (2) :25-0
URL: http://ijrm.ir/article-1-97-en.html
URL: http://ijrm.ir/article-1-97-en.html
1- Medical Manager, Empangeni Hospital, KwaZulu-Natal, New Germany 3610, South Africa , monjurul.hoque@kznhealth.gov.za
2- Lecturer, Statistician, Mangosuthu University of Technology, Jacobs, 4026, South Africa
3- Hospital Manager,Wentworth Hospital, Private Bag JACOBS, 4026, South Afric
2- Lecturer, Statistician, Mangosuthu University of Technology, Jacobs, 4026, South Africa
3- Hospital Manager,Wentworth Hospital, Private Bag JACOBS, 4026, South Afric
Full-Text [PDF 45 kb]
(555 Downloads)
| Abstract (HTML) (2261 Views)
Full-Text: (297 Views)
Introduction
The pregnancy complications are highly related to parity and continue to be of interest to obstetricians (1). Pregnancies in grandmultiparae have been considered risky for many decades (2). Grandmultiparity is associated with low-socio economic status and education, poor prenatal care and more previous intra-uterine and perinatal deaths (3). Intrapartam complications such as foetal malpresentation, placental abruption, dysfunctional labour, and postpartum haemorrhage are commonly linked to grandmultiparity (1, 4-7). In developed countries, grandmultiparity is becoming rare (3–4% of all pregnancies) but in developing countries it is higher and considered a public health problem (8). Studies from developed countries have reported minor risks or even fewer complications during antenatal and labour. Obstetric complications have been independently associated with progressive maternal age, yet most studies of grandmultipartity have failed to consider this potentially confounding effect in their analysis (8-10). The definition of grandmultiparity also varies from study to study and it remains unclear how the differing definitions contribute to the different observations. Some authors have considered grandmultipara to be women who gave birth after five or more previous deliveries and others considered women who have seven children and some used the definition of parity grater or equal to five (4-7). The International Federation of Gynecology and Obstetrics (1993) define grandmultiparity as delivery of the fifth or more infant. In South Africa (SA) grandmultiparity is defined when a pregnant woman have six or more previous births and considered risk pregnancy, therefore antenatal care should be provided at the community health centre but delivery should be conducted at hospital (11).
Several retrospective studies have found increased complication rates, such as gestational hypertension and diabetes, premature labour, perinatal mortality and intrauterine fetal death (12-15). The authors of these studies have argued that the grandmultiparas advanced maternal age thus might distort these findings. A study conducted in United Kingdom (Re:union: Hospital) found that grandmultipara had more previous intrauterine and perinatal deaths and had fewer intrapartum complications (16). Another study from Malaysia found that grandmultiparas women were significantly at risk of preterm and low-birth-weight deliveries (17). A recent study reported that young grandmultiparas were more likely to have preterm deliveries, and less likely to experience foetal distress, instrumental delivery and any intrapartum complication than young nulliparas. Young grandmultiparas were less likely to experience many complications than their older counterparts (18).
Some decades ago, the hazards of high parity in relation to maternal morbidity and mortality were viewed with genuine fear and respect. It is shown from recent studies, that in present-day obstetrics, maternal mortality is not increased among grandmultiparas. In most developed countries the incidence of grandmultiparity has decreased in recent years where family planning played a great role and high parity is not considered a risk marker for pregnancy complications (1, 19). Moreover, obstetrical care has improved considerably and the use of advanced electronic and biochemical foetal monitoring as well as intrauterine pressure measurement has greatly improved the possibility of safer obstetrical management of grandmultiparas. In the developing countries and many parts of Africa and sub-Saharan Africa, there is limited access to medical care and therefore, the need to identify women whose pregnancies are at risk of complication, is an important part of antenatal screening and care during delivery. There are few studies from sub-Saharan Africa and particularly in SA that address risk of grandmultiparity as independent of pregnancy complications. The objectives of this study were to evaluate the complications during pregnancy and delivery (labour) of grandmultiparas (refers to 6 or more previous deliveries after 28 weeks of gestation) and to compare with other parity groups (parity between 1–5 and nulliparas women).
Setting and population
Empangeni Hospital is situated in the Uthungulu health district (one of the 11 districts) in the province of KwaZulu-Natal and covers the residence of over 450 000 people who are mainly rural, black and speak the local language (isiZulu). It is a 256 bedded maternity hospital and provides obstetric, gynaecological and neonatal health services to its population and is a referral centre for 14 rural clinics for all aspects of maternal and infant care. There are two private hospitals run mainly by private specialists and there are over 40 general practitioners’ services based mainly at urban areas. Antenatal care and care during confinement are performed in the district according to the national protocol and guidelines (11).
Definition
Preterm delivery was considered when mothers delivered a new born baby at 28 weeks (or above 1000 gm baby) up to 36 weeks of gestational age. Whereas, the term delivery was considered between 37 to 41 weeks of gestation. Any delivery that occurred at 42 weeks or more gestation age was considered post term delivery.
Intrauterine foetal deaths referred to the birth of a dead fetus weighting more than 1000 gm or after 28 weeks of gestational age.
Prevalence of anaemia was considered as the percentage of women who had haemoglobin level < 10 gm/dL in accordance with the national definition of anaemia in pregnancy, measured at term (between 36–40 weeks) pregnancy or at the time of delivery if not done (11).
Statistical analysis
Data was collected on Microsoft Excel 2003 spreadsheet program and thereafter imported to SPSS 11.5 for window version for analysis. Pearson chi-square test was used to find the association (at 5% level of significance) among variables. Multivariate logistic regression analysis was undertaken to determine whether grandmultiparity was a risk factor for the outcome variables when other variables were included in a model with confounding variables. Prior permission was obtained from the hospital management for utilizing delivery data from maternity register to conduct the study.
Results
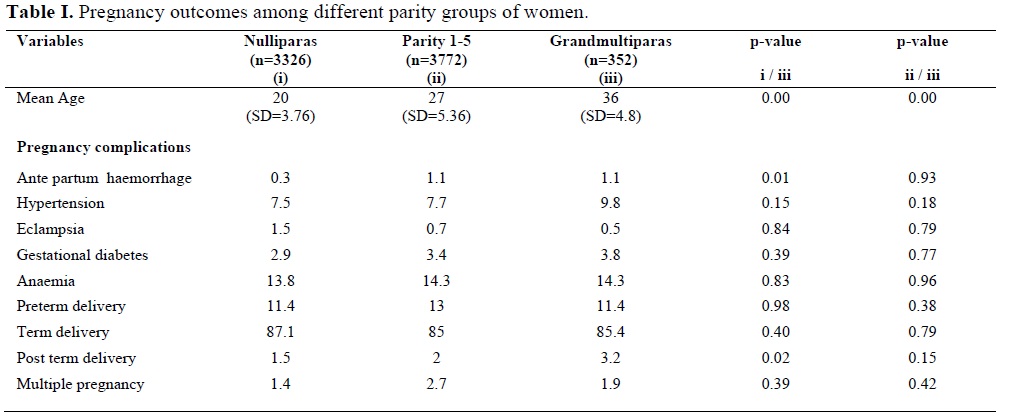
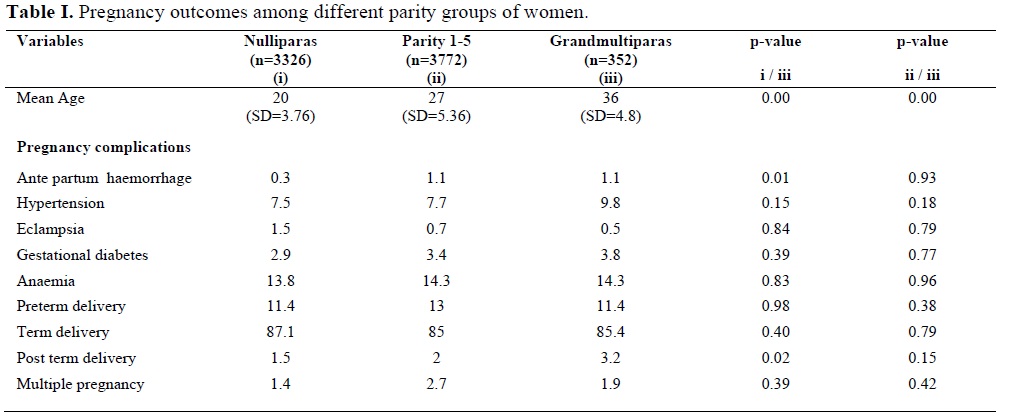
A total of 7836 deliveries were recorded in Empangeni Hospital between April and December 2004. Of them, 386 had missing parity thus excluded from the study. Among them 3326 (45%) were nulliparous, 3772 (50%) had parity between 1 and 5 and 352 (5%) were grandpultiparas women. The mean ages among the groups were significantly different as shown in Table I.
Grandpultiparas women were significantly older than women with lower parity. The antenatal medical disorders in grandmultiparas such as prevalence of anaemia (14.3%), gestational hypertension (9.8%), diabetes (3.8%) and eclampsia (0.5%) were not significantly different compared to nulliparas and multiparas (parity between 1 and 5).
Grandpultiparas women were significantly more likely to have ante partum haemorrhage than nulliparous women. But there were no differences in gestational age (preterm and term delivery rates), caesarean (14.2%) or emergency caesarean (9.8%) delivery and multiple pregnancy (1.9%) rates among three different parity groups.
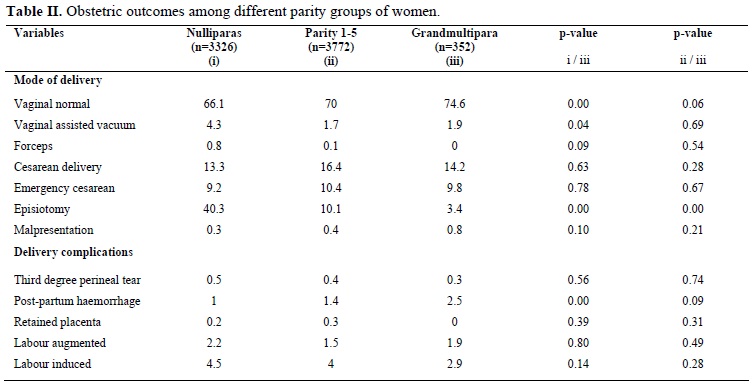
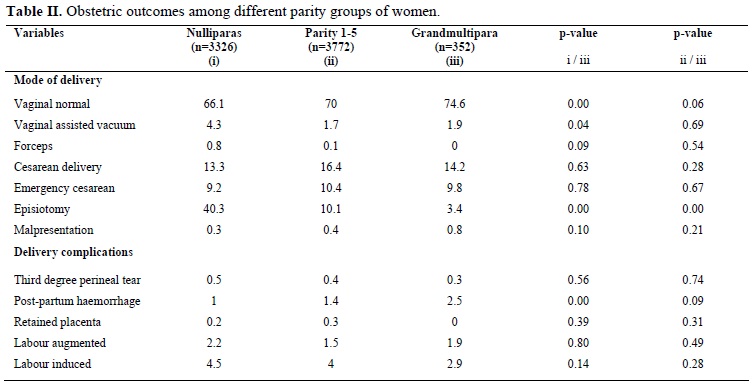
Post term delivery (3.2%) and normal vaginal delivery (75%) rates were significantly higher (p < 0.05) in grandpultiparas women compared to nulliparous women but no significant difference with parity 1-5 group. Assisted vaginal delivery rates (vacuum and forceps) were significantly lower in grandpultiparas women compared to nulliparous group (p < 0.05) but similar rate for parity 1-5 group. A significantly lower rate of episiotomy was given to grandpultiparas women (3.4%) during labour compared to other groups (40.3% in nulliparous and 10.1% in parity group 1-5).
Intrapartum complications most commonly thought to be associated with grandmultiparity were not significantly different e.g., incidence of malpresentation, third degree perineal tear, retained placenta, induction and augmentation of labour.
A significantly higher rate of post partum haemorrhage was observed in grandpultiparas women (2.5%) compared to nulliparous women (1%) but there was no difference with parity 1-5 group (1.4%).
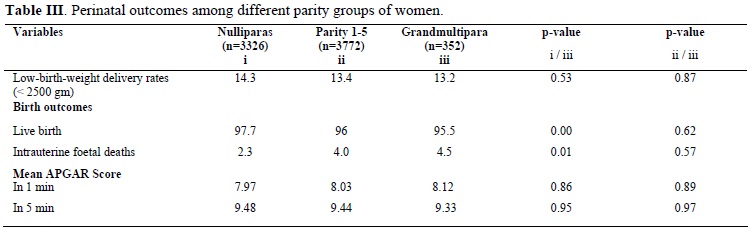
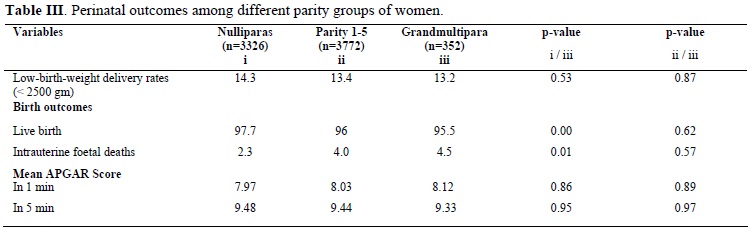
Perinatal outcomes in different parity groups are shown in Table III. There were no differences in the rates of low-birth-weight delivery, and mean APGAR scores of newborns in 1 and 5 minutes among different parity groups.
Live birth rate for grandpultiparas women (95.5%) was significantly lower (p<0.05) and intrauterine foetal death rate was significantly higher than nulliparous but these had no difference with other parity groups. Multivariate logistic regression analysis showed that grandmultiparity was not a risk factor for preterm birth, intrauterine foetal deaths, low birth weight and ante partum haemorrhage (Table IV).

Discussion
This study is of interest because of this tropical sub-Saharan region’s social characteristics, where a high prevalence of grandmaultiparity (5%) co-exist with free, standard level of care during antenatal and time of delivery (11). The mean ages of grandmultiparity are significantly higher in this population and are similar to other studies (3, 8). Women who had previously delivered six or more babies had shown higher rates of post-term deliveries and intrapartum foetal deaths compared to nulliparous women but similar to women who had previous deliveries between 1–5. Thus our study confirmed the findings of other studies which were conducted among women of higher socio-economic backgrounds and equal access to medical care in the other countries (1, 6). However, these were not a prerequisite for favorable results as it was also reported from other studies that highly favorable outcomes in women with lower socio-economic status (4, 20). The study conducted matching for age and socio-economic status and found that higher parity groups had their own risk factors, but the rates of some complications were decreased with higher parity (19). Therefore our study added weight to the overall view that in our modern health care
setting, grandmultiparity was associated with a significantly increased risk of complications and pregnancy outcome compared to lower parity. Although it had shown that there was a higher rate of normal vaginal and lower rate of assisted (vacuum, forceps, episiotomy) deliveries in grandmultipararous compared to nulliparous women. This was likely as grandmultiparas women had well developed birth canal and previously experienced the delivery process.
Higher rate of caesarean deliveries were expected in grandpultiparas women due to their previous caesarean deliveries from previous pregnancies. Decision of caesarean delivery was undertaken on the basis of obstetric reasons only. The standard protocol in Empangeni Hospital is that pregnant women with two or more previous caesarean delivery would have elective caesarean delivery done at subsequent pregnancy or pregnancies at term (between 37 and 38 weeks of gestation) besides other obstetric causes. However, the rates of elective and emergency caesarean delivery rates were similar in all parity groups. The conventional belief is that grandpultiparas women would have fully matured physically, the size of the bony pelvis might have had fully developed and had experienced consequences of previous pregnancies and deliveries thus did not require extra induction, augmentation of labour and assistance during delivery such as episiotomy, forceps or vacuum. It is also known and possible that pregnancy enhances the growth of the bony pelvis (21).
One would therefore expect that given the same foetal size, teenage mothers should have a higher instrumental and caesarean delivery rate, but this is disproved by our findings. It has been shown that longitudinal growth can occur during pregnancy in the teenager, therefore the increment is being greater in the nulliparas compared with the multiparas. Our results on medical complications such as incidence of anaemia, hypertension, diabetes, antepartum haemorrhage and emergency cesarean section were at similar rate among different parity groups. Earlier studies had indicated that there was no difference in the outcome of grandpultiparas pregnancies if adequate antenatal care was available (1, 5).
All pregnant women received standard level and types of antenatal care and services during labour as prescribed by national policy and guidelines in South Africa (11). In this study, we have compared grandpultiparas women with nulliparas (primigravida) and other parity (1 – 5) groups. Similarly, as in previous studies, grandmultiparity was not a risk factor for preterm delivery (8, 20, 22). In studies where ages of different parity groups are adjusted with same ages, grandmultiparity appear to have fewer intrapartum complications but had more previous intrauterine and perinatal deaths (3). When young grandmultiparas are compared with same age of nulliparas and multiparas they showed similar level of intrapartum and new born complications (18). However, the distribution of known risk factors for preterm delivery (such as alcohol consumption, smoking, socio-economic status etc.) among different parity groups were not known thus was the limitation of this study (23, 24).
The preterm delivery rates among the groups were high and comparable with other findings (16). But post term delivery rates were significantly higher in grandmultiparas women. Obstetric and perinatal complications are associated with post term delivery (25). An increased incidence of perinatal deaths observed (particularly intrauterine foetal deaths) in grandpultiparas women compared to nulliparous could be related to the significant difference in parity (>=6 parity vs. 0) but no difference with other group (parity 1–5). However, this difference in parity could not be the only explanation for the significant difference in perinatal deaths (1.9% vs. 0.7%). It can be related to high rate of post term deliveries as indicated as a risk factor for increased perinatal deaths (25). These events were in fact nearly three times more frequent in grandpultiparas women compared to nulliparas women (25). A large retrospective study showed that women with high parity, regardless of age, had an odds ratio of 1.8 for foetal death compared with women having a second or third child (23). Another prospective study found an increased rate of intrauterine foetal deaths in 382 grandmuliparous as compared with multiparous controls (26). Bai et al also found significantly higher perinatal deaths in a large grandpultiparas cohort (>17500 women) after adjustment for age, smoking and private health insurance status (2).
This was a facility-based retrospective study with limited variables for the study (variable present in labour ward register were used in the analysis). However, most of the important indicators of pregnancy, obstetric and perinatal complications and outcomes were measured and compared to come to a conclusion for grandmultiparity. Most (over 95%) of the institutional deliveries in the district are conducted in Empangeni Hospital and it was previously recorded that more than 95% of deliveries in rural district occur at health facilities (9, 27). Therefore, there was no reason to believe that, women with problems or no problem during pregnancy would come for hospital delivery. Therefore, we can assume that women who delivered at Empangeni Hospital are representative of the pregnant population of the communities of Uthungulu health district and the true reflection for pregnancy complications of grandmultiparity.
Conclusion
Grandmultiparity was not safer compared to other lower parity groups. Thus strategies are needed to guide women to seek proper care during pregnancy and if possible to avoid pregnancy in cases of grandmultiparas women.
Acknowledgement
The authors wish to acknowledge the contributions made by the professional nurses maintaining the hospital register and Empangeni Hospital management team for supporting the study.
The pregnancy complications are highly related to parity and continue to be of interest to obstetricians (1). Pregnancies in grandmultiparae have been considered risky for many decades (2). Grandmultiparity is associated with low-socio economic status and education, poor prenatal care and more previous intra-uterine and perinatal deaths (3). Intrapartam complications such as foetal malpresentation, placental abruption, dysfunctional labour, and postpartum haemorrhage are commonly linked to grandmultiparity (1, 4-7). In developed countries, grandmultiparity is becoming rare (3–4% of all pregnancies) but in developing countries it is higher and considered a public health problem (8). Studies from developed countries have reported minor risks or even fewer complications during antenatal and labour. Obstetric complications have been independently associated with progressive maternal age, yet most studies of grandmultipartity have failed to consider this potentially confounding effect in their analysis (8-10). The definition of grandmultiparity also varies from study to study and it remains unclear how the differing definitions contribute to the different observations. Some authors have considered grandmultipara to be women who gave birth after five or more previous deliveries and others considered women who have seven children and some used the definition of parity grater or equal to five (4-7). The International Federation of Gynecology and Obstetrics (1993) define grandmultiparity as delivery of the fifth or more infant. In South Africa (SA) grandmultiparity is defined when a pregnant woman have six or more previous births and considered risk pregnancy, therefore antenatal care should be provided at the community health centre but delivery should be conducted at hospital (11).
Several retrospective studies have found increased complication rates, such as gestational hypertension and diabetes, premature labour, perinatal mortality and intrauterine fetal death (12-15). The authors of these studies have argued that the grandmultiparas advanced maternal age thus might distort these findings. A study conducted in United Kingdom (Re:union: Hospital) found that grandmultipara had more previous intrauterine and perinatal deaths and had fewer intrapartum complications (16). Another study from Malaysia found that grandmultiparas women were significantly at risk of preterm and low-birth-weight deliveries (17). A recent study reported that young grandmultiparas were more likely to have preterm deliveries, and less likely to experience foetal distress, instrumental delivery and any intrapartum complication than young nulliparas. Young grandmultiparas were less likely to experience many complications than their older counterparts (18).
Some decades ago, the hazards of high parity in relation to maternal morbidity and mortality were viewed with genuine fear and respect. It is shown from recent studies, that in present-day obstetrics, maternal mortality is not increased among grandmultiparas. In most developed countries the incidence of grandmultiparity has decreased in recent years where family planning played a great role and high parity is not considered a risk marker for pregnancy complications (1, 19). Moreover, obstetrical care has improved considerably and the use of advanced electronic and biochemical foetal monitoring as well as intrauterine pressure measurement has greatly improved the possibility of safer obstetrical management of grandmultiparas. In the developing countries and many parts of Africa and sub-Saharan Africa, there is limited access to medical care and therefore, the need to identify women whose pregnancies are at risk of complication, is an important part of antenatal screening and care during delivery. There are few studies from sub-Saharan Africa and particularly in SA that address risk of grandmultiparity as independent of pregnancy complications. The objectives of this study were to evaluate the complications during pregnancy and delivery (labour) of grandmultiparas (refers to 6 or more previous deliveries after 28 weeks of gestation) and to compare with other parity groups (parity between 1–5 and nulliparas women).
Materials and methods
Setting and population
Empangeni Hospital is situated in the Uthungulu health district (one of the 11 districts) in the province of KwaZulu-Natal and covers the residence of over 450 000 people who are mainly rural, black and speak the local language (isiZulu). It is a 256 bedded maternity hospital and provides obstetric, gynaecological and neonatal health services to its population and is a referral centre for 14 rural clinics for all aspects of maternal and infant care. There are two private hospitals run mainly by private specialists and there are over 40 general practitioners’ services based mainly at urban areas. Antenatal care and care during confinement are performed in the district according to the national protocol and guidelines (11).
Study design and data collection
A retrospective case control study was conducted targeting all women delivered at Empangeni Hospital from April to December 2004. The cases in this study were 352 grandmultiparity women (who had 6 or more previous deliveries) and were compared with 3326 nulliparous women (had no experience of previous delivery) and 3772 women who had 1–5 previous deliveries. Abortions were excluded from previous deliveries. Data were collected from the labour ward maternity register. The register was the only official record of deliveries and recorded demographic (name, age, address of mothers), antenatal care information and complications of pregnancy (e.g. anaemia, gestational hypertension and diabetes, ante partum haemorrhage, eclampsia), obstetric, labour and perinatal information. The attending midwives recorded this information. All midwives working at labour ward are oriented and received in-service training on filling labour ward register and completing monthly summary presentation at weekly perinatal mortality meeting. The variables included in the study were anaemia, pregnancy induced hypertension, gestational diabetes, malpresentation, pre-eclampsia (defined as a diastolic blood pressure > 90 mm of Hg and + protein in urine for more than one occasion), dysfunctional labour (defined as oxytocin augmentation in active phase of labour), postpartum haemorrhage (blood loss >500ml after delivery), operative and assistive deliveries. Standard definitions were used for diagnosis of pregnancy, obstetric and intrapartum conditions.Definition
Preterm delivery was considered when mothers delivered a new born baby at 28 weeks (or above 1000 gm baby) up to 36 weeks of gestational age. Whereas, the term delivery was considered between 37 to 41 weeks of gestation. Any delivery that occurred at 42 weeks or more gestation age was considered post term delivery.
Intrauterine foetal deaths referred to the birth of a dead fetus weighting more than 1000 gm or after 28 weeks of gestational age.
Prevalence of anaemia was considered as the percentage of women who had haemoglobin level < 10 gm/dL in accordance with the national definition of anaemia in pregnancy, measured at term (between 36–40 weeks) pregnancy or at the time of delivery if not done (11).
Statistical analysis
Data was collected on Microsoft Excel 2003 spreadsheet program and thereafter imported to SPSS 11.5 for window version for analysis. Pearson chi-square test was used to find the association (at 5% level of significance) among variables. Multivariate logistic regression analysis was undertaken to determine whether grandmultiparity was a risk factor for the outcome variables when other variables were included in a model with confounding variables. Prior permission was obtained from the hospital management for utilizing delivery data from maternity register to conduct the study.
Results
A total of 7836 deliveries were recorded in Empangeni Hospital between April and December 2004. Of them, 386 had missing parity thus excluded from the study. Among them 3326 (45%) were nulliparous, 3772 (50%) had parity between 1 and 5 and 352 (5%) were grandpultiparas women. The mean ages among the groups were significantly different as shown in Table I.
Grandpultiparas women were significantly older than women with lower parity. The antenatal medical disorders in grandmultiparas such as prevalence of anaemia (14.3%), gestational hypertension (9.8%), diabetes (3.8%) and eclampsia (0.5%) were not significantly different compared to nulliparas and multiparas (parity between 1 and 5).
Grandpultiparas women were significantly more likely to have ante partum haemorrhage than nulliparous women. But there were no differences in gestational age (preterm and term delivery rates), caesarean (14.2%) or emergency caesarean (9.8%) delivery and multiple pregnancy (1.9%) rates among three different parity groups.
Post term delivery (3.2%) and normal vaginal delivery (75%) rates were significantly higher (p < 0.05) in grandpultiparas women compared to nulliparous women but no significant difference with parity 1-5 group. Assisted vaginal delivery rates (vacuum and forceps) were significantly lower in grandpultiparas women compared to nulliparous group (p < 0.05) but similar rate for parity 1-5 group. A significantly lower rate of episiotomy was given to grandpultiparas women (3.4%) during labour compared to other groups (40.3% in nulliparous and 10.1% in parity group 1-5).
Intrapartum complications most commonly thought to be associated with grandmultiparity were not significantly different e.g., incidence of malpresentation, third degree perineal tear, retained placenta, induction and augmentation of labour.
A significantly higher rate of post partum haemorrhage was observed in grandpultiparas women (2.5%) compared to nulliparous women (1%) but there was no difference with parity 1-5 group (1.4%).
Perinatal outcomes in different parity groups are shown in Table III. There were no differences in the rates of low-birth-weight delivery, and mean APGAR scores of newborns in 1 and 5 minutes among different parity groups.
Live birth rate for grandpultiparas women (95.5%) was significantly lower (p<0.05) and intrauterine foetal death rate was significantly higher than nulliparous but these had no difference with other parity groups. Multivariate logistic regression analysis showed that grandmultiparity was not a risk factor for preterm birth, intrauterine foetal deaths, low birth weight and ante partum haemorrhage (Table IV).

Discussion
This study is of interest because of this tropical sub-Saharan region’s social characteristics, where a high prevalence of grandmaultiparity (5%) co-exist with free, standard level of care during antenatal and time of delivery (11). The mean ages of grandmultiparity are significantly higher in this population and are similar to other studies (3, 8). Women who had previously delivered six or more babies had shown higher rates of post-term deliveries and intrapartum foetal deaths compared to nulliparous women but similar to women who had previous deliveries between 1–5. Thus our study confirmed the findings of other studies which were conducted among women of higher socio-economic backgrounds and equal access to medical care in the other countries (1, 6). However, these were not a prerequisite for favorable results as it was also reported from other studies that highly favorable outcomes in women with lower socio-economic status (4, 20). The study conducted matching for age and socio-economic status and found that higher parity groups had their own risk factors, but the rates of some complications were decreased with higher parity (19). Therefore our study added weight to the overall view that in our modern health care
setting, grandmultiparity was associated with a significantly increased risk of complications and pregnancy outcome compared to lower parity. Although it had shown that there was a higher rate of normal vaginal and lower rate of assisted (vacuum, forceps, episiotomy) deliveries in grandmultipararous compared to nulliparous women. This was likely as grandmultiparas women had well developed birth canal and previously experienced the delivery process.
Higher rate of caesarean deliveries were expected in grandpultiparas women due to their previous caesarean deliveries from previous pregnancies. Decision of caesarean delivery was undertaken on the basis of obstetric reasons only. The standard protocol in Empangeni Hospital is that pregnant women with two or more previous caesarean delivery would have elective caesarean delivery done at subsequent pregnancy or pregnancies at term (between 37 and 38 weeks of gestation) besides other obstetric causes. However, the rates of elective and emergency caesarean delivery rates were similar in all parity groups. The conventional belief is that grandpultiparas women would have fully matured physically, the size of the bony pelvis might have had fully developed and had experienced consequences of previous pregnancies and deliveries thus did not require extra induction, augmentation of labour and assistance during delivery such as episiotomy, forceps or vacuum. It is also known and possible that pregnancy enhances the growth of the bony pelvis (21).
One would therefore expect that given the same foetal size, teenage mothers should have a higher instrumental and caesarean delivery rate, but this is disproved by our findings. It has been shown that longitudinal growth can occur during pregnancy in the teenager, therefore the increment is being greater in the nulliparas compared with the multiparas. Our results on medical complications such as incidence of anaemia, hypertension, diabetes, antepartum haemorrhage and emergency cesarean section were at similar rate among different parity groups. Earlier studies had indicated that there was no difference in the outcome of grandpultiparas pregnancies if adequate antenatal care was available (1, 5).
All pregnant women received standard level and types of antenatal care and services during labour as prescribed by national policy and guidelines in South Africa (11). In this study, we have compared grandpultiparas women with nulliparas (primigravida) and other parity (1 – 5) groups. Similarly, as in previous studies, grandmultiparity was not a risk factor for preterm delivery (8, 20, 22). In studies where ages of different parity groups are adjusted with same ages, grandmultiparity appear to have fewer intrapartum complications but had more previous intrauterine and perinatal deaths (3). When young grandmultiparas are compared with same age of nulliparas and multiparas they showed similar level of intrapartum and new born complications (18). However, the distribution of known risk factors for preterm delivery (such as alcohol consumption, smoking, socio-economic status etc.) among different parity groups were not known thus was the limitation of this study (23, 24).
The preterm delivery rates among the groups were high and comparable with other findings (16). But post term delivery rates were significantly higher in grandmultiparas women. Obstetric and perinatal complications are associated with post term delivery (25). An increased incidence of perinatal deaths observed (particularly intrauterine foetal deaths) in grandpultiparas women compared to nulliparous could be related to the significant difference in parity (>=6 parity vs. 0) but no difference with other group (parity 1–5). However, this difference in parity could not be the only explanation for the significant difference in perinatal deaths (1.9% vs. 0.7%). It can be related to high rate of post term deliveries as indicated as a risk factor for increased perinatal deaths (25). These events were in fact nearly three times more frequent in grandpultiparas women compared to nulliparas women (25). A large retrospective study showed that women with high parity, regardless of age, had an odds ratio of 1.8 for foetal death compared with women having a second or third child (23). Another prospective study found an increased rate of intrauterine foetal deaths in 382 grandmuliparous as compared with multiparous controls (26). Bai et al also found significantly higher perinatal deaths in a large grandpultiparas cohort (>17500 women) after adjustment for age, smoking and private health insurance status (2).
This was a facility-based retrospective study with limited variables for the study (variable present in labour ward register were used in the analysis). However, most of the important indicators of pregnancy, obstetric and perinatal complications and outcomes were measured and compared to come to a conclusion for grandmultiparity. Most (over 95%) of the institutional deliveries in the district are conducted in Empangeni Hospital and it was previously recorded that more than 95% of deliveries in rural district occur at health facilities (9, 27). Therefore, there was no reason to believe that, women with problems or no problem during pregnancy would come for hospital delivery. Therefore, we can assume that women who delivered at Empangeni Hospital are representative of the pregnant population of the communities of Uthungulu health district and the true reflection for pregnancy complications of grandmultiparity.
Conclusion
Grandmultiparity was not safer compared to other lower parity groups. Thus strategies are needed to guide women to seek proper care during pregnancy and if possible to avoid pregnancy in cases of grandmultiparas women.
Acknowledgement
The authors wish to acknowledge the contributions made by the professional nurses maintaining the hospital register and Empangeni Hospital management team for supporting the study.
Type of Study: Original Article |
References
1. Eidelman AI, Kamar R, Schimmel MS, Baron E. The grand multipara: is she still at risk? Am J Obstet Gynecol 1998; 158: 389-392. [DOI:10.1016/0002-9378(88)90161-5]
2. Solomons B. The dangerous multipara. Lancet 1934; 2: 8-11. [DOI:10.1016/S0140-6736(00)90086-2]
3. Roman H, Robillard PY, Verspyck E, Hulsey TG, Marpeau L, Barau G. Obstetric and Neonatal Outcomes in Grand Multiparity. Am Obstet Gynecol 2004; 103: 1294- 1299. [DOI:10.1097/01.AOG.0000127426.95464.85]
4. King PA, Duthie SJ, Ma HK. Grandmultiparity: a reappraisal of risks. Int J Gynaecol Obstet 1994; 36: 13-16. [DOI:10.1016/0020-7292(91)90171-Z]
5. Seidman DS, Armor Y, Roff D, Stevenson DK, Gale R. Grandmultiparity: an obstetric or neonatal risk factors? Am J Obstet Gynecol 1988; 158: 1034 - 1039. [DOI:10.1016/0002-9378(88)90213-X]
6. Fuchs K, Peretz BA, Marcovic R, Timor-Tritsch I. The grandmultipara: is it a problem? A review of 5,785 cases. Int J Gynaecol Obstet 1985; 23: 321-325. [DOI:10.1016/0020-7292(85)90027-X]
7. Samueloff A, Mor-Yosef S, Seidman D, Rabinowitz R, Simon A, Schenker J. Grandmultiparity: a nationwide survey. Isr J Med Sci 1989; 25: 625-629.
8. Rizk DE, Khalfan M, Ezimokhai M. Obstetric outcome in the United Arab Emirates: a case control study. Arch Gynecol Obstet 2001; 264: 194-198. [DOI:10.1007/s004040000107]
9. Wilkinson D, Cutts F, Ntuli N, Abdul Karrim SS. Maternal and child health indicators in rural South African health district. S Afr Med J 1997; 87:456-459.
10. Lyrenas S. Labour in the grand multipara. Gynecol Obstet Invest 2002; 53: 6-12. [DOI:10.1159/000049403]
11. Department of Health. Guidelines for Maternity Care in South Africa - A manual for clinics, community health centers and district hospitals. Department of Health, Pretoria, 2002, 2nd Edition, ISBN 1- 875017:71-72.
12. Goldman GA, Kaplan B, Neri A, Hecht-Resnick R, Harel L, Ovadia J. The grand multipara. Eur J Obstet Gynecol Reprod Biol 1995; 61: 105-109. [DOI:10.1016/0301-2115(95)02108-J]
13. Tando TG, Bungum L. The grand multipara: maternal and neonatal complications. Acta Obstet Gynecol Acand 1987; 66:53-56. [DOI:10.3109/00016348709092954]
14. Mor-Yosef S, Seidman DS , Samueloff A, Schenker JG. The effects of the socioeconomic status on the perinatal outcome of grand multipara. Eur J Obstet Gynecol Reprod Biol 1990; 36:117-123. [DOI:10.1016/0028-2243(90)90057-8]
15. Abu-Heija AT, Chalabi HE. The great grandmultiparity: is it a risk? Int J Gynaecol Obstet 1997; 59: 213-216. [DOI:10.1016/S0020-7292(97)00198-7]
16. Roman H, Robillard PY, Verspyck E, Hulsey TC , Marpeau L, Barau G. Obstetric and neonatal outcomes in grandmultiparity. Obstet Gynecol 2004; 103: 1294-1299. [DOI:10.1097/01.AOG.0000127426.95464.85]
17. Tai C, Urquhart R. Grandmultiparity in Malaysian women. Asia Oceania J Obstet Gynaecol 1991; 17: 327-334. [DOI:10.1111/j.1447-0756.1991.tb00282.x]
18. Ellis Simonsen SM, Lyon JL, Alder SC, Varner MW. Effect of Grand Multiparity on Intrapartum and Newborn Complications in Young Women. Obstet Gynecol 2005; 106: 454 - 460. [DOI:10.1097/01.AOG.0000175839.46609.8e]
19. Babinzki A, Kerenyi T, Torok O, Grazi V, Lapinsky RH, Berkowitz RL. Perinatal outcome in grand and great-grandmultiparity: Effects of parity on obstetric risk factors. Am J Obstet Gynecol 1999; 181: 669 - 674. [DOI:10.1016/S0002-9378(99)70511-9]
20. Toohey JS, Keegan KA, Morgan MA, Francis J, Task S, de Veciana M. The dangerous multipara: fact or fiction? Am J Obstet Gynecol 1995; 172: 683 - 686. [DOI:10.1016/0002-9378(95)90593-6]
21. Scholl TO, Hediger ML, Ances IG, Cronk CE. Growth during early teenage pregnancies. Lancet 1988, 1: 710-711. [DOI:10.1016/S0140-6736(88)90205-X]
22. Bai J, Wong FM, Bauman A, Moshin M. Parity and pregnancy outcomes. Am J Obstet Gynecol 2002; 186: 274 - 278. [DOI:10.1067/mob.2002.119639]
23. Lundsberg LS, Bracken MB, Saftlas AF. Low-to-moderate gestational alcohol use and intrauterine growth retardation, low birth weight and preterm delivery. Ann Epidemiol 1997; 7: 498-508. [DOI:10.1016/S1047-2797(97)00081-1]
24. Fretts RG, Schmittdiel J, McLean FH, Usher RH, Goldman MB. Increased maternal age and the risk of fetal death. N Engl J Med 1995; 333: 953-957. [DOI:10.1056/NEJM199510123331501]
25. Olesen AW, Westergaard JG, Olsen J. Perinatal and maternal complications related to postterm delivery: A national register-based study, 1978-1993. Am J Obstet Gynecol 2003; 189: 222-227. [DOI:10.1067/mob.2003.446]
26. Bugg GJ, Atwal GS, Maresh M. Grandmultiparae in a modern setting. Br J Obstet Gynaecol 2002; 109: 249-253. [DOI:10.1111/j.1471-0528.2002.01058.x]
27. Tsoka JM, Le Seur D, Sharp BL. Maternal health services utilization in ubombo district. S Afr J Obs Gynae 2003; 9: 70 -73.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |