Fri, Feb 6, 2026
[Archive]
Volume 2, Issue 1 (7-2004)
IJRM 2004, 2(1): 9-11 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dehghani V A, Khalili M A, Zamani N, Dreh-Zereshki F. Comparison between Semen Parameters of Ejaculates Collected Via Masturbation Versus Coitus Interruptus. IJRM 2004; 2 (1) :9-11
URL: http://ijrm.ir/article-1-11-en.html
URL: http://ijrm.ir/article-1-11-en.html
Full-Text [PDF 25 kb]
(1482 Downloads)
| Abstract (HTML) (3866 Views)
Full-Text: (1058 Views)
Introduction
Normal semen is a mixture of motile and non-motile spermatozoa and viscous fluid. Therefore, proper collections and analysis of ejaculates must be undertaken by standard procedures in order to provide the valid information on the reproductive status of the individuals (Zavos 1986). In addition, with the advent of assisted reproductive techniques (ART), the standard collection of ejaculates along with manipulative techniques become more crucial for harvesting the maximum quality and quantity of spermatozoa for successful infertility treatment program (Lambard et al., 2004).
Various methods for semen collection have been employed for semen analysis or for ART program. These methods include masturbation, incomplete intercourse (coitus interruptus), and complete intercourse. WHO (1999) recommends collection of ejaculates via masturbation, and not with coitus interruptus. This is because the first portion of ejaculate, which contains the highest concentration of sperm may be lost at intercourse. Moreover, bacterial contamination of the sample and the acid PH of the vagina adversely affects the sperm quality. However, many patients prefer incomplete coitus as means of sperm collection in Islamic societies. Therefore, the objective of this investigation was to compare the semen characteristics in ejaculates of Iranian patients by means of masturbation and coitus interruptus by a 3 days interval.
Materials and Methods
Thirty men who were referred to the research and clinical center for infertility laboratory for andrological evaluation participated in this study. They were instructed to produce one semen specimen via masturbation and another one via incomplete intercourse by 3 days intervals. Each specimen was collected into a sterile, wide-mouthed container. Semen specimens were assessed according to the WHO standards for volume, viscosity, sperm concentration, progressive and non- progressive motility, normal morphology, and concentration of non-spermatozoal round cells. The semen samples used in this study were considered normozoospermic according to WHO guidelines (1999). Statistical analysis was performed using the student t-test and MC Nemar test. Differences were considered statistically significant when P<0.05.
Results
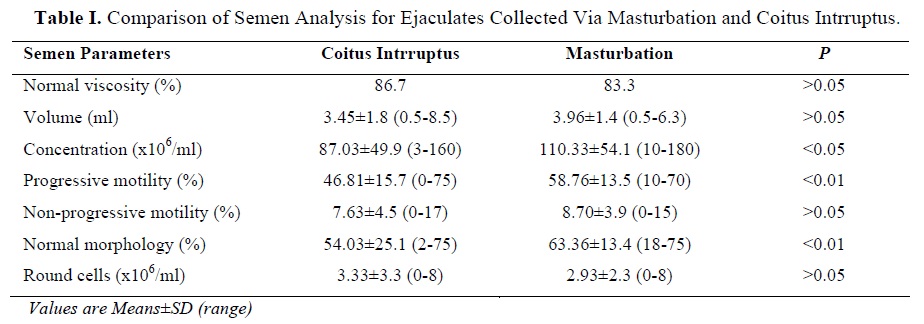
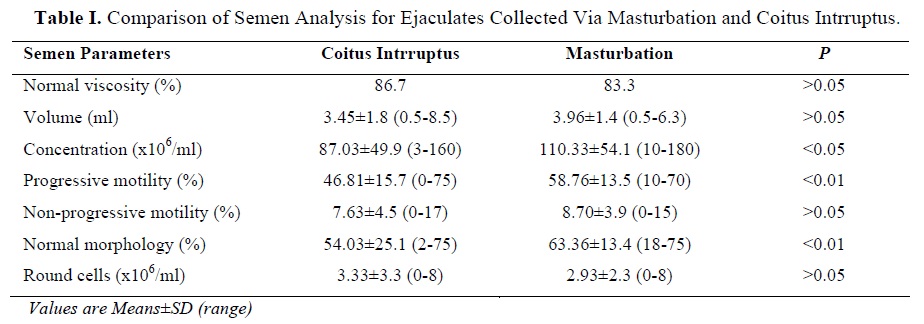
The results obtained from this study are reported in Table I. The sperm concentration from specimens collected via masturbation was significantly higher than coitus intrruptus ejaculates. Also, both progressive motility and normal morphology of
spermatozoa recovered via masturbation were qualitatively superior (P<0.01), compared with the ejaculates collected via interrupted intercourse. Furthermore, four samples were reported as severe oligospermia in coitus intrruptus group (2.5x106), which were improved to 11.2x106 when specimens were collected via masturbation.
Discussion
The most widely accepted method of semen collection for the purpose of semen analysis or ART is by means of masturbation (Sofikitis and Miyagawa 1993; WHO, 1999; Zavos 1986). The results from this study showed that collection of ejaculates via masturbation is more superior to coitus intrruptus. Collection of semen by means of masturbation resulted in reduction of non-spermatazoal round cell concentration, while the qualitative characteristics such as sperm concentration, progressive motility, and normal morphology were significantly enhanced when compared with results from incomplete coitus. The largest contributors to the round cell population are the immature germ cells followed by leukocytes which may indicate the presence of genital tract infections (Smith et al., 1989).
With ART advancements, the desire for using higher quality spermatozoa to achieve higher success rates has significantly increased (Lambard et al., 2004). Therefore, it seems that semen collection via coitus intrruptus should not be practiced for clinical purposes. The results clearly demonstrated that the aforementioned method of semen collection will alter the vital semen parameters which alternatively may result in reduction of fertilization and pregnancy rates.
Another important finding in our study was the fact that four cases were considered as severe oligozoospermia when ejaculates were collected with incomplete coitus. The samples were improved to a normal oligozoospermia when collections were done via masturbation. However, it should be emphasized that some patients in Iran due to psychological status or religious belief refuse to collect ejaculates via masturbation. For these subjects, Zarmakoupis and colleagues (1999) recommended to use a semen collection device at intercourse. These types of devices consist of a nonspermicidal condom that allows the patients to collect the ejaculates via the complete intercourse. The collected semen, as they assessed, contains high concentration of spermatozoa that have greater motility when compared with samples obtained via the coitus intrruptus method. (Zavos et al., 1994).
In conclusion, the generated results indicate that semen collection via coitus intrruptus is not recommended in infertility treatment programs. The method of choice for collection of high quality spermatozoa with low concentration of round cells is via masturbation. However, if patients refuse to employ the masturbation method, the ejaculates should be produced via the use of nonspermicidal condoms at intercourse.
Normal semen is a mixture of motile and non-motile spermatozoa and viscous fluid. Therefore, proper collections and analysis of ejaculates must be undertaken by standard procedures in order to provide the valid information on the reproductive status of the individuals (Zavos 1986). In addition, with the advent of assisted reproductive techniques (ART), the standard collection of ejaculates along with manipulative techniques become more crucial for harvesting the maximum quality and quantity of spermatozoa for successful infertility treatment program (Lambard et al., 2004).
Various methods for semen collection have been employed for semen analysis or for ART program. These methods include masturbation, incomplete intercourse (coitus interruptus), and complete intercourse. WHO (1999) recommends collection of ejaculates via masturbation, and not with coitus interruptus. This is because the first portion of ejaculate, which contains the highest concentration of sperm may be lost at intercourse. Moreover, bacterial contamination of the sample and the acid PH of the vagina adversely affects the sperm quality. However, many patients prefer incomplete coitus as means of sperm collection in Islamic societies. Therefore, the objective of this investigation was to compare the semen characteristics in ejaculates of Iranian patients by means of masturbation and coitus interruptus by a 3 days interval.
Materials and Methods
Thirty men who were referred to the research and clinical center for infertility laboratory for andrological evaluation participated in this study. They were instructed to produce one semen specimen via masturbation and another one via incomplete intercourse by 3 days intervals. Each specimen was collected into a sterile, wide-mouthed container. Semen specimens were assessed according to the WHO standards for volume, viscosity, sperm concentration, progressive and non- progressive motility, normal morphology, and concentration of non-spermatozoal round cells. The semen samples used in this study were considered normozoospermic according to WHO guidelines (1999). Statistical analysis was performed using the student t-test and MC Nemar test. Differences were considered statistically significant when P<0.05.
Results
The results obtained from this study are reported in Table I. The sperm concentration from specimens collected via masturbation was significantly higher than coitus intrruptus ejaculates. Also, both progressive motility and normal morphology of
spermatozoa recovered via masturbation were qualitatively superior (P<0.01), compared with the ejaculates collected via interrupted intercourse. Furthermore, four samples were reported as severe oligospermia in coitus intrruptus group (2.5x106), which were improved to 11.2x106 when specimens were collected via masturbation.
Discussion
The most widely accepted method of semen collection for the purpose of semen analysis or ART is by means of masturbation (Sofikitis and Miyagawa 1993; WHO, 1999; Zavos 1986). The results from this study showed that collection of ejaculates via masturbation is more superior to coitus intrruptus. Collection of semen by means of masturbation resulted in reduction of non-spermatazoal round cell concentration, while the qualitative characteristics such as sperm concentration, progressive motility, and normal morphology were significantly enhanced when compared with results from incomplete coitus. The largest contributors to the round cell population are the immature germ cells followed by leukocytes which may indicate the presence of genital tract infections (Smith et al., 1989).
With ART advancements, the desire for using higher quality spermatozoa to achieve higher success rates has significantly increased (Lambard et al., 2004). Therefore, it seems that semen collection via coitus intrruptus should not be practiced for clinical purposes. The results clearly demonstrated that the aforementioned method of semen collection will alter the vital semen parameters which alternatively may result in reduction of fertilization and pregnancy rates.
Another important finding in our study was the fact that four cases were considered as severe oligozoospermia when ejaculates were collected with incomplete coitus. The samples were improved to a normal oligozoospermia when collections were done via masturbation. However, it should be emphasized that some patients in Iran due to psychological status or religious belief refuse to collect ejaculates via masturbation. For these subjects, Zarmakoupis and colleagues (1999) recommended to use a semen collection device at intercourse. These types of devices consist of a nonspermicidal condom that allows the patients to collect the ejaculates via the complete intercourse. The collected semen, as they assessed, contains high concentration of spermatozoa that have greater motility when compared with samples obtained via the coitus intrruptus method. (Zavos et al., 1994).
In conclusion, the generated results indicate that semen collection via coitus intrruptus is not recommended in infertility treatment programs. The method of choice for collection of high quality spermatozoa with low concentration of round cells is via masturbation. However, if patients refuse to employ the masturbation method, the ejaculates should be produced via the use of nonspermicidal condoms at intercourse.
Type of Study: Original Article |
References
1. Lambard S., Galeraud-Denis I., Martin G., Levy R., and Chocat A. (2004) Analysis and significance of mRNA in human ejaculated sperm from normozoospermic donors: relationship to sperm motility and capacitation. Mol Hum Reprod 20: 302-308. [DOI:10.1093/molehr/gah064] [PMID]
2. Smith D.C., Barratt C.L.R., and Williams M.A. (1989) The characterization of non-sperm cells in the ejaculates of fertile men using transmission electron microscopy. Andrologia, 21: 319-333. [DOI:10.1111/j.1439-0272.1989.tb02417.x] [PMID]
3. Sofikitis N.V., and Miyagawa I. (1993) Endocrinological, biophysical and biochemical parameters of semen collected via masturbation versus sexual intercourse. J Androl 14: 366-373. [DOI:10.1002/j.1939-4640.1993.tb00402.x] [PMID]
4. World Health Organization. (1999) WHO laboratory manual for the examination of human semen and semen-cervical mucus interaction. Cambridge. Cambridge University press: 4-5.
5. Zarmakoupis-Zavos P.N., Correa J.R., Zarmakoupis C.N., and Zavos P.M. (1999) Multiple ejaculate collection via the use of a semen collection device at intercourse versus masturbation. Mid East Fert Soc J 4: 228-232.
6. Zavos P.M. (1986) Qualitative and quantitative seminal losses during production of ejaculates via masturbation. Infertility 9: 153-160.
7. Zavos P.M., Kofinas G.D., and Sofikitis N.V. (1994) Differences in seminal parameters in specimens collected via intercourse and incomplete intercourse. Fertil Steril 61: 1174-1176. [DOI:10.1016/S0015-0282(16)56779-X]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




