Sun, Jul 13, 2025
[Archive]
Volume 18, Issue 7 (July 2020)
IJRM 2020, 18(7): 531-538 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kohestani Y, Kohestani B, Shirmohamadi Z, Faghani M. Effect of tamsulosin on testis histopathology and serum hormones in adult rats: Experimental study. IJRM 2020; 18 (7) :531-538
URL: http://ijrm.ir/article-1-1320-en.html
URL: http://ijrm.ir/article-1-1320-en.html
1- Department of Anatomical Sciences, Bandar-Anzali Pardis, Faculty of Medicine, Guilan University of Medical Sciences, Bandar-Anzali, Iran.
2- Hematopoietic Stem Cell Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Department of Biostatistics, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Anatomical Sciences, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,mfaghani2000@gmail.com
2- Hematopoietic Stem Cell Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
3- Department of Biostatistics, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
4- Department of Anatomical Sciences, Faculty of Medicine, Guilan University of Medical Sciences, Rasht, Iran. ,
Full-Text [PDF 599 kb]
(1140 Downloads)
| Abstract (HTML) (2431 Views)
LUTS are treated by alpha 1-adrenergic receptor blocking drugs and 5-alpha-reductase inhibitor (9, 10). Alpha1 receptors are predominantly present in the stromal tissue of prostate, prostatic urethra, and urinary bladder (11). In other words, the relaxation of the smooth muscles of the prostate and bladder is reduced LUTS in patients with BPH (11). In addition, it is reported that alpha-adrenergic receptor function depends on multiple effectors systems such as multiple G proteins (12). These proteins activate a series of cellular mechanisms that alter the levels of cyclic AMP and intra- and extra cellular Ca++ (13). Of note, Alpha adrenergic receptor agonist might activate these mechanisms (12).
Tamsulosin (Flomax) is considered as one of the selective antagonists for α1A and α1D adrenergic receptors. One of its side effects is disturbance in the male fertility system (13). There are several effective factors on male fertility reduction, including important congenital malformations of the genitourinary system, infectious diseases, genetic disorders, immunologic factors and endocrine axes disorders, painful or difficult urination, abnormal ejaculation, and back pain (14). However, idiopathic cause was found in 60-70%of cases in male infertility (15).
Besides, most researchers, on the other hand, have investigated the effect of tamsulosin in the treatment of BPH (16). Researchers have reported that the use of tamsulosin relaxes the prostate and bladder neck muscles and increases bladder emptying (17). They have focused on tamsulosin therapeutic effects that reduce urinary retention and prostate hyperplasia; however, the probable cytotoxic effects of it on testicular tissue have not been considered yet. It is worth nothing that increasing old population in most societies resulted in higher incidence of BPH and LUTS. Therefore, to reduce the symptoms of patients with BPH and LUTS, tamsulosin is considered as a safe drug (16, 18) and is prescribed routinely; however, its effect on endocrine axis and histology of testicular tissue has not been fully studied. Thus, the present study was aimed to evaluate the effect of tamsulosin on serum concentration of male hormones and histopathology of the testicular tissue.
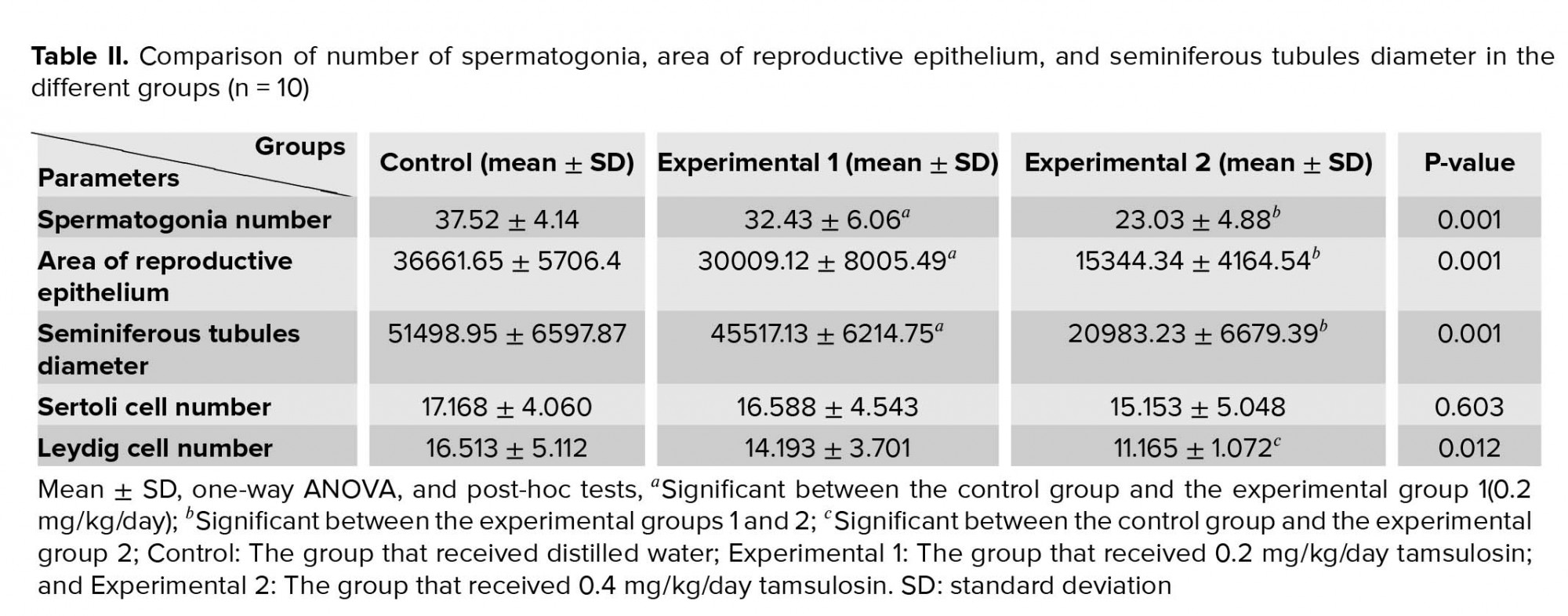
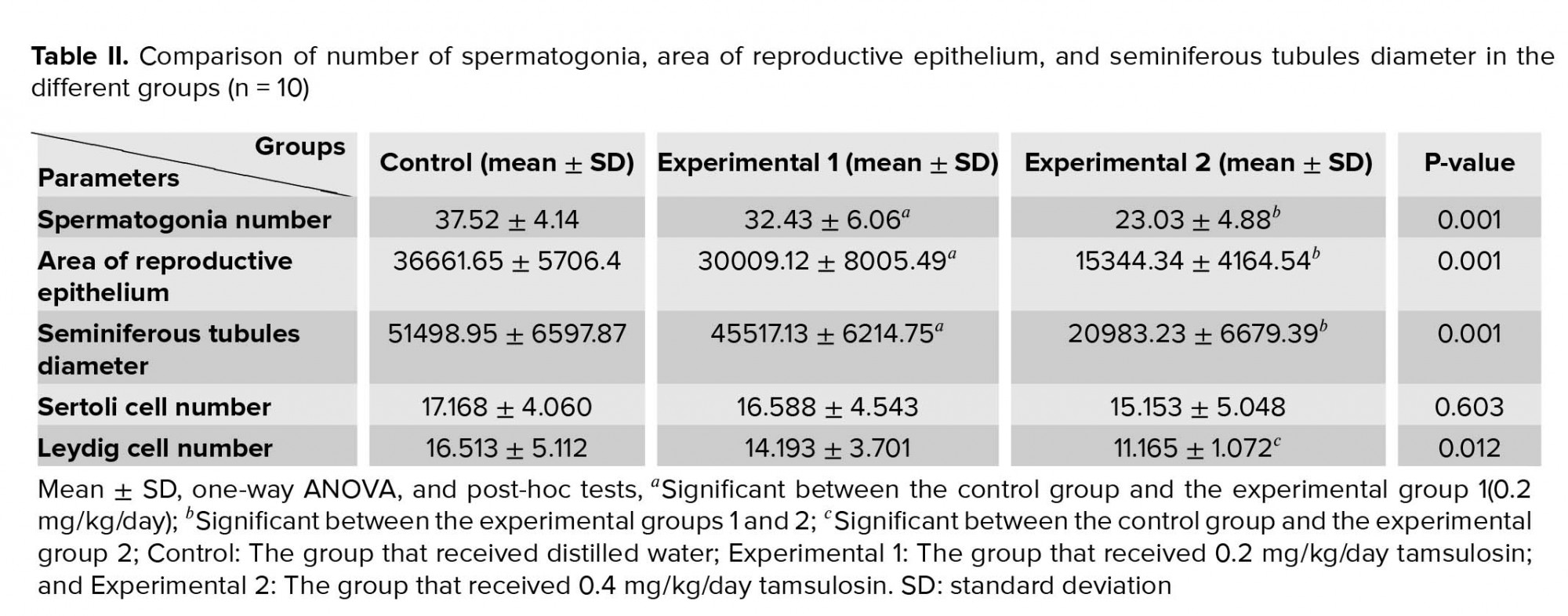
Sections measuring 5 µm were prepared and at least five slides from each testis were stained with Heiden Hain Azan for histopathological evaluation. This was performed according to the routine tissue-staining methods. In order to evaluate the testis tissue histopathological changes, four slices were assessed from each mouse. Five microscopic fields from each slide were observed at 400× magnification using a standard light microscope (Olympus, Japan). Spermatogonia, Sertoli, and Leydig cells were counted using the light microscope, and the images were prepared by a digital camera (BX 51 Japan) calibrated with a hemocytometer slide share attached to the microscope. Germinal epithelium area, seminiferous tubules diameter, and number of seminiferous tubules and interstitial cells were measured using the Image J 1.44P software (National institute of Health, USA).
Our findings revealed that tamsulosin significantly decreased the plasma concentration of testosterone in comparison with the control (p = 0.0001) (Table I). Moreover, testosterone level decreased more in the experimental group 2 compared to the experimental group 1 (p = 0001) (Table I; Figure 1). Of note, tamsulosin significantly increased the FSH level in the experimental groups (p= 0.009).
The spermatogenesis was evaluated in germinal epithelium through spermatogonia cell numbers. It showed a significant decrease in the numbers of spermatogonia across all groups (p= 0.0001). In addition, there was a significant difference in the number of spermatogonia between the experimental groups in dose-dependent manner of tamsulosin (Table II). Furthermore, areas of reproductive epithelium remarkably reduced in the experimental groups (p = 0.0001). Interestingly, some vacuoles were observed in germinal epithelium especially in the experimental group 2 (Figure 1).


4. Discussion
The present study showed that tamsulosin resulted in pathological changes in testis and the secretion of testosterone in male rats. In addition, it is suggested that tamsulosin could inhibit androgenesis process. The serum testosterone level was decreased significantly among the experimental groups (p < 0.05), which indicates the strong impact of higher dose of tamsulosin on androgenesis. It is suggested that the tamsulosin exerts its function on the activity of gonadotropin-releasing hormone under the influence of norepinephrine by alpha-adrenergic receptors. Norepinephrine, as a neurotransmitter that is secreted from adrenergic neurons, has a significant impact on adrenergic receptors, especially alpha receptors. Also, these adrenergic neurons can target gonadotropin-releasing hormone (14, 21, 22). Furthermore, norepinephrine can release the LH-releasing hormone.
According to Selvage’s findings, prazosin and adrenergic receptors inhibitor reduced the production of LH-releasing hormone in the hypothalamus and resulted in LH decrease (23). In other words, this axis is able to influence the secretion of testosterone through the inhibition of LH. In addition, some studies have shown that the alternative releasing of LHRH is modulated by adrenergic neurons, particularly norepinephrine, via alpha1-adrenergic receptors (22, 24).
Alpha-blockers are usually used as the first choice of treatment for patients suffering from LUTS because the safety and effectiveness of these have been confirmed in many randomized studies (17, 25, 26).
Androgens exert their effects on prostate proliferation by binding and activating the androgen receptors. Anti-androgens competitively inhibit the binding of the receptors by agonists. When anti-androgens are combined to their receptors, they, therefore, don’t bind to DNA and transcription would be inhibited (27).
On the other hand, based on Gotkas and coworker’s study, the advantage of taking single dose of tamsulosin compared to the rest of α1-adrenoceptor antagonist is not convincing enough for this medicine to be used in all patients (20). Therefore, it seems that clinicians routinely use different doses of tamsulosin depending on the severity of the disease. In addition, α-blockers often influence the secretion of testosterone. According to our results, taking 0.2 and 0.4 mg/kg of tamsulosin for 28 days significantly decreased the testosterone concentration and disturbed the testicular tissue histology in the experimental groups. This may be described by the harmful effects of tamsulosin on the gonadotropin-hypothalamic axis and Leydig cells. Our finding was confirmed by the reduction of the numbers of Leydig cells between the experimental groups (p = 0.009).
Some studies used 0.4 mg/kg of tamsulosin to treat BPH based on the severity of the disease and did not consider the side effects of tamsulosin in reducing spermatogonia and Leydig cells (26, 28). Of note, our study showed that tamsulosin at a dose of 0.2 mg/kg can also significantly reduce the number of spermatogonia. and Leydig cells. Significant reduction of androgens with a 0.2 mg/kg of tamsulosin can sufficiently reduce androgens for the desirable therapeutic effect. To prevent the side effects of tamsulosin, it is recommended to use a lower dose of 0.2 mg/kg for the treatment of LUTS.
Our study revealed a significant decrease in the number of spermatogonia, the areas of reproductive epithelium, and the diameter of seminiferous tubules in the experimental groups (p < 0.001), which indicates the destructive effect of tamsulosin in the testicular tissue. In addition, our study showed that there were many vacuoles in germinal epithelium in experimental groups 1 and 2 compared to the control group that may indicate tissue damage in the germinal epithelium. Our data are consistent with the results of previous studies on the dose-dependent use of this drug. Beltagy and coworkers found that the treatment with tamsulosin hydrochloride had more harmful side effects than finasteride on rats, which leads to the disturbances in prostatic, testicular function, and neurotransmitters indices (29). Besides, they also reported that combined treatment of finasteride with tamsulosin hydrochloride has lower side effects than tamsulosin hydrochloride alone.
In another study, researchers combined the tamsulosin with non- α-blockers such as Omega 3 fatty acid and the results were fantastic. They reported that this co-treatment had better clinical results (30). In another study, drugs combination therapy was used to reduce the deleterious effects of tamsulosin. They showed that the combination of three drugs LDD175, tamsulosin, and finasteride is more effective in the treatment of BPH patients because some patients are ressistnt to individual administration of these drugs (31). On In another study, the researchers observed a significant decrease in the number, mobility, activity, and survival of the epididymal sperm after tamsulosin injection, especially at higher doses. Higher doses of drug results in a significant decrease in testosterone levels, testes and body weight, diameter of seminiferous tubules, and number of Leydig cells (32). It seems that tamsulosin has destructive effects on testis tissue, imbalance hormones level and infertility. Therefore, using low dose of this drug alongside the application of other proper antagonist drugs is recommended.
5. Conclusion
Finally, according to the results of this study, the secretion of testosterone hormone reduced after the administration of tamsulosin and could possibly have a significant effect on hypothalamic- hypophysial axis. Testosterone impacts the activity of the gonadotrophin-releasing hormone, which is itself influenced by norepinephrine and adrenergic receptors. Considering the AUA Guideline and ejaculatory dysfunction at higher doses of tamsulosin, it is better to avoid using higher doses of tamsulosin to prevent its adverse side effects on testicular tissue. It is revealed that histopathological changes of testicular tissue resulted in the reduction of hormone levels. Therefore, it is suggested that a combination therapy with other drugs could probably reduce the harmful side effects of tamsulosin.
Acknowledgments
This research was supported by the Anzali International Campus, Faculty of Medicine, Guilan University of Medical Sciences under ethic number IR.GUMS.REC.1398.388. The authors are thankful to the Honorable Vice Chancellor for Research, Anzali International Campus of Medical University Guilan for providing the financial support to this study and also to Mr. Ali Farzanegan for his cooperation throughout the study.
Conflict of interest
The authors declare no conflict of interest.
Full-Text: (664 Views)
- Introduction
LUTS are treated by alpha 1-adrenergic receptor blocking drugs and 5-alpha-reductase inhibitor (9, 10). Alpha1 receptors are predominantly present in the stromal tissue of prostate, prostatic urethra, and urinary bladder (11). In other words, the relaxation of the smooth muscles of the prostate and bladder is reduced LUTS in patients with BPH (11). In addition, it is reported that alpha-adrenergic receptor function depends on multiple effectors systems such as multiple G proteins (12). These proteins activate a series of cellular mechanisms that alter the levels of cyclic AMP and intra- and extra cellular Ca++ (13). Of note, Alpha adrenergic receptor agonist might activate these mechanisms (12).
Tamsulosin (Flomax) is considered as one of the selective antagonists for α1A and α1D adrenergic receptors. One of its side effects is disturbance in the male fertility system (13). There are several effective factors on male fertility reduction, including important congenital malformations of the genitourinary system, infectious diseases, genetic disorders, immunologic factors and endocrine axes disorders, painful or difficult urination, abnormal ejaculation, and back pain (14). However, idiopathic cause was found in 60-70%of cases in male infertility (15).
Besides, most researchers, on the other hand, have investigated the effect of tamsulosin in the treatment of BPH (16). Researchers have reported that the use of tamsulosin relaxes the prostate and bladder neck muscles and increases bladder emptying (17). They have focused on tamsulosin therapeutic effects that reduce urinary retention and prostate hyperplasia; however, the probable cytotoxic effects of it on testicular tissue have not been considered yet. It is worth nothing that increasing old population in most societies resulted in higher incidence of BPH and LUTS. Therefore, to reduce the symptoms of patients with BPH and LUTS, tamsulosin is considered as a safe drug (16, 18) and is prescribed routinely; however, its effect on endocrine axis and histology of testicular tissue has not been fully studied. Thus, the present study was aimed to evaluate the effect of tamsulosin on serum concentration of male hormones and histopathology of the testicular tissue.
- Materials and Methods
- 1. Animals and treatment
- 2. Blood sampling and testis weight measurement
- 3. Preparing the tissue samples
Sections measuring 5 µm were prepared and at least five slides from each testis were stained with Heiden Hain Azan for histopathological evaluation. This was performed according to the routine tissue-staining methods. In order to evaluate the testis tissue histopathological changes, four slices were assessed from each mouse. Five microscopic fields from each slide were observed at 400× magnification using a standard light microscope (Olympus, Japan). Spermatogonia, Sertoli, and Leydig cells were counted using the light microscope, and the images were prepared by a digital camera (BX 51 Japan) calibrated with a hemocytometer slide share attached to the microscope. Germinal epithelium area, seminiferous tubules diameter, and number of seminiferous tubules and interstitial cells were measured using the Image J 1.44P software (National institute of Health, USA).
- 4. Serum hormones level analysis
- 5. Ethical consideration
- 6. Statistical analysis
- Results
Our findings revealed that tamsulosin significantly decreased the plasma concentration of testosterone in comparison with the control (p = 0.0001) (Table I). Moreover, testosterone level decreased more in the experimental group 2 compared to the experimental group 1 (p = 0001) (Table I; Figure 1). Of note, tamsulosin significantly increased the FSH level in the experimental groups (p= 0.009).
The spermatogenesis was evaluated in germinal epithelium through spermatogonia cell numbers. It showed a significant decrease in the numbers of spermatogonia across all groups (p= 0.0001). In addition, there was a significant difference in the number of spermatogonia between the experimental groups in dose-dependent manner of tamsulosin (Table II). Furthermore, areas of reproductive epithelium remarkably reduced in the experimental groups (p = 0.0001). Interestingly, some vacuoles were observed in germinal epithelium especially in the experimental group 2 (Figure 1).


4. Discussion
The present study showed that tamsulosin resulted in pathological changes in testis and the secretion of testosterone in male rats. In addition, it is suggested that tamsulosin could inhibit androgenesis process. The serum testosterone level was decreased significantly among the experimental groups (p < 0.05), which indicates the strong impact of higher dose of tamsulosin on androgenesis. It is suggested that the tamsulosin exerts its function on the activity of gonadotropin-releasing hormone under the influence of norepinephrine by alpha-adrenergic receptors. Norepinephrine, as a neurotransmitter that is secreted from adrenergic neurons, has a significant impact on adrenergic receptors, especially alpha receptors. Also, these adrenergic neurons can target gonadotropin-releasing hormone (14, 21, 22). Furthermore, norepinephrine can release the LH-releasing hormone.
According to Selvage’s findings, prazosin and adrenergic receptors inhibitor reduced the production of LH-releasing hormone in the hypothalamus and resulted in LH decrease (23). In other words, this axis is able to influence the secretion of testosterone through the inhibition of LH. In addition, some studies have shown that the alternative releasing of LHRH is modulated by adrenergic neurons, particularly norepinephrine, via alpha1-adrenergic receptors (22, 24).
Alpha-blockers are usually used as the first choice of treatment for patients suffering from LUTS because the safety and effectiveness of these have been confirmed in many randomized studies (17, 25, 26).
Androgens exert their effects on prostate proliferation by binding and activating the androgen receptors. Anti-androgens competitively inhibit the binding of the receptors by agonists. When anti-androgens are combined to their receptors, they, therefore, don’t bind to DNA and transcription would be inhibited (27).
On the other hand, based on Gotkas and coworker’s study, the advantage of taking single dose of tamsulosin compared to the rest of α1-adrenoceptor antagonist is not convincing enough for this medicine to be used in all patients (20). Therefore, it seems that clinicians routinely use different doses of tamsulosin depending on the severity of the disease. In addition, α-blockers often influence the secretion of testosterone. According to our results, taking 0.2 and 0.4 mg/kg of tamsulosin for 28 days significantly decreased the testosterone concentration and disturbed the testicular tissue histology in the experimental groups. This may be described by the harmful effects of tamsulosin on the gonadotropin-hypothalamic axis and Leydig cells. Our finding was confirmed by the reduction of the numbers of Leydig cells between the experimental groups (p = 0.009).
Some studies used 0.4 mg/kg of tamsulosin to treat BPH based on the severity of the disease and did not consider the side effects of tamsulosin in reducing spermatogonia and Leydig cells (26, 28). Of note, our study showed that tamsulosin at a dose of 0.2 mg/kg can also significantly reduce the number of spermatogonia. and Leydig cells. Significant reduction of androgens with a 0.2 mg/kg of tamsulosin can sufficiently reduce androgens for the desirable therapeutic effect. To prevent the side effects of tamsulosin, it is recommended to use a lower dose of 0.2 mg/kg for the treatment of LUTS.
Our study revealed a significant decrease in the number of spermatogonia, the areas of reproductive epithelium, and the diameter of seminiferous tubules in the experimental groups (p < 0.001), which indicates the destructive effect of tamsulosin in the testicular tissue. In addition, our study showed that there were many vacuoles in germinal epithelium in experimental groups 1 and 2 compared to the control group that may indicate tissue damage in the germinal epithelium. Our data are consistent with the results of previous studies on the dose-dependent use of this drug. Beltagy and coworkers found that the treatment with tamsulosin hydrochloride had more harmful side effects than finasteride on rats, which leads to the disturbances in prostatic, testicular function, and neurotransmitters indices (29). Besides, they also reported that combined treatment of finasteride with tamsulosin hydrochloride has lower side effects than tamsulosin hydrochloride alone.
In another study, researchers combined the tamsulosin with non- α-blockers such as Omega 3 fatty acid and the results were fantastic. They reported that this co-treatment had better clinical results (30). In another study, drugs combination therapy was used to reduce the deleterious effects of tamsulosin. They showed that the combination of three drugs LDD175, tamsulosin, and finasteride is more effective in the treatment of BPH patients because some patients are ressistnt to individual administration of these drugs (31). On In another study, the researchers observed a significant decrease in the number, mobility, activity, and survival of the epididymal sperm after tamsulosin injection, especially at higher doses. Higher doses of drug results in a significant decrease in testosterone levels, testes and body weight, diameter of seminiferous tubules, and number of Leydig cells (32). It seems that tamsulosin has destructive effects on testis tissue, imbalance hormones level and infertility. Therefore, using low dose of this drug alongside the application of other proper antagonist drugs is recommended.
5. Conclusion
Finally, according to the results of this study, the secretion of testosterone hormone reduced after the administration of tamsulosin and could possibly have a significant effect on hypothalamic- hypophysial axis. Testosterone impacts the activity of the gonadotrophin-releasing hormone, which is itself influenced by norepinephrine and adrenergic receptors. Considering the AUA Guideline and ejaculatory dysfunction at higher doses of tamsulosin, it is better to avoid using higher doses of tamsulosin to prevent its adverse side effects on testicular tissue. It is revealed that histopathological changes of testicular tissue resulted in the reduction of hormone levels. Therefore, it is suggested that a combination therapy with other drugs could probably reduce the harmful side effects of tamsulosin.
Acknowledgments
This research was supported by the Anzali International Campus, Faculty of Medicine, Guilan University of Medical Sciences under ethic number IR.GUMS.REC.1398.388. The authors are thankful to the Honorable Vice Chancellor for Research, Anzali International Campus of Medical University Guilan for providing the financial support to this study and also to Mr. Ali Farzanegan for his cooperation throughout the study.
Conflict of interest
The authors declare no conflict of interest.
Type of Study: Original Article |
Subject:
Reproductive Biology
References
1. Lim KB. Epidemiology of clinical benign prostatic hyperplasia. Asian J Urol 2017; 4: 148-151. [DOI:10.1016/j.ajur.2017.06.004] [PMID] [PMCID]
2. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol 1984; 132: 474-479. [DOI:10.1016/S0022-5347(17)49698-4]
3. Kok ET, Schouten BW, Bohnen AM, Groeneveld FP, Thomas S, Bosch JR. Risk factors for lower urinary tract symptoms suggestive of benign prostatic hyperplasia in a community based population of healthy aging men: the Krimpen Study. J Urol 2009; 181: 710-716. [DOI:10.1016/j.juro.2008.10.025] [PMID]
4. Guess HA, Arrighi HM, Metter EJ, Fozard JL. Cumulative prevalence of prostatism matches the autopsy prevalence of benign prostatic hyperplasia. Prostate 1990; 17: 241-246. [DOI:10.1002/pros.2990170308] [PMID]
5. Taylor BC, Wilt TJ, Fink HA, Lambert LC, Marshall LM, Hoffman AR, et al. Prevalence, severity, and health correlates of lower urinary tract symptoms among older men: the MrOS study. Urology 2006; 68: 804-809. [DOI:10.1016/j.urology.2006.04.019] [PMID]
6. Bosch JL, Tilling K, Bohnen AM, Bangma CH, Donovan JL. Establishing normal reference ranges for prostate volume change with age in the population‐based Krimpen‐study: Prediction of future prostate volume in individual men. Prostate 2007; 67: 1816-1824. [DOI:10.1002/pros.20663] [PMID]
7. Loeb S, Kettermann A, Carter HB, Ferrucci L, Metter EJ, Walsh PC. Prostate volume changes over time: results from the Baltimore Longitudinal Study of Aging. J Urol 2009; 182: 1458-1462. [DOI:10.1016/j.juro.2009.06.047] [PMID] [PMCID]
8. Bosch JL, Bangma CH, Groeneveld FP, Bohnen AM. The long-term relationship between a real change in prostate volume and a significant change in lower urinary tract symptom severity in population-based men: the Krimpen study. Eur Urol 2008; 53: 819-825. [DOI:10.1016/j.eururo.2007.08.042] [PMID]
9. Konstantinidis C, Samarinas M, Andreadakis S, Xanthis S, Skriapas K. Lower urinary tract symptoms associated with benign prostatic hyperplasia: combined treatment with fesoterodine fumarate extended-release and tamsulosin-a prospective study. Urol Int 2013; 90: 156-160. [DOI:10.1159/000345050] [PMID]
10. Bruskewitz RC. Quality of life and sexual function in patients with benign prostatic hyperplasia. Rev Urol 2003; 5: 72-80.
11. Dunn CJ, Matheson A, Faulds DM. Tamsulosin: a review of its pharmacology and therapeutic efficacy in the management of lower urinary tract symptoms. Drugs Aging 2002; 19: 135-161. [DOI:10.2165/00002512-200219020-00004] [PMID]
12. Insel PA. Structure and function of alpha-adrenergic receptors. Am J Med 1989; 87: S12-S18. [DOI:10.1016/0002-9343(89)90108-3]
13. Kim JJ, Han DH, Sung HH, Choo SH, Lee SW. Efficacy and tolerability of tamsulosin 0.4 mg in A sian patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia refractory to tamsulosin 0.2 mg: a randomized placebo controlled trial. Int J Urol 2014; 21: 677-682. [DOI:10.1111/iju.12412] [PMID]
14. Rowe PJ, Comhaire FH, Hargreave TB, Mahmoud AM. WHO manual for the standardized investigation and diagnosis of the infertile male. Cambridge University Press: UK; 2000.
15. Dohle GR, Colpi GM, Hargreave TB, Papp GK, Jungwirth A, Weidner W, et al. EAU guidelines on male infertility. Eur Urol 2005; 48: 703-711. [DOI:10.1016/j.eururo.2005.06.002] [PMID]
16. Zhou Z, Cui Y, Wu J, Ding R, Cai T, Gao Z. Meta-analysis of the efficacy and safety of combination of tamsulosin plus dutasteride compared with tamsulosin monotherapy in treating benign prostatic hyperplasia. BMC Urol 2019; 19: 17-28. [DOI:10.1186/s12894-019-0446-8] [PMID] [PMCID]
17. Pogula VR, Kadiyala LS, Gouru VR, Challa SR, Byram R, Bodduluri S. Tadalafil vs. tamsulosin in the treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: a prospective, randomized study. Cent Eur J Urol 2019; 72: 44-50.
18. Lepor H. Phase III multicenter placebo-controlled study of tamsulosin in benign prostatic hyperplasia. Tamsulosin Investigator Group. Urology 1998; 51: 892-900. [DOI:10.1016/S0090-4295(98)00126-5]
19. Arruzazabala ML, Mas R, Molina V, Noa M, Carbajal D, Mendoza N. Effect of D-004, a lipid extract from the Cuban royal palm fruit, on atypical prostate hyperplasia induced by phenylephrine in rats. Drugs R D 2006; 7: 233-241. [DOI:10.2165/00126839-200607040-00003] [PMID]
20. Goktas S, Kibar Y, Kilic S, Topac H, Coban H, Seckin B. Recovery of abnormal ejaculation by intermittent tamsulosin treatment. J Urol 2006; 175: 650-653. [DOI:10.1016/S0022-5347(05)00157-6]
21. Kamimura H, Oishi S, Matsushima H, Watanabe T, Higuchi S, Hall M, et al. Identification of cytochrome P450 isozymes involved in metabolism of the α 1-adrenoceptor blocker tamsulosin in human liver microsomes. Xenobiotica 1998; 28: 909-922. [DOI:10.1080/004982598238985] [PMID]
22. Ratnasooriya WD, Wadsworth RM. Tamsulosin, a selective alpha 1‐adrenoceptor antagonist, inhibits fertility of male rats. Andrologia 1994; 26: 107-110. [DOI:10.1111/j.1439-0272.1994.tb00766.x] [PMID]
23. Selvage DJ, Lee SY, Parsons LH, Seo DO, Rivier CL. A hypothalamic-testicular neural pathway is influenced by brain catecholamines, but not testicular blood flow. Endocrinology 2004; 145: 1750-1759. [DOI:10.1210/en.2003-1441] [PMID]
24. Lee S, Miselis R, Rivier C. Anatomical and functional evidence for a neural hypothalamic-testicular pathway that is independent of the pituitary. Endocrinology 2002; 143: 4447-4454. [DOI:10.1210/en.2002-220392] [PMID]
25. Djavan B, Marberger M. A meta-analysis on the efficacy and tolerability of α1-adrenoceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic obstruction. Eur Urol 1999; 36: 1-13. [DOI:10.1159/000019919] [PMID]
26. Yang PS, Chen CL, Hou CP, Lin YH, Tsui KH. An open-label, prospective interventional study of the tolerability and efficacy of 0.4 mg oral tamsulosin oral controlled absorption system in men with lower urinary tract symptoms associated with benign prostatic hyperplasia who are unsatisfied with treatment with 0.2 mg tamsulosin. Clin Interv Aging 2018; 13: 235-242. [DOI:10.2147/CIA.S152701] [PMID] [PMCID]
27. Chen Y, Clegg NJ, Scher HI. Anti-androgens and androgen-depleting therapies in prostate cancer: new agents for an established target. lancet Oncol 2009; 10: 981-991. [DOI:10.1016/S1470-2045(09)70229-3]
28. Roehrborn CG, Oyarzabal Perez I, Roos EP, Calomfirescu N, Brotherton B, Wang F, et al. Efficacy and safety of a fixed‐dose combination of dutasteride and tamsulosin treatment (D uodart®) compared with watchful waiting with initiation of tamsulosin therapy if symptoms do not improve, both provided with lifestyle advice, in the management of treatment‐naïve men with moderately symptomatic benign prostatic hyperplasia: 2‐year CONDUCT study results. BJU Int 2015; 116: 450-459. [DOI:10.1111/bju.13033] [PMID]
29. Beltagy D, Ali H, Abdel-Gelil A, Abdel-Gawad A, Abdel Aziz K. Impact of Finasteride and Tamsulosin Hydrochloride Administration on sex hormones, prostatic markers and neurotransmitters in male rats. 2015. Available at: https://apps.who.int/iris/handle/10665/42437.
30. Ghadian A, Rezaei M. Combination therapy with omega-3 fatty acids plus tamsulocin and finasteride in the treatment of men with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH). Inflammopharmacology 2017; 25: 451-458. [DOI:10.1007/s10787-017-0343-2] [PMID]
31. Choi BR, Kim HK, Soni KK, Karna KK, Lee SW, So I, et al. Additive effect of oral LDD175 to tamsulosin and finasteride in a benign prostate hyperplasia rat model. Drug Des Devel Ther 2018; 12: 1855-1863. [DOI:10.2147/DDDT.S164049] [PMID] [PMCID]
32. Alwachi SN, Husain DK. Research article Tamsulosin hydrochloride (flomax) effects on fertility of albino male mice. Int J Recent Sci Res 2014; 5: 326-331.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |