Sun, Feb 22, 2026
[Archive]
Volume 19, Issue 1 (January 2021)
IJRM 2021, 19(1): 57-62 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammad jafari R, Zargar M, Barati M, Ershadian S. The comparison of predictive value of cervical length in singleton spontaneous preterm labor with in vitro fertilization pregnancies: A cohort study. IJRM 2021; 19 (1) :57-62
URL: http://ijrm.ir/article-1-1435-en.html
URL: http://ijrm.ir/article-1-1435-en.html
1- Fertility Infertility and Perinatology Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
2- Fertility Infertility and Perinatology Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,dr.ershadian@gmail.com
2- Fertility Infertility and Perinatology Research Center, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. ,
Full-Text [PDF 264 kb]
(1499 Downloads)
| Abstract (HTML) (2458 Views)
Full-Text: (586 Views)
1. Introduction
Preterm delivery (PTD) is a significant cause of neonatal morbidity and mortality. Over the last two decades, a worldwide increase has been seen in the rate of PTD (1). PTD is comprised of 10% of deliveries; it causes 75% of perinatal mortalities. However, owing to the improvement in the premature neonatal care, the morbidity and mortality resulting from preterm labor (PTL) has decreased. The increased rate of PTL may be due to the increase in the usage of infertility therapies and assisted reproduction technologies and increased age of pregnancy. Transvaginal ultrasound (TVU) for the measurement of cervical length (CL) has been evaluated in both asymptomatic and symptomatic women in terms of PTL (2). The correlation between a short CL and PTD is well established in singleton pregnancies and even the shortened cervix is a better predictor for PTD than clinical examination or fetal fibronectin (3, 4). Also, compared to normal singleton pregnancies, in vitro fertilization (IVF)-conceived singleton pregnancies is associated with higher pregnancy-related complications, including increased risk of cesarean delivery, intrauterine growth restriction, preeclampsia, congenital malformations, low birth weight, and higher risk of PTD (5). Similarly, PTD is more prevalent in IVF-conceived pregnancies as compared with those conceived naturally (6). A meta-analysis of 15 studies showed that the risk of spontaneous preterm birth (PTB) in singleton pregnancies resulting from IVF is significantly higher than that in spontaneously conceived singletons (7). In high-risk women for PTL, the CL is short. Therefore, the CL measurement is used to predict higher-risk pregnancies (8). Data pertaining to the measurement of CL and specifically studies assessing whether the increased risk of spontaneous PTB is predicted by a difference in CL are limited.
Therefore, the aim of this study was to evaluate the predictive value of transvaginal sonographic CL for the prediction of PTD before 37 wk between two groups of spontaneous and IVF pregnancies in asymptomatic women.
2. Materials and Methods
This prospective cohort study included 154 singleton pregnant women who attended the Prenatal Care Clinic and Infertility Clinic at Imam Khomeini Hospital affiliated to the Jundishapur University of Medical Sciences between March 2016 and June 2017 in Ahvaz, Iran. Participants were divided into two groups of spontaneously (n = 77) and IVF-conceived (n = 77) pregnancies. Patients were enrolled at 16-26 wk of gestation and followed up until the delivery. The exclusion criteria of the study included women with multiple pregnancies, placenta previa, cerclage, fetal anomalies, and elective PTL. In both groups, CL was measured from 16 through 26 weeks of gestation using TVU. Sonography was performed by two sonographers who are certified by FMF for CL measurement (V20 Madison). For the TVU, the women were first asked to empty their bladder after which they were placed in the lithotomy position. The sonography probe was inserted in anterior vaginal fornix without pressure. Sagittal cervix was shown and linear distance between internal and external OS was measured. All patients were followed until delivery and demographic data, gestational age at delivery, and CL (mm) at 16-26 weeks of gestation were recorded. Gestational age was determined from the date of the last menstrual period (LMP) and confirmed by the measurement of the CRL. PTL was defined as delivery <37 weeks of gestation in both groups. Pregnancy outcome was obtained from the interview with mothers. For the determination of the cut-off, the Roc analysis was used and the sensitivity, negative and positive predictive values were calculated.
2.1. Ethical considerations
This study was approved by Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IRAJUMS.REC.1396.889). All participants signed an informed consent form prior to the study.
2.2. Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences, version 18.0, SPSS Inc., Chicago, IL, USA (SPSS). The cut-off was determined according to the Roc analysis. The significance of differences between two groups was assessed using independent t tests and Chi square test. P < 0.05 was considered as statistically significant.
3. Results
A total of 154 pregnant women aged range of 19-46 yr with a mean age of 29.9±4.9 yr in the normal group and 32.18±5.58 yr in the IVF group (p = 0.052) were included in the study. Table I shows the demographic data and outcomes of the pregnancies. The average BMI in the spontaneous and IVF groups is shown in the table mentioned (Table I).The average birth’s weeks in spontaneous group was significantly higher than the IVF group (p < 0.001). Six women in spontaneous group and 18 women in IVF group delivered before 37 weeks.
The mean CL did not significantly differ between while the mean CL did not differ significantly between the PTL and term pregnancies in the normal group, it was significantly lower in the PTL than the term pregnancies in the IVF group. Additionally, the mean CL in the PTL subgroup of spontaneous pregnancy was significantly greater than the mean CL in the PTL subgroup of IVF pregnancy (according to Table II).
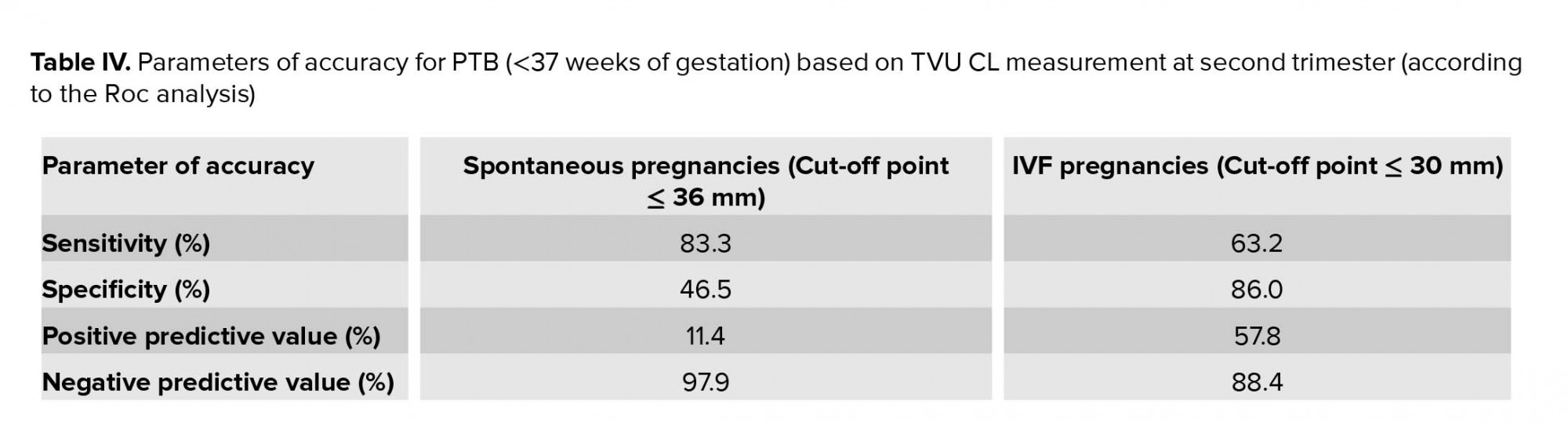
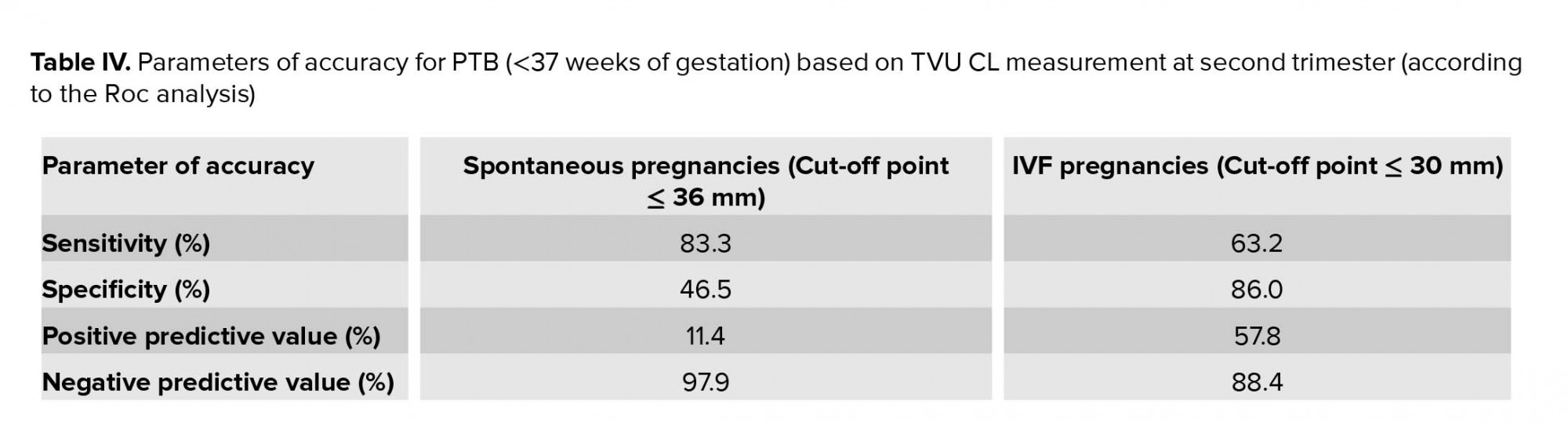
The classification of CL according to Table III showed that all patients with CL < 25 mm were preterm, while all patients with CL ≥ 45 mm were term. Therefore, as presented in table IV, the best cut-off points obtained from the ROC curve were ≤ 36 mm for the spontaneous group, with a high negative predictive value (NPV) of 97.9%, low positive predictive value (PPV) of 11.4%, high sensitivity of 83.3%, and low specificity of 46.5% and ≤ 30 mm for the IVF group with a high NPV of 88.4%, low PPV of 57.8%, sensitivity of 63.2%, and low specificity of 86.0%.
According to tables V and VI, the number of cesarean deliveries in the IVF group was 20, of which 12 were term and 8 preterm. The number of cesarean deliveries in the spontaneous group was 10, with 9 term and 1 preterm.
The mean + SD CL for the all the subjects was 36.4 + 7.6 mm (range: 21-70 mm). The CL did not differ significantly between the two groups of IVF and spontaneously-conceived pregnancies (p = 0.06).
Of the 154 patients of the study, 130 (83.7%) were term and 24 (16.4%) PTL. The mean CL in the PTL group was significantly lower than that in the term group (Table III).





4. Discussion
The predictive value of cervical measurement were compared via transvaginal sonography at second trimester (16-26 weeks) for predicting the PTB between the two groups of asymptomatic singleton pregnant women conceived spontaneously or by IVF. The ROC curve was used to suggest best cut-off rather than the percentile of CL measurement. The studies comparing the predictive value of CL for PTB between spontaneous and IVF singleton pregnancies are rare. Many studies have investigated the relationship between CL and PTB adopting different methodologies to obtain the cut-off point, either percentile or ROC curve.
The current study showed that the best cut-off points obtained from the ROC curve were ≤36 mm for the spontaneous group, with a high NPV of 97.9%, low PPV of 11.4%, high sensitivity of 83.3%, and low specificity of 46.5%, and ≤ 30 mm for the IVF group with high NPV 88.4%, low PPV of 57.8%, sensitivity of 63.2%, and low specificity of 86.0%. The most accurate cut-off for a screening test should have a high sensitivity and an adequate PPV and NPV (9). Therefore, our study has confirmed that the TVU CL measurement at the second trimester is a better screening test for spontaneous PTB in naturally conceived pregnancies compared to the IVF ones, since it has higher NVP (97.9% vs 88.4%, respectively).
In our study, the rate of PTB in the IVF group was significantly higher than that in the spontaneous group. These results are strongly in agreement with previously published studies and a large meta-analysis that have reported that the PTB is more prevalent in IVF-conceived pregnancies compare to those conceived spontaneously (5-7, 10, 11). Although, none of the studies so far has presented the clarification for such findings. However, we decided to find out whether IVF and naturally conceived pregnancies differ in CL measured by TVU in the second trimester. The only available meta-analysis showed that the decrease in the length of cervix is associated with the increase in the risk of PTB (12, 13). This conclusion was confirmed in all studies and also in the current study. However, we found that the mean CL did not significantly differ between the spontaneous and IVF groups (p = 0.06). The subgroups analysis showed that the length of cervix in the term and preterm pregnancies in the IVF group showed a significant difference (p = 0.001). In our study, none of the patients in the spontaneous group had a short cervix (CL < 25 mm), however, the rate of short cervix in the IVF group was 11.7%. A cut-off value of ≤36 mm was obtained in our study for predicting the PTB in spontaneous group which is greater than the values reported by other published studies. This discrepancy may be attributed to no case of short cervix in our study. While the lower cut-off point of CL (≤ 30 mm) suggested in our study for predicting PTB in IVF group can be attributed to the rate of short cervix of IVF patients (11.7%). Iams et al. published the first large study of CL measurement at 26 weeks of gestation in singleton pregnancies in 1996 (14). They reported cut-off points of 30, 25, and 20 mm related to the 25th, 10th, and 5th percentile in their studied population according to the ROC curves.
5. Conclusion
In this study, IVF had a significant direct correlation with PTL. In addition, CL had a significant indirect relationship with PTL. The results of this study indicated that CL measurement in the second trimester of pregnancy in women with singleton baby has a lower cut-off for predicting PTD.
Acknowledgements
This article has been extracted from the thesis of Somayeh Ershadian. The author would like to acknowledge the Department of Obstetrics and Gynecology at Imam Khomeini Hospital in Ahvaz.
Conflict of Interest
The authors declare that there is no conflict of interest.
Preterm delivery (PTD) is a significant cause of neonatal morbidity and mortality. Over the last two decades, a worldwide increase has been seen in the rate of PTD (1). PTD is comprised of 10% of deliveries; it causes 75% of perinatal mortalities. However, owing to the improvement in the premature neonatal care, the morbidity and mortality resulting from preterm labor (PTL) has decreased. The increased rate of PTL may be due to the increase in the usage of infertility therapies and assisted reproduction technologies and increased age of pregnancy. Transvaginal ultrasound (TVU) for the measurement of cervical length (CL) has been evaluated in both asymptomatic and symptomatic women in terms of PTL (2). The correlation between a short CL and PTD is well established in singleton pregnancies and even the shortened cervix is a better predictor for PTD than clinical examination or fetal fibronectin (3, 4). Also, compared to normal singleton pregnancies, in vitro fertilization (IVF)-conceived singleton pregnancies is associated with higher pregnancy-related complications, including increased risk of cesarean delivery, intrauterine growth restriction, preeclampsia, congenital malformations, low birth weight, and higher risk of PTD (5). Similarly, PTD is more prevalent in IVF-conceived pregnancies as compared with those conceived naturally (6). A meta-analysis of 15 studies showed that the risk of spontaneous preterm birth (PTB) in singleton pregnancies resulting from IVF is significantly higher than that in spontaneously conceived singletons (7). In high-risk women for PTL, the CL is short. Therefore, the CL measurement is used to predict higher-risk pregnancies (8). Data pertaining to the measurement of CL and specifically studies assessing whether the increased risk of spontaneous PTB is predicted by a difference in CL are limited.
Therefore, the aim of this study was to evaluate the predictive value of transvaginal sonographic CL for the prediction of PTD before 37 wk between two groups of spontaneous and IVF pregnancies in asymptomatic women.
2. Materials and Methods
This prospective cohort study included 154 singleton pregnant women who attended the Prenatal Care Clinic and Infertility Clinic at Imam Khomeini Hospital affiliated to the Jundishapur University of Medical Sciences between March 2016 and June 2017 in Ahvaz, Iran. Participants were divided into two groups of spontaneously (n = 77) and IVF-conceived (n = 77) pregnancies. Patients were enrolled at 16-26 wk of gestation and followed up until the delivery. The exclusion criteria of the study included women with multiple pregnancies, placenta previa, cerclage, fetal anomalies, and elective PTL. In both groups, CL was measured from 16 through 26 weeks of gestation using TVU. Sonography was performed by two sonographers who are certified by FMF for CL measurement (V20 Madison). For the TVU, the women were first asked to empty their bladder after which they were placed in the lithotomy position. The sonography probe was inserted in anterior vaginal fornix without pressure. Sagittal cervix was shown and linear distance between internal and external OS was measured. All patients were followed until delivery and demographic data, gestational age at delivery, and CL (mm) at 16-26 weeks of gestation were recorded. Gestational age was determined from the date of the last menstrual period (LMP) and confirmed by the measurement of the CRL. PTL was defined as delivery <37 weeks of gestation in both groups. Pregnancy outcome was obtained from the interview with mothers. For the determination of the cut-off, the Roc analysis was used and the sensitivity, negative and positive predictive values were calculated.
2.1. Ethical considerations
This study was approved by Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (IRAJUMS.REC.1396.889). All participants signed an informed consent form prior to the study.
2.2. Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences, version 18.0, SPSS Inc., Chicago, IL, USA (SPSS). The cut-off was determined according to the Roc analysis. The significance of differences between two groups was assessed using independent t tests and Chi square test. P < 0.05 was considered as statistically significant.
3. Results
A total of 154 pregnant women aged range of 19-46 yr with a mean age of 29.9±4.9 yr in the normal group and 32.18±5.58 yr in the IVF group (p = 0.052) were included in the study. Table I shows the demographic data and outcomes of the pregnancies. The average BMI in the spontaneous and IVF groups is shown in the table mentioned (Table I).The average birth’s weeks in spontaneous group was significantly higher than the IVF group (p < 0.001). Six women in spontaneous group and 18 women in IVF group delivered before 37 weeks.
The mean CL did not significantly differ between while the mean CL did not differ significantly between the PTL and term pregnancies in the normal group, it was significantly lower in the PTL than the term pregnancies in the IVF group. Additionally, the mean CL in the PTL subgroup of spontaneous pregnancy was significantly greater than the mean CL in the PTL subgroup of IVF pregnancy (according to Table II).
The classification of CL according to Table III showed that all patients with CL < 25 mm were preterm, while all patients with CL ≥ 45 mm were term. Therefore, as presented in table IV, the best cut-off points obtained from the ROC curve were ≤ 36 mm for the spontaneous group, with a high negative predictive value (NPV) of 97.9%, low positive predictive value (PPV) of 11.4%, high sensitivity of 83.3%, and low specificity of 46.5% and ≤ 30 mm for the IVF group with a high NPV of 88.4%, low PPV of 57.8%, sensitivity of 63.2%, and low specificity of 86.0%.
According to tables V and VI, the number of cesarean deliveries in the IVF group was 20, of which 12 were term and 8 preterm. The number of cesarean deliveries in the spontaneous group was 10, with 9 term and 1 preterm.
The mean + SD CL for the all the subjects was 36.4 + 7.6 mm (range: 21-70 mm). The CL did not differ significantly between the two groups of IVF and spontaneously-conceived pregnancies (p = 0.06).
Of the 154 patients of the study, 130 (83.7%) were term and 24 (16.4%) PTL. The mean CL in the PTL group was significantly lower than that in the term group (Table III).





4. Discussion
The predictive value of cervical measurement were compared via transvaginal sonography at second trimester (16-26 weeks) for predicting the PTB between the two groups of asymptomatic singleton pregnant women conceived spontaneously or by IVF. The ROC curve was used to suggest best cut-off rather than the percentile of CL measurement. The studies comparing the predictive value of CL for PTB between spontaneous and IVF singleton pregnancies are rare. Many studies have investigated the relationship between CL and PTB adopting different methodologies to obtain the cut-off point, either percentile or ROC curve.
The current study showed that the best cut-off points obtained from the ROC curve were ≤36 mm for the spontaneous group, with a high NPV of 97.9%, low PPV of 11.4%, high sensitivity of 83.3%, and low specificity of 46.5%, and ≤ 30 mm for the IVF group with high NPV 88.4%, low PPV of 57.8%, sensitivity of 63.2%, and low specificity of 86.0%. The most accurate cut-off for a screening test should have a high sensitivity and an adequate PPV and NPV (9). Therefore, our study has confirmed that the TVU CL measurement at the second trimester is a better screening test for spontaneous PTB in naturally conceived pregnancies compared to the IVF ones, since it has higher NVP (97.9% vs 88.4%, respectively).
In our study, the rate of PTB in the IVF group was significantly higher than that in the spontaneous group. These results are strongly in agreement with previously published studies and a large meta-analysis that have reported that the PTB is more prevalent in IVF-conceived pregnancies compare to those conceived spontaneously (5-7, 10, 11). Although, none of the studies so far has presented the clarification for such findings. However, we decided to find out whether IVF and naturally conceived pregnancies differ in CL measured by TVU in the second trimester. The only available meta-analysis showed that the decrease in the length of cervix is associated with the increase in the risk of PTB (12, 13). This conclusion was confirmed in all studies and also in the current study. However, we found that the mean CL did not significantly differ between the spontaneous and IVF groups (p = 0.06). The subgroups analysis showed that the length of cervix in the term and preterm pregnancies in the IVF group showed a significant difference (p = 0.001). In our study, none of the patients in the spontaneous group had a short cervix (CL < 25 mm), however, the rate of short cervix in the IVF group was 11.7%. A cut-off value of ≤36 mm was obtained in our study for predicting the PTB in spontaneous group which is greater than the values reported by other published studies. This discrepancy may be attributed to no case of short cervix in our study. While the lower cut-off point of CL (≤ 30 mm) suggested in our study for predicting PTB in IVF group can be attributed to the rate of short cervix of IVF patients (11.7%). Iams et al. published the first large study of CL measurement at 26 weeks of gestation in singleton pregnancies in 1996 (14). They reported cut-off points of 30, 25, and 20 mm related to the 25th, 10th, and 5th percentile in their studied population according to the ROC curves.
5. Conclusion
In this study, IVF had a significant direct correlation with PTL. In addition, CL had a significant indirect relationship with PTL. The results of this study indicated that CL measurement in the second trimester of pregnancy in women with singleton baby has a lower cut-off for predicting PTD.
Acknowledgements
This article has been extracted from the thesis of Somayeh Ershadian. The author would like to acknowledge the Department of Obstetrics and Gynecology at Imam Khomeini Hospital in Ahvaz.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Fertility & Infertility
References
1. Berghella V, Palacio M, Ness A, Alfirevic Z, Nicolaides KH, Saccone G. Cervical length screening for prevention of preterm birth in singleton pregnancy with threatened preterm labor: systematic review and meta-analysis of randomized controlled trials using individual patient-level data. Ultrasound Obstet Gynecol 2017; 49: 322-329. [DOI:10.1002/uog.17388] [PMID]
2. Sharvit M, Weiss R, Ganor Paz Y, Tzadikevitch Geffen K, Danielli Miller N, Biron-Shental T. Vaginal examination vs. cervical length - which is superior in predicting preterm birth?. J Perinat Med 2017; 45: 977-983. [DOI:10.1515/jpm-2016-0273] [PMID]
3. Leitich H, Brunbauer M, Kaider A, Egarter Ch, Husslein P. Cervical length and dilatation of the internal cervical os detected by vaginal ultrasonography as markers for preterm delivery: A systematic review. Am J Obstet Gynecol 1999; 181: 1465-1472. [DOI:10.1016/S0002-9378(99)70407-2]
4. Saccone G, Zullo F, Roman A, Ward A, Maruotti G, Martinelli P, et al. Risk of spontaneous preterm birth in IVF-conceived twin pregnancies. J Matern Fetal Neonatal Med 2017; 32: 369-376. [DOI:10.1080/14767058.2017.1378339] [PMID]
5. Qin J, Liu X, Sheng X, Wang H, Gao Sh. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril 2016; 105: 73-85.
https://doi.org/10.1016/j.fertnstert.2015.12.131 [DOI:10.1016/j.fertnstert.2015.09.007]
6. Kim D, Saada A. The social determinants of infant mortality and birth outcomes in Western developed nations: a cross-country systematic review. Int J Environ Res Public Health 2013; 10: 2296-2335. [DOI:10.3390/ijerph10062296] [PMID] [PMCID]
7. Cavoretto P, Candiani M, Giorgione V, Inversetti A, Abu-Saba MM, Tiberio F, et al. Risk of spontaneous preterm birth in singleton pregnancies conceived after IVF/ICSI treatment: meta-analysis of cohort studies. Ultrasound Obstet Gynecol 2018; 51: 43-53. [DOI:10.1002/uog.18930] [PMID]
8. Mohamadjafari R, Nagafian M, Vahaby E, Gharibzadeh S. [Correlation between cervical length by transvaginal sonography at 16-24wks of pregnancy and preterm labor.] Stud Med Sci 2013; 24: 441-448. (in Persian)
9. Pasquini L, Sisti G, Nasioudis D, Kanninen T, Sorbi F, Fambrini M, et al. Ability of cervical length to predict spontaneous preterm delivery in twin pregnancies using the receiver-operating characteristic curve analysis and an a priori cut-off value. J Obstet Gynaecol 2017; 37: 562-565. [DOI:10.1080/01443615.2016.1258046] [PMID]
10. Szymusik I, Wegrzyn P, Marianowski P, Dziadecki W, Bablok L, Wielgos M. Is mid-gestational cervical length measurement as sensitive prediction factor of preterm delivery in IVF as in spontaneous singleton pregnancies? Neuro Endocrinol Lett 2011; 32: 453-457.
11. Al-Safi ZA, Shavell VI, Roberts RP, Singh M, Puscheck EE, Diamond MP. First trimester cervical length and preterm delivery in pregnancies conceived through in vitro fertilization. Fertil Steril 2011; 96: S13. [DOI:10.1016/j.fertnstert.2011.07.057]
12. Berghella V, Baxter JK, Hendrix NW. Cervical assessment by ultrasound for preventing preterm delivery. Cochrane Database Syst Rev 2009; 2: CD007235. [DOI:10.1002/14651858.CD007235.pub2]
13. O'Hara S, Zelesco M, Sun Z. Cervical length for predicting preterm birth and a comparison of ultrasonic measurement techniques. Aust J Ultrasound Med 2013; 16: 124-134. [DOI:10.1002/j.2205-0140.2013.tb00100.x] [PMID] [PMCID]
14. Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med 1996; 334: 567-572. [DOI:10.1056/NEJM199602293340904] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |