BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://ijrm.ir/article-1-18-en.html
Introduction
The embryo transfer procedure is the last decisive step of IVF. Embryo transfer is the most inefficient step in IVF provoking bleeding or uterine contractions. Thus until very recently, this technique has received little attention (Fryman et al., 2004).Embryo transfer is an essential step in IVF and ICSI. Factors which appear to influence implantation rates are: contamination of the catheter tip with cervical bacteria, stimulation of uterine contraction during the procedure, the type of catheter, ultrasound guidance during the transfer and the position of the embryos in the uterine cavity (Levi Setti et al., 2003). Numerous attempts to improve the technique of embryo transfer have been described including the need for a gentle and a non-traumatic technique (Vaught et al., 1987) such as performing a trial transfer before the actual procedure, removing the cervical mucus prior to embryo transfer, avoiding the use of a tenaculum, using specific catheters, depositing the embryos near the uterine fundus, using a fibrin sealant, as well as determination of the position and length of
The embryos’ fate in the uterine cavity is beyond our control and not much is known about the location of the embryo after transfer or how much they move before implantation occurs (Englert et al., 1982). An awareness of the position and length of the uterus has been reported to lead to possible improvement in the clinical pregnancy rates in patients undergoing IVF/ICSI cycles (Egbase et al., 1997). However, there is debate in the literature on the optimal site within the uterine cavity to deposit the embryos, whether in the lower uterine cavity (Waterstone et al., 1991), mid-cavity (Agarwal et al., 1997; Vaught et al., 1987), or 5mm from the fondues. This study examined the influence of the position and length of uterus on pregnancy rate, when embryos are routinely deposited 5mm from the fondus in an otherwise classical transcervical embryo transfer procedure (Agarwal et al., 1997).
Material and Methods
This was a retrospective, randomized controlled trial study of 80 infertile women attending IVF/ICSI Embryo transfer in the period of September to December 2003 at the IVF research center, Yazd Medical University, Iran.
Inclusion criteria were age <38 and normal uterus on hysterosalpingography (HSG), hysteroscopy and/or pelvic vaginal ultrasonography.
Ovarian stimulation protocol:
Controlled ovarian stimulation was achieved using a long down-regulation protocol followed by HMG stimulation (Pergonal, Menopure, Humegon, Organon; Wittland, Germany).
Monitoring was effected by serial ultrasonography and HCG (Profasi, Serono; Germany) 10,000 IU was administered by IM injection when the leading follicle reached 18 mm in diameter, as described elsewhere. Oocyte retrieval was performed 36 hours later through the transvaginal ultrasound-guided route.
Embryos were transferred 48 hours after retrieval. 100 mg/progesterone IM was administered daily to provide the luteal phase support. The serum β-HCG concentration was measured 2 weeks after embryo transfer. Clinical pregnancy was defined as the observation of a fetus with a pulsing heart at 8 weeks after ET.
All patients received gonadotropin releasing hormone (GnRH, Buserlin, Hoechst, Germany) analog administered in the previous mid-luteal phase to achieve pituitary desensitization.
The patients were randomly allocated into two groups. With group A (n=40), the length and position of the uterus was determined by using steril spaculum and hystrometer and was recorded. In the control group B (n = 40), the length and position of uterus were not investigated.
Trans cervical intra uterine embryo transfer in 15-25ml of culture medium (Albomin Bayer, Corporation, U.S.A), was performed on all patients 48 hours after oocyte retrieval by using a labotect embryo replacement catheter (Labotect GmbH/72 h, Gottingen, Germany). This catheter was marked with 1 cm graduation allowing the clinician to advance it to 5mm from the uterine fondues based on the previously determined length of the uterine cavity from the external cervical OS.
Thus, the embryos were routinely deposited 5mm from the fondues irrespective of the length of the uterine cavity. The entire embryos transfer procedure was performed in the modified lithotomy position and patients with anteverted uterine had half-full bladder prior to the embryo transfer. Then the clinical pregnancy rate was evaluated in both groups.
Statistical analysis
Data analysis was performed by using chi-square, fisher-exact and ANOVA tests. The statistical significant was defined at P≤0.05. The pregnancy rate was compared according to the length and position of the uterus in group A and then in both groups as a whole.
Results
There were no significant differences in the mean age, duration of infertility and clinical pregnancy in both groups.
The mean age and duration of infertility in the study group (A) and control group (B) were 28.5±4.4, 27.8±2.2 and 7±3.4, 8.7±5.4 respectively. There were no significant differences. In 14 (35%) women in group A, the uterus was retroverted and in 26 (65%) the uterus was anteverted.
The clinical pregnancy rate was marginally higher in the women with anteverted uteri (15% versus 10%), but the difference was not statistically significant (Table I) ( P= 0.764).
The incidence of difficult transfer was similar in both uterine positions.
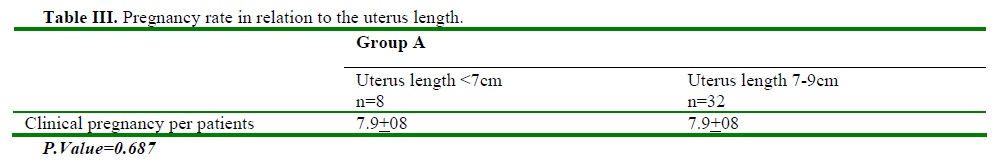
In group A (the study group) the mean length of uterine cavity in pregnant women was 7.9±0.8 and in non-pregnant women was 7.8±0.5. The clinical pregnancy rate in relation to the uterine length was not statistically significant (P= 0.687) (Table III). There were no ectopic pregnancies (EP) in both groups.


The pregnancy rate in group A was 25% and in group B was 22.5% but the difference was not statistically significant (table II).
Discussion
According to the results of the study, the pregnancy rate was marginally higher in the study group (A) than the control group (B), but the difference was not statistically significance.
There were no ectopic pergancies in both groups while some of the patients had uterine length <7cm. Thus the results do not support Lesly et al study (1999) in that they found statistically significant higher ectopic pregnancy in patients with small uterine cavity <7cm compared with patients with normal uterine cavity lengths. They suggest that ectopic pregnancy may be related to the size of the uterine cavity but is not necessarily exclusive of the clinical technique of placing the embryos 5 mm from the fondues in IVF-embryo transfer as previously suggested (Yovich and et al., 1985; Nazav et al., 1993). However their study is probably the first report in the medical literature implicating the size of the uterine cavity in the etiology of ectopic pregnancy. Difficult embryo transfer probably increases the odds ratio for ectopic pregnancy in IVF-embryo transfer, but not the size of the uterus. In regard to the position of the uterus, the results of our study indicate that the patients with retroverted uterus had lower pregnancy rate compared with anteverted uterus (10% versus 15%) which was not statistically significant. Thus we conclude that the position of uterus (anteverted or retroverted) does not adversely affect implantation or clinical pregnancy rate.
Further studies are required to examine the in-depth role of position and length of the uterus or any mechanisms in relation to pregnancy rate.
Acknowledgement
We would like to thank Miss A Kermani and Mrs M Shirvani for their help in the preparation of the data.
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |




