Tue, Apr 30, 2024
[Archive]
Volume 20, Issue 7 (July 2022)
IJRM 2022, 20(7): 529-538 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tabatabai R S, Asadi L, Mohammadi M, Rahmani M, Rezaeian E, Ghasemi F et al . Prenatal and clinical characteristics of pregnant women infected with COVID-19 in Yazd, Iran: A multicenter cross-sectional study. IJRM 2022; 20 (7) :529-538
URL: http://ijrm.ir/article-1-2260-en.html
URL: http://ijrm.ir/article-1-2260-en.html
Razieh Sadat Tabatabai1 

 , Leila Asadi *
, Leila Asadi * 

 2, Maryam Mohammadi3
2, Maryam Mohammadi3 

 , Mina Rahmani1
, Mina Rahmani1 

 , Elahe Rezaeian4
, Elahe Rezaeian4 

 , Fatemeh Ghasemi5
, Fatemeh Ghasemi5 

 , Mohammad Javad Tarahi6
, Mohammad Javad Tarahi6 




 , Leila Asadi *
, Leila Asadi * 

 2, Maryam Mohammadi3
2, Maryam Mohammadi3 

 , Mina Rahmani1
, Mina Rahmani1 

 , Elahe Rezaeian4
, Elahe Rezaeian4 

 , Fatemeh Ghasemi5
, Fatemeh Ghasemi5 

 , Mohammad Javad Tarahi6
, Mohammad Javad Tarahi6 


1- Department of Gynecology and Obstetrics, Mother and Newborn Health Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Department of Midwifery, Research Center for Infection Disease, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran. , l_asadi66@yahoo.com
3- Department of Midwifery, Research Center for Nursing and Midwifery Care, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
5- Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
6- Departments of Epidemiology and Biostatistics, Isfahan University of Medical Sciences, Isfahan, Iran.
2- Department of Midwifery, Research Center for Infection Disease, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Isfahan University of Medical Sciences, Isfahan, Iran. , l_asadi66@yahoo.com
3- Department of Midwifery, Research Center for Nursing and Midwifery Care, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
5- Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
6- Departments of Epidemiology and Biostatistics, Isfahan University of Medical Sciences, Isfahan, Iran.
Full-Text [PDF 288 kb]
(562 Downloads)
| Abstract (HTML) (872 Views)
1. Introduction
Coronavirus disease-2019 (COVID-19) is a disease that has been associated with a rapid increase in morbidity and mortality since its first diagnosis in Wuhan, China in December 2019. The outbreak of COVID-19 became a major epidemic in China from February 2020 (1) and then spread rapidly worldwide. In January 2020, the World Health Organization issued a statement identifying the new coronavirus as the 6th leading cause of public health emergencies worldwide and identifying the new coronavirus as a threat to all countries (2 3). The World Health Organization's International Classification Committee has identified the causative agent of COVID-19 as the SARS-cov-2 virus (4). The China National Health Commission published a set of guidelines for the prevention, diagnosis, and treatment of COVID-19 pneumonia, as well as epidemiological and clinical features (5). Following the outbreak of the coronavirus crisis worldwide, the outbreak of the virus in Iran was officially confirmed by health officials in February 2020 (6), although cases of suspected COVID-19 disease had been previously reported (7, 8).
The spread of COVID-19 is mainly caused by respiratory droplets transmitted from the infected person by coughing or sneezing, similar to influenza or other respiratory conditions. There are a wide range of symptoms, from general to severe respiratory illness and death (9). COVID-19 can be transmitted to others even from a carrier without symptoms (10). According to studies, the average incubation period in this disease is 5 days (range: 2-14 days) and its symptoms include fever, cough, myalgia, headache, diarrhea and gastrointestinal symptoms. Also, according to the findings, Acute Distress Respiratory Syndrome (SARS) occurs in 27-29% of hospitalized patients. In general, the mortality rate of this disease seems to be 1%. However, it seems that based on new data there may be higher mortality rates (11).
Limited information is available on the incidence of COVID-19 during pregnancy. However, information on other diseases associated with highly pathogenic coronaviruses such as SARS and Middle East Respiratory Syndrome can be useful in raising awareness of the effects of COVID-19 during pregnancy. Various studies have shown that emerging infections can have a significant impact on the health of pregnant women and their fetuses (12, 13). For example, in 2009 some maternal and fetal complications increased with the outbreak of the H1N1 influenza virus (14, 15). In times of rapidly increasing incidence of disease that could have a significant impact on the general health of the community and the medical infrastructure, the needs of pregnant women should be included as a matter of urgency in preparedness and response programs. In similar outbreaks in the past, we have seen that physicians are sometimes reluctant to treat or vaccinate pregnant women due to concerns about fetal safety (16). In establishing monitoring systems for COVID-19 cases, it is essential to collect and report information on clinical findings in pregnancy as well as maternal and fetal outcomes (11).
Therefore, the aim of this study was to evaluate the clinical and prenatal findings of pregnant women with COVID-19.
2. Materials and Methods
In this cross-sectional study, all women with COVID-19 referred to 6 mother and child care centers in Yazd city, Iran were studied. The study population consisted of women who were registered on the national system of the Medical Care Monitoring Center for high-risk pregnant women from the beginning of March 2020 (the beginning of the virus epidemic in Iran) until the end of September 2020. Data were collected using a demographic questionnaire and a researcher-made data collection checklist in accordance with the research variables (which were based on previous studies and adjusted according to the research objectives).
All recorded data of pregnant women with COVID-19 at the Medical Care Monitoring Center for high-risk pregnant women were collected during the mentioned period. The participant's clinical condition was extracted based on their documents. In cases of incomplete information, physicians and caregivers were asked to complete the information.
The inclusion criteria in the present study were: COVID-19+ pregnant women of any gestational age who were registered in the medical care monitoring system of high-risk mothers, having symptoms of COVID-19 according to the diagnostic algorithms in pregnancy announced by the Ministry of Health. The exclusion criteria included files that did not have enough data and were unable to complete.
2.1. Ethical considerations
The present study is the result of a research project approved in the second session of reviewing the research projects participating in the call for obtaining a COVID-19 grant from Shahid Sadoughi University of Medical Sciences, Yazd, Iran with letter number 19239 dated 25/4/2020. It also has an ethics code in the bioethics system (Code: IR.SSU.REC.1399.050).
2.2. Statistical analysis
The research data were categorical and numerical (discrete and continuous). Due to the fact that in this study we examined the cases, the data were not normalized and were measured by rank, nominal and relative scales. Descriptive statistics methods (mean, maximum, minimum, standard deviation, frequency distribution) were used to analyze the data and an error of 0.05 was considered for all tests. The Statistical Package for the Social Sciences (SPSS) version 16 was used (IBM, USA, 2007).
3. Results
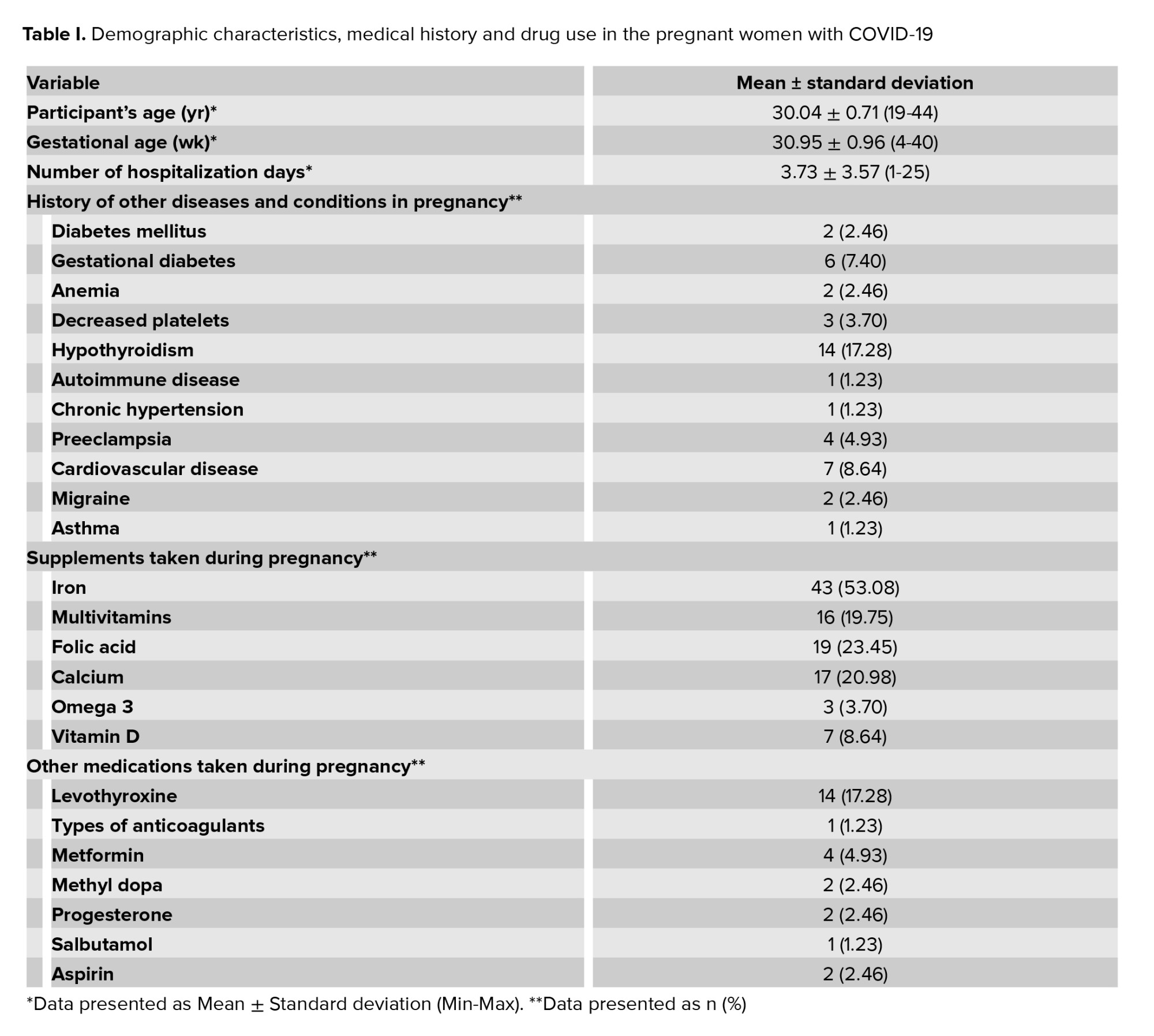
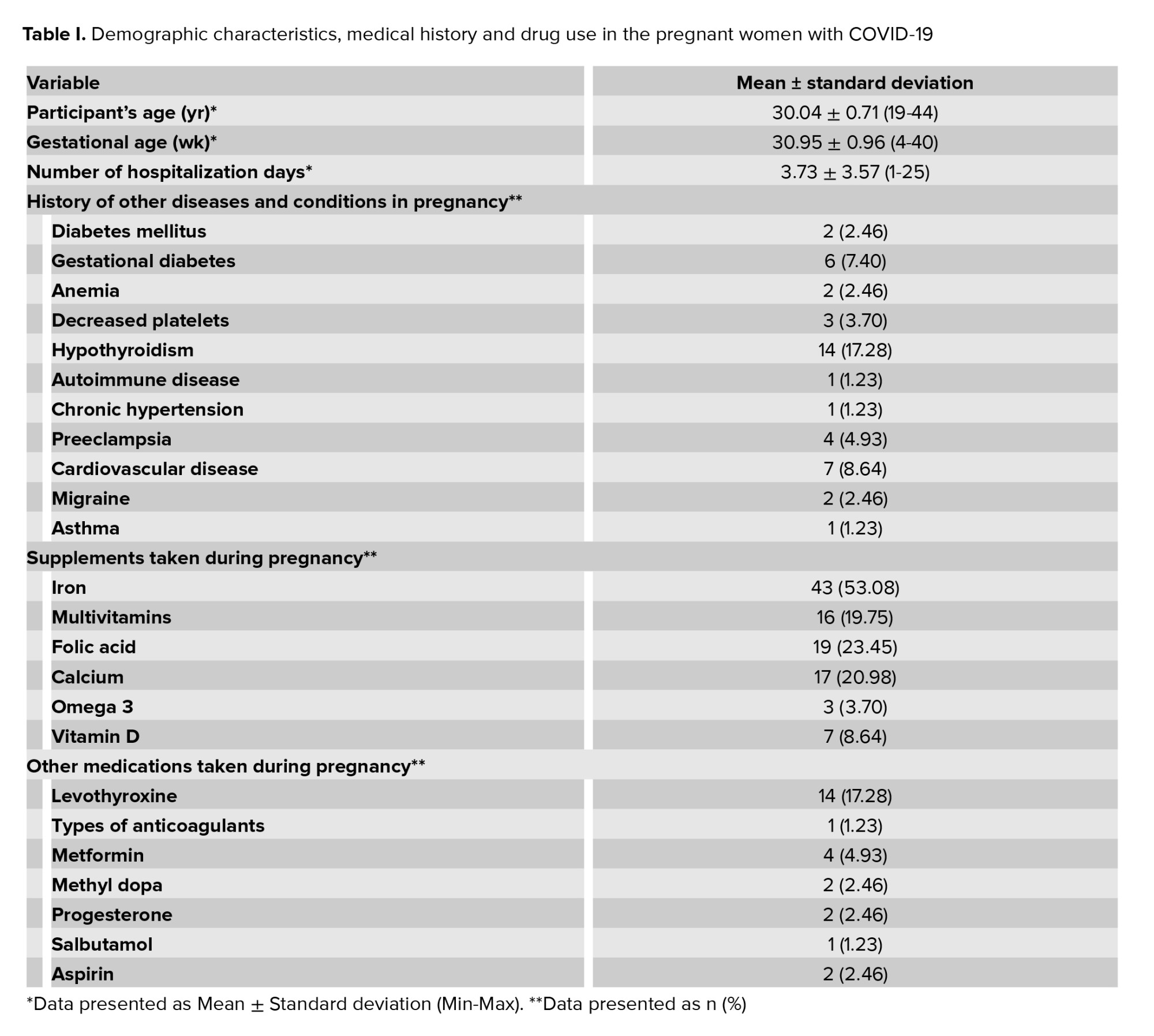
A total of 81 pregnant women with COVID-19 from 6 mother and child care centers were studied according to the inclusion criteria. Of these, 73 (90.1%) were hospitalized in public hospitals and 8 (9.9%) in private hospitals. 24 participants were first gravid, 21 were second, 18 were third gravid, and 18 participants were ≥ 4th. The mean age of the pregnant women was 30.04 ± 0.71 yr with a gestational age of 4-40 wk, and in hospitalized participants, a mean age of the pregnancy was 30 wk (Table I). Based on the results, the average number of hospitalization days in women was 3.73 ± 40.00 days (Table I). Data examination showed that 46 (56.79%) women had a history of contact with a person infected with the virus. Other family members were infected in 35 cases (43.20%). Examination of the medical records of the pregnant women showed that the most commonly reported diseases in the pregnant women were, in order of frequency, hypothyroidism, cardiovascular disease, and gestational diabetes (Table I).
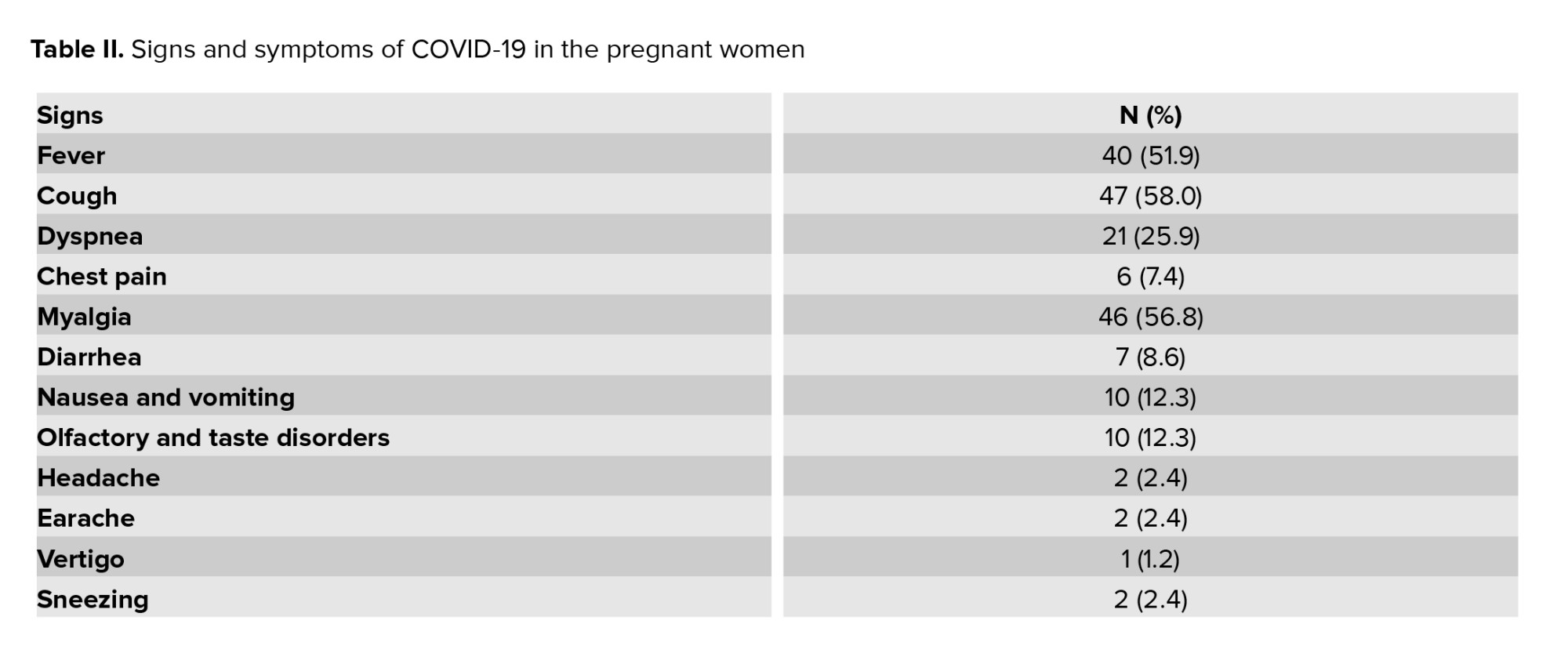
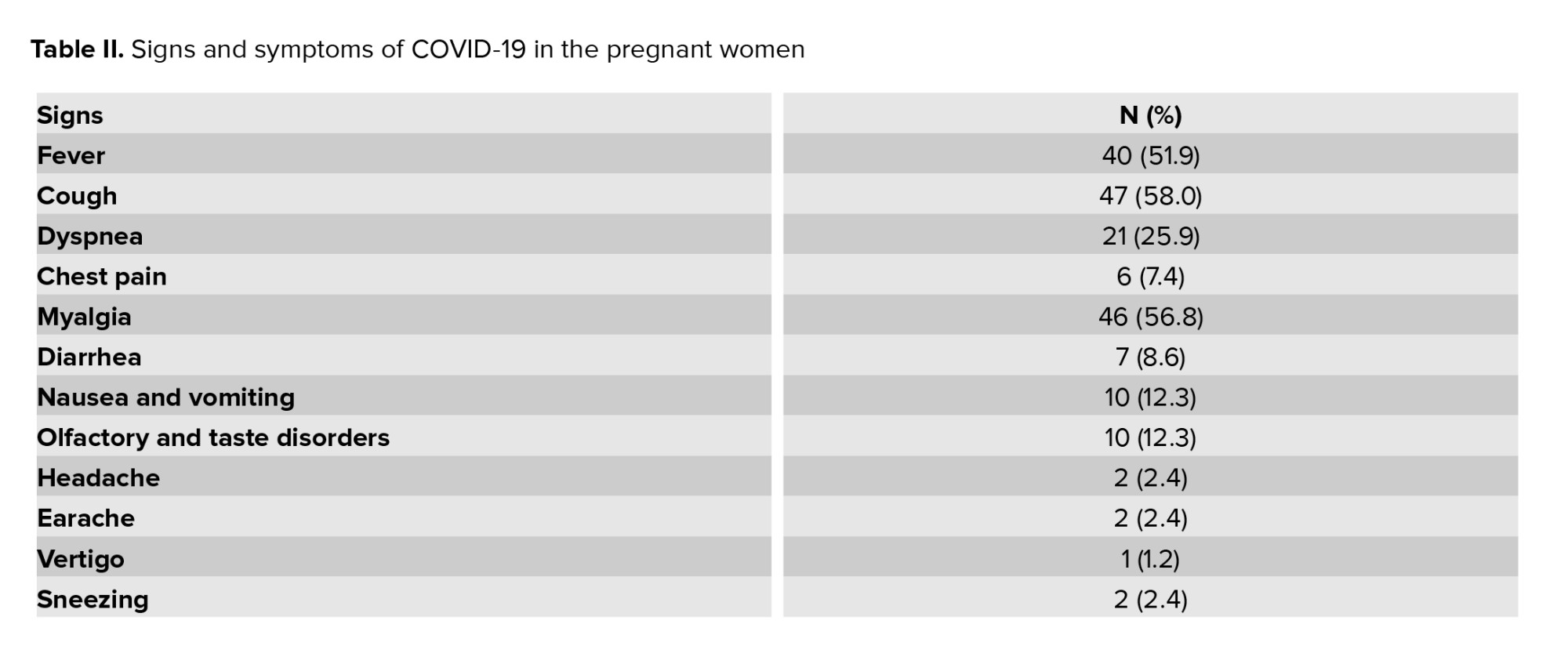
Participants’ symptoms were examined at the time of referral and it was found that, in order of frequency, dry cough, myalgia and fever had the highest prevalence of the symptoms (Table II).
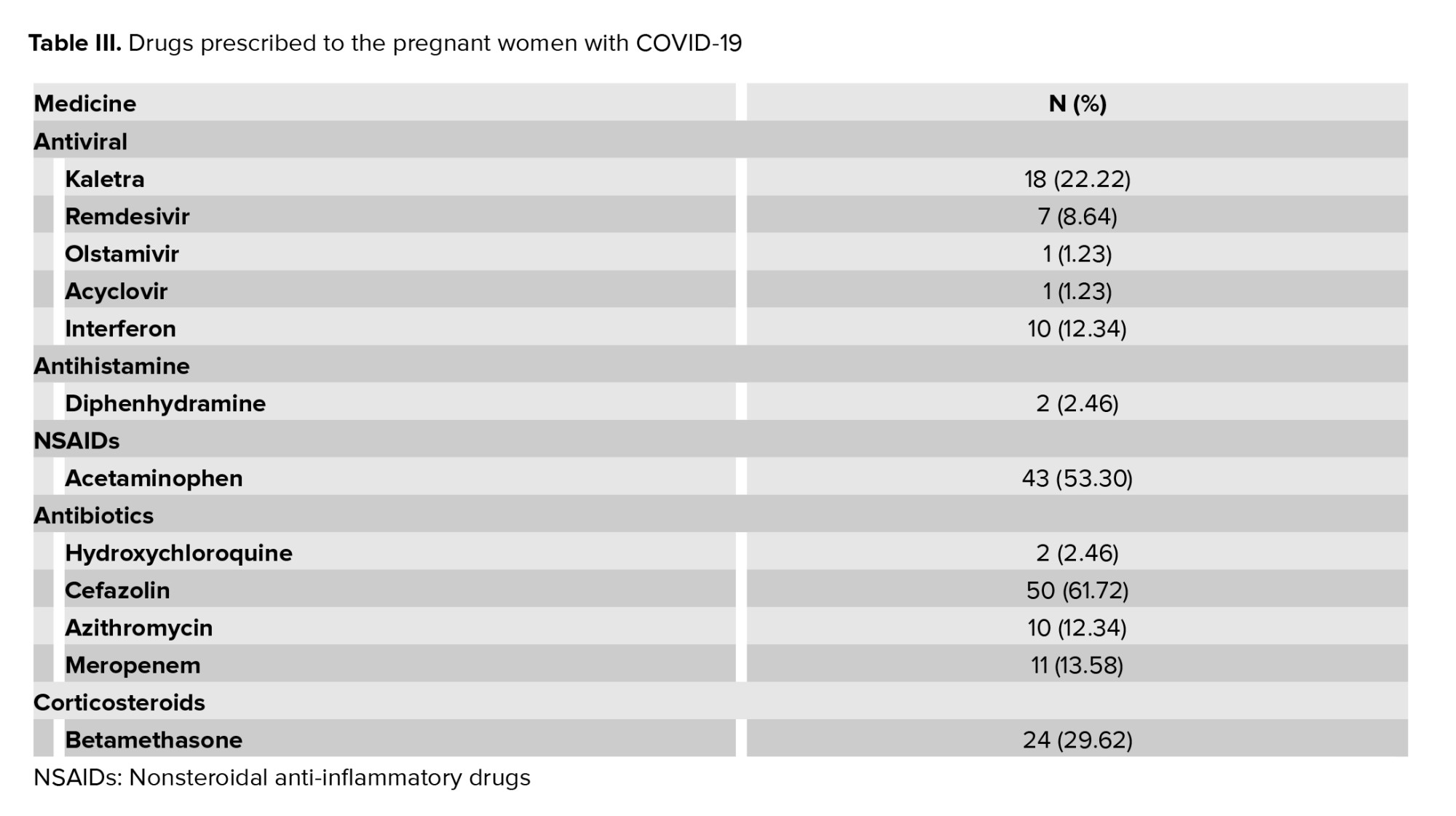
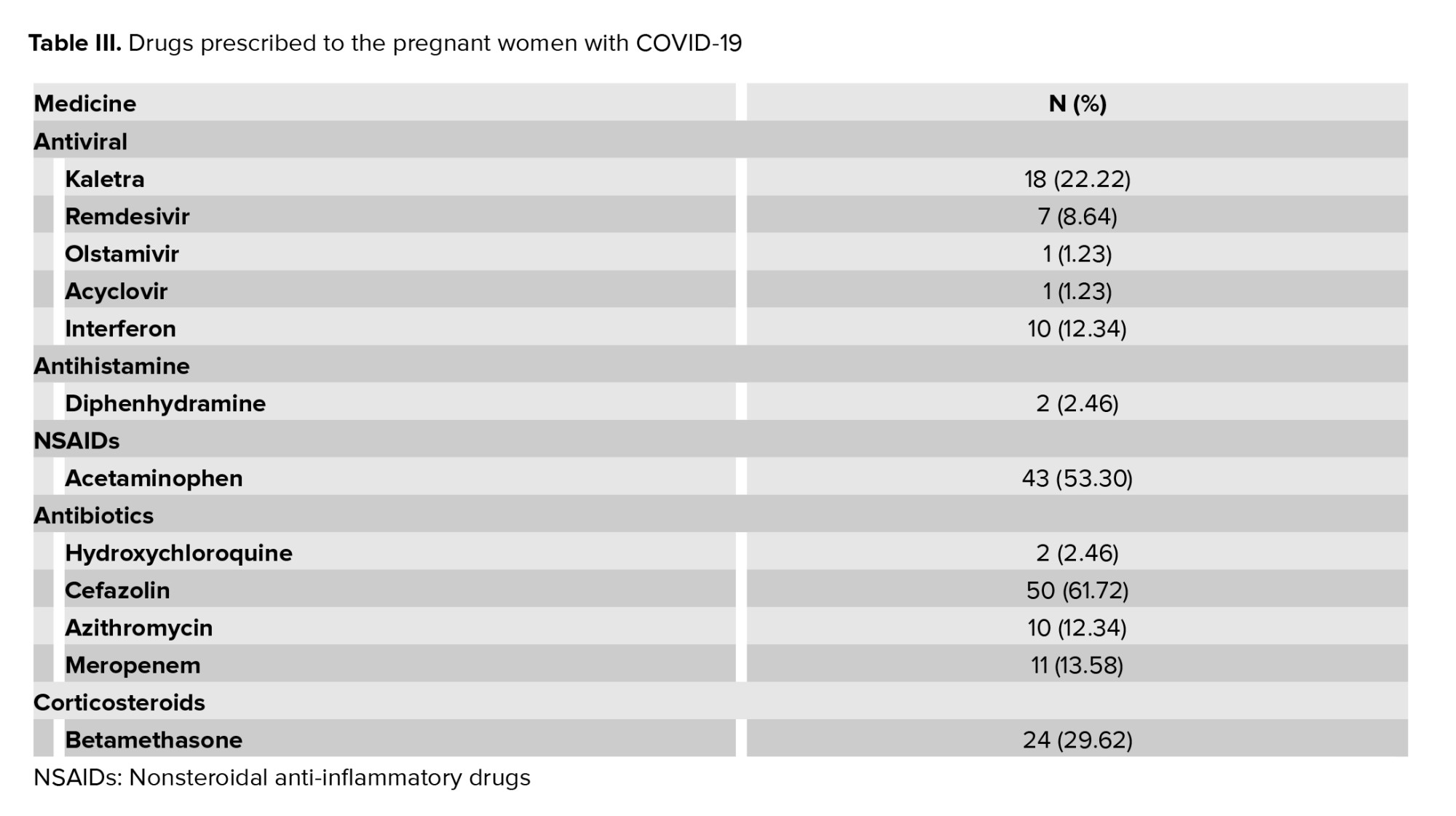
The results of the laboratory findings showed that the most reported disorder was related to an increase in C-reactive protein (CRP) (55 [67.90%]). Lymphopenia, elevated liver enzymes, and decreased white blood cells were seen in 15 (18.51%), 15 (18.51%), and 22 (27.61%) cases, respectively. The pulmonary findings showed that in 28 (34.56%) cases the blood oxygen saturation level was ≤ 95% and in 53 (65.43%) was > 95%. Of the 16 cases examined by lung CT scan, 13 (81.25%) had pulmonary involvement. 32 (39.50%) women received supportive oxygenation and 12 (14.8%) were referred to the intensive care unit for further services. According to our study, 2 (2.46%) cases used mechanical ventilation and no deaths were reported. The prescribed drugs were categorized into 5 groups: antivirals, antihistamines, nonsteroidal anti-inflammatory drugs, antibiotics, and corticosteroids. In total, the most commonly prescribed drugs were cefazolin, acetaminophen, betamethasone, Keltra, meropenem, interferon, and azithromycin, in order of frequency (Table III).
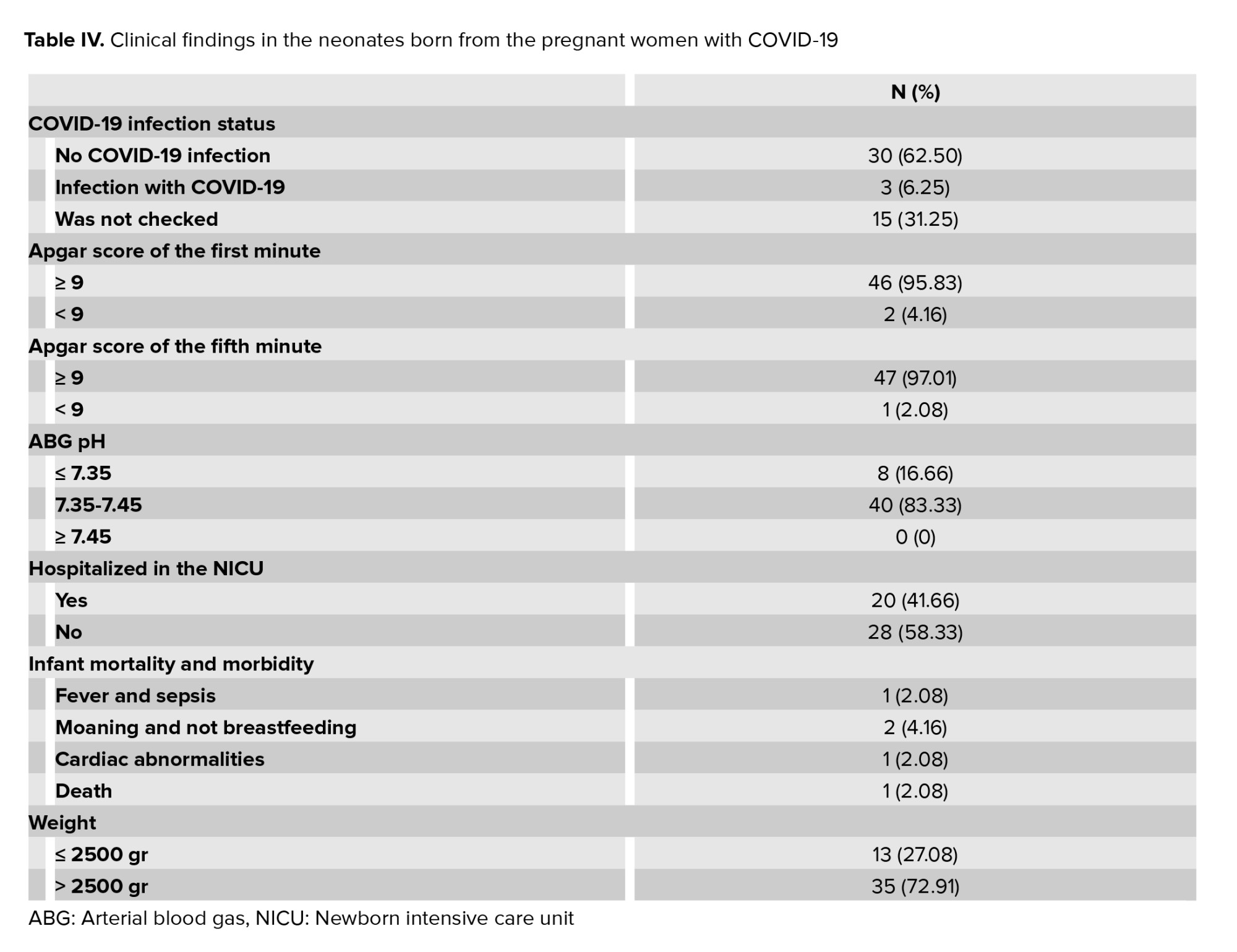
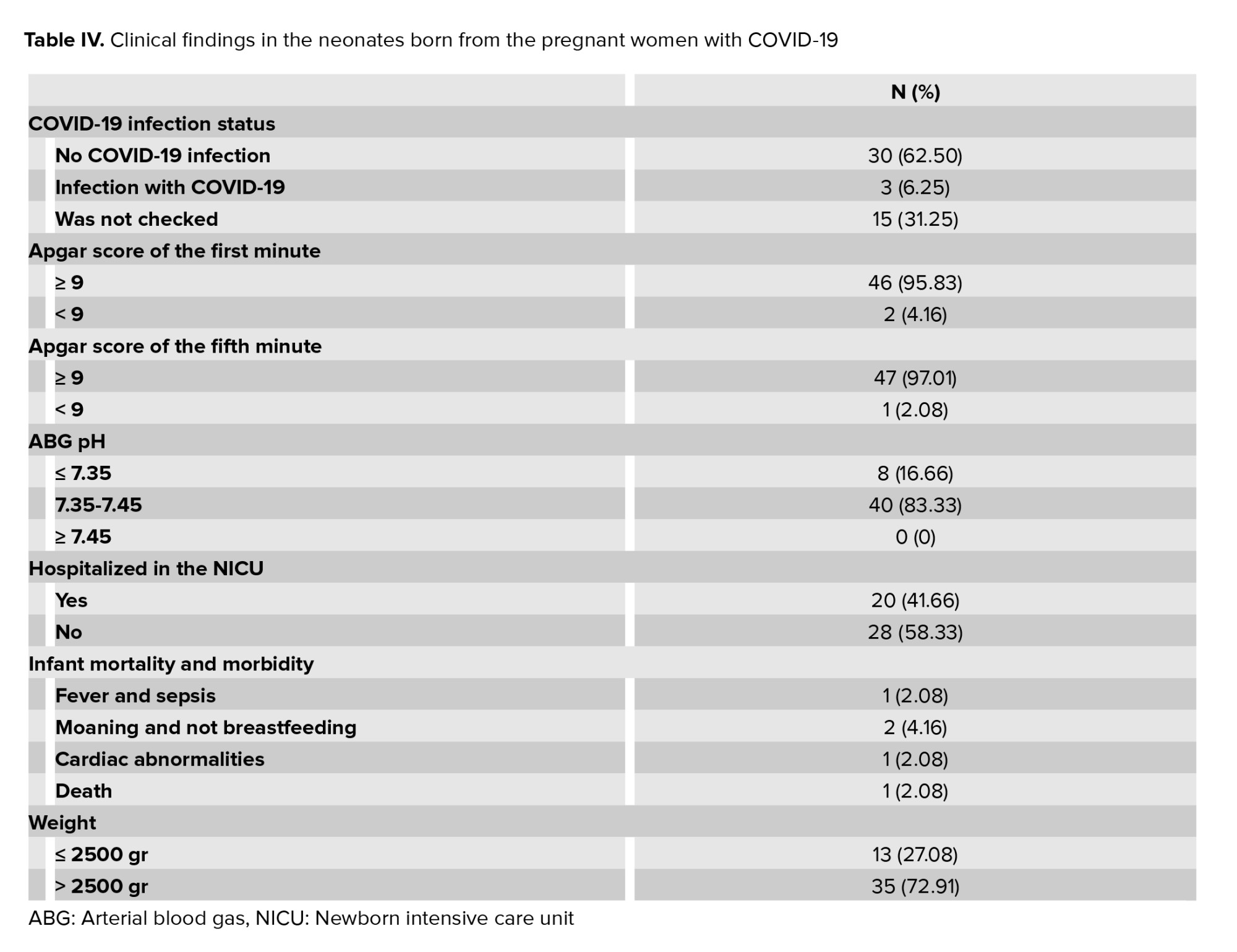
The perinatal findings showed that 48 out of the 81 women gave birth during the study period and the rest of the women were discharged after receiving hospital treatment or were still hospitalized at the end of the study period. Out of the 48 deliveries, 29 deliveries were performed by cesarean section and 19 deliveries by normal vaginal delivery, of which 25% were preterm deliveries. Participant management showed that in 34 cases, breastfeeding started immediately after delivery, following approved health protocols and provided training. 31 of the women were discharged from hospital without childbirth and 2 cases were discharged from hospital after spontaneous and missed abortions at wk 17 and 18. The case study showed that in 24 cases the pregnancy was terminated, of which only in 4 cases was the COVID-19 infection the main reason for termination. Other causes of termination were: fetal distress, preeclampsia, miscarriage, placental abruption, intrauterine fetal death, and fetal abnormalities (7, 5, 5, 1, 1, and 1, respectively). The demographic characteristics of the infants born from the infected mothers showed that the mean age of the infants at birth was 30.95 ± 0.96 wk with a mean neonatal weight of 2.63 ± 30.804 kg. Out of the 48 deliveries, 20 cases were boys and 28 cases were girls. A total of 33 infants were examined for infection using their amniotic fluid and cord blood. 3 cases had COVID-19 and 30 cases were healthy. The neonatal clinical findings showed that 3 neonates had intrauterine growth restriction. Evaluation of the 1st and 5th min newborn Apgar scores showed that the 1st min Apgar score in 2 infants and the 5th min Apgar score in 1 infant were < 9. In relation to arterial blood gas (ABG) pH, the pH level of 8 infants was ≤ 7.35. Finally, a total of 20 infants needed to be admitted to the neonatal intensive care unit (Table IV).
4. Discussion
In the present study, 81 pregnant women with COVID-19 were clinically evaluated from 6 centers. The aim of this study was to evaluate the clinical and prenatal findings of pregnant women with COVID-19. Regarding the clinical findings of the participants, the most common symptoms reported at the time of admission were dry cough, muscle aches, myalgia, fever, sore throat, and dyspnea. In other studies (17-19), the most common symptoms found were fever, cough, shortness of breath, fatigue, and myalgia, which is generally consistent with the results of our research. The results of our study and literature review showed that fever, cough, and myalgia are the most common symptoms of COVID-19 in pregnant women.
According to the laboratory findings, the most commonly reported disorders were increased CRP, lymphopenia, decreased white blood cells, and increased liver enzymes. In previous studies (20-23), (24)an increase in CRP was also reported, which is in line with the results of our research. One study showed that an increase in CRP was seen in 45.7% of cases (24). Also, leukopenia, lymphopenia, increased aspartate aminotransferase and increased creatine kinase were found in another study (25). It seems that the discrepancies in the laboratory findings may be due to the limited number of participants examined in some studies.
Examination of the participants pulmonary findings showed that in 28 cases, the blood oxygen saturation level was equal to or less than 95%. Of the 16 cases examined by lung CT scan, 13 cases had pulmonary involvement. Moreover, 32 cases needed supportive oxygenation, and 12 were referred to the intensive care unit for additional services. According to our study, 2 cases used mechanical ventilation, and no maternal deaths were reported. A previous meta-analysis showed that the rate of severe pneumonia in the women they examined ranged from 0-14%, and most cases required admission to the intensive care unit. In this study, invasive mechanical ventilation was needed in only a few cases. 2 cases of maternal death were reported in another Iranian study (24).
The most commonly prescribed drugs in the present study were cefazolin, non-steroidal anti-inflammatory drugs (acetaminophen), corticosteroids (betamethasone), and antivirals (Kaletra), in order of frequency. The most prescribed drugs for treating COVID-19 were ribavirin and arubidol. Ceftzol sodium and ceftriaxone were also used to prevent bacterial infections during the cesarean section for pregnant participants. Dexamethasone was used to mature the fetal lung. It should be noted that sodium heparin was used to prevent thrombosis, and diamine glycyrrhizinate was used to protect liver function (25). In the previously mentioned meta-analysis, the drugs prescribed to participants were: 70.7% antibiotics, 37.8% antiviral therapy, 17.6% corticosteroids, and 2 cases of hydroxychloroquine (24). The comparison of prescription drugs in medical centers in our study with other studies shows that most prescribed drugs were similar despite different regional treatment protocols.
In the present study, preterm labor occurred in 25% of cases. In 4 pregnancies, COVID-19 was the main reason for termination of pregnancy. In this regard, most other studies have demonstrated an increase in preterm delivery following COVID-19 (20). In other studies, preterm labor was reported in 6 out of 10 pregnancies (26), and in 6 out of 9 pregnancies (27). It seems that this increase in the number of preterm deliveries could be due to complications from COVID-19. In our study, fetal distress was the second leading cause of termination of pregnancy.
Examination of participant's management showed that in 34 cases, immediately after delivery, breastfeeding was started in accordance with approved health protocols and provided training. A review of the literature in this regard suggests 2 types of care approaches. In some studies, the mother and infant were quarantined and separated for 14 days, and breastfeeding did not occur (25). In other studies, breastfeeding was performed with strict health recommendations and supervision (28-30).
A total of 33 infants were screened for COVID-19. The examination was performed through the amniotic fluid and cord blood. 3 cases of COVID-19 and 30 healthy cases were reported. In this regard, in many other studies, vertical infection did not occur in any of the infants, and there is no evidence proving that vertical transmission can occur (25, 31). Despite the results of these studies, a meta-analysis showed that out of 163 participants, according to samples taken from amniotic fluid, placenta, and/or umbilical cord blood, 10 were positive for the SARS-CoV-2 virus, 61 newborns were positive for SARS-CoV-2, and 4 out of 92 breastmilk samples showed evidence of SARS-CoV-2. Therefore, according to the results of our study and the meta-analysis, it seems that vertical transfer is not impossible (30).
Examination of the neonatal clinical findings showed that 3 of the newborns had fetal growth restriction. Examination of the neonates’ first minute and 5th min Apgar scores showed that 2 infants had a 1st min Apgar score < 9. Also, the 5th min Apgar score in one infant was < 9. In relation to the ABG pH, in 8 infants the pH level was lower than or equal to 7.35. Finally, a total of 20 infants needed to be admitted to the neonatal intensive care unit. A similar study showed that the Apgar score of the examined newborns in the first minute was 8-9 and in the 5th min was 9-10 (27).
The most important limitation of the present study was the lack of a long follow-up period for pregnant women to evaluate the consequences of the COVID-19 virus. In this regard, the researchers suggest that future studies are conducted to investigate the long-term consequences on motherhood and infancy. Also, the present study was a case study, and testing to assess the incidence of COVID-19 in infants born in the province's hospitals was not mandatory according to national guidelines. As a result, another limitation of the study was that not all infants born to infected mothers were tested for COVID-19. It is therefore suggested that future studies examine the incidence of COVID-19 in infants according to the approved tests. Also, the relationship between infant infection and neonatal complications and consequences should be examined.
5. Conclusion
The present study’s results showed that the most common symptoms of pregnant women with COVID-19 when visiting medical centers are: dry cough, muscle aches, myalgia and fever. These symptoms are similar to those in other adults. The most common laboratory findings in the affected women were increased CRP, lymphopenia, decreased white blood cells, and increased liver enzymes. The most common medical disorders in these women were hypothyroidism, cardiovascular disease, and diabetes. 33 infants were screened for COVID-19, 3 of whom had COVID-19, which may be evidence of vertical transmission.
Acknowledgments
The authors would like to thank all the participants whose information was used for this study and all the colleagues at the health centers who helped us gather the information. The present study is the result of a research project approved in the second session of reviewing the research projects participating in the call for obtaining a COVID-19 grant from Shahid Sadoughi University of Medical Sciences, Yazd, Iran with letter number 19239 dated 25/4/2020.
Conflict of Interest
The authors declare that there is no conflict of interest.
Full-Text: (158 Views)
1. Introduction
Coronavirus disease-2019 (COVID-19) is a disease that has been associated with a rapid increase in morbidity and mortality since its first diagnosis in Wuhan, China in December 2019. The outbreak of COVID-19 became a major epidemic in China from February 2020 (1) and then spread rapidly worldwide. In January 2020, the World Health Organization issued a statement identifying the new coronavirus as the 6th leading cause of public health emergencies worldwide and identifying the new coronavirus as a threat to all countries (2 3). The World Health Organization's International Classification Committee has identified the causative agent of COVID-19 as the SARS-cov-2 virus (4). The China National Health Commission published a set of guidelines for the prevention, diagnosis, and treatment of COVID-19 pneumonia, as well as epidemiological and clinical features (5). Following the outbreak of the coronavirus crisis worldwide, the outbreak of the virus in Iran was officially confirmed by health officials in February 2020 (6), although cases of suspected COVID-19 disease had been previously reported (7, 8).
The spread of COVID-19 is mainly caused by respiratory droplets transmitted from the infected person by coughing or sneezing, similar to influenza or other respiratory conditions. There are a wide range of symptoms, from general to severe respiratory illness and death (9). COVID-19 can be transmitted to others even from a carrier without symptoms (10). According to studies, the average incubation period in this disease is 5 days (range: 2-14 days) and its symptoms include fever, cough, myalgia, headache, diarrhea and gastrointestinal symptoms. Also, according to the findings, Acute Distress Respiratory Syndrome (SARS) occurs in 27-29% of hospitalized patients. In general, the mortality rate of this disease seems to be 1%. However, it seems that based on new data there may be higher mortality rates (11).
Limited information is available on the incidence of COVID-19 during pregnancy. However, information on other diseases associated with highly pathogenic coronaviruses such as SARS and Middle East Respiratory Syndrome can be useful in raising awareness of the effects of COVID-19 during pregnancy. Various studies have shown that emerging infections can have a significant impact on the health of pregnant women and their fetuses (12, 13). For example, in 2009 some maternal and fetal complications increased with the outbreak of the H1N1 influenza virus (14, 15). In times of rapidly increasing incidence of disease that could have a significant impact on the general health of the community and the medical infrastructure, the needs of pregnant women should be included as a matter of urgency in preparedness and response programs. In similar outbreaks in the past, we have seen that physicians are sometimes reluctant to treat or vaccinate pregnant women due to concerns about fetal safety (16). In establishing monitoring systems for COVID-19 cases, it is essential to collect and report information on clinical findings in pregnancy as well as maternal and fetal outcomes (11).
Therefore, the aim of this study was to evaluate the clinical and prenatal findings of pregnant women with COVID-19.
2. Materials and Methods
In this cross-sectional study, all women with COVID-19 referred to 6 mother and child care centers in Yazd city, Iran were studied. The study population consisted of women who were registered on the national system of the Medical Care Monitoring Center for high-risk pregnant women from the beginning of March 2020 (the beginning of the virus epidemic in Iran) until the end of September 2020. Data were collected using a demographic questionnaire and a researcher-made data collection checklist in accordance with the research variables (which were based on previous studies and adjusted according to the research objectives).
All recorded data of pregnant women with COVID-19 at the Medical Care Monitoring Center for high-risk pregnant women were collected during the mentioned period. The participant's clinical condition was extracted based on their documents. In cases of incomplete information, physicians and caregivers were asked to complete the information.
The inclusion criteria in the present study were: COVID-19+ pregnant women of any gestational age who were registered in the medical care monitoring system of high-risk mothers, having symptoms of COVID-19 according to the diagnostic algorithms in pregnancy announced by the Ministry of Health. The exclusion criteria included files that did not have enough data and were unable to complete.
2.1. Ethical considerations
The present study is the result of a research project approved in the second session of reviewing the research projects participating in the call for obtaining a COVID-19 grant from Shahid Sadoughi University of Medical Sciences, Yazd, Iran with letter number 19239 dated 25/4/2020. It also has an ethics code in the bioethics system (Code: IR.SSU.REC.1399.050).
2.2. Statistical analysis
The research data were categorical and numerical (discrete and continuous). Due to the fact that in this study we examined the cases, the data were not normalized and were measured by rank, nominal and relative scales. Descriptive statistics methods (mean, maximum, minimum, standard deviation, frequency distribution) were used to analyze the data and an error of 0.05 was considered for all tests. The Statistical Package for the Social Sciences (SPSS) version 16 was used (IBM, USA, 2007).
3. Results
A total of 81 pregnant women with COVID-19 from 6 mother and child care centers were studied according to the inclusion criteria. Of these, 73 (90.1%) were hospitalized in public hospitals and 8 (9.9%) in private hospitals. 24 participants were first gravid, 21 were second, 18 were third gravid, and 18 participants were ≥ 4th. The mean age of the pregnant women was 30.04 ± 0.71 yr with a gestational age of 4-40 wk, and in hospitalized participants, a mean age of the pregnancy was 30 wk (Table I). Based on the results, the average number of hospitalization days in women was 3.73 ± 40.00 days (Table I). Data examination showed that 46 (56.79%) women had a history of contact with a person infected with the virus. Other family members were infected in 35 cases (43.20%). Examination of the medical records of the pregnant women showed that the most commonly reported diseases in the pregnant women were, in order of frequency, hypothyroidism, cardiovascular disease, and gestational diabetes (Table I).
Participants’ symptoms were examined at the time of referral and it was found that, in order of frequency, dry cough, myalgia and fever had the highest prevalence of the symptoms (Table II).
The results of the laboratory findings showed that the most reported disorder was related to an increase in C-reactive protein (CRP) (55 [67.90%]). Lymphopenia, elevated liver enzymes, and decreased white blood cells were seen in 15 (18.51%), 15 (18.51%), and 22 (27.61%) cases, respectively. The pulmonary findings showed that in 28 (34.56%) cases the blood oxygen saturation level was ≤ 95% and in 53 (65.43%) was > 95%. Of the 16 cases examined by lung CT scan, 13 (81.25%) had pulmonary involvement. 32 (39.50%) women received supportive oxygenation and 12 (14.8%) were referred to the intensive care unit for further services. According to our study, 2 (2.46%) cases used mechanical ventilation and no deaths were reported. The prescribed drugs were categorized into 5 groups: antivirals, antihistamines, nonsteroidal anti-inflammatory drugs, antibiotics, and corticosteroids. In total, the most commonly prescribed drugs were cefazolin, acetaminophen, betamethasone, Keltra, meropenem, interferon, and azithromycin, in order of frequency (Table III).
The perinatal findings showed that 48 out of the 81 women gave birth during the study period and the rest of the women were discharged after receiving hospital treatment or were still hospitalized at the end of the study period. Out of the 48 deliveries, 29 deliveries were performed by cesarean section and 19 deliveries by normal vaginal delivery, of which 25% were preterm deliveries. Participant management showed that in 34 cases, breastfeeding started immediately after delivery, following approved health protocols and provided training. 31 of the women were discharged from hospital without childbirth and 2 cases were discharged from hospital after spontaneous and missed abortions at wk 17 and 18. The case study showed that in 24 cases the pregnancy was terminated, of which only in 4 cases was the COVID-19 infection the main reason for termination. Other causes of termination were: fetal distress, preeclampsia, miscarriage, placental abruption, intrauterine fetal death, and fetal abnormalities (7, 5, 5, 1, 1, and 1, respectively). The demographic characteristics of the infants born from the infected mothers showed that the mean age of the infants at birth was 30.95 ± 0.96 wk with a mean neonatal weight of 2.63 ± 30.804 kg. Out of the 48 deliveries, 20 cases were boys and 28 cases were girls. A total of 33 infants were examined for infection using their amniotic fluid and cord blood. 3 cases had COVID-19 and 30 cases were healthy. The neonatal clinical findings showed that 3 neonates had intrauterine growth restriction. Evaluation of the 1st and 5th min newborn Apgar scores showed that the 1st min Apgar score in 2 infants and the 5th min Apgar score in 1 infant were < 9. In relation to arterial blood gas (ABG) pH, the pH level of 8 infants was ≤ 7.35. Finally, a total of 20 infants needed to be admitted to the neonatal intensive care unit (Table IV).
4. Discussion
In the present study, 81 pregnant women with COVID-19 were clinically evaluated from 6 centers. The aim of this study was to evaluate the clinical and prenatal findings of pregnant women with COVID-19. Regarding the clinical findings of the participants, the most common symptoms reported at the time of admission were dry cough, muscle aches, myalgia, fever, sore throat, and dyspnea. In other studies (17-19), the most common symptoms found were fever, cough, shortness of breath, fatigue, and myalgia, which is generally consistent with the results of our research. The results of our study and literature review showed that fever, cough, and myalgia are the most common symptoms of COVID-19 in pregnant women.
According to the laboratory findings, the most commonly reported disorders were increased CRP, lymphopenia, decreased white blood cells, and increased liver enzymes. In previous studies (20-23), (24)an increase in CRP was also reported, which is in line with the results of our research. One study showed that an increase in CRP was seen in 45.7% of cases (24). Also, leukopenia, lymphopenia, increased aspartate aminotransferase and increased creatine kinase were found in another study (25). It seems that the discrepancies in the laboratory findings may be due to the limited number of participants examined in some studies.
Examination of the participants pulmonary findings showed that in 28 cases, the blood oxygen saturation level was equal to or less than 95%. Of the 16 cases examined by lung CT scan, 13 cases had pulmonary involvement. Moreover, 32 cases needed supportive oxygenation, and 12 were referred to the intensive care unit for additional services. According to our study, 2 cases used mechanical ventilation, and no maternal deaths were reported. A previous meta-analysis showed that the rate of severe pneumonia in the women they examined ranged from 0-14%, and most cases required admission to the intensive care unit. In this study, invasive mechanical ventilation was needed in only a few cases. 2 cases of maternal death were reported in another Iranian study (24).
The most commonly prescribed drugs in the present study were cefazolin, non-steroidal anti-inflammatory drugs (acetaminophen), corticosteroids (betamethasone), and antivirals (Kaletra), in order of frequency. The most prescribed drugs for treating COVID-19 were ribavirin and arubidol. Ceftzol sodium and ceftriaxone were also used to prevent bacterial infections during the cesarean section for pregnant participants. Dexamethasone was used to mature the fetal lung. It should be noted that sodium heparin was used to prevent thrombosis, and diamine glycyrrhizinate was used to protect liver function (25). In the previously mentioned meta-analysis, the drugs prescribed to participants were: 70.7% antibiotics, 37.8% antiviral therapy, 17.6% corticosteroids, and 2 cases of hydroxychloroquine (24). The comparison of prescription drugs in medical centers in our study with other studies shows that most prescribed drugs were similar despite different regional treatment protocols.
In the present study, preterm labor occurred in 25% of cases. In 4 pregnancies, COVID-19 was the main reason for termination of pregnancy. In this regard, most other studies have demonstrated an increase in preterm delivery following COVID-19 (20). In other studies, preterm labor was reported in 6 out of 10 pregnancies (26), and in 6 out of 9 pregnancies (27). It seems that this increase in the number of preterm deliveries could be due to complications from COVID-19. In our study, fetal distress was the second leading cause of termination of pregnancy.
Examination of participant's management showed that in 34 cases, immediately after delivery, breastfeeding was started in accordance with approved health protocols and provided training. A review of the literature in this regard suggests 2 types of care approaches. In some studies, the mother and infant were quarantined and separated for 14 days, and breastfeeding did not occur (25). In other studies, breastfeeding was performed with strict health recommendations and supervision (28-30).
A total of 33 infants were screened for COVID-19. The examination was performed through the amniotic fluid and cord blood. 3 cases of COVID-19 and 30 healthy cases were reported. In this regard, in many other studies, vertical infection did not occur in any of the infants, and there is no evidence proving that vertical transmission can occur (25, 31). Despite the results of these studies, a meta-analysis showed that out of 163 participants, according to samples taken from amniotic fluid, placenta, and/or umbilical cord blood, 10 were positive for the SARS-CoV-2 virus, 61 newborns were positive for SARS-CoV-2, and 4 out of 92 breastmilk samples showed evidence of SARS-CoV-2. Therefore, according to the results of our study and the meta-analysis, it seems that vertical transfer is not impossible (30).
Examination of the neonatal clinical findings showed that 3 of the newborns had fetal growth restriction. Examination of the neonates’ first minute and 5th min Apgar scores showed that 2 infants had a 1st min Apgar score < 9. Also, the 5th min Apgar score in one infant was < 9. In relation to the ABG pH, in 8 infants the pH level was lower than or equal to 7.35. Finally, a total of 20 infants needed to be admitted to the neonatal intensive care unit. A similar study showed that the Apgar score of the examined newborns in the first minute was 8-9 and in the 5th min was 9-10 (27).
The most important limitation of the present study was the lack of a long follow-up period for pregnant women to evaluate the consequences of the COVID-19 virus. In this regard, the researchers suggest that future studies are conducted to investigate the long-term consequences on motherhood and infancy. Also, the present study was a case study, and testing to assess the incidence of COVID-19 in infants born in the province's hospitals was not mandatory according to national guidelines. As a result, another limitation of the study was that not all infants born to infected mothers were tested for COVID-19. It is therefore suggested that future studies examine the incidence of COVID-19 in infants according to the approved tests. Also, the relationship between infant infection and neonatal complications and consequences should be examined.
5. Conclusion
The present study’s results showed that the most common symptoms of pregnant women with COVID-19 when visiting medical centers are: dry cough, muscle aches, myalgia and fever. These symptoms are similar to those in other adults. The most common laboratory findings in the affected women were increased CRP, lymphopenia, decreased white blood cells, and increased liver enzymes. The most common medical disorders in these women were hypothyroidism, cardiovascular disease, and diabetes. 33 infants were screened for COVID-19, 3 of whom had COVID-19, which may be evidence of vertical transmission.
Acknowledgments
The authors would like to thank all the participants whose information was used for this study and all the colleagues at the health centers who helped us gather the information. The present study is the result of a research project approved in the second session of reviewing the research projects participating in the call for obtaining a COVID-19 grant from Shahid Sadoughi University of Medical Sciences, Yazd, Iran with letter number 19239 dated 25/4/2020.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Pregnancy Health
References
1. Gorbalenya AE, Baker SC, Baric R, Groot RJ, Drosten C, Gulyaeva AA, et al. Severe acute respiratory syndrome-related coronavirus: The species and its viruses-a statement of the coronavirus study group. Nat Microbiol 2020; 5: 536-544. [DOI:10.1101/2020.02.07.937862]
2. Lai Ch-Ch, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): The epidemic and the challenges. Int J Antimicrob Agents 2020; 55: 105924. [DOI:10.1016/j.ijantimicag.2020.105924] [PMID] [PMCID]
3. Jebril N. World Health Organization declared a pandemic public health menace: A systematic review of the coronavirus disease 2019 "COVID-19". Int J Psychosocial Rehabilit 2020; 24: 2784-2795. [DOI:10.2139/ssrn.3566298]
4. World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. Braz J Implant Health Sci 2020; 2: 1-3.
5. Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet 2020; 395: 760-762. [DOI:10.1016/S0140-6736(20)30365-2]
6. Nikpouraghdam M, Farahani AJ, Alishiri Gh, Heydari S, Ebrahimnia M, Samadinia H, et al. Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in Iran: A single center study. J Clin Virology 2020; 127: 104378. [DOI:10.1016/j.jcv.2020.104378] [PMID] [PMCID]
7. Abdi M. Coronavirus disease 2019 (COVID-19) outbreak in Iran: Actions and problems. In: Mody L. Infection control & hospital epidemiology. USA: Combridge University Press; 2020. [DOI:10.1017/ice.2020.86] [PMID] [PMCID]
8. Zand AD, Heir AV. Environmental impacts of new Coronavirus outbreak in Iran with an emphasis on waste management sector. J Mater Cycles Waste Manag 2020; 23: 240-247. [DOI:10.1007/s10163-020-01123-1] [PMID] [PMCID]
9. Acker K, Eagen-Torkko M, Riley LE, Saiman L. COVID-19 infection, prevention, and control considerations in the obstetric environment. Clin Obstet Gynecol 2022; 65: 134-147. [DOI:10.1097/GRF.0000000000000666] [PMID] [PMCID]
10. Lotfi M, Hamblin MR, Rezaei N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clinica Chimica Acta 2020; 508: 254-266. [DOI:10.1016/j.cca.2020.05.044] [PMID] [PMCID]
11. Chua MSQ, Lee JCS, Sulaiman S, Tan HK. From the frontlines of COVID‐19- How prepared are we as obstetricians: A commentary. BJOG 2020; 127: 786-788.
https://doi.org/10.1111/1471-0528.16254 [DOI:10.1111/1471-0528.16192]
12. Ahlers-Schmidt CR, Hervey AM, Neil T, Kuhlmann S, Kuhlmann Z. Concerns of women regarding pregnancy and childbirth during the COVID-19 pandemic. Patient Educ Couns 2020; 103: 2578-2582. [DOI:10.1016/j.pec.2020.09.031] [PMID] [PMCID]
13. Rasmussen SA, Hayes EB. Public health approach to emerging infections among pregnant women. Am J Public Health 2005; 95: 1942-1944. [DOI:10.2105/AJPH.2004.054957] [PMID] [PMCID]
14. Moore CA, Staples JE, Dobyns WB, Pessoa A, Ventura CV, Da Fonseca EB, et al. Characterizing the pattern of anomalies in congenital Zika syndrome for pediatric clinicians. JAMA Pediatr 2017; 171: 288-295. [DOI:10.1001/jamapediatrics.2016.3982] [PMID] [PMCID]
15. Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects-reviewing the evidence for causality. N Engl J Med 2016; 374: 1981-1987. [DOI:10.1056/NEJMsr1604338] [PMID]
16. Haddad LB, Jamieson DJ, Rasmussen SA. Pregnant women and the Ebola crisis. N Engl J Med 2018; 379: 2492-2493. [DOI:10.1056/NEJMp1814020] [PMID]
17. Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: A report based on 116 cases. Am J Obstet Gynecol 2020; 223: 111. [DOI:10.1016/j.ajog.2020.04.014] [PMID] [PMCID]
18. Liu W, Wang J, Li W, Zhou Z, Liu S, Rong Z. Clinical characteristics of 19 neonates born to mothers with COVID-19. Front Med 2020; 14: 193-198.
https://doi.org/10.3389/fmed.2020.00193 [DOI:10.1007/s11684-020-0772-y]
19. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020; 395: 507-513. [DOI:10.1016/S0140-6736(20)30211-7]
20. Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, et al. Maternal and neonatal outcomes of pregnant women with coronavirus disease 2019 (COVID-19) pneumonia: A case-control study. Clin Infect Dis 2020; 71: 2035-2041. [DOI:10.1093/cid/ciaa352] [PMID] [PMCID]
21. Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, Seferovic MD, Aski SK, Arian SE, et al. Maternal death due to COVID-19. Am J Obstet Gynecol 2020; 223: 109. [DOI:10.1016/j.ajog.2020.04.030] [PMID] [PMCID]
22. Liu H, Liu F, Li J, Zhang T, Wang D, Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: Focus on pregnant women and children. J Infect 2020; 80: e7-e13. [DOI:10.1016/j.jinf.2020.03.007] [PMID] [PMCID]
23. Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: A preliminary analysis. Am J Roentgenol 2020; 215: 127-132. [DOI:10.2214/AJR.20.23072] [PMID]
24. Juan J, Gil MM, Rong Z, Zhang Y, Yang H, Poon LC. Effect of coronavirus disease 2019 (COVID‐19) on maternal, perinatal and neonatal outcome: Systematic review. Ultrasound Obstet Gynecol 2020; 56: 15-27.
https://doi.org/10.1002/uog.22088 [DOI:10.1002/uog.23059] [PMID] [PMCID]
25. Chen Y, Bai J. Maternal and infant outcomes of full-term pregnancy combined with COVID-2019 in Wuhan, China: Retrospective case series. Arch Gynecol Obstet 2020; 302: 545-551. [DOI:10.1007/s00404-020-05573-8] [PMID] [PMCID]
26. Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr 2020; 9: 51-60. [DOI:10.21037/tp.2020.02.06] [PMID] [PMCID]
27. Chen H, Guo J, Wang Ch, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: A retrospective review of medical records. Lancet 2020; 395: 809-815. [DOI:10.1016/S0140-6736(20)30360-3]
28. Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Forti A, et al. Breastfeeding mothers with COVID-19 infection: A case series. Int Breastfeed J 2020; 15: 69. [DOI:10.1186/s13006-020-00314-8] [PMID] [PMCID]
29. Brown A, Shenker N. Experiences of breastfeeding during COVID‐19: Lessons for future practical and emotional support. Matern Child Nutr 2021; 17: e13088. [DOI:10.1111/mcn.13088]
30. Rodrigues C, Baía I, Domingues R, Barros H. Pregnancy and breastfeeding during COVID-19 pandemic: A systematic review of published pregnancy cases. Front Public Health 2020; 8: 558144. [DOI:10.3389/fpubh.2020.558144] [PMID] [PMCID]
31. Liu W, Wang Q, Zhang Q, Chen L, Chen J, Zhang B, et al. Coronavirus disease 2019 (COVID-19) during pregnancy: A case series. Preprints 2020: 2020020373.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |