Sun, Feb 1, 2026
[Archive]
Volume 22, Issue 1 (January 2024)
IJRM 2024, 22(1): 55-60 |
Back to browse issues page
Ethics code: IR.SSU.MEDICINE.REC.1398.303
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nafisi Moghadam R, Tamizi F, Razavi Ratki S K, Nafisi Moghadam A, Javaheri A, Namiranian N. Evaluation of diagnostic value of pelvic MRI in endometriosis in comparison with surgical findings: A cross-sectional study. IJRM 2024; 22 (1) :55-60
URL: http://ijrm.ir/article-1-2589-en.html
URL: http://ijrm.ir/article-1-2589-en.html
Reza Nafisi Moghadam1 

 , Fatemeh Tamizi1
, Fatemeh Tamizi1 

 , Seid Kazem Razavi Ratki1
, Seid Kazem Razavi Ratki1 

 , Amin Nafisi Moghadam2
, Amin Nafisi Moghadam2 

 , Atiyeh Javaheri3
, Atiyeh Javaheri3 

 , Nasim Namiranian *4
, Nasim Namiranian *4 




 , Fatemeh Tamizi1
, Fatemeh Tamizi1 

 , Seid Kazem Razavi Ratki1
, Seid Kazem Razavi Ratki1 

 , Amin Nafisi Moghadam2
, Amin Nafisi Moghadam2 

 , Atiyeh Javaheri3
, Atiyeh Javaheri3 

 , Nasim Namiranian *4
, Nasim Namiranian *4 


1- Department of Radiology, Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Faculty of Medicine, Aliebnabitaleb Azad University, Yazd, Iran.
3- Department of Obstetrics and Gynecology, Shahid Sadoughi Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Diabetes Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,namiranian.nasim@gmail.com
2- Faculty of Medicine, Aliebnabitaleb Azad University, Yazd, Iran.
3- Department of Obstetrics and Gynecology, Shahid Sadoughi Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Diabetes Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Keywords: Deep infiltrating endometriosis, Magnetic resonance imaging, Diagnosis, Laparoscopy, Sensitivity, Specificity.
Full-Text [PDF 266 kb]
(779 Downloads)
| Abstract (HTML) (1320 Views)
Full-Text: (285 Views)
1. Introduction
Endometriosis is defined as ectopic endometrial tissue including glands and stromal tissue outside the uterus (1, 2). The incidence of endometriosis varies, but the prevalence of this disease in fertile women is reported 10-15%. The most common symptoms are periodic pelvic pain and infertility (1, 3). Endometriosis is a multifocal gynecologic disorder, and may take up to 10 yr to be diagnosed. Therefore, it can have social and psychological difficulties, and it comes a lot to the health care system (4-6). There can be 3 forms of endometriosis including ovarian, peritoneal, and deep infiltrating endometriosis (DIE). DIE is one of the most important chronic pelvic pain in women and often leads to surgery. Diagnosing, staging, and treatment management is challenging. Although transvaginal ultrasonography (TVS) is considered to be the first noninvasive diagnostic method, laparoscopy is the minimally invasive method as the gold standard (7-9).
Magnetic resonance imaging (MRI) is a noninvasive and supplementary method that can detect endometrial lesions in the pelvic (7, 10). Since surgery is the best treatment for endometriosis, detection and localizing of endometriosis lesions (foci) is very important, but detecting the severity of DIE by physical examination and laparoscopy is difficult. The evaluation of DIE in occult spaces and subperitoneal areas is limited by pelvic adhesion (7, 11). MRI is an appropriate imaging modality because it provides high spatial resolution, a large field of view, and multi-planar imaging and tissue differentiation. The sensitivity and accuracy of MRI in DIE are 84% and 85%, respectively (12). However, there are some limitations in the detection of endometriosis. For instance, the diagnosis of intestinal DIE is difficult due to motion artifacts or retroflection uterus making the detection of endometriosis in uterosacral ligaments difficult.
Also, recto vaginal septal lesions are mostly seen as nodules or infiltrative masses that are mainly composed of fibrotic tissues with a few hemorrhagic foci, so they are demonstrated hypo signals in T1 and T2 weighted images in MRI. Therefore, normal fibrotic tissue in the rectovaginal septal may lead to a false positive predictive value (PPV) (13). According to the evidence, the diagnostic accuracy of MRI in pelvic endometriosis is significant, though its accuracy is variable in different parts of the pelvic (14). MRI is a valuable method for detecting endometriosis with or without TVS (15). It is important that despite all the benefits of MRI, TVS is the first choice in diagnostic methods. Although in the detection of small focus (< 1/5 cm) in the uterosacral ligament and bladder, TVS is found to be more effective than MRI, and its accuracy for deep pelvic and superficial peritoneal lesions is not clear (12, 16).
This study aims to compare the accuracy of MRI with laparoscopic findings in deep pelvic endometriosis at Shahid Sadoughi hospital, Yazd, Iran.
2. Materials and Methods
This diagnostic cross-sectional study was conducted on 40 women suspicious of DIE who referred to the gynecology clinic of Shahid Sadoughi hospital, Yazd, Iran from November 2020-2021.
The inclusion criteria were ≥ 20 yr women suspicious of endometriosis who did not have contraindications for MRI. Those who visited the gynecologic clinic and were diagnosed with DIE endometriosis after checking their history, physical examination, and vaginal ultrasonography by a gynecologist were referred to the imaging center for MRI. The women were selected based on endometriosis criteria (17) that included infertility history, endometriosis surgery, dysmenorrhea, deep dyspareunia, periodic painful deification, dysuria, and asthenia or were defective with lesions in the posterior vaginal fornix, vaginal infiltration or nodules, lesion in the pouch of Douglas in vaginal and rectal examination (18). Excluding criteria included a cochlear implant, pacemaker, and claustrophobia.
All women underwent diagnosis MRI before performing the laparoscopy. Images in this study were acquired on a 1.5-T imager (Avanto; Siemens, Erlangen, Germany). Our standard imaging protocol is detailed and includes an axial dark fluid inversion-recovery T1-weighted sequence; axial and sagittal fat-suppressed fast spin-echo T1-weighted sequences; and axial, oblique coronal, and sagittal T2-weighted sequences.
In this study, contrast media was not used because there is no difference between inflammatory lesions and endometriosis foci in post-contrast images. 2 radiologists interpreted these images. They were experienced separately and the findings were rewarded. In addition, women were examined by laparoscopic surgery by a gynecologist who was blind to the results of MRI.
Pathological findings and MRI images were collected in a data sheet designed by the researchers and compared.
2.1. Sample size
The sample size of 40 women was determined according to Thomeer and colleagues study and interval coefficient of 95% (16). The α was 0.05 and the β was 20%. Also 15% attrition rate was considered.
2.2. Ethical considerations
The proposal was confirmed by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.MEDICINE.REC.1398.303). The researchers respected the Helsinki Declaration all along the process. Written consent form were obtained from all participants, and they were assumed that their data would be considered confidential and would only be used for research proposes. It was also guaranteed that this research would have no effect on their treatment process and would not cost any expenses.
2.3. Statistical analysis
Data were analyzed using SPSS (Statistical Package for the Social Sciences, version 22.0, SPSS Inc., Chicago, Illinois, USA) to calculate the mean value standard deviation and relative frequency. The sensitivity and specificity of laparoscopic and MRI findings were calculated.
3. Results
This study involved 40 women suspected of having DIE (aged 20-67 yr, with a mean age of 37.75 ± 8.34 yr). Among the participants, 16 (40%) had a history of infertility, 9 (22.5%) had undergone endometriosis surgery, 18 (45%) reported dyspareunia, 31 (77.5%) reported dysmenorrhea, and 2 (5%) reported dysuria (each woman had one or more of these signs and symptoms).
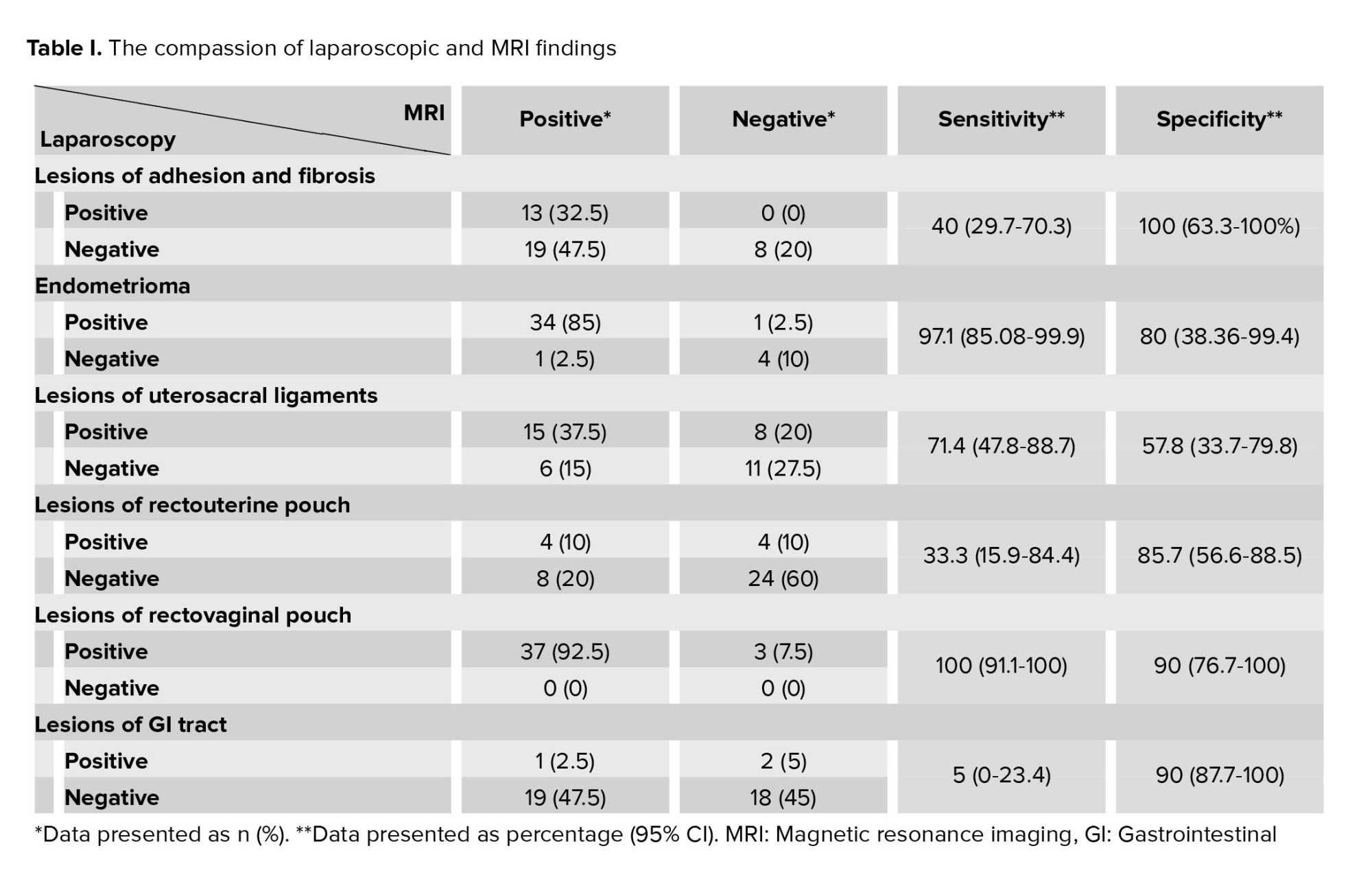
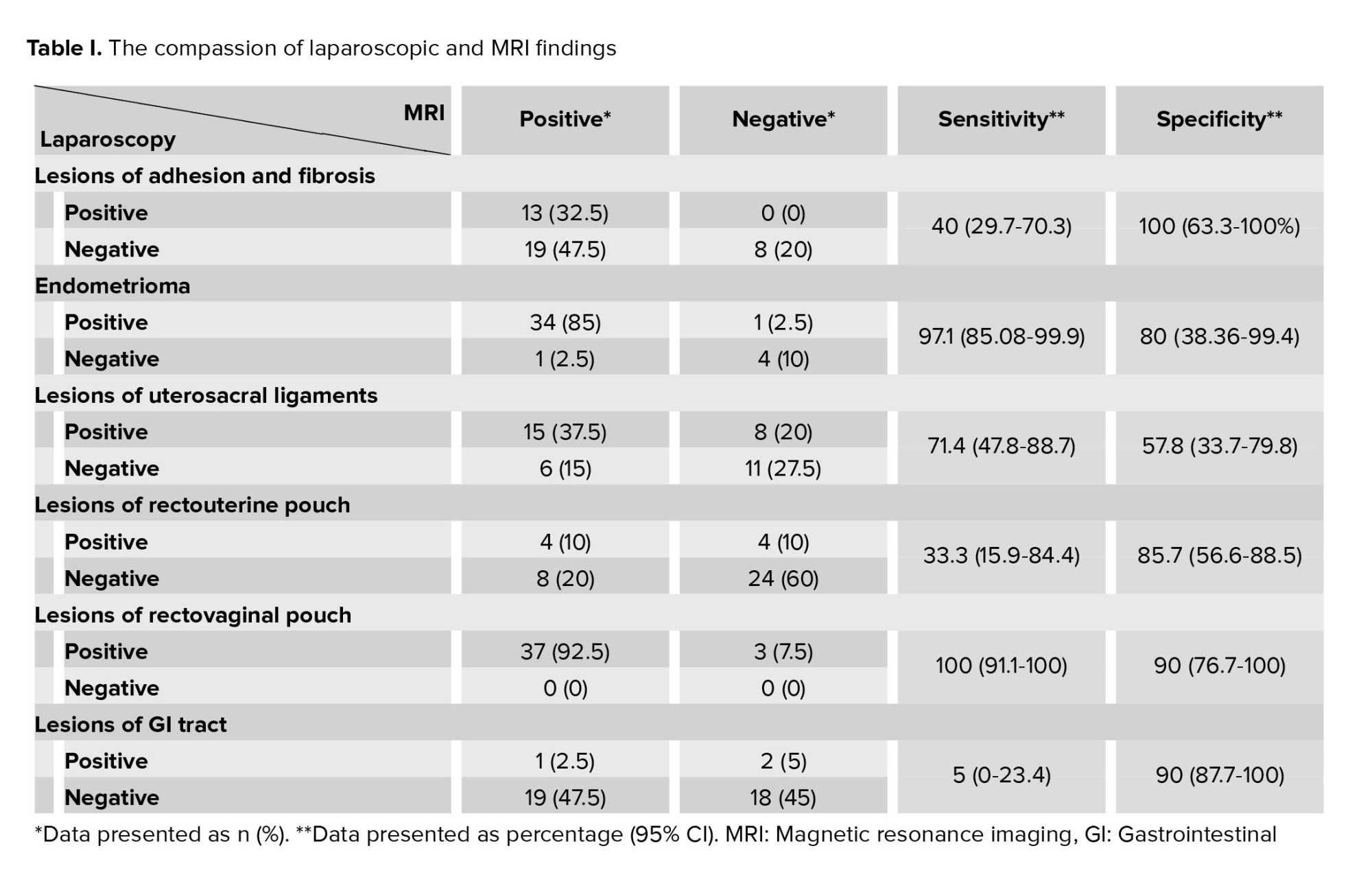
Laparoscopy and MRI findings regarding adhesions and fibrosis, endometrioma, uterosacral ligaments, rectouterine pouch, rectovaginal pouch, and GI tract lesions were compared (Table I). The sensitivity and specificity (95% CI), PPV, and negative predictive value (NPV) were also reported.
According to laparoscopy as a gold standard method in endometriosis detection, the sensitivity and specificity of MRI in endometriosis disease were 94.8% (9.1-99.8%) and 20% (11-67%), respectively. PPV and NPV of MRI were 90.2% and 33.3%, respectively.
4. Discussion
In this study, 40 women suspected of endometriosis were investigated by MRI and laparoscopy. Generally, pelvic MRI in endometriosis was efficient with a sensitivity of 94.8%. However, the specificity of findings is about 20%. The sensitivity and specificity of endometriosis are different depending on the anatomic location and size of the lesions. The difference in MRI accuracy in various anatomic locations is also reported earlier expected that the detection of deep pelvic endometriosis and adhesion bands would be more accurate by laparoscopy compared to MRI (14). The detection of endometrioma is highly accurate by MRI and laparoscopy because the appearance of these lesions is large and cystic. Our study showed the detection of uterosacral ligament lesions. MRI can detect utero sacral ligament lesions as efficiently as laparoscopy, but it is not efficient enough in the detection of the GI tract.
In general, PPV is 90.2% and NPV is 33.3% for all detected lesions by MRI. In a study out of 363 cases suspicious of endometriosis, 89 patients were operated, and 79 of them were investigated on the history, physical examination, ultrasonography, and MRI. Their study showed that if MRI is added to other methods for diagnosing endometriosis, sensitivity will decrease from 93.7-85.9, and specificity will increase from 55.6-62.5. Thus, the authors concluded that MRI does not significantly help diagnose endometriosis (19).
In our study, MRI was an efficient method in detection of endometrioma while it was less efficient in the detection of deep endometriosis, they have used MRI in endometriosis depending on the kind of lesions. Our findings demonstrate that the PPV and sensitivity of MRI in detecting the most of lesions are acceptable, but the specificity and NPV of these lesions are low. So, in cases suspicious of endometriosis, MRI can be recommended as a non-interventional method for diagnosis. If lesions are detected by MRI, laparoscopic surgery is indicated. MRI helps reduce unnecessary surgery to some extent which decreases medical costs for patients.
In another study, 74 women suspected to have DIE were examined by ultrasonography, urethrography, barium enema, and MRI to evaluate pelvic lesions. The image findings were compared with laparoscopic findings as the gold standard method (20). It increased the diagnostic value percentage from 2.7-6.8 using MRI which is compatible with our study. In similar study, 42 women were diagnosed with endometriosis by pathologic samples of which 28 cases were detected with MRI. MRI was suggested for 5 suspicious endometriosis and 9 cases were reported normal. As a result, the sensitivity of MRI was 69% and the specificity was 75% (21). This difference can be related to the experience of the radiologist. It was shown that the experience of the radiologist and their relationship with the gynecologist is of great importance in the diagnosis of endometriosis (22). In our study, the radiologist was experienced enough to report pelvic MRI.
In another study 74 patients were examined and 10 of them were operated. In MRI, lesions were detected in 52% of patients in T1w MRI and were increased to 81% in SW images in MRI. In their study, increased accuracy of susceptibility weighted imaging (SWI) especially, in rectovaginal and uterosacral ligaments was approved. So SWI was suggested as a complementary sequence in MRI (23). As a result, SWI can be added to conventional sequences (T1w and T2w) to improve the diagnosis.
5. Conclusion
Non-interventional diagnosis of endometriosis is a big challenge for gynecologists and radiologists. MRI can be used as an efficient method for the detection of endometrial lesions and can decrease laparoscopic surgery. It is recommended that similar feature studies are conducted on larger samples and the use of SWI sequences in MRI imaging.
Data availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author contributions
RNM, FT and AJ designed the study and conducted the research. NN, SKRR and FT monitored, evaluated, and analyzed the result of the study. ANM drafted the manuscript. RNM, FT, SKRR, ANM, AJ, NN reviewed the article. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
This study was supported by Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Endometriosis is defined as ectopic endometrial tissue including glands and stromal tissue outside the uterus (1, 2). The incidence of endometriosis varies, but the prevalence of this disease in fertile women is reported 10-15%. The most common symptoms are periodic pelvic pain and infertility (1, 3). Endometriosis is a multifocal gynecologic disorder, and may take up to 10 yr to be diagnosed. Therefore, it can have social and psychological difficulties, and it comes a lot to the health care system (4-6). There can be 3 forms of endometriosis including ovarian, peritoneal, and deep infiltrating endometriosis (DIE). DIE is one of the most important chronic pelvic pain in women and often leads to surgery. Diagnosing, staging, and treatment management is challenging. Although transvaginal ultrasonography (TVS) is considered to be the first noninvasive diagnostic method, laparoscopy is the minimally invasive method as the gold standard (7-9).
Magnetic resonance imaging (MRI) is a noninvasive and supplementary method that can detect endometrial lesions in the pelvic (7, 10). Since surgery is the best treatment for endometriosis, detection and localizing of endometriosis lesions (foci) is very important, but detecting the severity of DIE by physical examination and laparoscopy is difficult. The evaluation of DIE in occult spaces and subperitoneal areas is limited by pelvic adhesion (7, 11). MRI is an appropriate imaging modality because it provides high spatial resolution, a large field of view, and multi-planar imaging and tissue differentiation. The sensitivity and accuracy of MRI in DIE are 84% and 85%, respectively (12). However, there are some limitations in the detection of endometriosis. For instance, the diagnosis of intestinal DIE is difficult due to motion artifacts or retroflection uterus making the detection of endometriosis in uterosacral ligaments difficult.
Also, recto vaginal septal lesions are mostly seen as nodules or infiltrative masses that are mainly composed of fibrotic tissues with a few hemorrhagic foci, so they are demonstrated hypo signals in T1 and T2 weighted images in MRI. Therefore, normal fibrotic tissue in the rectovaginal septal may lead to a false positive predictive value (PPV) (13). According to the evidence, the diagnostic accuracy of MRI in pelvic endometriosis is significant, though its accuracy is variable in different parts of the pelvic (14). MRI is a valuable method for detecting endometriosis with or without TVS (15). It is important that despite all the benefits of MRI, TVS is the first choice in diagnostic methods. Although in the detection of small focus (< 1/5 cm) in the uterosacral ligament and bladder, TVS is found to be more effective than MRI, and its accuracy for deep pelvic and superficial peritoneal lesions is not clear (12, 16).
This study aims to compare the accuracy of MRI with laparoscopic findings in deep pelvic endometriosis at Shahid Sadoughi hospital, Yazd, Iran.
2. Materials and Methods
This diagnostic cross-sectional study was conducted on 40 women suspicious of DIE who referred to the gynecology clinic of Shahid Sadoughi hospital, Yazd, Iran from November 2020-2021.
The inclusion criteria were ≥ 20 yr women suspicious of endometriosis who did not have contraindications for MRI. Those who visited the gynecologic clinic and were diagnosed with DIE endometriosis after checking their history, physical examination, and vaginal ultrasonography by a gynecologist were referred to the imaging center for MRI. The women were selected based on endometriosis criteria (17) that included infertility history, endometriosis surgery, dysmenorrhea, deep dyspareunia, periodic painful deification, dysuria, and asthenia or were defective with lesions in the posterior vaginal fornix, vaginal infiltration or nodules, lesion in the pouch of Douglas in vaginal and rectal examination (18). Excluding criteria included a cochlear implant, pacemaker, and claustrophobia.
All women underwent diagnosis MRI before performing the laparoscopy. Images in this study were acquired on a 1.5-T imager (Avanto; Siemens, Erlangen, Germany). Our standard imaging protocol is detailed and includes an axial dark fluid inversion-recovery T1-weighted sequence; axial and sagittal fat-suppressed fast spin-echo T1-weighted sequences; and axial, oblique coronal, and sagittal T2-weighted sequences.
In this study, contrast media was not used because there is no difference between inflammatory lesions and endometriosis foci in post-contrast images. 2 radiologists interpreted these images. They were experienced separately and the findings were rewarded. In addition, women were examined by laparoscopic surgery by a gynecologist who was blind to the results of MRI.
Pathological findings and MRI images were collected in a data sheet designed by the researchers and compared.
2.1. Sample size
The sample size of 40 women was determined according to Thomeer and colleagues study and interval coefficient of 95% (16). The α was 0.05 and the β was 20%. Also 15% attrition rate was considered.
2.2. Ethical considerations
The proposal was confirmed by the Ethics Committee of Shahid Sadoughi University of Medical Sciences, Yazd, Iran (Code: IR.SSU.MEDICINE.REC.1398.303). The researchers respected the Helsinki Declaration all along the process. Written consent form were obtained from all participants, and they were assumed that their data would be considered confidential and would only be used for research proposes. It was also guaranteed that this research would have no effect on their treatment process and would not cost any expenses.
2.3. Statistical analysis
Data were analyzed using SPSS (Statistical Package for the Social Sciences, version 22.0, SPSS Inc., Chicago, Illinois, USA) to calculate the mean value standard deviation and relative frequency. The sensitivity and specificity of laparoscopic and MRI findings were calculated.
3. Results
This study involved 40 women suspected of having DIE (aged 20-67 yr, with a mean age of 37.75 ± 8.34 yr). Among the participants, 16 (40%) had a history of infertility, 9 (22.5%) had undergone endometriosis surgery, 18 (45%) reported dyspareunia, 31 (77.5%) reported dysmenorrhea, and 2 (5%) reported dysuria (each woman had one or more of these signs and symptoms).
Laparoscopy and MRI findings regarding adhesions and fibrosis, endometrioma, uterosacral ligaments, rectouterine pouch, rectovaginal pouch, and GI tract lesions were compared (Table I). The sensitivity and specificity (95% CI), PPV, and negative predictive value (NPV) were also reported.
According to laparoscopy as a gold standard method in endometriosis detection, the sensitivity and specificity of MRI in endometriosis disease were 94.8% (9.1-99.8%) and 20% (11-67%), respectively. PPV and NPV of MRI were 90.2% and 33.3%, respectively.
4. Discussion
In this study, 40 women suspected of endometriosis were investigated by MRI and laparoscopy. Generally, pelvic MRI in endometriosis was efficient with a sensitivity of 94.8%. However, the specificity of findings is about 20%. The sensitivity and specificity of endometriosis are different depending on the anatomic location and size of the lesions. The difference in MRI accuracy in various anatomic locations is also reported earlier expected that the detection of deep pelvic endometriosis and adhesion bands would be more accurate by laparoscopy compared to MRI (14). The detection of endometrioma is highly accurate by MRI and laparoscopy because the appearance of these lesions is large and cystic. Our study showed the detection of uterosacral ligament lesions. MRI can detect utero sacral ligament lesions as efficiently as laparoscopy, but it is not efficient enough in the detection of the GI tract.
In general, PPV is 90.2% and NPV is 33.3% for all detected lesions by MRI. In a study out of 363 cases suspicious of endometriosis, 89 patients were operated, and 79 of them were investigated on the history, physical examination, ultrasonography, and MRI. Their study showed that if MRI is added to other methods for diagnosing endometriosis, sensitivity will decrease from 93.7-85.9, and specificity will increase from 55.6-62.5. Thus, the authors concluded that MRI does not significantly help diagnose endometriosis (19).
In our study, MRI was an efficient method in detection of endometrioma while it was less efficient in the detection of deep endometriosis, they have used MRI in endometriosis depending on the kind of lesions. Our findings demonstrate that the PPV and sensitivity of MRI in detecting the most of lesions are acceptable, but the specificity and NPV of these lesions are low. So, in cases suspicious of endometriosis, MRI can be recommended as a non-interventional method for diagnosis. If lesions are detected by MRI, laparoscopic surgery is indicated. MRI helps reduce unnecessary surgery to some extent which decreases medical costs for patients.
In another study, 74 women suspected to have DIE were examined by ultrasonography, urethrography, barium enema, and MRI to evaluate pelvic lesions. The image findings were compared with laparoscopic findings as the gold standard method (20). It increased the diagnostic value percentage from 2.7-6.8 using MRI which is compatible with our study. In similar study, 42 women were diagnosed with endometriosis by pathologic samples of which 28 cases were detected with MRI. MRI was suggested for 5 suspicious endometriosis and 9 cases were reported normal. As a result, the sensitivity of MRI was 69% and the specificity was 75% (21). This difference can be related to the experience of the radiologist. It was shown that the experience of the radiologist and their relationship with the gynecologist is of great importance in the diagnosis of endometriosis (22). In our study, the radiologist was experienced enough to report pelvic MRI.
In another study 74 patients were examined and 10 of them were operated. In MRI, lesions were detected in 52% of patients in T1w MRI and were increased to 81% in SW images in MRI. In their study, increased accuracy of susceptibility weighted imaging (SWI) especially, in rectovaginal and uterosacral ligaments was approved. So SWI was suggested as a complementary sequence in MRI (23). As a result, SWI can be added to conventional sequences (T1w and T2w) to improve the diagnosis.
5. Conclusion
Non-interventional diagnosis of endometriosis is a big challenge for gynecologists and radiologists. MRI can be used as an efficient method for the detection of endometrial lesions and can decrease laparoscopic surgery. It is recommended that similar feature studies are conducted on larger samples and the use of SWI sequences in MRI imaging.
Data availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author contributions
RNM, FT and AJ designed the study and conducted the research. NN, SKRR and FT monitored, evaluated, and analyzed the result of the study. ANM drafted the manuscript. RNM, FT, SKRR, ANM, AJ, NN reviewed the article. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
This study was supported by Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
Type of Study: Original Article |
Subject:
Fertility & Infertility
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |