Thu, Jan 29, 2026
[Archive]
Volume 23, Issue 7 (July 2025)
IJRM 2025, 23(7): 569-576 |
Back to browse issues page
Ethics code: IR.TUMS.IKHC.REC.1401.100
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Dashtkoohi M, Ghaemi M, Rahimi S, Eshraqi N, Haddadi M, Sedighi E, et al . Association of normal-range fetal heart rate variations during labor with umbilical cord arterial blood gas parameters and neonatal outcomes: A cross-sectional study. IJRM 2025; 23 (7) :569-576
URL: http://ijrm.ir/article-1-3345-en.html
URL: http://ijrm.ir/article-1-3345-en.html
Mohadese Dashtkoohi1 

 , Marjan Ghaemi1
, Marjan Ghaemi1 

 , Shima Rahimi2
, Shima Rahimi2 

 , Nasim Eshraqi1
, Nasim Eshraqi1 

 , Mohammad Haddadi1
, Mohammad Haddadi1 

 , Elham Sedighi1
, Elham Sedighi1 

 , Sedigheh Hantoushzadeh1
, Sedigheh Hantoushzadeh1 

 , Fatemeh Golshahi *3
, Fatemeh Golshahi *3 




 , Marjan Ghaemi1
, Marjan Ghaemi1 

 , Shima Rahimi2
, Shima Rahimi2 

 , Nasim Eshraqi1
, Nasim Eshraqi1 

 , Mohammad Haddadi1
, Mohammad Haddadi1 

 , Elham Sedighi1
, Elham Sedighi1 

 , Sedigheh Hantoushzadeh1
, Sedigheh Hantoushzadeh1 

 , Fatemeh Golshahi *3
, Fatemeh Golshahi *3 


1- Vali-E-Asr Reproductive Health Research Center, Family Health Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Obstetrics and Gynecology, School of Medicine, Yas Complex Hospital, Tehran University of Medical Sciences, Tehran, Iran.
3- Maternal, Fetal, and Neonatal Research Center, Yas Complex Hospital, Tehran University of Medical Sciences, Tehran, Iran. ,golshahi@sina.tums.ac.ir
2- Department of Obstetrics and Gynecology, School of Medicine, Yas Complex Hospital, Tehran University of Medical Sciences, Tehran, Iran.
3- Maternal, Fetal, and Neonatal Research Center, Yas Complex Hospital, Tehran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 389 kb]
(395 Downloads)
| Abstract (HTML) (481 Views)
Full-Text: (82 Views)
1. Introduction
Fetal heart rate (FHR) monitoring is a widely used technique for evaluating fetal well-being during labor due to its non-invasive nature, cost-effectiveness, and ease of implementation. The assessment of fetal health during labor aims to prevent fetal mortality, neurological complications, and unnecessary interventions during labor (1, 2). While normal results of fetal monitoring suggest that the fetus is receiving sufficient oxygen, cardiotocography, also known as a non-stress test (NST) has been found to have low sensitivity during labor and is associated with a high rate of false positives, leading to an increased number of cesarean deliveries due to suspected fetal distress (3).
To accurately identify intrauterine fetal hypoxia, the analysis of fetal scalp blood pH during childbirth has been considered a reliable method. However, this approach has its limitations, including complexity, high cost, and the requirement of a relatively large amount of blood (30-50 ml). Additionally, there is a failure rate of 11-20% in obtaining a suitable sample for pH analysis (4, 5). Metabolic acidosis is associated with both short- and long-term neurological morbidity in neonates (6). The threshold for defining acidosis in neonates varies, with mild acidosis typically characterized by an umbilical cord arterial blood pH < 7.2. It has been observed that lower neonatal pH levels are correlated with adverse neonatal outcomes, even in cases where the Apgar score at 5 min is within the normal range (7).
Timely diagnosis of fetal hypoxia or acidosis is crucial to minimize the risk of adverse neonatal outcomes, such as cerebral palsy. Hypoxia during childbirth can lead to changes in the fetal central nervous system, which directly affects fetal cardiac electrical activity and can potentially result in cerebral palsy (8).
Therefore, this study aimed to explore the relationship between changes in FHR patterns within the normal range during labor, umbilical cord arterial blood gas (ABG) analysis, and neonatal outcomes.
2. Materials and Methods
2.1. Study design and eligibility criteria
This cross-sectional study evaluated data from the medical records of all mothers and their neonates delivered at Yas hospital, Tehran, Iran, between August and December 2022. Maternal data included age, gravidity, parity, gestational age, history of medical conditions, prior surgeries, and delivery mode. Neonatal data comprised birth weight, sex, Apgar scores at 1 and 5 min, ABG parameters (pH, base excess, PCO₂, PO₂), and neonatal intensive care unit admission status.
The inclusion criteria were mothers older than 18 yr, with singleton pregnancies, gestational age of ≥ 37 wk (calculated based on crown-rump length measured in the first trimester), and candidates for natural vaginal delivery.
Exclusion criteria included cases of fetal growth restriction (estimated fetal weight < 10%), congenital abnormalities, hypoxic-ischemic encephalopathy, and seizures. These criteria were applied to ensure that the study population was representative of healthy term pregnancies and to minimize confounding factors that could influence the relationship between beat-to-beat variability and neonatal outcomes.
2.2. FHR monitoring
FHR monitoring was conducted for all participants. Recordings were taken twice: upon admission and 30 min before delivery, each session lasting at least 20 min. The Edan Express F9 fetal and maternal monitor (Edan Instruments Inc., China) was used for FHR recordings. Recorded data included baseline FHR, beat-to-beat variability, and their respective characteristics.
2.3. Umbilical cord ABG analysis
ABG samples were routinely obtained immediately after delivery. All participants were in the active phase of labor. Cesarean sections were performed only for those experiencing fetal distress, arrest of the active phase, or meconium-stained amniotic fluid. Within the 1st hr after birth, 1 ml of heparinized arterial blood was collected from all neonates, placed on ice, and sent to the hospital laboratory for acid-base analysis. This was done by clamping and cutting a 10-20 cm segment of the umbilical cord and collecting ABG samples from the umbilical cord artery. Neonates were divided into 2 groups based on ABG pH: those with acidosis (pH < 7.2) and those without acidosis (pH ≥ 7.2).
2.4. Sample size
The sample size for this cross-sectional study was determined using a priori power analysis for multiple linear regression with 4 predictors, based on the primary objective of evaluating the association between FHR variability and umbilical cord ABG parameters. Assuming a medium effect size (f² = 0.15) as per Cohen's (1988) guidelines, an alpha level of 0.05, and a desired statistical power of 0.80, the minimum required sample size was calculated to be 140 participants. This calculation was performed using an online sample size calculator (Soper, 2025, available at: https://www.danielsoper.com/statcalc/calculator.aspx?id = 1).
Due to practical constraints, including time limitations and availability of eligible participants, a total of 120 participants were included in the study. While this number is slightly below the calculated minimum, it was considered adequate for the exploratory nature of this cross-sectional study, providing sufficient statistical power for preliminary analyses and laying a foundation for future research with larger sample sizes.
2.5. Ethical Considerations
The study was approved by the Research Ethics Committee of Imam Khomeini hospital Complex, Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.IKHC.REC.1401.100). Written informed consent was obtained from each participant.
2.6. Statistical Analysis
Statistical analysis was conducted using SPSS software (version 24.0, SPSS Inc., Chicago, Illinois, USA). Descriptive statistics, such as mean and standard deviation, were used for quantitative variables, while frequencies and percentages were used for qualitative variables. The Chi-square test or Fisher's exact test was employed to compare qualitative variables. Independent t test were used to compare means between 2 groups for normally distributed quantitative variables, while the Mann-Whitney test was used for non-normal data. Multiple regression analysis was utilized to examine the correlation between umbilical cord pH, base excess, and Apgar score at 1 min with associated factors and FHR monitoring parameters. The significance level for all statistical analyses was set at 0.05.
3. Results
Initially, 133 pregnant women met the inclusion criteria; however, 13 were excluded due to fetal growth restriction (estimated fetal weight < 10%), congenital abnormalities, hypoxic-ischemic encephalopathy, and seizures. Therefore, the final evaluation was carried out on 120 neonates.
The mean gestational age at delivery was 270.3 ± 7.7 days. The neonates were divided into 2 groups based on the pH value of cord blood. Among them, 17 neonates (14.2%) had a pH value of < 7.2, indicating neonatal acidosis, while the remaining 103 neonates (85.8%) did not have acidosis (pH ≥ 7.2).
All women in the study had entered the active phase of labor. Among them, 9 (7.5%) underwent caesarean section due to fetal distress, 22 (18.3%) due to arrest of the active phase of labor, and 8 (6.7%) due to meconium-stained amniotic fluid.
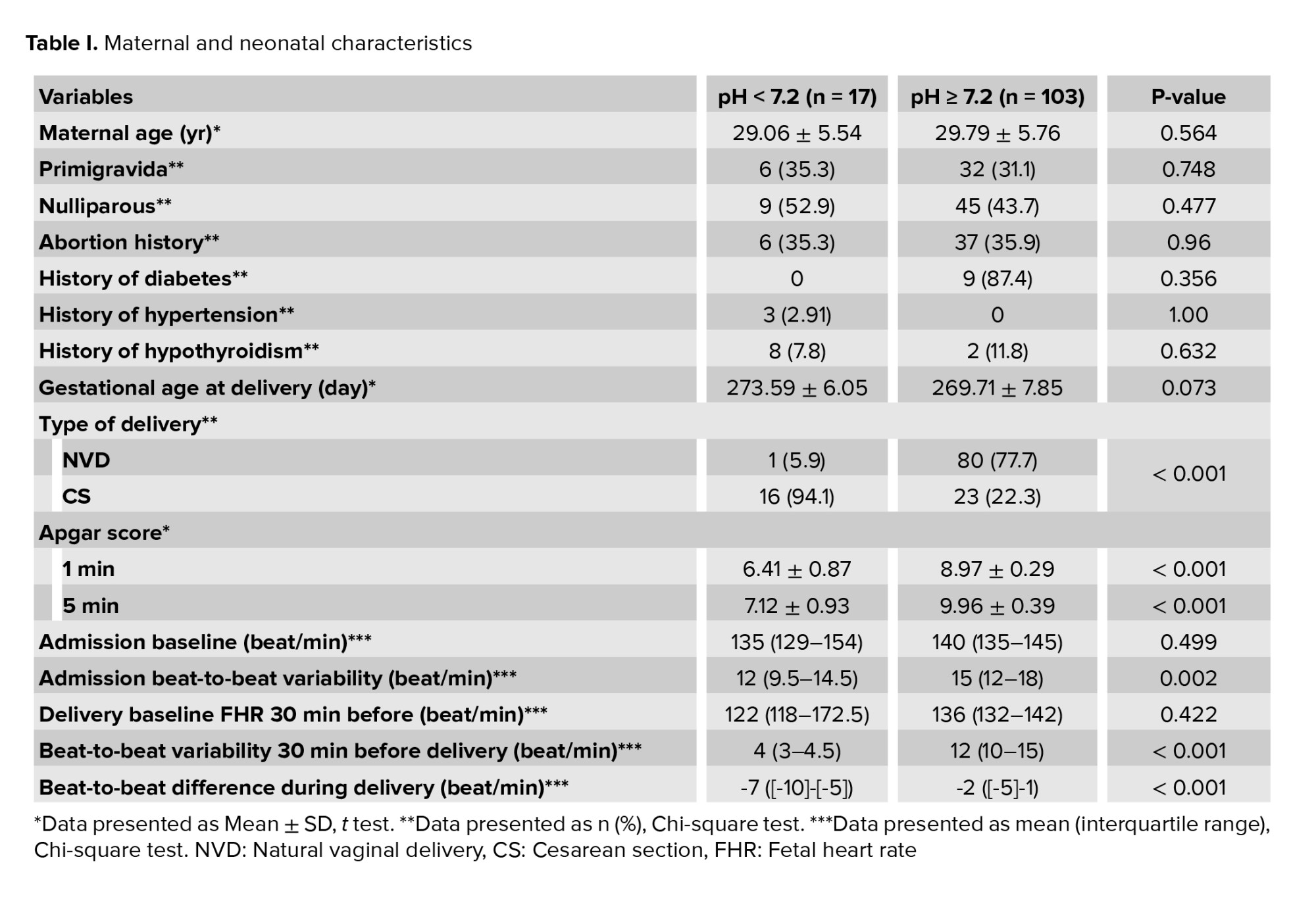
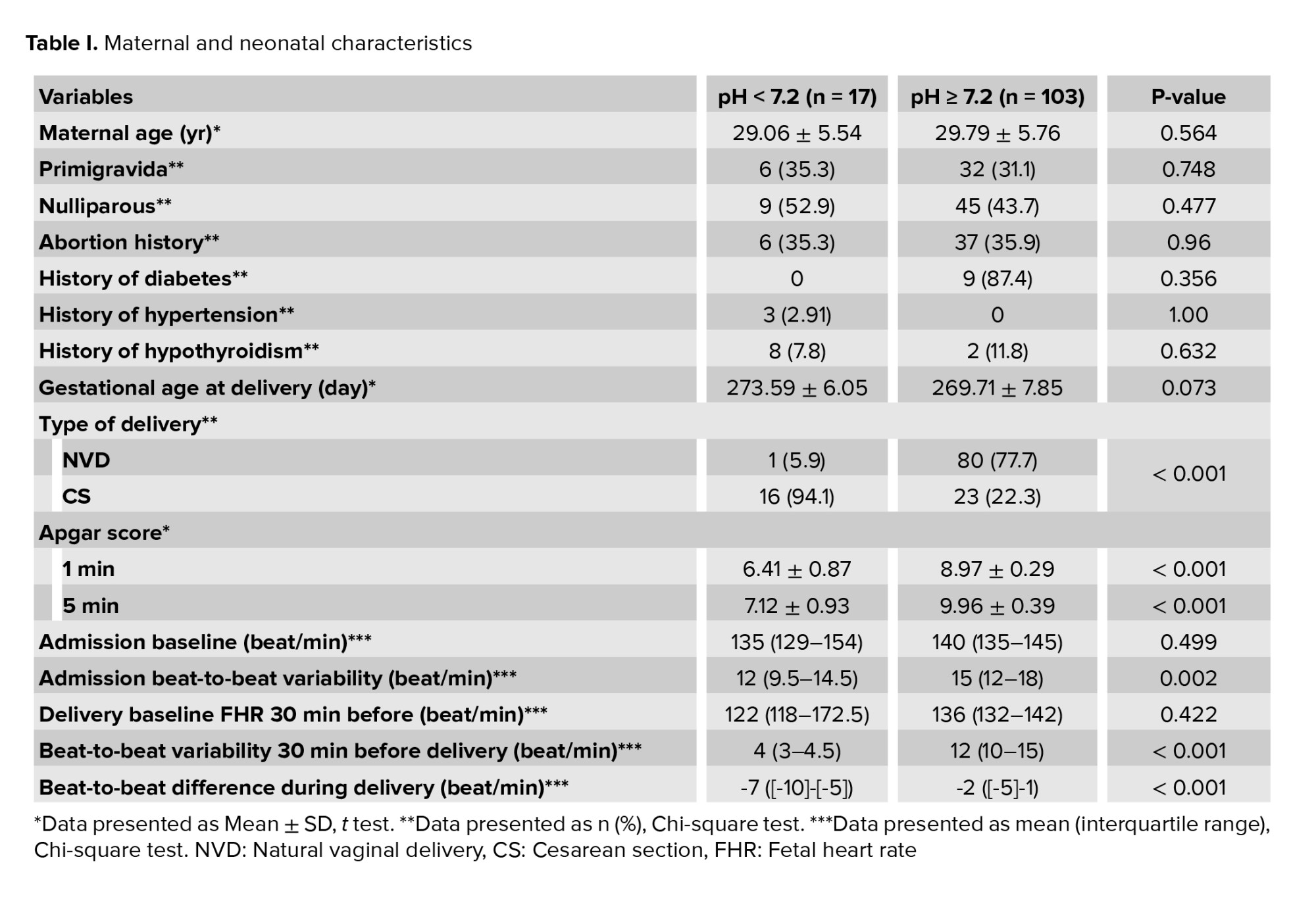
Table I presents the characteristics and outcomes of maternal and neonatal factors. No significant differences were observed between the groups in terms of maternal age, primigravida pregnancy, nullipara pregnancy, abortion history, past medical history (diabetes, hypertension, and hypothyroidism), and gestational age at delivery. However, the rate of cesarean section was significantly higher in neonates with a cord blood pH < 7.2 compared to neonates without acidosis (p < 0.001). Furthermore, both the Apgar score at 1 min and the Apgar score at 5 min were significantly higher in neonates with umbilical cord pH ≥ 7.2 compared to those with lower pH values (p < 0.001).
The study found that no significant differences were observed in the median baseline FHR between the groups during admission and 30 min before delivery FHR monitoring. Furthermore, it was observed that the beat-to-beat variability during admission and 30 min before delivery FHR monitoring were significantly lower in neonates with acidosis compared to normal neonates, with p = 0.002 and < 0.001, respectively. Moreover, the beat-to-beat variability decreased during labor, and the extent of reduction was also found to be significantly different (p < 0.001).
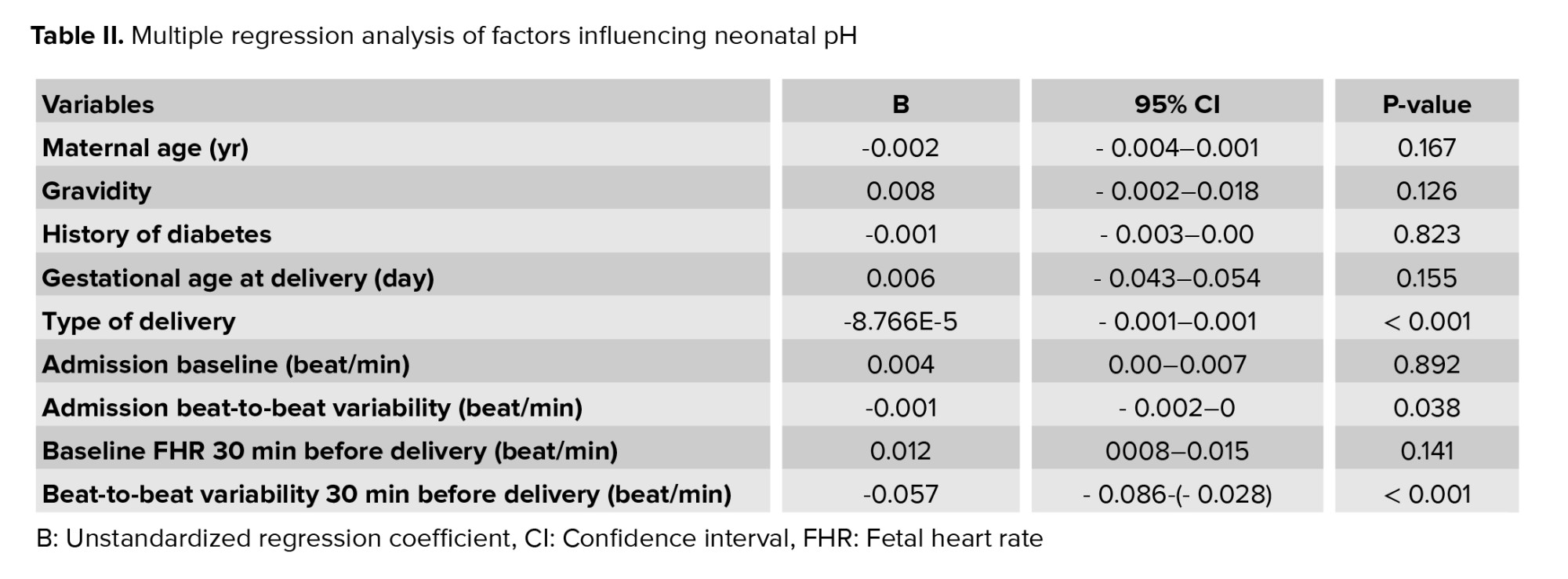
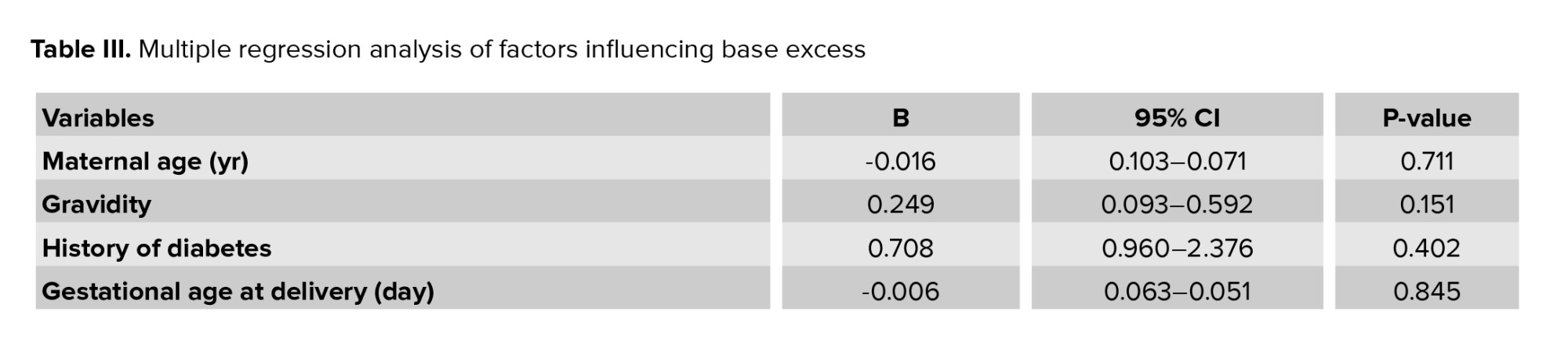
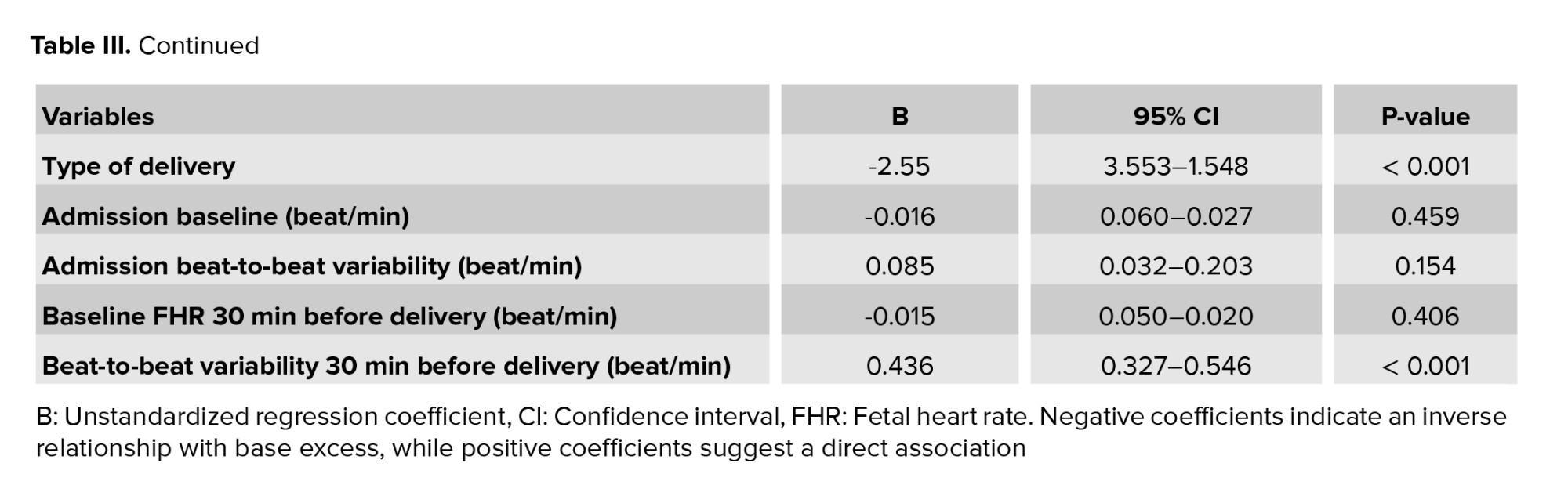
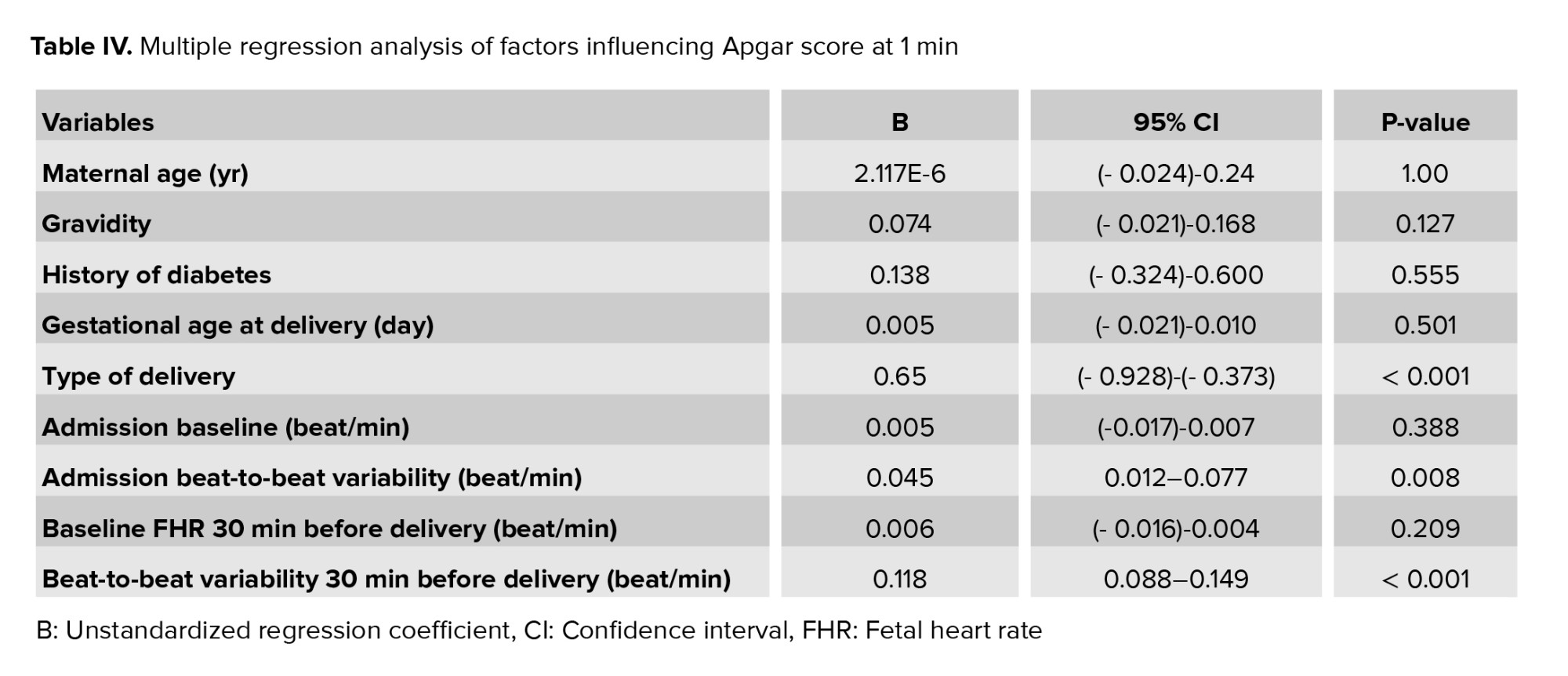
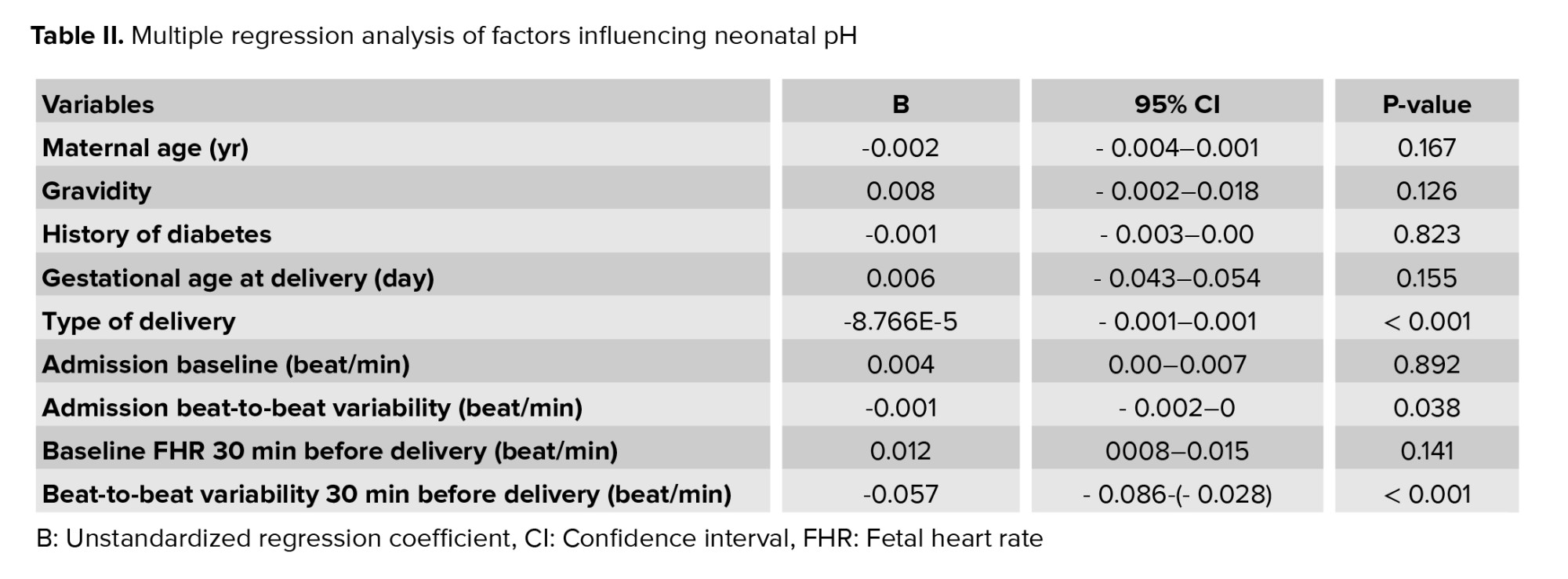
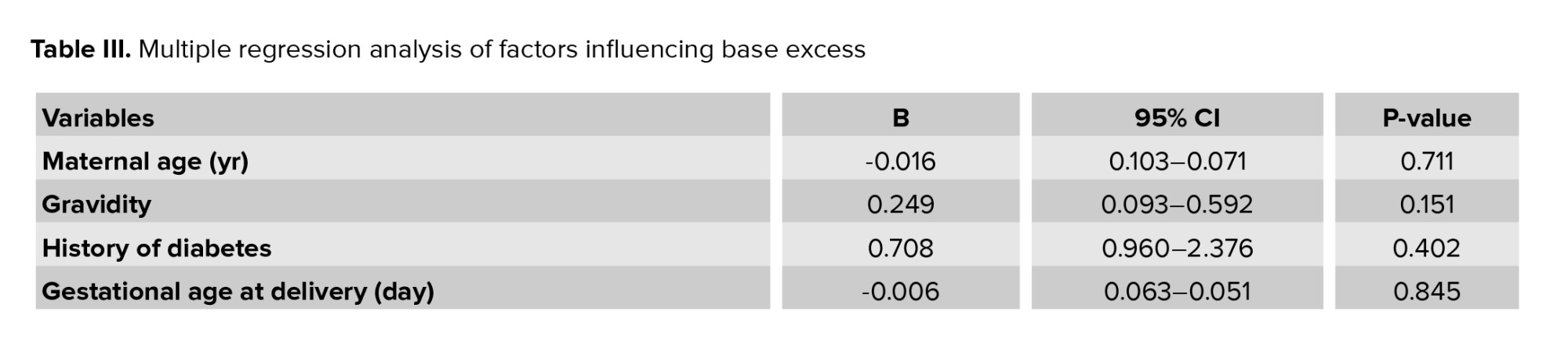
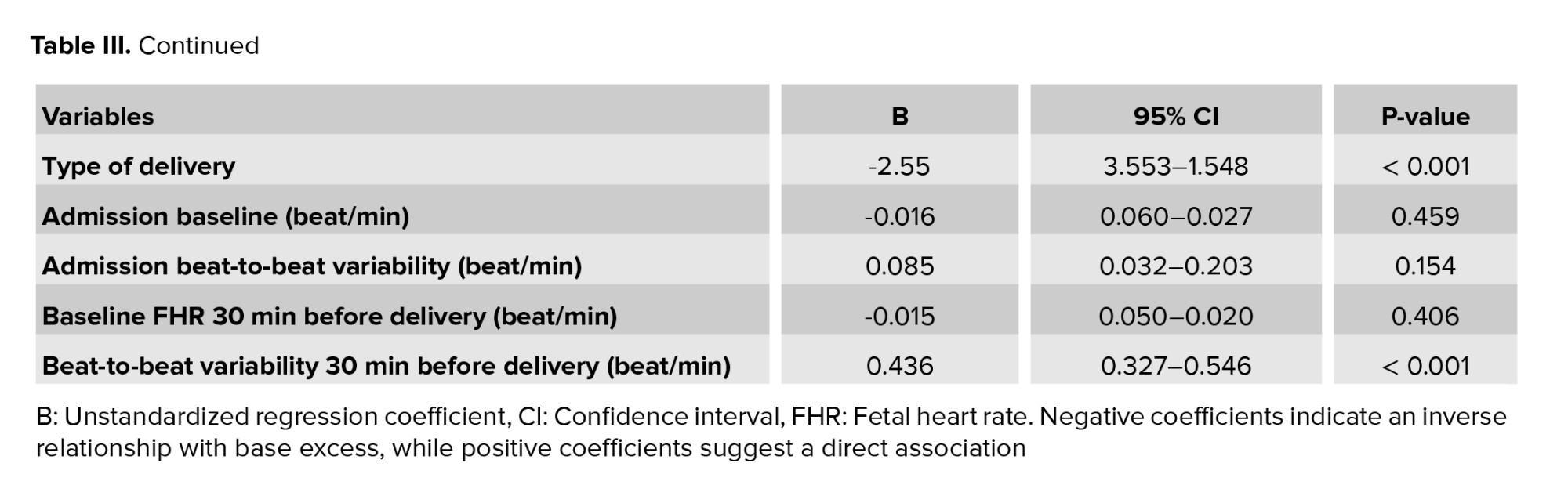
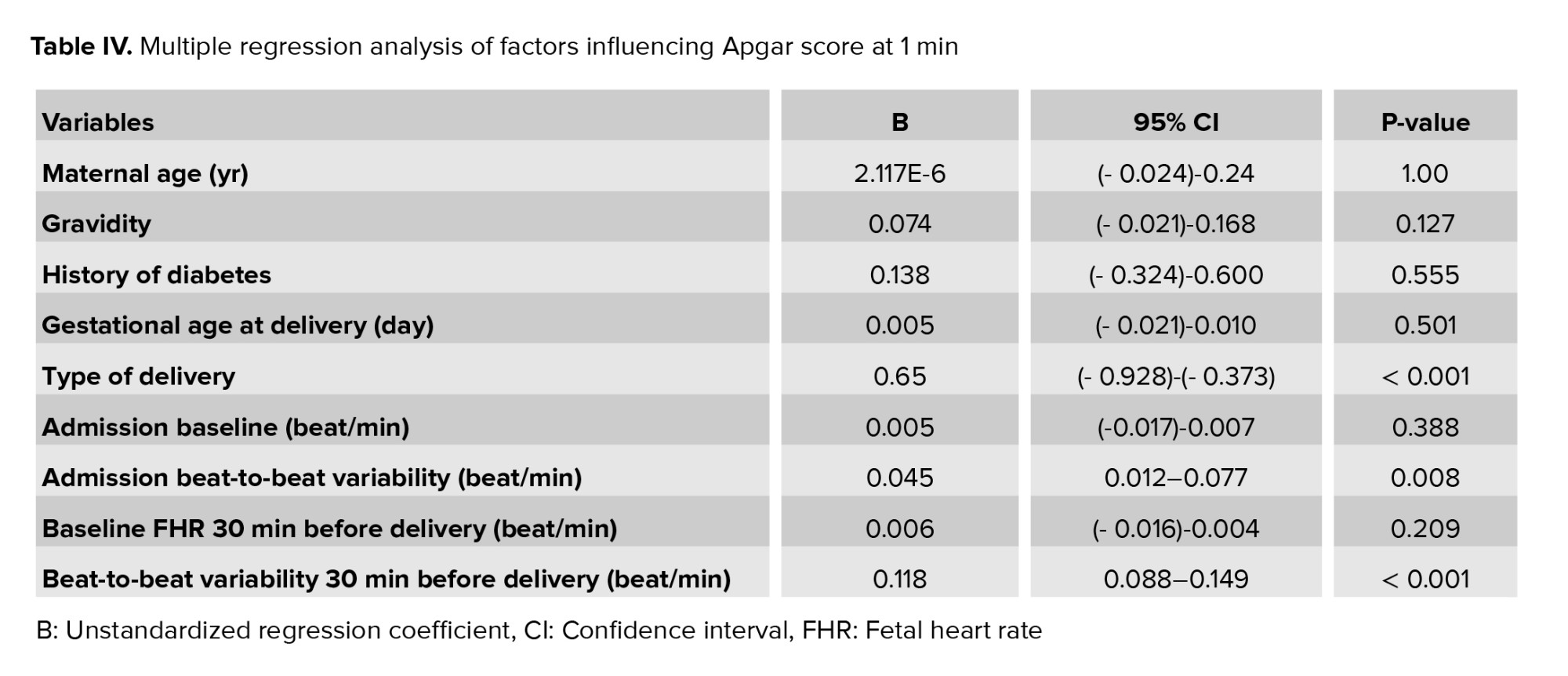
The median value of pH in cord blood was 7.32 (interquartile range: 7.30-7.34), while the median base excess was -3.6 (interquartile range: -4.47 to -2.9) among the participants. Multiple adjusted regression analysis revealed significant associations between neonatal pH and several factors, as shown in table II. The type of delivery (cesarean delivery vs. natural vaginal delivery), beat-to-beat variability during admission, NST, and the beat-to-beat variability during FHR tracing 30 min before delivery were found to be significantly associated with neonatal pH. Furthermore, table III demonstrates that the type of delivery and beat-to-beat variability during FHR monitoring 30 min before delivery were also significantly associated with base excess. However, no significant associations were observed between the remaining parameters and cord blood pH or base excess. Similarly, table IV highlights the factors influencing the Apgar score at 1 min, providing further insight into neonatal outcomes.
4. Discussion
The results of this study demonstrated a significant association between beat-to-beat variability during the admission NST and FHR monitoring conducted 30 min before delivery, with cord blood pH and Apgar score at 1 min. These associations remained significant even after adjusting for maternal age, gravidity, parity, gestational age at delivery, and maternal history of diabetes. Additionally, cord blood base excess was significantly correlated with both the 1-min Apgar score and beat-to-beat variability in FHR tracings 30 min before delivery.
While no significant differences were observed in baseline FHR and its changes during labor between neonates with acidosis and those with normal pH, notable differences were observed in beat-to-beat variability and its changes during labor.
Predicting neonatal acidosis during labor is crucial due to its association with an increased risk of neonatal mortality and morbidity, including adverse neurological outcomes (7, 9). The NST is commonly used to evaluate fetal well-being, particularly in pregnant women with a history of medical complications or existing fetal complications (10). In a retrospective study of 314 term neonates using the National Institute of Child Health and Human Development categories for FHR tracing, an abnormal FHR pattern was associated with neonatal acidosis, low pH, and more negative base excess (11). Moreover, research has indicated that not only the degree of pathological FHR tracing but also the duration of abnormalities correlates with neonatal outcomes (12).
Beat-to-beat variability plays an important role in evaluating neonatal asphyxia. Absent beat-to-beat variability has been linked to fetal distress, and approximately 40% of fetuses with non-reactive NST exhibit distress (13). Even when beat-to-beat variability was within the normal range, changes in its pattern were associated with pH levels and Apgar scores.
Due to challenges in continuous maternal monitoring in developing countries, a study in India investigated the relationship between admission NST results, cord blood pH, and neonatal outcomes. The findings indicated a significant association between neonatal distress and abnormal NST results, with admission NST showing approximately 90% sensitivity in predicting fetal distress (14). Another retrospective study of 552 neonates found that both the mean and coefficient of variation of FHR were significantly associated with neonatal pH, base excess, and Apgar score at 1 min (15). However, in the present study, only beat-to-beat variability of FHR showed a significant association with neonatal pH.
A separate study compared neonates with severe acidosis (pH < 7) to those with normal pH and found that bradycardia and late decelerations were significantly associated with severe acidosis, though decreased beat-to-beat variability was not (13). A recent study examining increased variability during FHR monitoring 1 hr before delivery found a significant association between elevated variability and lower cord blood pH (16). It should be noted that in this study, the beat-to-beat variabilities remained either within the normal range or lower than the normal range. Consequently, we were unable to assess the impact of increased variability on neonatal cord blood pH levels.
Indeed, predicting neonatal acidosis is of great importance, and FHR monitoring is a critical tool in assessing fetal well-being. The strength of this study was its examination of the relationship between FHR tracing parameters and neonatal outcomes. However, it is crucial to acknowledge the main limitation of this study, which is the small sample size. Therefore, further research with a larger number of participants is needed to validate and confirm these findings. Conducting studies with a larger sample size will enhance statistical power and improve the reliability of the results.
5. Conclusion
Based on the results of this study, it is recommended that fetal monitoring during pregnancy should be thoroughly documented, and any changes observed should be taken into consideration, even if the measured parameters fall within the normal range. The study suggests that a reduction in beat-to-beat variability of FHR, even within the normal range, may be associated with poor outcomes. Therefore, it is important to closely monitor and evaluate FHR patterns to ensure the well-being of the fetus.
Data Availability
Data sharing is available by contacting the corresponding author.
Author Contributions
All authors met the ICMJE criteria for authorship. S. Hantoushzadeh and F. Golshahi conceptualized and designed the study, developed the methodology, and provided supervision throughout the project. Sh. Rahimi and M. Ghaemi were responsible for data acquisition, including patient recruitment and data collection, and contributed to data curation. M. Dashtkoohi and N. Eshraqi conducted formal statistical analysis and verified the analytical methods. M. Dashtkoohi and M. Haddadi performed the investigation, interpreted the data, and validated the results. M. Dashtkoohi and E. Sedighi drafted the initial manuscript. M. Haddadi, M. Dashtkoohi, and E. Sedighi: Critically revised the manuscript for important intellectual content. All authors reviewed and approved the final version of the manuscript and agree to be accountable for all aspects of the work, ensuring its accuracy and integrity.
Acknowledgments
This study was not financially supported. We acknowledge the use of Grok 3, an AI assistant developed by xAI, for assistance in improving the language and clarity of the manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest.
Fetal heart rate (FHR) monitoring is a widely used technique for evaluating fetal well-being during labor due to its non-invasive nature, cost-effectiveness, and ease of implementation. The assessment of fetal health during labor aims to prevent fetal mortality, neurological complications, and unnecessary interventions during labor (1, 2). While normal results of fetal monitoring suggest that the fetus is receiving sufficient oxygen, cardiotocography, also known as a non-stress test (NST) has been found to have low sensitivity during labor and is associated with a high rate of false positives, leading to an increased number of cesarean deliveries due to suspected fetal distress (3).
To accurately identify intrauterine fetal hypoxia, the analysis of fetal scalp blood pH during childbirth has been considered a reliable method. However, this approach has its limitations, including complexity, high cost, and the requirement of a relatively large amount of blood (30-50 ml). Additionally, there is a failure rate of 11-20% in obtaining a suitable sample for pH analysis (4, 5). Metabolic acidosis is associated with both short- and long-term neurological morbidity in neonates (6). The threshold for defining acidosis in neonates varies, with mild acidosis typically characterized by an umbilical cord arterial blood pH < 7.2. It has been observed that lower neonatal pH levels are correlated with adverse neonatal outcomes, even in cases where the Apgar score at 5 min is within the normal range (7).
Timely diagnosis of fetal hypoxia or acidosis is crucial to minimize the risk of adverse neonatal outcomes, such as cerebral palsy. Hypoxia during childbirth can lead to changes in the fetal central nervous system, which directly affects fetal cardiac electrical activity and can potentially result in cerebral palsy (8).
Therefore, this study aimed to explore the relationship between changes in FHR patterns within the normal range during labor, umbilical cord arterial blood gas (ABG) analysis, and neonatal outcomes.
2. Materials and Methods
2.1. Study design and eligibility criteria
This cross-sectional study evaluated data from the medical records of all mothers and their neonates delivered at Yas hospital, Tehran, Iran, between August and December 2022. Maternal data included age, gravidity, parity, gestational age, history of medical conditions, prior surgeries, and delivery mode. Neonatal data comprised birth weight, sex, Apgar scores at 1 and 5 min, ABG parameters (pH, base excess, PCO₂, PO₂), and neonatal intensive care unit admission status.
The inclusion criteria were mothers older than 18 yr, with singleton pregnancies, gestational age of ≥ 37 wk (calculated based on crown-rump length measured in the first trimester), and candidates for natural vaginal delivery.
Exclusion criteria included cases of fetal growth restriction (estimated fetal weight < 10%), congenital abnormalities, hypoxic-ischemic encephalopathy, and seizures. These criteria were applied to ensure that the study population was representative of healthy term pregnancies and to minimize confounding factors that could influence the relationship between beat-to-beat variability and neonatal outcomes.
2.2. FHR monitoring
FHR monitoring was conducted for all participants. Recordings were taken twice: upon admission and 30 min before delivery, each session lasting at least 20 min. The Edan Express F9 fetal and maternal monitor (Edan Instruments Inc., China) was used for FHR recordings. Recorded data included baseline FHR, beat-to-beat variability, and their respective characteristics.
2.3. Umbilical cord ABG analysis
ABG samples were routinely obtained immediately after delivery. All participants were in the active phase of labor. Cesarean sections were performed only for those experiencing fetal distress, arrest of the active phase, or meconium-stained amniotic fluid. Within the 1st hr after birth, 1 ml of heparinized arterial blood was collected from all neonates, placed on ice, and sent to the hospital laboratory for acid-base analysis. This was done by clamping and cutting a 10-20 cm segment of the umbilical cord and collecting ABG samples from the umbilical cord artery. Neonates were divided into 2 groups based on ABG pH: those with acidosis (pH < 7.2) and those without acidosis (pH ≥ 7.2).
2.4. Sample size
The sample size for this cross-sectional study was determined using a priori power analysis for multiple linear regression with 4 predictors, based on the primary objective of evaluating the association between FHR variability and umbilical cord ABG parameters. Assuming a medium effect size (f² = 0.15) as per Cohen's (1988) guidelines, an alpha level of 0.05, and a desired statistical power of 0.80, the minimum required sample size was calculated to be 140 participants. This calculation was performed using an online sample size calculator (Soper, 2025, available at: https://www.danielsoper.com/statcalc/calculator.aspx?id = 1).
Due to practical constraints, including time limitations and availability of eligible participants, a total of 120 participants were included in the study. While this number is slightly below the calculated minimum, it was considered adequate for the exploratory nature of this cross-sectional study, providing sufficient statistical power for preliminary analyses and laying a foundation for future research with larger sample sizes.
2.5. Ethical Considerations
The study was approved by the Research Ethics Committee of Imam Khomeini hospital Complex, Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.IKHC.REC.1401.100). Written informed consent was obtained from each participant.
2.6. Statistical Analysis
Statistical analysis was conducted using SPSS software (version 24.0, SPSS Inc., Chicago, Illinois, USA). Descriptive statistics, such as mean and standard deviation, were used for quantitative variables, while frequencies and percentages were used for qualitative variables. The Chi-square test or Fisher's exact test was employed to compare qualitative variables. Independent t test were used to compare means between 2 groups for normally distributed quantitative variables, while the Mann-Whitney test was used for non-normal data. Multiple regression analysis was utilized to examine the correlation between umbilical cord pH, base excess, and Apgar score at 1 min with associated factors and FHR monitoring parameters. The significance level for all statistical analyses was set at 0.05.
3. Results
Initially, 133 pregnant women met the inclusion criteria; however, 13 were excluded due to fetal growth restriction (estimated fetal weight < 10%), congenital abnormalities, hypoxic-ischemic encephalopathy, and seizures. Therefore, the final evaluation was carried out on 120 neonates.
The mean gestational age at delivery was 270.3 ± 7.7 days. The neonates were divided into 2 groups based on the pH value of cord blood. Among them, 17 neonates (14.2%) had a pH value of < 7.2, indicating neonatal acidosis, while the remaining 103 neonates (85.8%) did not have acidosis (pH ≥ 7.2).
All women in the study had entered the active phase of labor. Among them, 9 (7.5%) underwent caesarean section due to fetal distress, 22 (18.3%) due to arrest of the active phase of labor, and 8 (6.7%) due to meconium-stained amniotic fluid.
Table I presents the characteristics and outcomes of maternal and neonatal factors. No significant differences were observed between the groups in terms of maternal age, primigravida pregnancy, nullipara pregnancy, abortion history, past medical history (diabetes, hypertension, and hypothyroidism), and gestational age at delivery. However, the rate of cesarean section was significantly higher in neonates with a cord blood pH < 7.2 compared to neonates without acidosis (p < 0.001). Furthermore, both the Apgar score at 1 min and the Apgar score at 5 min were significantly higher in neonates with umbilical cord pH ≥ 7.2 compared to those with lower pH values (p < 0.001).
The study found that no significant differences were observed in the median baseline FHR between the groups during admission and 30 min before delivery FHR monitoring. Furthermore, it was observed that the beat-to-beat variability during admission and 30 min before delivery FHR monitoring were significantly lower in neonates with acidosis compared to normal neonates, with p = 0.002 and < 0.001, respectively. Moreover, the beat-to-beat variability decreased during labor, and the extent of reduction was also found to be significantly different (p < 0.001).
The median value of pH in cord blood was 7.32 (interquartile range: 7.30-7.34), while the median base excess was -3.6 (interquartile range: -4.47 to -2.9) among the participants. Multiple adjusted regression analysis revealed significant associations between neonatal pH and several factors, as shown in table II. The type of delivery (cesarean delivery vs. natural vaginal delivery), beat-to-beat variability during admission, NST, and the beat-to-beat variability during FHR tracing 30 min before delivery were found to be significantly associated with neonatal pH. Furthermore, table III demonstrates that the type of delivery and beat-to-beat variability during FHR monitoring 30 min before delivery were also significantly associated with base excess. However, no significant associations were observed between the remaining parameters and cord blood pH or base excess. Similarly, table IV highlights the factors influencing the Apgar score at 1 min, providing further insight into neonatal outcomes.
4. Discussion
The results of this study demonstrated a significant association between beat-to-beat variability during the admission NST and FHR monitoring conducted 30 min before delivery, with cord blood pH and Apgar score at 1 min. These associations remained significant even after adjusting for maternal age, gravidity, parity, gestational age at delivery, and maternal history of diabetes. Additionally, cord blood base excess was significantly correlated with both the 1-min Apgar score and beat-to-beat variability in FHR tracings 30 min before delivery.
While no significant differences were observed in baseline FHR and its changes during labor between neonates with acidosis and those with normal pH, notable differences were observed in beat-to-beat variability and its changes during labor.
Predicting neonatal acidosis during labor is crucial due to its association with an increased risk of neonatal mortality and morbidity, including adverse neurological outcomes (7, 9). The NST is commonly used to evaluate fetal well-being, particularly in pregnant women with a history of medical complications or existing fetal complications (10). In a retrospective study of 314 term neonates using the National Institute of Child Health and Human Development categories for FHR tracing, an abnormal FHR pattern was associated with neonatal acidosis, low pH, and more negative base excess (11). Moreover, research has indicated that not only the degree of pathological FHR tracing but also the duration of abnormalities correlates with neonatal outcomes (12).
Beat-to-beat variability plays an important role in evaluating neonatal asphyxia. Absent beat-to-beat variability has been linked to fetal distress, and approximately 40% of fetuses with non-reactive NST exhibit distress (13). Even when beat-to-beat variability was within the normal range, changes in its pattern were associated with pH levels and Apgar scores.
Due to challenges in continuous maternal monitoring in developing countries, a study in India investigated the relationship between admission NST results, cord blood pH, and neonatal outcomes. The findings indicated a significant association between neonatal distress and abnormal NST results, with admission NST showing approximately 90% sensitivity in predicting fetal distress (14). Another retrospective study of 552 neonates found that both the mean and coefficient of variation of FHR were significantly associated with neonatal pH, base excess, and Apgar score at 1 min (15). However, in the present study, only beat-to-beat variability of FHR showed a significant association with neonatal pH.
A separate study compared neonates with severe acidosis (pH < 7) to those with normal pH and found that bradycardia and late decelerations were significantly associated with severe acidosis, though decreased beat-to-beat variability was not (13). A recent study examining increased variability during FHR monitoring 1 hr before delivery found a significant association between elevated variability and lower cord blood pH (16). It should be noted that in this study, the beat-to-beat variabilities remained either within the normal range or lower than the normal range. Consequently, we were unable to assess the impact of increased variability on neonatal cord blood pH levels.
Indeed, predicting neonatal acidosis is of great importance, and FHR monitoring is a critical tool in assessing fetal well-being. The strength of this study was its examination of the relationship between FHR tracing parameters and neonatal outcomes. However, it is crucial to acknowledge the main limitation of this study, which is the small sample size. Therefore, further research with a larger number of participants is needed to validate and confirm these findings. Conducting studies with a larger sample size will enhance statistical power and improve the reliability of the results.
5. Conclusion
Based on the results of this study, it is recommended that fetal monitoring during pregnancy should be thoroughly documented, and any changes observed should be taken into consideration, even if the measured parameters fall within the normal range. The study suggests that a reduction in beat-to-beat variability of FHR, even within the normal range, may be associated with poor outcomes. Therefore, it is important to closely monitor and evaluate FHR patterns to ensure the well-being of the fetus.
Data Availability
Data sharing is available by contacting the corresponding author.
Author Contributions
All authors met the ICMJE criteria for authorship. S. Hantoushzadeh and F. Golshahi conceptualized and designed the study, developed the methodology, and provided supervision throughout the project. Sh. Rahimi and M. Ghaemi were responsible for data acquisition, including patient recruitment and data collection, and contributed to data curation. M. Dashtkoohi and N. Eshraqi conducted formal statistical analysis and verified the analytical methods. M. Dashtkoohi and M. Haddadi performed the investigation, interpreted the data, and validated the results. M. Dashtkoohi and E. Sedighi drafted the initial manuscript. M. Haddadi, M. Dashtkoohi, and E. Sedighi: Critically revised the manuscript for important intellectual content. All authors reviewed and approved the final version of the manuscript and agree to be accountable for all aspects of the work, ensuring its accuracy and integrity.
Acknowledgments
This study was not financially supported. We acknowledge the use of Grok 3, an AI assistant developed by xAI, for assistance in improving the language and clarity of the manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Perinatology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |