Thu, Jan 29, 2026
[Archive]
Volume 23, Issue 2 (February 2025)
IJRM 2025, 23(2): 207-216 |
Back to browse issues page
Ethics code: 0701-PF-2020M26
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jwad M A, Hussein Khaleefah M, Abd AlFattah Naser R. Impact of ovarian hyperstimulation syndrome on intracytoplasmic sperm injection outcomes in poly-cystic ovarian syndrome women: A cross-sectional study. IJRM 2025; 23 (2) :207-216
URL: http://ijrm.ir/article-1-3369-en.html
URL: http://ijrm.ir/article-1-3369-en.html
1- Department of Physiology, High Institute for Infertility Diagnosis and Assisted Reproductive Technologies, Al-Nahrain University, Baghdad, Iraq. , dr.mufedaali@st.nahrainuniv.edu.iq
2- Department of Applied Embryology, High Institute for Infertility Diagnosis and Assisted Reproductive Technologies, Al-Nahrain University, Baghdad, Iraq.
2- Department of Applied Embryology, High Institute for Infertility Diagnosis and Assisted Reproductive Technologies, Al-Nahrain University, Baghdad, Iraq.
Abstract: (869 Views)
Background: Polycystic ovarian syndrome (PCOS) is a complex disorder that affects the endocrine, metabolic, and reproductive systems. While controlled ovarian hyperstimulation can increase the number of oocytes retrieved and improve the number of good-quality embryos, it may also negatively affect oocyte maturity, embryo quality, endometrial receptivity, and pregnancy outcomes.
Objective: This study aimed to find out if ovarian hyperstimulation syndrome (OHSS) has negative effects on intracytoplasmic sperm injection outcomes in a sample of PCOS women.
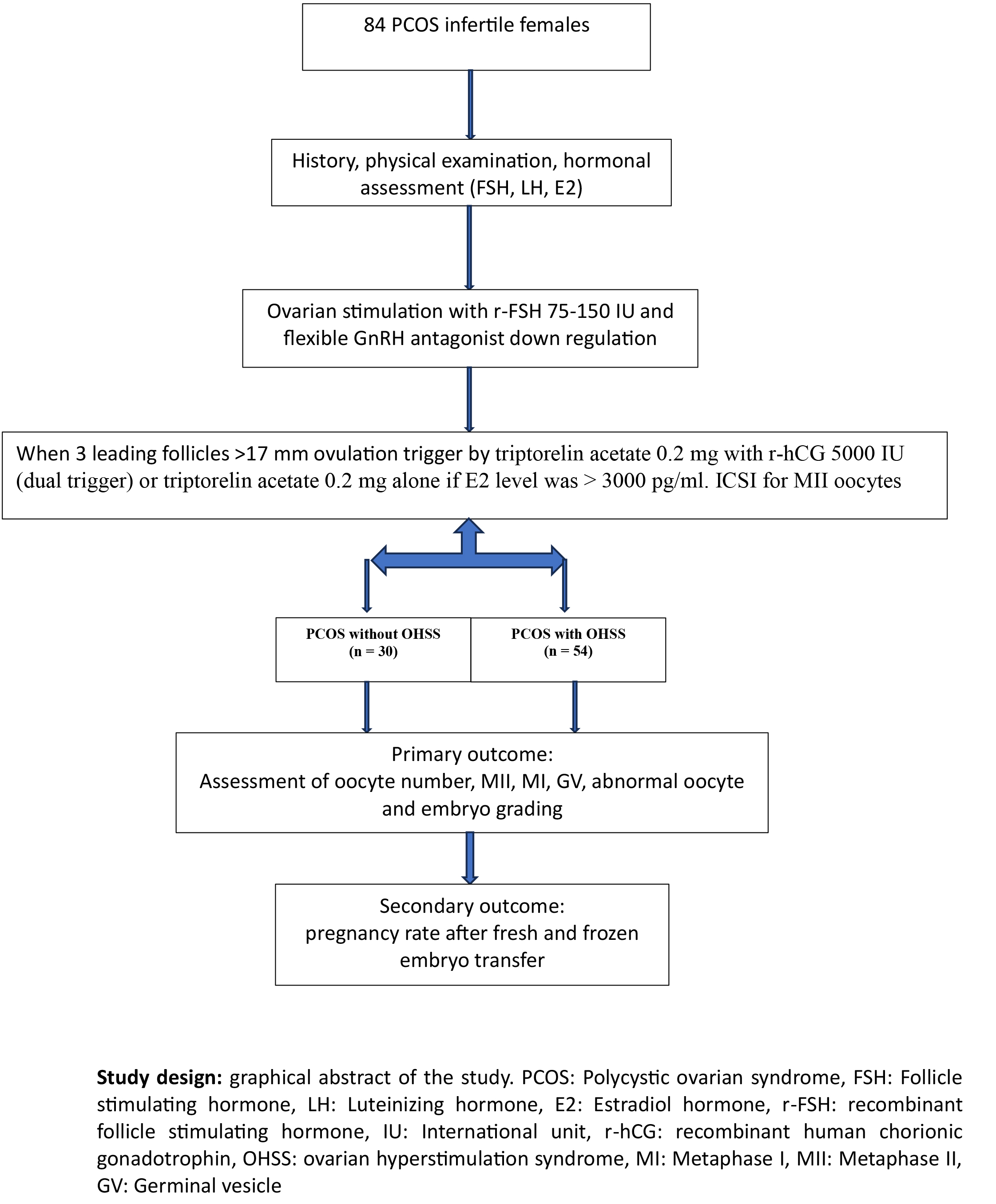
Materials and Methods: In this cross-sectional study, data of 84 PCOS women who underwent controlled ovarian stimulation using a flexible antagonist protocol-treated intracytoplasmic sperm injection cycles referred to the Infertility Department of Higher Institute for the Diagnosis of Infertility and Assisted Reproduction Techniques, Baghdad, Iraq between January 2020 and December 2023 was extracted from their medical records. Participants were categorized into 2 groups after undergoing controlled ovarian hyperstimulation protocol: PCOS with OHSS (n = 54) and PCOS without OHSS (n = 30). The dosage was tailored based on age, body mass index, and response to previous stimulation cycles, if applicable. The trigger was administered using decapeptyl 0.2 mg alone or in combination with recombinant human chorionic gonadotrophin, depending on the estradiol levels at the time of the trigger.
Results: Significant differences were observed in the duration of stimulation (p = 0.005), oocyte yield (p = 0.001), mature oocytes (p = 0.001), and fertilized oocytes (p = 0.036); however, no significant difference was observed, neither in number of good quality embryos (p = 0.52) nor in pregnancy rate (p = 0.54) after fresh and frozen embryo transfer between the 2 groups.
Conclusion: OHSS does not affect the embryo quality or pregnancy rate in PCOS women.
Objective: This study aimed to find out if ovarian hyperstimulation syndrome (OHSS) has negative effects on intracytoplasmic sperm injection outcomes in a sample of PCOS women.
Materials and Methods: In this cross-sectional study, data of 84 PCOS women who underwent controlled ovarian stimulation using a flexible antagonist protocol-treated intracytoplasmic sperm injection cycles referred to the Infertility Department of Higher Institute for the Diagnosis of Infertility and Assisted Reproduction Techniques, Baghdad, Iraq between January 2020 and December 2023 was extracted from their medical records. Participants were categorized into 2 groups after undergoing controlled ovarian hyperstimulation protocol: PCOS with OHSS (n = 54) and PCOS without OHSS (n = 30). The dosage was tailored based on age, body mass index, and response to previous stimulation cycles, if applicable. The trigger was administered using decapeptyl 0.2 mg alone or in combination with recombinant human chorionic gonadotrophin, depending on the estradiol levels at the time of the trigger.
Results: Significant differences were observed in the duration of stimulation (p = 0.005), oocyte yield (p = 0.001), mature oocytes (p = 0.001), and fertilized oocytes (p = 0.036); however, no significant difference was observed, neither in number of good quality embryos (p = 0.52) nor in pregnancy rate (p = 0.54) after fresh and frozen embryo transfer between the 2 groups.
Conclusion: OHSS does not affect the embryo quality or pregnancy rate in PCOS women.
Keywords: Polycystic ovary syndrome, Ovarian hyperstimulation syndrome, Intracytoplasmic sperm injection, Ovulation induction.
Type of Study: Original Article |
Subject:
Assisted Reproductive Technologies
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |