Wed, Jan 28, 2026
[Archive]
Volume 23, Issue 10 (October 2025)
IJRM 2025, 23(10): 827-842 |
Back to browse issues page
Ethics code: IR.TUMS.SPH.REC.1402.010
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Sajjadi H, Choobineh H, Safdari R. Presenting a conceptual model for decision support systems in infertility: A developmental study. IJRM 2025; 23 (10) :827-842
URL: http://ijrm.ir/article-1-3521-en.html
URL: http://ijrm.ir/article-1-3521-en.html
1- Department of Health Information Management and Medical Informatics, School of Allied Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Medical Laboratory Sciences, School of Allied Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran. & Zeoonosis Research Center, Tehran University of Medical Sciences, Tehran, Iran. ,hchobineh@tums.ac.ir
2- Department of Medical Laboratory Sciences, School of Allied Medical Sciences, Tehran University of Medical Sciences, Tehran, Iran. & Zeoonosis Research Center, Tehran University of Medical Sciences, Tehran, Iran. ,
Full-Text [PDF 581 kb]
(375 Downloads)
| Abstract (HTML) (258 Views)
Full-Text: (4 Views)
1. Introduction
Fertility and having children are the main focus of people who have started their lives together, and the issue of infertility can be one of the most critical drivers of concern for these people (1). Infertility is defined as the failure of a couple to conceive after 1 yr of regular, unprotected intercourse (2). Due to the importance of infertility, the World Health Organization has introduced infertility as a public health issue worldwide (3-5). This condition is estimated to affect 8-12% of couples of reproductive age worldwide, comprising 186 million people (6, 7). In Iran, the overall prevalence of infertility was reported as 7.88% (8). Increasing public awareness, easy availability, and improvement of infertility treatments are the main reasons why more couples are seeking infertility treatment today.
Reproductive medicine has seen huge strides in artificial intelligence (AI) technology, greatly improving how we diagnose and treat reproductive disorders (9). AI and its applications in various fields, including medicine, have expanded in the last decade. Machine learning (ML), a subset of AI, enables systems to identify complex patterns in biomedical data and use them to guide clinical practice (10-12). Decision-support systems (DSS) demonstrate how AI is used in medical decision-making and offer treatment and diagnostic suggestions based on it (13). Many DSSs using ML tools have been developed to improve healthcare and reduce costs. Their aim is to help healthcare providers make the right decisions by giving them medical recommendations. These systems will not replace human experts but will be auxiliary (14). DSSs are rule-based tools that provide intelligent, filtered data at the right time to improve individual care. Due to the high volume of clinical data, using these systems in clinical decision-making has become vital. These systems can help health professionals by providing clinical information, guidelines, and warnings (15). Additionally, clinical DSS (CDSSs) can help clinicians make timely and accurate decisions in complex situations, reducing the workload on medical staff (16).
Several studies have developed CDSSs for treating infertility. Abu-Naser and Alhabbash studied male infertility and created an expert system that used collected data to diagnose the condition and recommend suitable treatment (17). Another study by Letterie et al. focused on decision support for ovarian stimulation during in vitro fertilization (IVF). They demonstrated that their proposed predictive algorithm is highly accurate and aligns with evidence-based decisions made by expert teams during ovarian stimulation and IVF. The authors claimed that their algorithm improves clinical decision-making during IVF (18).
Considering the importance of infertility and its effects on people’s lives, as well as the challenges mentioned for infertility treatment, including the probability of success, high treatment costs, and possible risks to the health of the mother and child, it is essential to make the right decision and the appropriate treatment method by infertility specialists. Based on the research team’s investigations, no study has been conducted to determine the factors required for developing a DSS for infertility and provide a conceptual model for such a system in Iran. Therefore, this study aimed to present a comprehensive conceptual model for DSS in infertility.
2. Materials and Methods
2.1. Identification of requirements
This developmental study was conducted from April-November 2024 and consisted of 3 steps. First, it was necessary to determine the characteristics and data required for DSSs in infertility. Common scientific databases were used to search for and access existing infertility systems. Then, search engines and AI tools were used to identify similar systems. Finally, for more certainty, the opinions of infertility experts were obtained. Each of these 3 steps is explained separately in the following:
2.2. Step 1: literature review
We conducted this step based on the PRISMA extension for scoping reviews (PRISMA-ScR) checklist (19).
2.2.1. Search strategy
Keywords were searched in PubMed, Web of Science, and Scopus databases to identify the characteristics of DSSs in infertility, and the available articles in this field were identified. The first category’s keywords were “Clinical Decision Support Systems”, “Expert Systems”, “Smart Systems”, “Automated Systems”, “Software”, “Applications”, and “Electronic Health Records”. The second category's keywords were “Infertility”, “Sterility”, and “Reproductive Sterility”.
2.2.2. Inclusion and exclusion criteria
The study’s inclusion criteria were original articles written in English that examined data elements for implementing DSSs in infertility. Additionally, the exclusion criteria included studies that did not align with the study’s objectives, publications in languages other than English, review articles, conference paper abstracts, and books and book chapters.
2.2.3. Data extraction process
One of the researchers (HS) reviewed the included articles and identified the required data elements and features.
2.3. Step 2: finding similar systems
In second step, popular search engines like Google, Yahoo, and Bing were used. The search procedure was such that, first, the systems that were identified from the first method (scientific databases) were searched using the phrase "systems similar to" in the mentioned search engines. Similar systems not mentioned in scientific articles were identified by relying on this method. Also, to complete the searches, AI tools such as ChatGPT, Gemini, and Perplexity were asked to introduce existing systems in infertility. Furthermore, describe the characteristics and data required in DSS for infertility.
2.3.1. Inclusion and exclusion criteria
The inclusion criteria for systems included systems found through reputable and well-known articles and search engines in health, treatment, and infertility. Although systems that had been implemented and used by users were also excluded from the study.
2.3.2. Data extraction process
One of the researchers (HS) reviewed the included systems and identified the required data elements and features. The researcher (HS) then combined the factors identified in this step and the previous step, and made a questionnaire to gather the experts’ opinions.
2.4. Step 3: experts’ opinion
To identify the importance of each of the requirements identified for the infertility DSS in the previous 2 steps, it was necessary to determine the opinion of infertility experts about each requirement. To determine the opinion of the experts, a researcher-made questionnaire based on a 5-point Likert scale according to the degree of agreement from 1 to 5 in the form of 5 = completely agree, 4 = agree, 3 = no opinion, 2 = disagree, and 1 = completely disagree, was designed. The criterion for including the requirements was to achieve a level of at least 70% agreement.
For expert opinion, the participants from the “23rd International Congress of Iranian Society for Reproductive Medicine” were considered as the research community of this study. The participants mentioned earlier were specialists in the field of infertility treatment. According to Morgan table (20), 32 participants were selected as the sample group and invited to complete the questionnaire, which was accessible via an online link and QR code. For this study, the authors created an online survey, including 49 questions in 5 domains on Porsline’s website to collect experts’ opinions. Porsline is a web platform that helps researchers create, distribute, collect data from, and analyze surveys (21). Cronbach’s alpha was used to study the questionnaire’s reliability, which was confirmed with a value of 0.78. The research team also confirmed its validity with content validity ratio of 0.60. In the last step, based on the experts questionnaire results and identification of each feature that received the desired score, a conceptual model of DSSs in infertility was designed and presented.
2.5. Risk of bias and quality assessment
A systematic assessment of evidence through a critical appraisal is not obligatory in scoping reviews (22). Since assessing the trustworthiness, reliability, and bias of evidence adds value, one of the researchers (HS) evaluated the risk of bias in the included studies using the Joanna Briggs Institute (JBI) critical appraisal guidelines. Because different types of papers were included, we utilized the checklist for qualitative research (23) and the checklist for systematic reviews and research syntheses (24). These quality assessment checklists comprise 11 questions and offer 4 options: “Yes”, “No”, “Unclear”, and “Not Applicable” to evaluate the quality of included studies. Articles were included if they met more than half of the JBI criteria.
2.6. Ethical Considerations
This study was approved by the Ethics Committee of the Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.SPH.REC.1402.010). Verbal informed consent was obtained from all 32 infertility experts before conducting the study. Since the questionnaires were collected anonymously based on the Porsline platform, the confidentiality of the data was maintained by the research team.
2.7. Statistical Analysis
In this study, the Statistical Package for the Social Sciences software, version 24.0 (SPSS Inc., Chicago, Illinois, USA) was used to analyze numerical data from a researcher-made questionnaire and to verify its reliability with Cronbach’s alpha.
3. Results
3.1. Step 1: scoping literature review
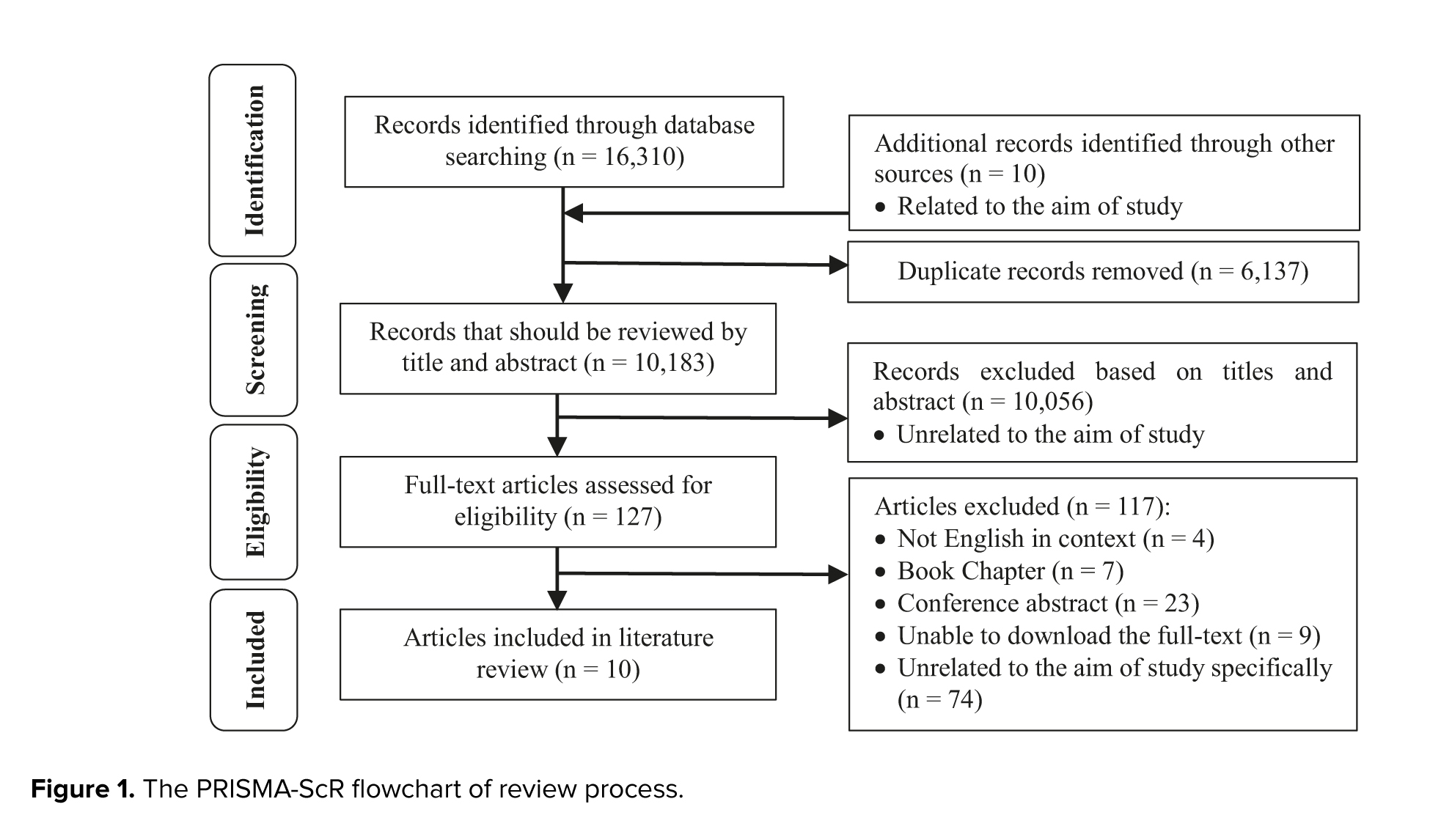
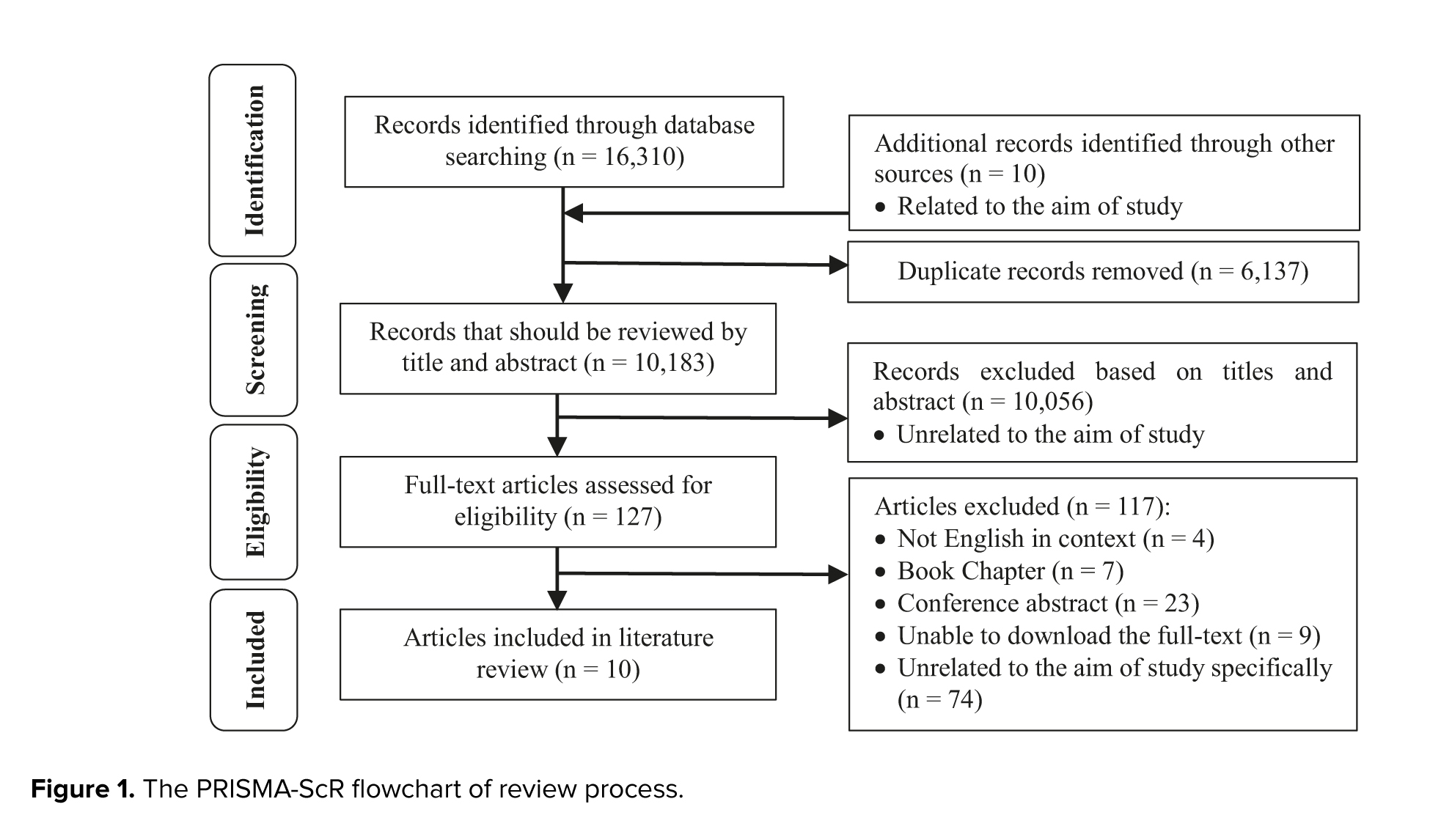
After searching PubMed, Scopus, and Web of Science, we identified 16,310 potentially relevant articles. We removed duplicates (n = 6137) and conducted further searches on Google Scholar, which led to the inclusion of 10 studies specifically related to our aim. We excluded 10,056 articles based on title and abstract due to low relevance, and only screened 127 full-text articles. Following a thorough review of all articles against eligibility criteria, we selected 10 articles for the study. Figure 1 illustrates the PRISMA flowchart indicating results of identification and screening process.
3.1.1. Attributes of the included studies
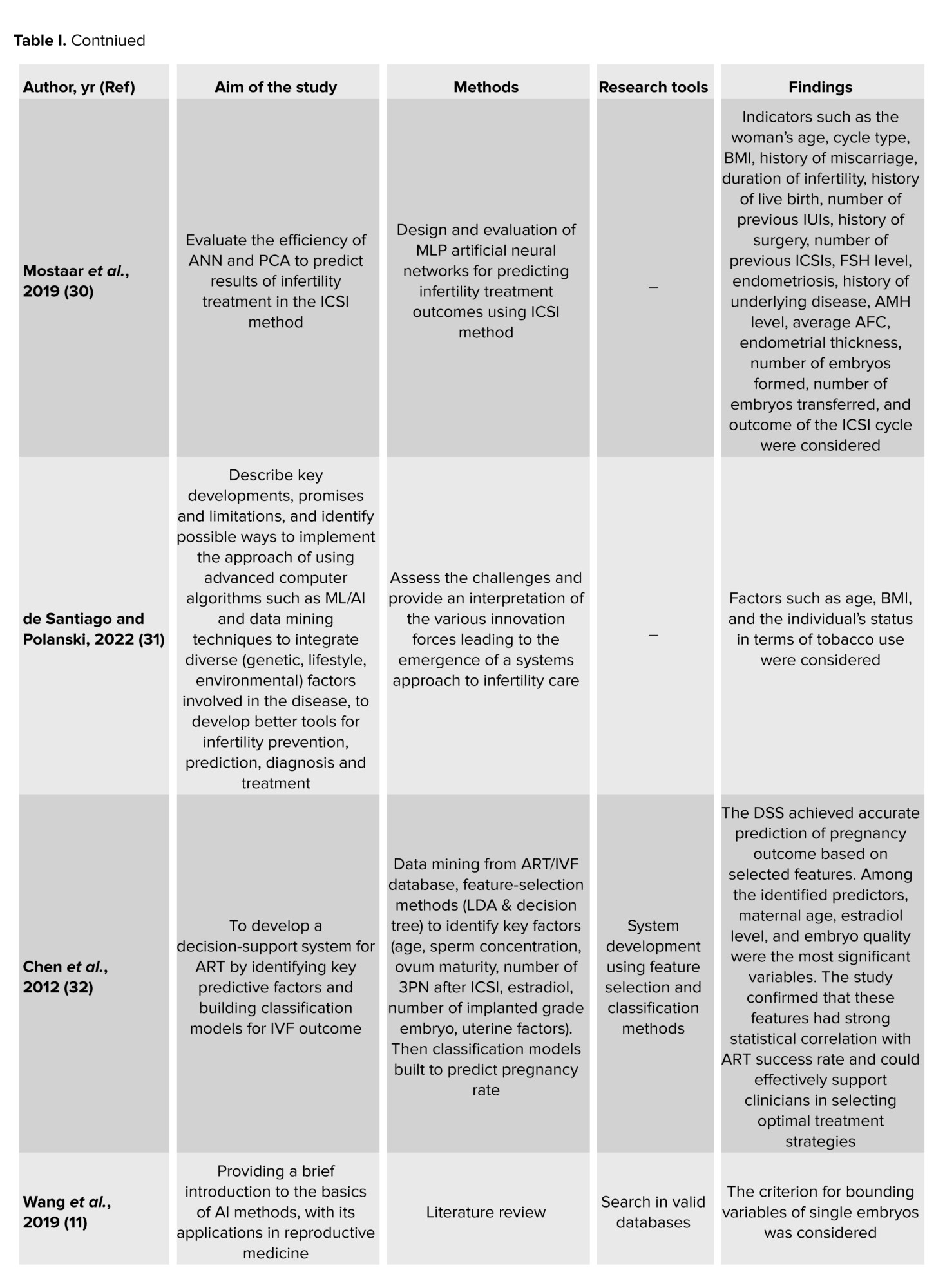
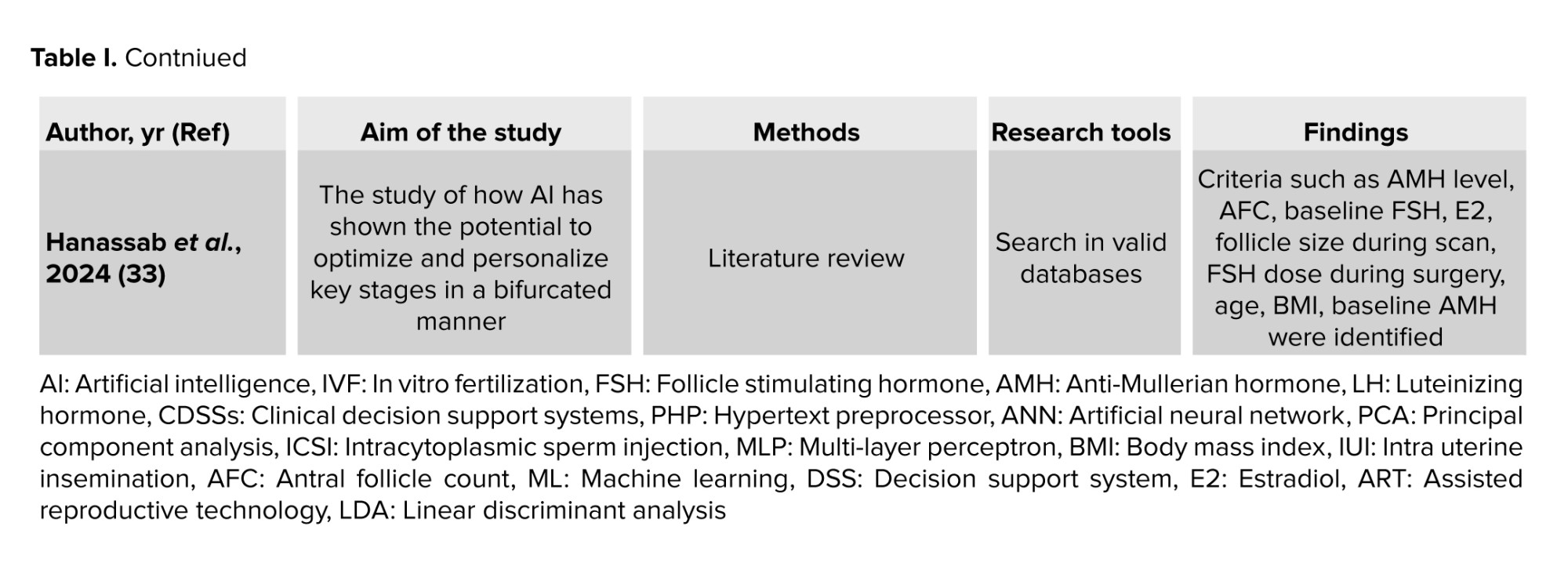
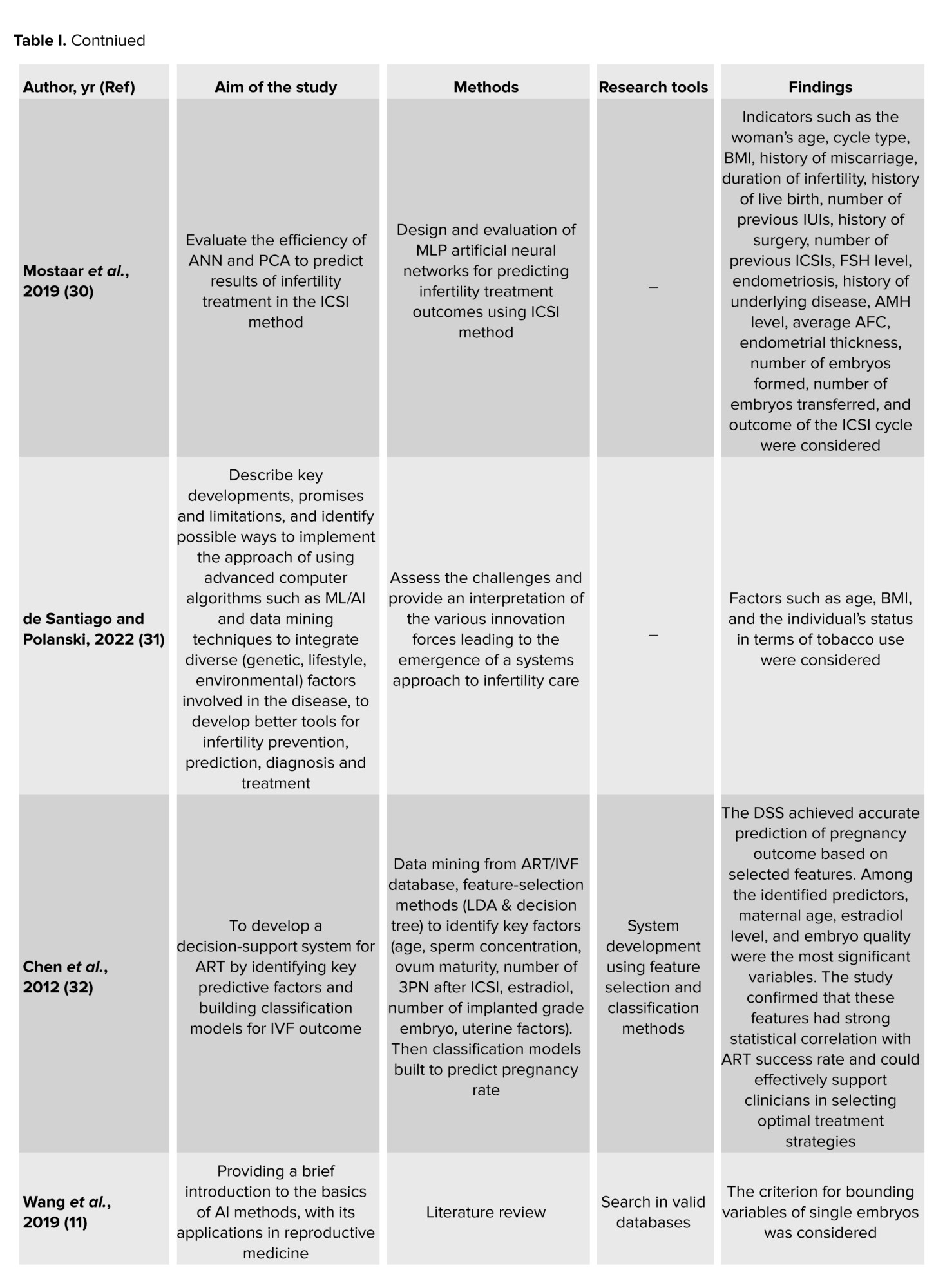
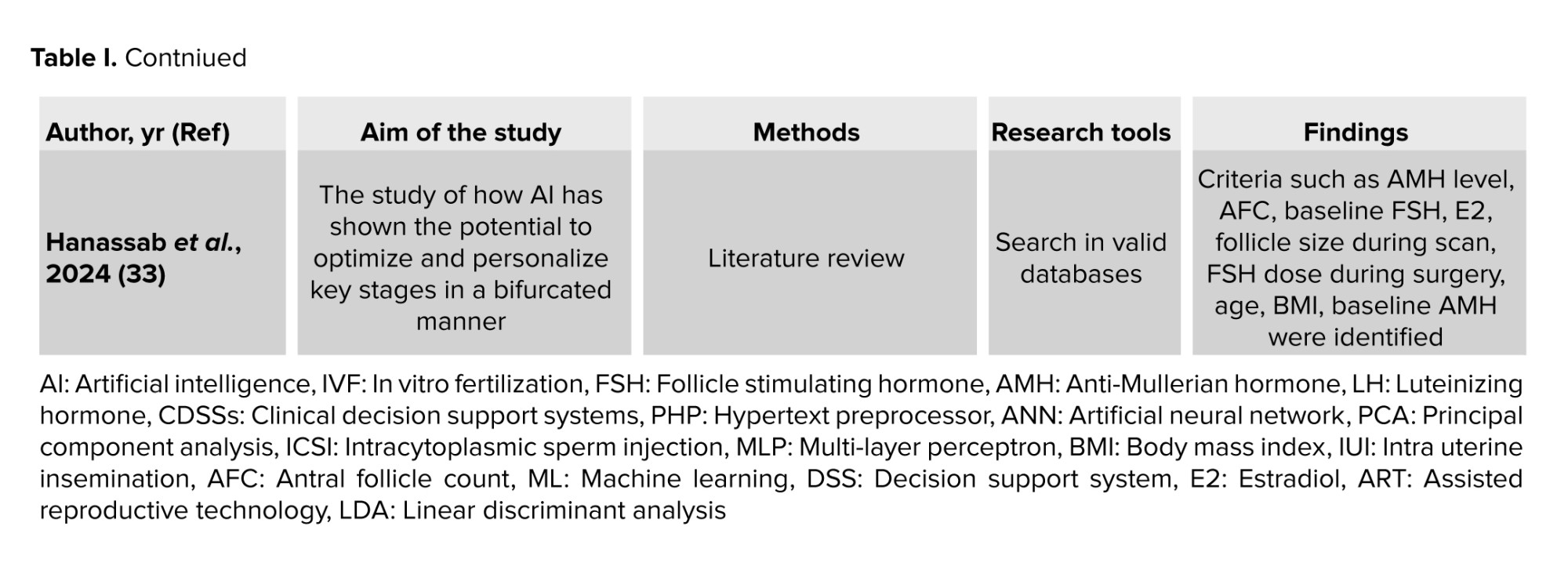
Table I provides a summary of characteristics of the included studies.
3.2. Step 2: finding similar systems
71 potentially relevant systems were identified from popular search engines like Google, Yahoo, and Bing, as well as AI tools such as ChatGPT, Gemini, and Perplexity. We excluded 58 systems that were implemented and used by users, and finally, 13 systems were included in the study for further investigations.
3.3. Step 3: experts’ opinion
Our researcher-made questionnaire included 49 questions in 5 domains, including main features of the system (11 questions), system data (patient information management/registry data and recommended treatment methods) (19 questions), system data (prediction module – predicting the likelihood of having children for single individuals and the probability of fertility for couples) (11 questions), system data (data for the patient prediction section – predicting fertility probability for couples – additional data related to couples) (5 questions), and secondary features of the system (3 questions). Using this questionnaire, in addition to married people, we can also find out for single people what data elements we should have to predict their fertility/infertility in the future.
32 experts, 13 (41%) male and 19 (59%) female, completed the questionnaire. The participants expertise was as follows: 8 obstetrician/gynecologists, 14 embryologists, 6 urologists, and 4 midwives. About one-third (38%) were 36-45 yr old.
3.4. Identified features and data elements
Considering the importance of DSSs in infertility, it seems necessary to identify the features and data required in these systems. Additionally, an infrastructure should be provided to facilitate easier, higher-quality, and faster development of these systems. After implementing the study method, these features were extracted, categorized, and used in designing the conceptual model:
Fertility and having children are the main focus of people who have started their lives together, and the issue of infertility can be one of the most critical drivers of concern for these people (1). Infertility is defined as the failure of a couple to conceive after 1 yr of regular, unprotected intercourse (2). Due to the importance of infertility, the World Health Organization has introduced infertility as a public health issue worldwide (3-5). This condition is estimated to affect 8-12% of couples of reproductive age worldwide, comprising 186 million people (6, 7). In Iran, the overall prevalence of infertility was reported as 7.88% (8). Increasing public awareness, easy availability, and improvement of infertility treatments are the main reasons why more couples are seeking infertility treatment today.
Reproductive medicine has seen huge strides in artificial intelligence (AI) technology, greatly improving how we diagnose and treat reproductive disorders (9). AI and its applications in various fields, including medicine, have expanded in the last decade. Machine learning (ML), a subset of AI, enables systems to identify complex patterns in biomedical data and use them to guide clinical practice (10-12). Decision-support systems (DSS) demonstrate how AI is used in medical decision-making and offer treatment and diagnostic suggestions based on it (13). Many DSSs using ML tools have been developed to improve healthcare and reduce costs. Their aim is to help healthcare providers make the right decisions by giving them medical recommendations. These systems will not replace human experts but will be auxiliary (14). DSSs are rule-based tools that provide intelligent, filtered data at the right time to improve individual care. Due to the high volume of clinical data, using these systems in clinical decision-making has become vital. These systems can help health professionals by providing clinical information, guidelines, and warnings (15). Additionally, clinical DSS (CDSSs) can help clinicians make timely and accurate decisions in complex situations, reducing the workload on medical staff (16).
Several studies have developed CDSSs for treating infertility. Abu-Naser and Alhabbash studied male infertility and created an expert system that used collected data to diagnose the condition and recommend suitable treatment (17). Another study by Letterie et al. focused on decision support for ovarian stimulation during in vitro fertilization (IVF). They demonstrated that their proposed predictive algorithm is highly accurate and aligns with evidence-based decisions made by expert teams during ovarian stimulation and IVF. The authors claimed that their algorithm improves clinical decision-making during IVF (18).
Considering the importance of infertility and its effects on people’s lives, as well as the challenges mentioned for infertility treatment, including the probability of success, high treatment costs, and possible risks to the health of the mother and child, it is essential to make the right decision and the appropriate treatment method by infertility specialists. Based on the research team’s investigations, no study has been conducted to determine the factors required for developing a DSS for infertility and provide a conceptual model for such a system in Iran. Therefore, this study aimed to present a comprehensive conceptual model for DSS in infertility.
2. Materials and Methods
2.1. Identification of requirements
This developmental study was conducted from April-November 2024 and consisted of 3 steps. First, it was necessary to determine the characteristics and data required for DSSs in infertility. Common scientific databases were used to search for and access existing infertility systems. Then, search engines and AI tools were used to identify similar systems. Finally, for more certainty, the opinions of infertility experts were obtained. Each of these 3 steps is explained separately in the following:
2.2. Step 1: literature review
We conducted this step based on the PRISMA extension for scoping reviews (PRISMA-ScR) checklist (19).
2.2.1. Search strategy
Keywords were searched in PubMed, Web of Science, and Scopus databases to identify the characteristics of DSSs in infertility, and the available articles in this field were identified. The first category’s keywords were “Clinical Decision Support Systems”, “Expert Systems”, “Smart Systems”, “Automated Systems”, “Software”, “Applications”, and “Electronic Health Records”. The second category's keywords were “Infertility”, “Sterility”, and “Reproductive Sterility”.
2.2.2. Inclusion and exclusion criteria
The study’s inclusion criteria were original articles written in English that examined data elements for implementing DSSs in infertility. Additionally, the exclusion criteria included studies that did not align with the study’s objectives, publications in languages other than English, review articles, conference paper abstracts, and books and book chapters.
2.2.3. Data extraction process
One of the researchers (HS) reviewed the included articles and identified the required data elements and features.
2.3. Step 2: finding similar systems
In second step, popular search engines like Google, Yahoo, and Bing were used. The search procedure was such that, first, the systems that were identified from the first method (scientific databases) were searched using the phrase "systems similar to" in the mentioned search engines. Similar systems not mentioned in scientific articles were identified by relying on this method. Also, to complete the searches, AI tools such as ChatGPT, Gemini, and Perplexity were asked to introduce existing systems in infertility. Furthermore, describe the characteristics and data required in DSS for infertility.
2.3.1. Inclusion and exclusion criteria
The inclusion criteria for systems included systems found through reputable and well-known articles and search engines in health, treatment, and infertility. Although systems that had been implemented and used by users were also excluded from the study.
2.3.2. Data extraction process
One of the researchers (HS) reviewed the included systems and identified the required data elements and features. The researcher (HS) then combined the factors identified in this step and the previous step, and made a questionnaire to gather the experts’ opinions.
2.4. Step 3: experts’ opinion
To identify the importance of each of the requirements identified for the infertility DSS in the previous 2 steps, it was necessary to determine the opinion of infertility experts about each requirement. To determine the opinion of the experts, a researcher-made questionnaire based on a 5-point Likert scale according to the degree of agreement from 1 to 5 in the form of 5 = completely agree, 4 = agree, 3 = no opinion, 2 = disagree, and 1 = completely disagree, was designed. The criterion for including the requirements was to achieve a level of at least 70% agreement.
For expert opinion, the participants from the “23rd International Congress of Iranian Society for Reproductive Medicine” were considered as the research community of this study. The participants mentioned earlier were specialists in the field of infertility treatment. According to Morgan table (20), 32 participants were selected as the sample group and invited to complete the questionnaire, which was accessible via an online link and QR code. For this study, the authors created an online survey, including 49 questions in 5 domains on Porsline’s website to collect experts’ opinions. Porsline is a web platform that helps researchers create, distribute, collect data from, and analyze surveys (21). Cronbach’s alpha was used to study the questionnaire’s reliability, which was confirmed with a value of 0.78. The research team also confirmed its validity with content validity ratio of 0.60. In the last step, based on the experts questionnaire results and identification of each feature that received the desired score, a conceptual model of DSSs in infertility was designed and presented.
2.5. Risk of bias and quality assessment
A systematic assessment of evidence through a critical appraisal is not obligatory in scoping reviews (22). Since assessing the trustworthiness, reliability, and bias of evidence adds value, one of the researchers (HS) evaluated the risk of bias in the included studies using the Joanna Briggs Institute (JBI) critical appraisal guidelines. Because different types of papers were included, we utilized the checklist for qualitative research (23) and the checklist for systematic reviews and research syntheses (24). These quality assessment checklists comprise 11 questions and offer 4 options: “Yes”, “No”, “Unclear”, and “Not Applicable” to evaluate the quality of included studies. Articles were included if they met more than half of the JBI criteria.
2.6. Ethical Considerations
This study was approved by the Ethics Committee of the Tehran University of Medical Sciences, Tehran, Iran (Code: IR.TUMS.SPH.REC.1402.010). Verbal informed consent was obtained from all 32 infertility experts before conducting the study. Since the questionnaires were collected anonymously based on the Porsline platform, the confidentiality of the data was maintained by the research team.
2.7. Statistical Analysis
In this study, the Statistical Package for the Social Sciences software, version 24.0 (SPSS Inc., Chicago, Illinois, USA) was used to analyze numerical data from a researcher-made questionnaire and to verify its reliability with Cronbach’s alpha.
3. Results
3.1. Step 1: scoping literature review
After searching PubMed, Scopus, and Web of Science, we identified 16,310 potentially relevant articles. We removed duplicates (n = 6137) and conducted further searches on Google Scholar, which led to the inclusion of 10 studies specifically related to our aim. We excluded 10,056 articles based on title and abstract due to low relevance, and only screened 127 full-text articles. Following a thorough review of all articles against eligibility criteria, we selected 10 articles for the study. Figure 1 illustrates the PRISMA flowchart indicating results of identification and screening process.
3.1.1. Attributes of the included studies
Table I provides a summary of characteristics of the included studies.
3.2. Step 2: finding similar systems
71 potentially relevant systems were identified from popular search engines like Google, Yahoo, and Bing, as well as AI tools such as ChatGPT, Gemini, and Perplexity. We excluded 58 systems that were implemented and used by users, and finally, 13 systems were included in the study for further investigations.
3.3. Step 3: experts’ opinion
Our researcher-made questionnaire included 49 questions in 5 domains, including main features of the system (11 questions), system data (patient information management/registry data and recommended treatment methods) (19 questions), system data (prediction module – predicting the likelihood of having children for single individuals and the probability of fertility for couples) (11 questions), system data (data for the patient prediction section – predicting fertility probability for couples – additional data related to couples) (5 questions), and secondary features of the system (3 questions). Using this questionnaire, in addition to married people, we can also find out for single people what data elements we should have to predict their fertility/infertility in the future.
32 experts, 13 (41%) male and 19 (59%) female, completed the questionnaire. The participants expertise was as follows: 8 obstetrician/gynecologists, 14 embryologists, 6 urologists, and 4 midwives. About one-third (38%) were 36-45 yr old.
3.4. Identified features and data elements
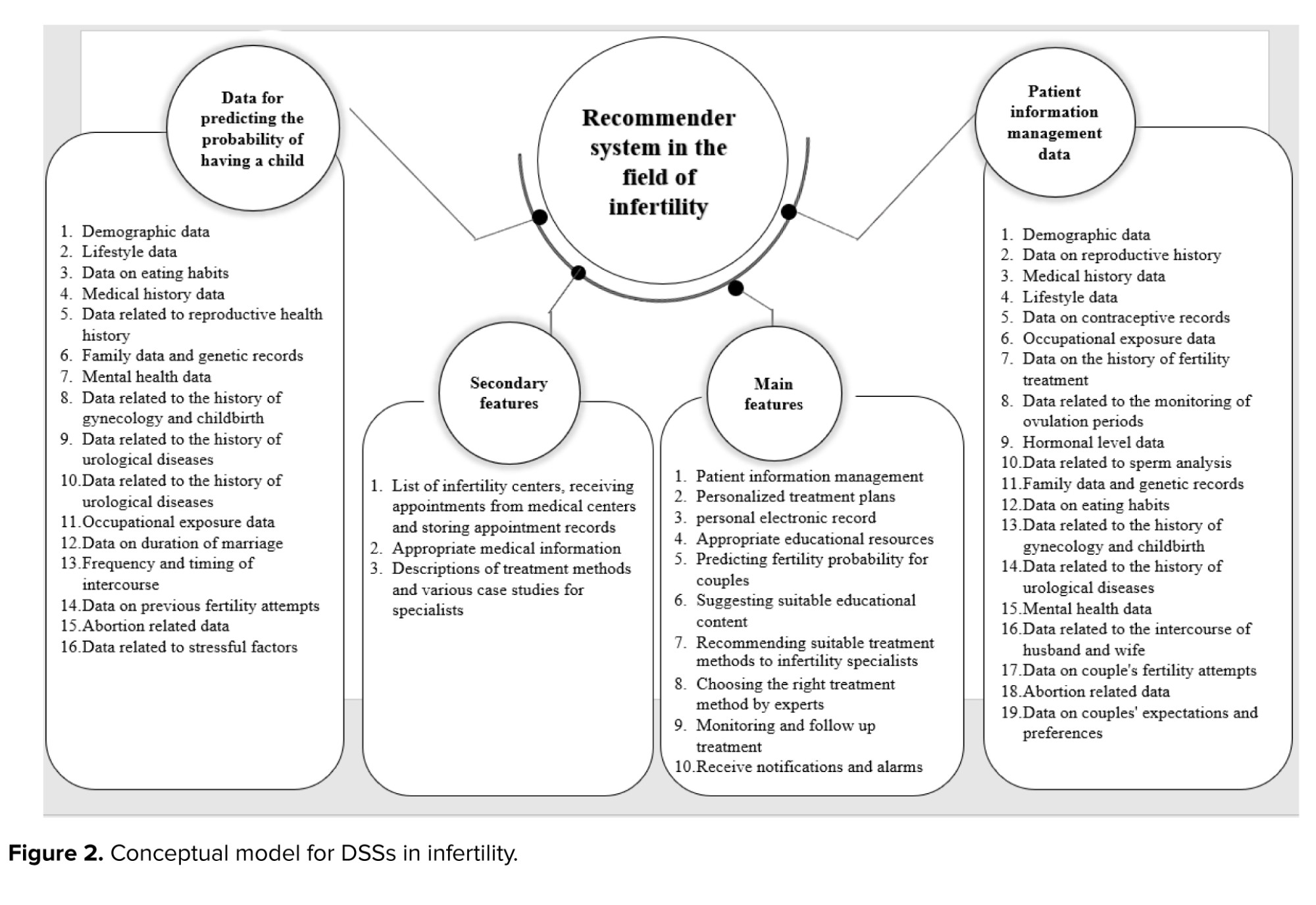
Considering the importance of DSSs in infertility, it seems necessary to identify the features and data required in these systems. Additionally, an infrastructure should be provided to facilitate easier, higher-quality, and faster development of these systems. After implementing the study method, these features were extracted, categorized, and used in designing the conceptual model:
- Main features: a DSS in infertility should have.
- The data required to recommend the treatment method: the data related to the couple must be recorded so that the DSS can help the experts choose the most appropriate treatment method.
- Infertility prediction data: the data must be collected from couples or single people so that the system can predict to what extent a couple or single individual may face the issue of infertility in the future (to perform appropriate treatments at a better time).
- Secondary features: features that are not required and only help to improve and complete the system’s functionality and better use by users.
The results of the implemented method are as follows. The items that received the quorum score (70% agreement) were also considered to present the conceptual model of the infertility DSS. The overall agreement of this model was 85%.
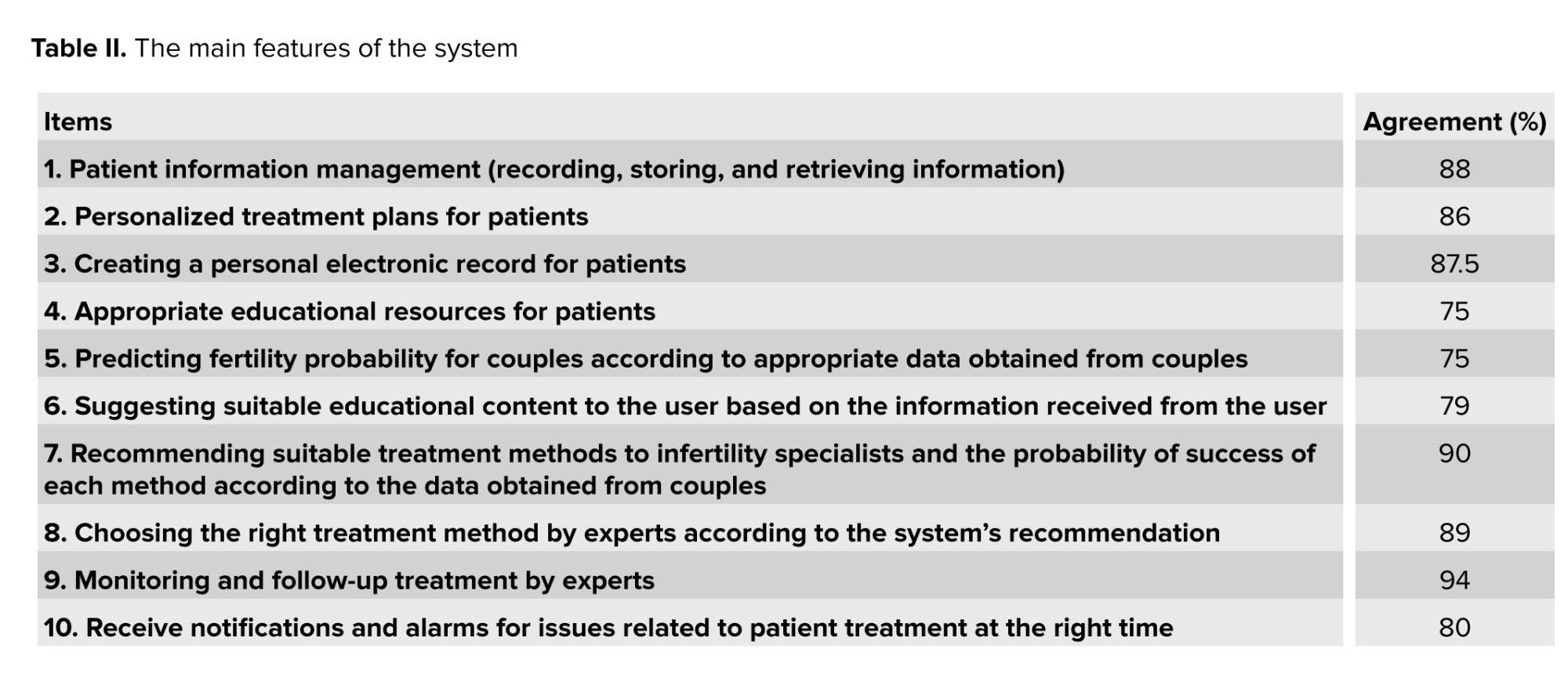
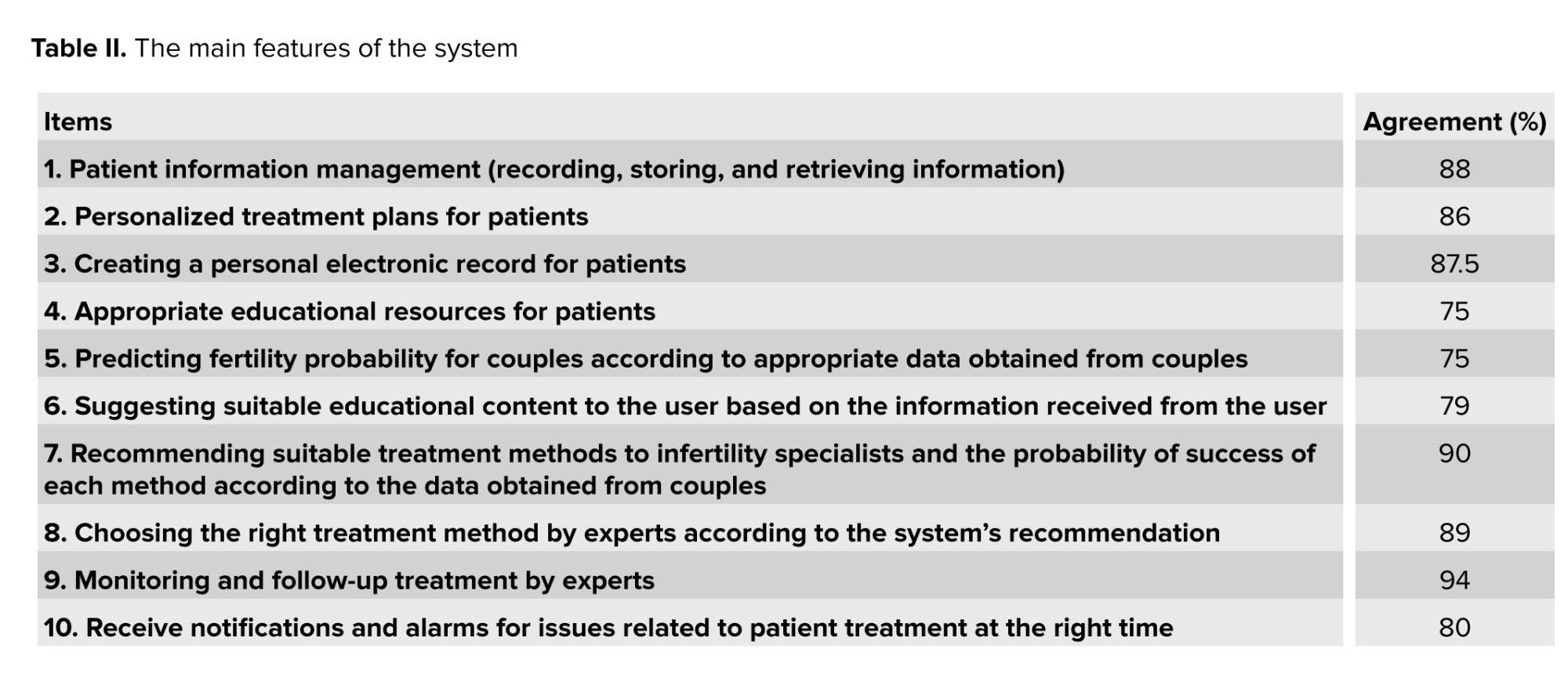
Table II illustrates the main features of the system. Monitoring and follow-up treatment by experts is the most critical factor, with 94% agreement.
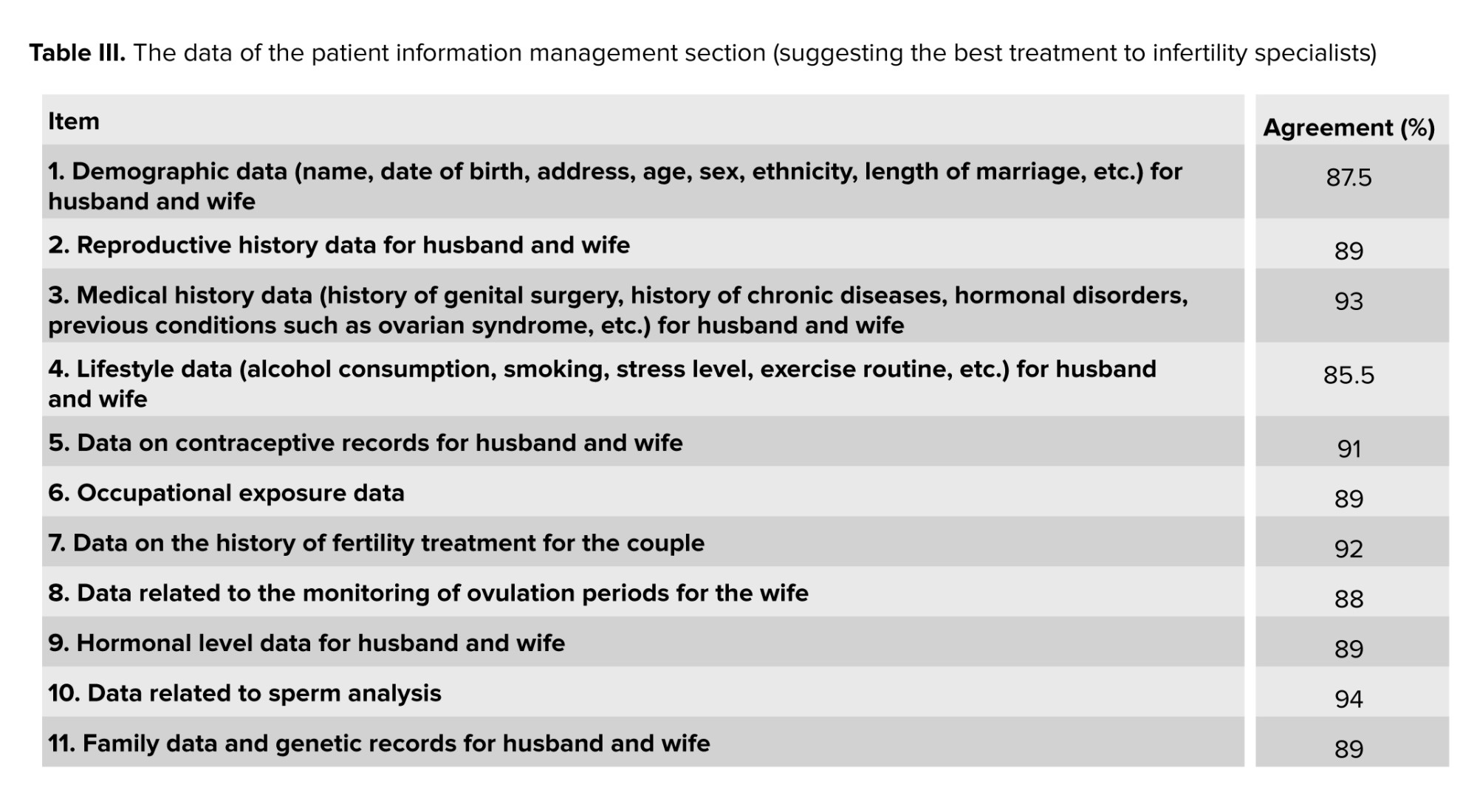
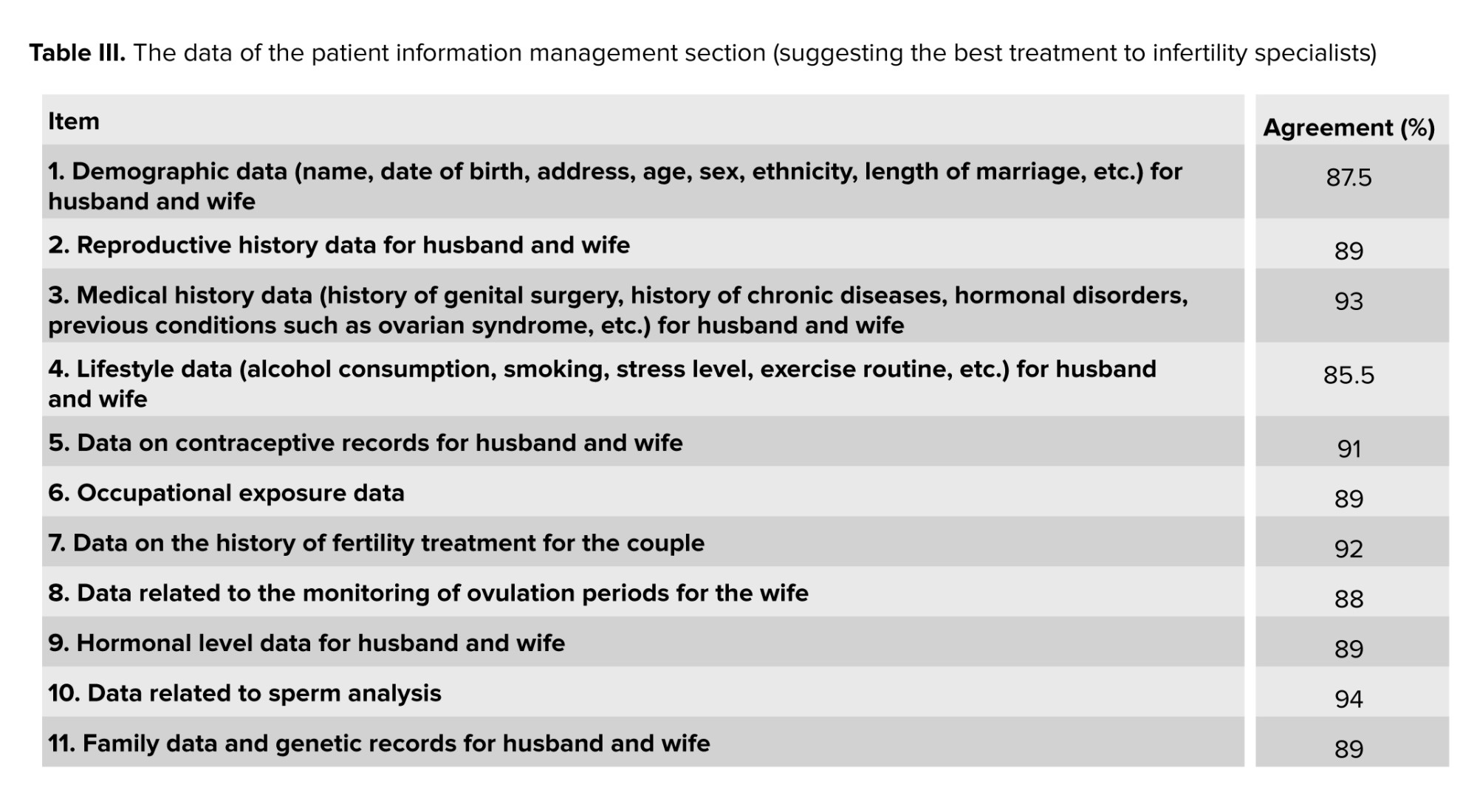
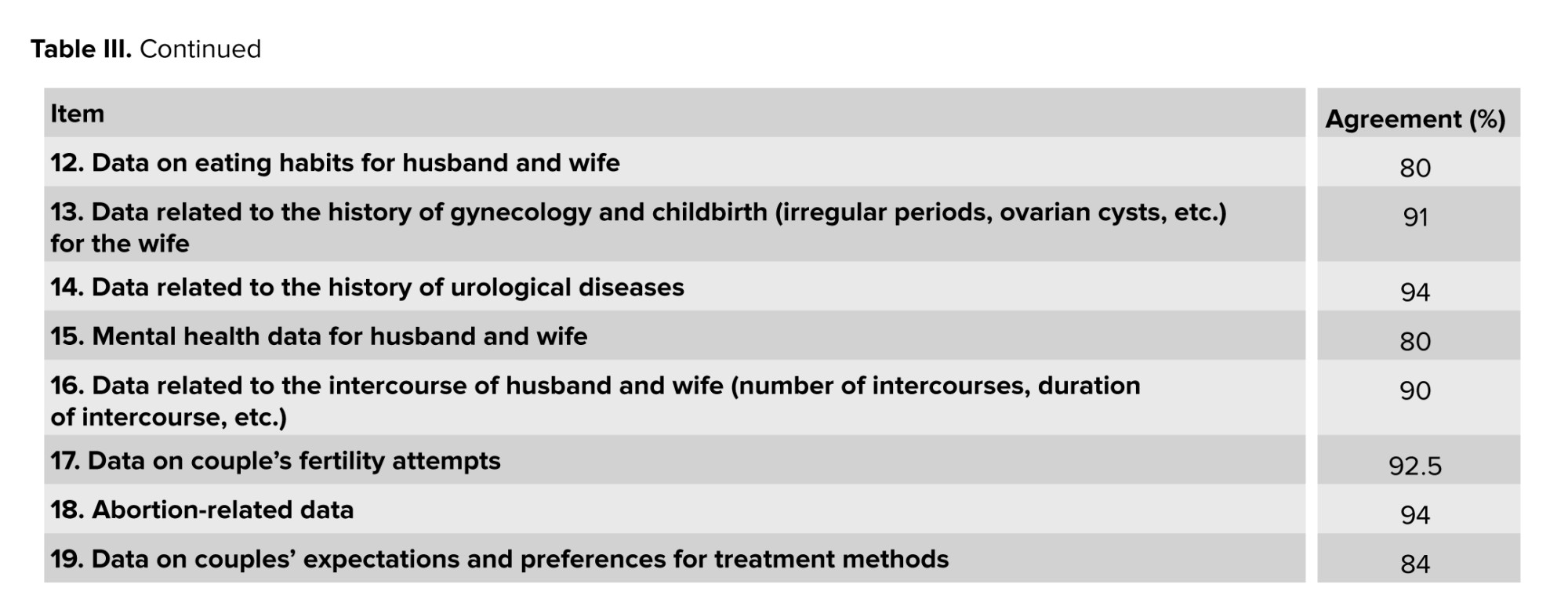
Table III indicates the data from the patient information management section, which suggests the best treatment for an infertility specialist. Data related to sperm analysis, history of urological diseases, and abortion achieved the most agreement between experts (94%).
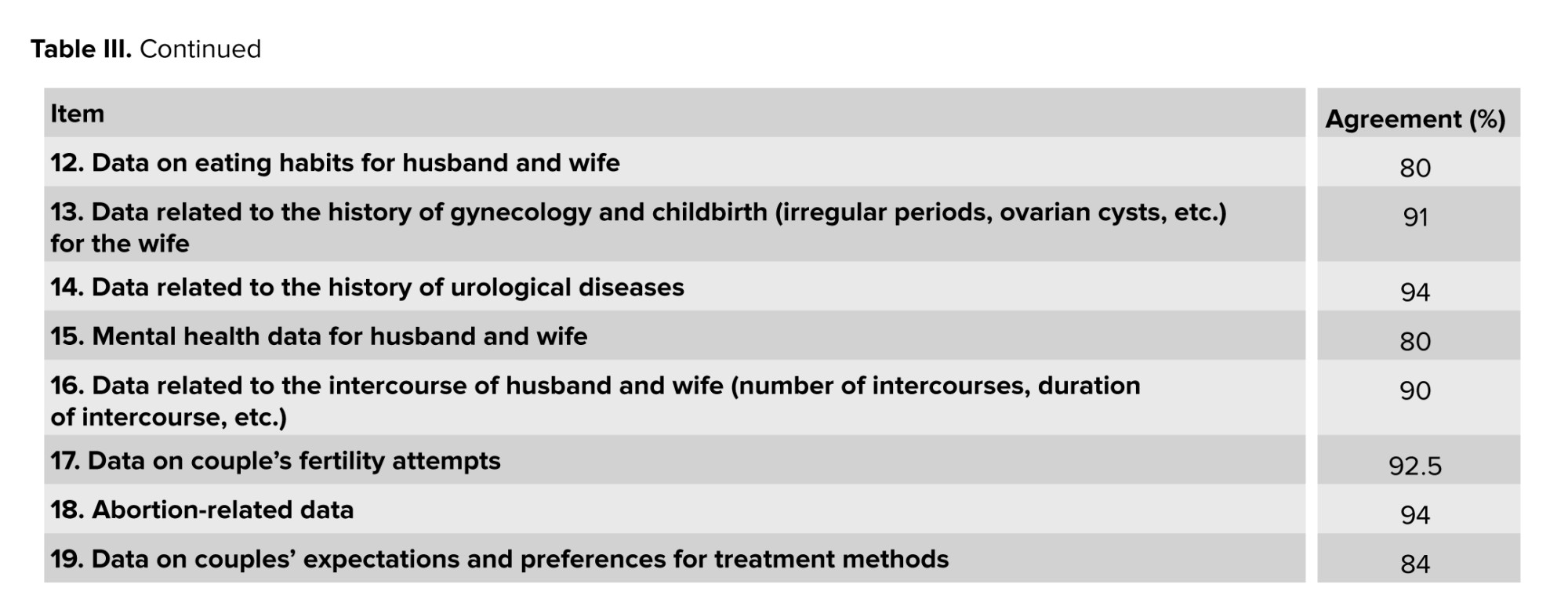
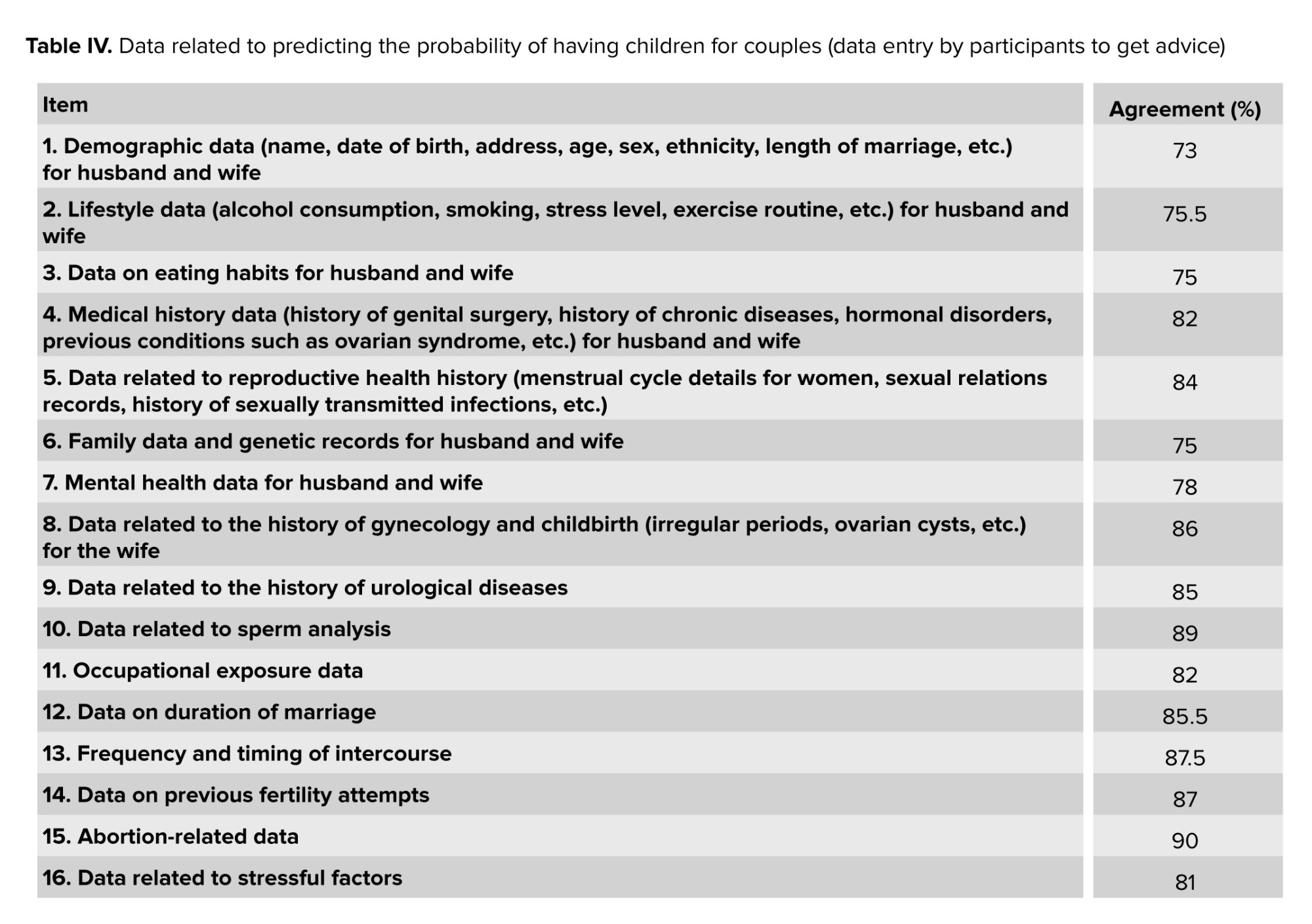
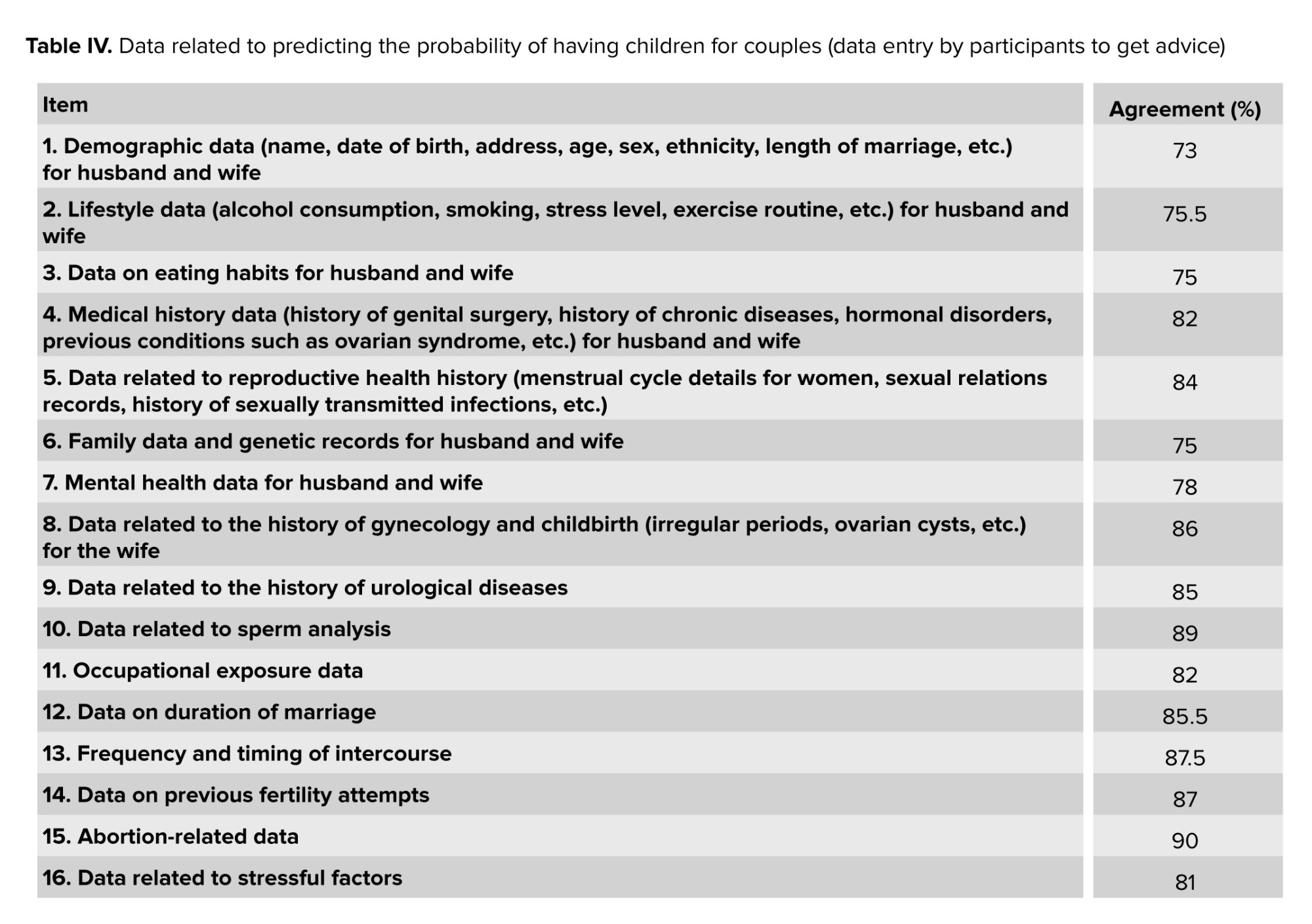
Table IV demonstrates the data related to predicting the probability of having children for couples. The highest level of agreement among experts was on “Abortion-related data”, with 90% agreement, and the lowest level of agreement was on “Demographic data (name, date of birth, address, age, sex, ethnicity, and length of the marriage) for husband and wife”, with 73% agreement.
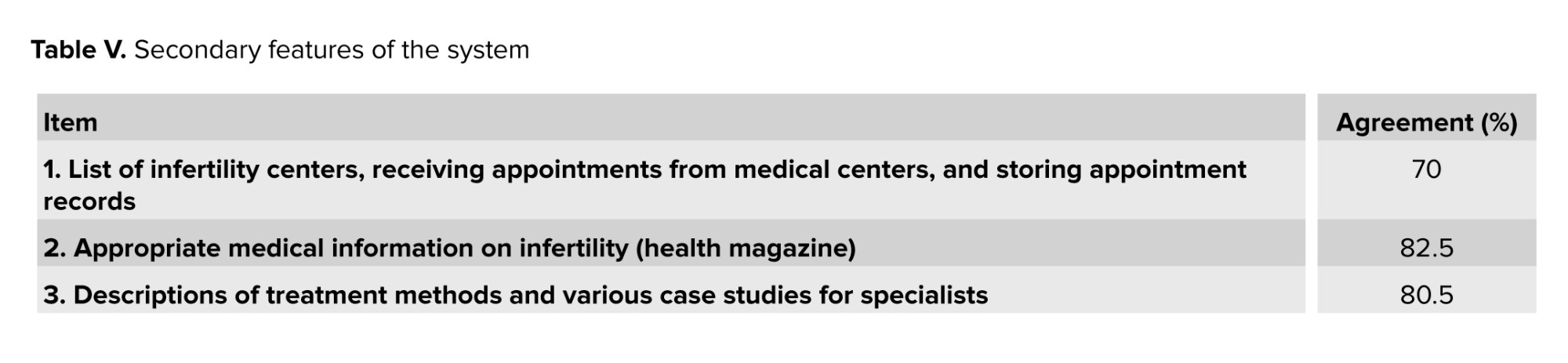
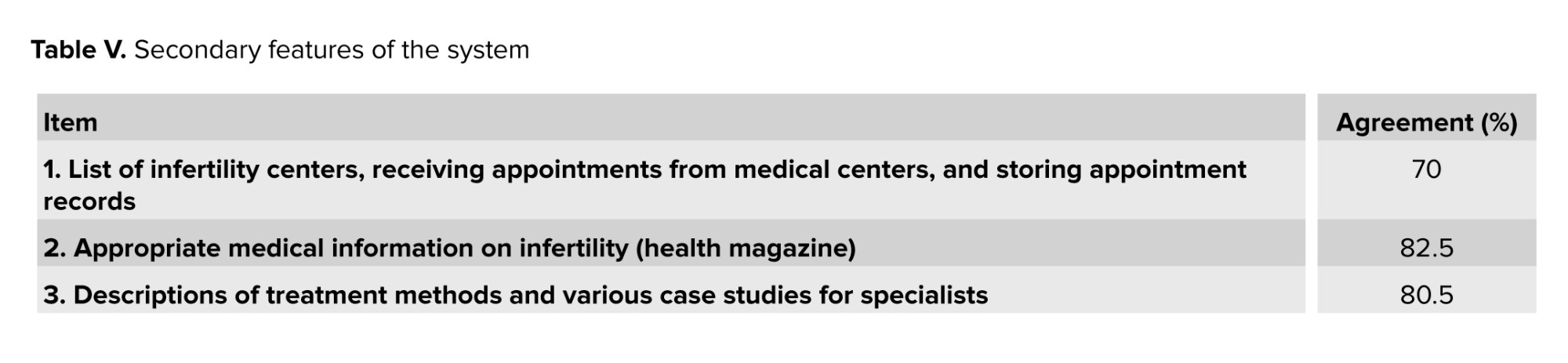
Table V illustrates the system’s secondary features. The highest level of agreement among experts was on “Appropriate medical information in infertility (health magazine)”, with 82.5% agreement, and the lowest level of agreement was on “List of infertility centers, receiving appointments from medical centers and storing appointment records”, with 70% agreement.
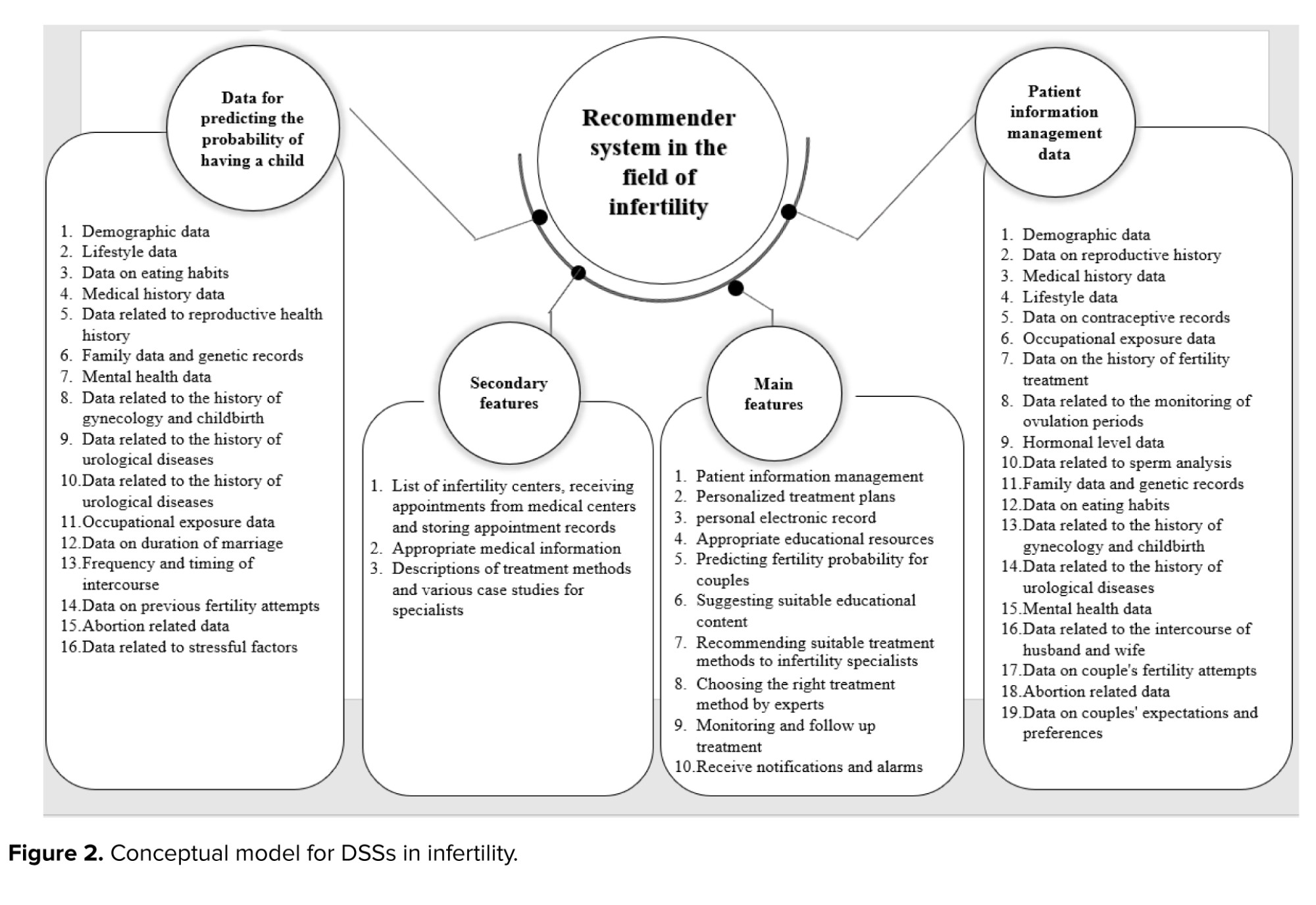
According to the identification of the characteristics and data that got the desired score, the following conceptual model is presented to create a DSS in infertility (Figure 2).
In this study, we developed a DSS for infertility. This DSS includes an AI micro service that recommends the appropriate treatment method based on the input data. Additionally, there are micro services for administrators to add new centers and specialists, as well as for specialists and center representatives to input demographic, laboratory, and medical records.
According to this diagram, in laboratory data of the developed system, some features such as antral follicle count, anti-Mullerian hormone, body mass index (BMI), Estradiol, follicle stimulating hormone, luteinizing hormone, polycystic ovary syndrome, fresh/frozen embryo, fresh/frozen oocyte quality of retrieved oocytes, number of retrieved oocytes, number of transferred embryos, previous pregnancy, previous live birth, previous IVF-intracytoplasmic injection-intrauterine insemination, female age, male age, follicle size, and cause of infertility were considered.
3.5. Risk of bias and quality assessment
The qualitative assessment of the reviewed articles indicated a strong methodology across the included studies. The studies that received “Yes” on at least half of the questions were included. All included studies qualified for further investigation.

4. Discussion
This study aimed to present a conceptual model for DSSs in infertility. The current study found 4 necessary groups of features and data to build a DSS in infertility, including data for predicting the probability of having a child (16 data elements), main features (10 features), secondary features (3 features), and patient information management data (19 data elements). After attracting the opinion of experts, the items that obtained the required quorum score were used in designing the conceptual model. The review of previous relevant studies indicated that the use of AI and ML through DSSs in infertility is increasing. In a study, the growing trend of using AI and ML in women and infertility was pointed out (34).
Our study found that many factors in the modeling related to the recommendation and prediction of infertility treatment, and the axes of these cases were identified in the presented conceptual model. Due to the abundance of factors affecting the timing of infertility treatment, the importance of using AI in this issue increases. These findings are consistent with (35). In our study, the experts assigned a score to each of the characteristics and data specified for the DSS in infertility. In other studies, data mining and statistical studies determined the most important factors affecting fertility. In a study, age, thyroid-stimulating hormones, BMI, and others were found to be essential factors in fertility, and these factors are consistent with the items specified in the presented conceptual model (36). In the study of (37), an investigation was conducted to determine the minimum data set needed for designing an infertility monitoring system. They organized their identified elements into managerial and clinical categories, each containing 4 sections comprising 60 and 940 data elements, respectively. Demographic data, medical history, treatment results, family history, and medication history were among the most critical data elements. These findings were consistent with ours.
Similar to our study, a systematic review investigated the application of AI, clinical decision support algorithms, mathematical models, and calculators in infertility. Key components identified in the development of clinical decision support algorithms in infertility included BMI, lifestyle factors, the number of previous treatments, a presumptive diagnosis of infertility, and an assessment of IVF cycle outcomes (38).
Another cross-sectional study used data mining techniques to predict the implantation outcome of IVF and intracytoplasmic sperm injection. They used an IVF/intracytoplasmic injection dataset with 29 variables and a unique identifier for each individual, indicating either a negative or positive outcome (39). Among the factors highlighted in this research, the age of both the man and woman, BMI, sperm count, sperm motility, the type of treatment, and the number of oocytes of MI quality are consistent with our results.
The potential for developing a DSS to aid in infertility decision-making was explored, finding that certain factors, such as endometriosis, psychosomatic, and cervical issues, are statistically linked to the final diagnosis (40). Similar to this study, we considered these items in data for predicting the probability of having a child section.
This study presented a conceptual model to create DSSs in infertility so that future developments can be done with less cost and more accuracy. Using conceptual models to provide solutions and a central structure in DSSs is one of the well-known approaches in this field. A model was provided for implementing these systems in the nursing field by presenting a conceptual framework for implementing DSSs in the nursing field (41). In another study, a critical theoretical framework was demonstrated for adopting and applying DSSs in clinical settings (42). In the study, a conceptual model was presented for setting up and implementing DSSs called BEAR (behavior and acceptance framework) (7). It can be used to facilitate the implementation of these systems, and for those who intend to use them. The study introduced a conceptual model of fertility concerns among adolescents and young adults with cancer (43). The model has 4 domains: affective, information, coping, and logistical. The information domain covers information needs, access, delivery, or comprehension themes. The affective domain deals with fertility-related emotional experiences. The coping domain involves attempts to cope with fertility concerns. The logistical domain focuses on timing, organization, planning, and access. Since this study focused on fertility concerns in cancer patients and the authors did not develop a DSS system, these findings do not align with ours. In another study, a conceptual model of psychosocial burden in infertile couples undergoing assisted reproductive treatments was designed (44). This study was conducted in 4 stages using a mixed-methods and sequential exploratory approach, and as a result, a conceptual model of psychosocial burden was designed. The authors did not develop a DSS system; these findings also do not align with ours.
4.1. Strengths and limitations
The strengths of this study include the development of a general model for creating a DSS for infertility. Additionally, the study not only reviewed available evidence from scientific databases but also surveyed relevant experts. The selection of experts was diverse, incorporating specialists from all pertinent fields. Furthermore, this review has several limitations that can be considered in future studies. First, despite our efforts to perform a comprehensive search across multiple online databases and search engines, we may have missed non-English studies about DSSs in infertility. Also, there were limitations in access to some existing systems in infertility, which prevented a full review of these systems. This study presented essential data that are effective for decision-making when selecting infertility treatment methods as a conceptual model. Due to the possibility of other influential factors, future studies can try to complete these data.
5. Conclusion
In this study, a conceptual model for DSSs in infertility was presented, and the requirements of these systems were determined in terms of characteristics and data classification based on experts opinions. The requirements mentioned in this conceptual model are categorized into 4 domains: main features, patient information management, fertility prediction data, and secondary features. This conceptual model can reduce the costs to analyze, review, and create these systems. Therefore, the main focus in developing these systems can be the best possible implementation of ML algorithms and AI. Future studies should focus on prospective testing, including a diverse range of patients, and using advanced ML to develop robust and globally applicable DSSs, ultimately leading to improved reproductive healthcare outcomes.
Data Availability
All data generated or analyzed during this study are included in this published article.
Author Contributions
H. Sajjadi, H. Choobineh, and R. Safdari: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or reviewing it critically for important intellectual content. Final approval of the version to be published, agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
The authors would like to express their gratitude to all colleagues who assisted in conducting this research. No funding sources were used in this study. This article is supported by the Iranian Society of Embryology and Reproductive Biology and Red Crescent Infertility Treatment Center, Tehran, Iran. In the grammar-checking process, the authors utilized the Grammarly web application, version 2025.
Conflict of Interest
The authors declare that there is no conflict of interest.
Table II illustrates the main features of the system. Monitoring and follow-up treatment by experts is the most critical factor, with 94% agreement.
Table III indicates the data from the patient information management section, which suggests the best treatment for an infertility specialist. Data related to sperm analysis, history of urological diseases, and abortion achieved the most agreement between experts (94%).
Table IV demonstrates the data related to predicting the probability of having children for couples. The highest level of agreement among experts was on “Abortion-related data”, with 90% agreement, and the lowest level of agreement was on “Demographic data (name, date of birth, address, age, sex, ethnicity, and length of the marriage) for husband and wife”, with 73% agreement.
Table V illustrates the system’s secondary features. The highest level of agreement among experts was on “Appropriate medical information in infertility (health magazine)”, with 82.5% agreement, and the lowest level of agreement was on “List of infertility centers, receiving appointments from medical centers and storing appointment records”, with 70% agreement.
According to the identification of the characteristics and data that got the desired score, the following conceptual model is presented to create a DSS in infertility (Figure 2).
In this study, we developed a DSS for infertility. This DSS includes an AI micro service that recommends the appropriate treatment method based on the input data. Additionally, there are micro services for administrators to add new centers and specialists, as well as for specialists and center representatives to input demographic, laboratory, and medical records.
According to this diagram, in laboratory data of the developed system, some features such as antral follicle count, anti-Mullerian hormone, body mass index (BMI), Estradiol, follicle stimulating hormone, luteinizing hormone, polycystic ovary syndrome, fresh/frozen embryo, fresh/frozen oocyte quality of retrieved oocytes, number of retrieved oocytes, number of transferred embryos, previous pregnancy, previous live birth, previous IVF-intracytoplasmic injection-intrauterine insemination, female age, male age, follicle size, and cause of infertility were considered.
3.5. Risk of bias and quality assessment
The qualitative assessment of the reviewed articles indicated a strong methodology across the included studies. The studies that received “Yes” on at least half of the questions were included. All included studies qualified for further investigation.

4. Discussion
This study aimed to present a conceptual model for DSSs in infertility. The current study found 4 necessary groups of features and data to build a DSS in infertility, including data for predicting the probability of having a child (16 data elements), main features (10 features), secondary features (3 features), and patient information management data (19 data elements). After attracting the opinion of experts, the items that obtained the required quorum score were used in designing the conceptual model. The review of previous relevant studies indicated that the use of AI and ML through DSSs in infertility is increasing. In a study, the growing trend of using AI and ML in women and infertility was pointed out (34).
Our study found that many factors in the modeling related to the recommendation and prediction of infertility treatment, and the axes of these cases were identified in the presented conceptual model. Due to the abundance of factors affecting the timing of infertility treatment, the importance of using AI in this issue increases. These findings are consistent with (35). In our study, the experts assigned a score to each of the characteristics and data specified for the DSS in infertility. In other studies, data mining and statistical studies determined the most important factors affecting fertility. In a study, age, thyroid-stimulating hormones, BMI, and others were found to be essential factors in fertility, and these factors are consistent with the items specified in the presented conceptual model (36). In the study of (37), an investigation was conducted to determine the minimum data set needed for designing an infertility monitoring system. They organized their identified elements into managerial and clinical categories, each containing 4 sections comprising 60 and 940 data elements, respectively. Demographic data, medical history, treatment results, family history, and medication history were among the most critical data elements. These findings were consistent with ours.
Similar to our study, a systematic review investigated the application of AI, clinical decision support algorithms, mathematical models, and calculators in infertility. Key components identified in the development of clinical decision support algorithms in infertility included BMI, lifestyle factors, the number of previous treatments, a presumptive diagnosis of infertility, and an assessment of IVF cycle outcomes (38).
Another cross-sectional study used data mining techniques to predict the implantation outcome of IVF and intracytoplasmic sperm injection. They used an IVF/intracytoplasmic injection dataset with 29 variables and a unique identifier for each individual, indicating either a negative or positive outcome (39). Among the factors highlighted in this research, the age of both the man and woman, BMI, sperm count, sperm motility, the type of treatment, and the number of oocytes of MI quality are consistent with our results.
The potential for developing a DSS to aid in infertility decision-making was explored, finding that certain factors, such as endometriosis, psychosomatic, and cervical issues, are statistically linked to the final diagnosis (40). Similar to this study, we considered these items in data for predicting the probability of having a child section.
This study presented a conceptual model to create DSSs in infertility so that future developments can be done with less cost and more accuracy. Using conceptual models to provide solutions and a central structure in DSSs is one of the well-known approaches in this field. A model was provided for implementing these systems in the nursing field by presenting a conceptual framework for implementing DSSs in the nursing field (41). In another study, a critical theoretical framework was demonstrated for adopting and applying DSSs in clinical settings (42). In the study, a conceptual model was presented for setting up and implementing DSSs called BEAR (behavior and acceptance framework) (7). It can be used to facilitate the implementation of these systems, and for those who intend to use them. The study introduced a conceptual model of fertility concerns among adolescents and young adults with cancer (43). The model has 4 domains: affective, information, coping, and logistical. The information domain covers information needs, access, delivery, or comprehension themes. The affective domain deals with fertility-related emotional experiences. The coping domain involves attempts to cope with fertility concerns. The logistical domain focuses on timing, organization, planning, and access. Since this study focused on fertility concerns in cancer patients and the authors did not develop a DSS system, these findings do not align with ours. In another study, a conceptual model of psychosocial burden in infertile couples undergoing assisted reproductive treatments was designed (44). This study was conducted in 4 stages using a mixed-methods and sequential exploratory approach, and as a result, a conceptual model of psychosocial burden was designed. The authors did not develop a DSS system; these findings also do not align with ours.
4.1. Strengths and limitations
The strengths of this study include the development of a general model for creating a DSS for infertility. Additionally, the study not only reviewed available evidence from scientific databases but also surveyed relevant experts. The selection of experts was diverse, incorporating specialists from all pertinent fields. Furthermore, this review has several limitations that can be considered in future studies. First, despite our efforts to perform a comprehensive search across multiple online databases and search engines, we may have missed non-English studies about DSSs in infertility. Also, there were limitations in access to some existing systems in infertility, which prevented a full review of these systems. This study presented essential data that are effective for decision-making when selecting infertility treatment methods as a conceptual model. Due to the possibility of other influential factors, future studies can try to complete these data.
5. Conclusion
In this study, a conceptual model for DSSs in infertility was presented, and the requirements of these systems were determined in terms of characteristics and data classification based on experts opinions. The requirements mentioned in this conceptual model are categorized into 4 domains: main features, patient information management, fertility prediction data, and secondary features. This conceptual model can reduce the costs to analyze, review, and create these systems. Therefore, the main focus in developing these systems can be the best possible implementation of ML algorithms and AI. Future studies should focus on prospective testing, including a diverse range of patients, and using advanced ML to develop robust and globally applicable DSSs, ultimately leading to improved reproductive healthcare outcomes.
Data Availability
All data generated or analyzed during this study are included in this published article.
Author Contributions
H. Sajjadi, H. Choobineh, and R. Safdari: Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or reviewing it critically for important intellectual content. Final approval of the version to be published, agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Acknowledgments
The authors would like to express their gratitude to all colleagues who assisted in conducting this research. No funding sources were used in this study. This article is supported by the Iranian Society of Embryology and Reproductive Biology and Red Crescent Infertility Treatment Center, Tehran, Iran. In the grammar-checking process, the authors utilized the Grammarly web application, version 2025.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Fertility & Infertility
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |