Sat, Jan 31, 2026
[Archive]
Volume 23, Issue 8 (August 2025)
IJRM 2025, 23(8): 659-664 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Vosough Taghi Dizaj A, Sadighi Gilani M A, Pahlavan F, Saadat Varnosfaderani A. A rare case of crossed-ectopic testis, a primary infertile affected: A case report. IJRM 2025; 23 (8) :659-664
URL: http://ijrm.ir/article-1-3586-en.html
URL: http://ijrm.ir/article-1-3586-en.html
Ahmad Vosough Taghi Dizaj *1 

 , Mohammad Ali Sadighi Gilani2
, Mohammad Ali Sadighi Gilani2 

 , Fattaneh Pahlavan3
, Fattaneh Pahlavan3 

 , Ameneh Saadat Varnosfaderani3
, Ameneh Saadat Varnosfaderani3 




 , Mohammad Ali Sadighi Gilani2
, Mohammad Ali Sadighi Gilani2 

 , Fattaneh Pahlavan3
, Fattaneh Pahlavan3 

 , Ameneh Saadat Varnosfaderani3
, Ameneh Saadat Varnosfaderani3 


1- Department of Reproductive Imaging, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran. , vosough@royaninstitute.org
2- Department of Andrology, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
3- Department of Reproductive Imaging, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
2- Department of Andrology, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
3- Department of Reproductive Imaging, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
Full-Text [PDF 2909 kb]
(467 Downloads)
| Abstract (HTML) (458 Views)
Full-Text: (64 Views)
1. Introduction
Crossed ectopic testis is one of the rare congenital anomalies of testicular migration where both testes descend to the single inguinal canal and is observed in < 0.67% of men (1, 2). Being a multifactorial anomaly, crossed ectopic testis is often found with other congenital anomalies, including inguinal hernia, persistent Mullerian structure anomalies, hypospadias, bifid scrotum, pseudohermaphroditism, renal anomalies, and seminal vesicle cysts (3). While this disease's symptoms vary substantially, ranging from inguinal hernia to infertility. It could be a completely asymptomatic and incidental finding (4, 5). Imaging techniques, along with medical history, physical examination, and laboratory tests, are utilized to diagnose this anomaly (6).
In this study, we indicate imaging tests as a more useful method for diagnosing crossed-ectopic testis. Therefore, we have reported a rare case of an infertile man with crossed ectopic testis.
2. Case Presentation
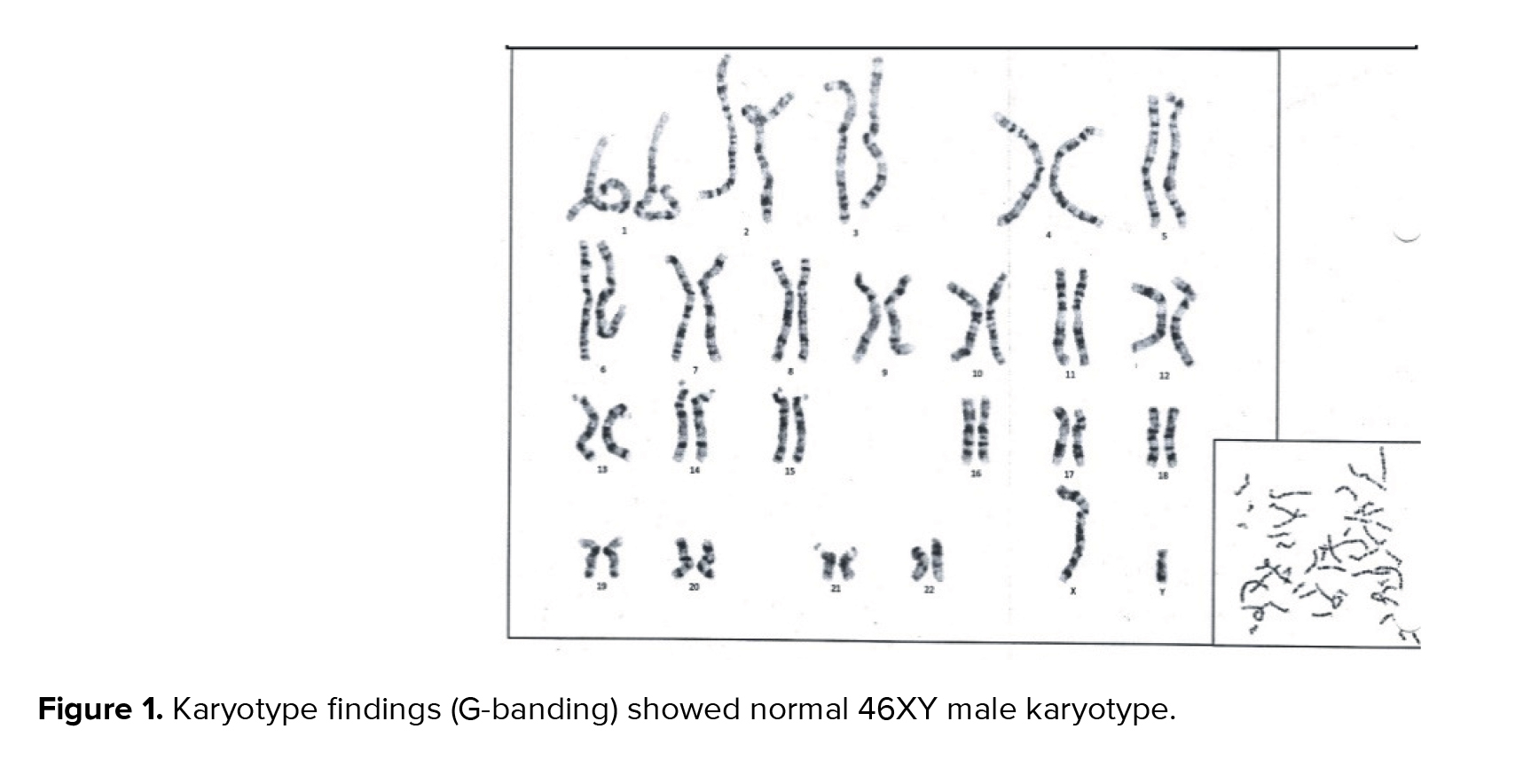
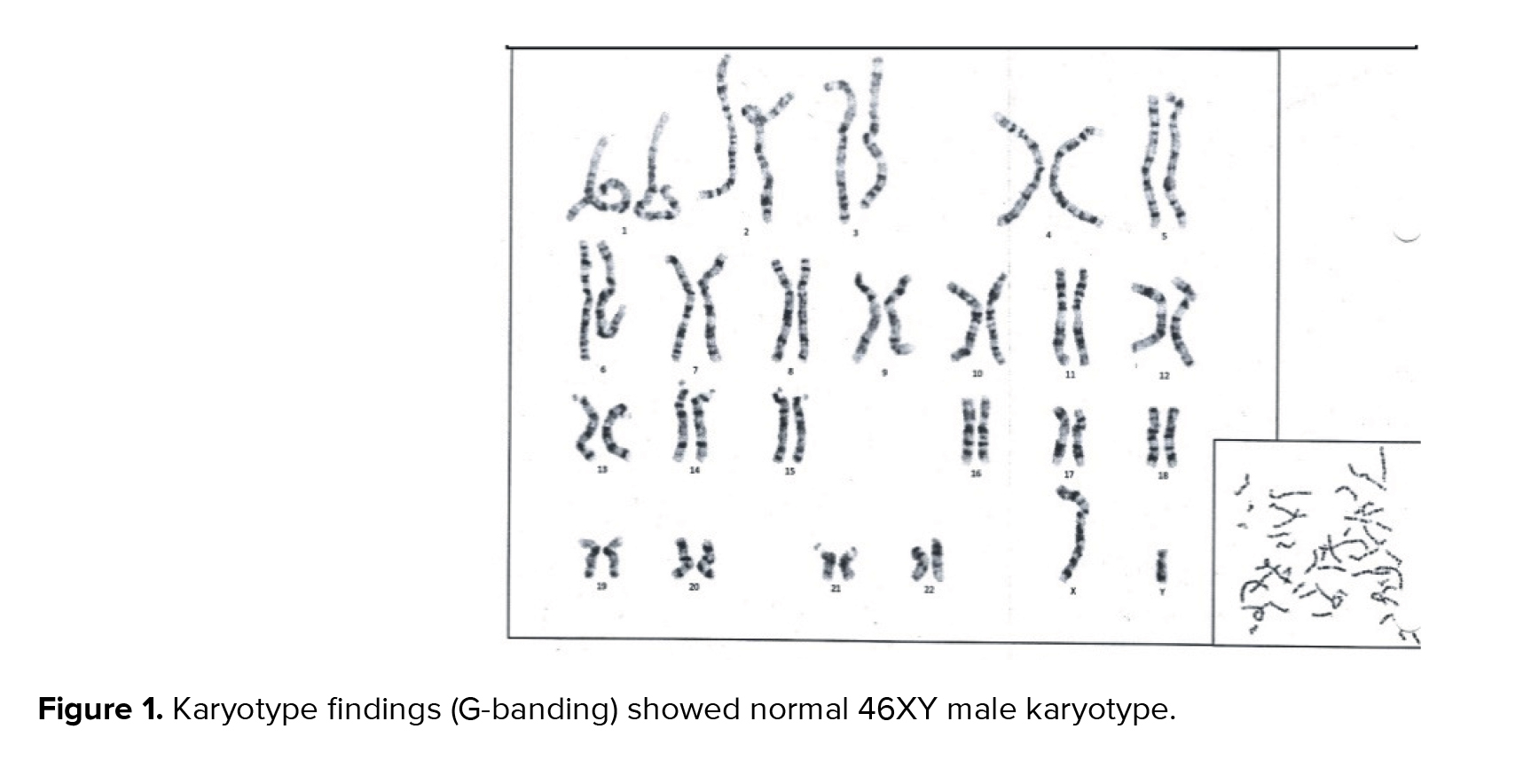
A 36-yr-old man who dealt with infertility after 8 yr of marriage, referred to our infertility clinic at the Royan Institute, Tehran, Iran included in this study. He had a history of inguinal hernia surgery. A physical examination was done by an expert urologist, which revealed a non-palpable right testis. The left testis was normal in size. The right vas deferens and right spermatic cord were nonpalpable. The left cord was thick, and a mass-like structure was palpable in the left inguinal canal. The hormonal study showed normal levels of luteinizing hormone, follicle-stimulating hormone, and luteinizing hormone/follicle-stimulating hormone ratio. Testosterone was lower than the normal range (Table I). Azoospermia was confirmed in semen analysis. Also, the seminal fructose level elevation was lower than the normal range (Table II). Cytogenetic analysis showed a normal karyotype (46, XY), compatible with normal male (Figure 1). An ultrasound examination was performed. The right testis was not seen in the right scrotum. The right ectopic testis was seen in the superior part of the left scrotum, and the inferior part of the left inguinal canal had a significantly small size (40*25*14 mm) with a normal shape and non-hemogenic parenchymal echogenicity. Echo-free tubular structures were seen in the right testicular parenchyma and suggested seminiferous tubule ectasia. Multiple spermatoceles were seen in the head of the epididymis. The biggest one was 10*11 mm.
The left testis was normal in size, shape, and location. Echo-free tubular structures were seen in the left testicular parenchyma and suggested seminiferous tubule ectasia. Multiple spermatoceles were seen in the head of the epididymis. The biggest one was 10*13 mm. On the left side, the pampiniform vein plexus was normal. The left spermatic cord was thicker than the normal range. The ultrasonographic findings comprise crossed ectopic right testis, bilateral seminiferous tubule ectasia, bilateral multiple spermatoceles, and a thick cord on the left side (Figure 2).
A magnetic resonance imaging (MRI) study was performed to confirm the diagnosis. It revealed an empty right scrotum. The right spermatic cord was not seen in the right inguinal region. 2 normal testis tissues were seen on the left hemiscrotum. 2 thick spermatic cords in the left inguinal canal were attached to the enlarged left side seminal vesicle. An asymmetric seminal vesicle (hypoplastic vesicle on the right side) was reported (Figure 3). These findings confirmed the transverse ectopic testis (Figure 4A, B).
Testicular sperm extraction (TESE) was performed. In the operating room and under sterile conditions, the scrotum is incised superficially after the prep and drep. Tunica vaginalis and albuginea opened (Figure 5). A piece of testicular tissue was excised and sent to the embryology and pathology departments, Royan Institute, Tehran, Iran. The sperm concentration was 0-1 ml in a high-power field, and normal morphology was 0-1% (Figure 6). Assisted reproduction treatment was considered.
2.1. Ethical Considerations
Informed written consent was obtained from the case to use his medical records for any research purpose.







3. Discussion
In this study, we reported a rare case of an infertile man who was diagnosed with crossed ectopic testis by ultrasound. Crossed ectopic testis, also called testicular pseudo-duplication, unilateral double testis, and transverse aberrant testicular mal-descent, is a congenital anomaly. The ectopic testis might be located in the abdomen, inguinal canal, or hemiscrotum (1, 2). Also, the inguinal hernia is the most common coexisting anomaly and is observed in 40-50% of crossed ectopic testis (5).
Although there is no definite etiology for crossed ectopic testis, it was proposed that different factors, such as testicular adherence to Mullerian structures, a fusion of the Wolffian ducts, or defective gubernacular development, may be involved. Conversely, a positive family history also plays an important role in this anomaly (7). The clinical sign is the absence of testis along with an ipsilateral inguinal hernia. This anomaly should be followed since it might lead to infertility. It may contribute to the increasing risk of testicular cancer in these cases (4).
The diagnosis of crossed ectopic testis could be incidental or during the treatment of infertility. Crossed ectopic testis may be diagnosed before the age of 4 yr (4). Imaging methods, including ultrasound examination, computed tomography scan, and MRI are utilized to find this anomaly (8). However, MRI is more specific in finding this anomaly.
The options for treatment vary regarding the symptoms and other associated anomalies. Along with the treatment of infertility, the correction and relocation of ectopic testis should be considered. Sometimes, the cord is very short, and the position of the ectopic testis is very high, so the orchidopexy would be the best choice. If the testis has been atrophying, orchidectomy is considered to prevent malignancy (1, 9).
In our case, ultrasound examination and MRI were able to detect crossed ectopic testis that were consistent with Nunna et al. studies. They recommended undertaking MRI and/or ultrasonography before surgery (10). In our study, both testes were completely descended into the left hemiscrotum. Crossed ectopic testis and its complications had affected testosterone and semen fructose. He did not mention this kind of anomaly in his family. No genetic disease was observed; hence, gonadotropins were in the normal range. Our case dealt with infertility and underwent TESE surgery since he suffered from azoospermia. The case was recommended to return for infertility treatment with assisted reproduction treatment techniques.
4. Conclusion
The crossed ectopic testis is a rare anomaly. However, early diagnosis is important due to the coexisting complications, including infertility and testicular cancer. Imaging methods such as ultrasound examination, MRI, and CT scan could be used to diagnose this anomaly in suspected cases. Treatment would be surgical correction of coexisting anomalies and relocation of crossed ectopic testis. TESE procedure is utilized for the treatment of infertility.
Data Availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author Contributions
Contribution A. Vosough Taghi Dizaj: Designed, supervised the research, and revised the manuscript. M.A. Sadighi Gilani: Urologist, and the administrative supporter for collecting sample, F. Pahlavan: Drafting the manuscript, data collection, data analysis, and interpretation. A. Saadat Varnosfaderani: Data collection and revised the manuscript. All authors studied and approved the final manuscript.
Acknowledgments
The authors would like to thank the patient who participated in this study, also the Royan Institute, Tehran, Iran for their cooperation. No Artificial intelligence was used in this study.
Conflict of Interest
The authors declare that there is no conflict of interest.
Crossed ectopic testis is one of the rare congenital anomalies of testicular migration where both testes descend to the single inguinal canal and is observed in < 0.67% of men (1, 2). Being a multifactorial anomaly, crossed ectopic testis is often found with other congenital anomalies, including inguinal hernia, persistent Mullerian structure anomalies, hypospadias, bifid scrotum, pseudohermaphroditism, renal anomalies, and seminal vesicle cysts (3). While this disease's symptoms vary substantially, ranging from inguinal hernia to infertility. It could be a completely asymptomatic and incidental finding (4, 5). Imaging techniques, along with medical history, physical examination, and laboratory tests, are utilized to diagnose this anomaly (6).
In this study, we indicate imaging tests as a more useful method for diagnosing crossed-ectopic testis. Therefore, we have reported a rare case of an infertile man with crossed ectopic testis.
2. Case Presentation
A 36-yr-old man who dealt with infertility after 8 yr of marriage, referred to our infertility clinic at the Royan Institute, Tehran, Iran included in this study. He had a history of inguinal hernia surgery. A physical examination was done by an expert urologist, which revealed a non-palpable right testis. The left testis was normal in size. The right vas deferens and right spermatic cord were nonpalpable. The left cord was thick, and a mass-like structure was palpable in the left inguinal canal. The hormonal study showed normal levels of luteinizing hormone, follicle-stimulating hormone, and luteinizing hormone/follicle-stimulating hormone ratio. Testosterone was lower than the normal range (Table I). Azoospermia was confirmed in semen analysis. Also, the seminal fructose level elevation was lower than the normal range (Table II). Cytogenetic analysis showed a normal karyotype (46, XY), compatible with normal male (Figure 1). An ultrasound examination was performed. The right testis was not seen in the right scrotum. The right ectopic testis was seen in the superior part of the left scrotum, and the inferior part of the left inguinal canal had a significantly small size (40*25*14 mm) with a normal shape and non-hemogenic parenchymal echogenicity. Echo-free tubular structures were seen in the right testicular parenchyma and suggested seminiferous tubule ectasia. Multiple spermatoceles were seen in the head of the epididymis. The biggest one was 10*11 mm.
The left testis was normal in size, shape, and location. Echo-free tubular structures were seen in the left testicular parenchyma and suggested seminiferous tubule ectasia. Multiple spermatoceles were seen in the head of the epididymis. The biggest one was 10*13 mm. On the left side, the pampiniform vein plexus was normal. The left spermatic cord was thicker than the normal range. The ultrasonographic findings comprise crossed ectopic right testis, bilateral seminiferous tubule ectasia, bilateral multiple spermatoceles, and a thick cord on the left side (Figure 2).
A magnetic resonance imaging (MRI) study was performed to confirm the diagnosis. It revealed an empty right scrotum. The right spermatic cord was not seen in the right inguinal region. 2 normal testis tissues were seen on the left hemiscrotum. 2 thick spermatic cords in the left inguinal canal were attached to the enlarged left side seminal vesicle. An asymmetric seminal vesicle (hypoplastic vesicle on the right side) was reported (Figure 3). These findings confirmed the transverse ectopic testis (Figure 4A, B).
Testicular sperm extraction (TESE) was performed. In the operating room and under sterile conditions, the scrotum is incised superficially after the prep and drep. Tunica vaginalis and albuginea opened (Figure 5). A piece of testicular tissue was excised and sent to the embryology and pathology departments, Royan Institute, Tehran, Iran. The sperm concentration was 0-1 ml in a high-power field, and normal morphology was 0-1% (Figure 6). Assisted reproduction treatment was considered.
2.1. Ethical Considerations
Informed written consent was obtained from the case to use his medical records for any research purpose.







3. Discussion
In this study, we reported a rare case of an infertile man who was diagnosed with crossed ectopic testis by ultrasound. Crossed ectopic testis, also called testicular pseudo-duplication, unilateral double testis, and transverse aberrant testicular mal-descent, is a congenital anomaly. The ectopic testis might be located in the abdomen, inguinal canal, or hemiscrotum (1, 2). Also, the inguinal hernia is the most common coexisting anomaly and is observed in 40-50% of crossed ectopic testis (5).
Although there is no definite etiology for crossed ectopic testis, it was proposed that different factors, such as testicular adherence to Mullerian structures, a fusion of the Wolffian ducts, or defective gubernacular development, may be involved. Conversely, a positive family history also plays an important role in this anomaly (7). The clinical sign is the absence of testis along with an ipsilateral inguinal hernia. This anomaly should be followed since it might lead to infertility. It may contribute to the increasing risk of testicular cancer in these cases (4).
The diagnosis of crossed ectopic testis could be incidental or during the treatment of infertility. Crossed ectopic testis may be diagnosed before the age of 4 yr (4). Imaging methods, including ultrasound examination, computed tomography scan, and MRI are utilized to find this anomaly (8). However, MRI is more specific in finding this anomaly.
The options for treatment vary regarding the symptoms and other associated anomalies. Along with the treatment of infertility, the correction and relocation of ectopic testis should be considered. Sometimes, the cord is very short, and the position of the ectopic testis is very high, so the orchidopexy would be the best choice. If the testis has been atrophying, orchidectomy is considered to prevent malignancy (1, 9).
In our case, ultrasound examination and MRI were able to detect crossed ectopic testis that were consistent with Nunna et al. studies. They recommended undertaking MRI and/or ultrasonography before surgery (10). In our study, both testes were completely descended into the left hemiscrotum. Crossed ectopic testis and its complications had affected testosterone and semen fructose. He did not mention this kind of anomaly in his family. No genetic disease was observed; hence, gonadotropins were in the normal range. Our case dealt with infertility and underwent TESE surgery since he suffered from azoospermia. The case was recommended to return for infertility treatment with assisted reproduction treatment techniques.
4. Conclusion
The crossed ectopic testis is a rare anomaly. However, early diagnosis is important due to the coexisting complications, including infertility and testicular cancer. Imaging methods such as ultrasound examination, MRI, and CT scan could be used to diagnose this anomaly in suspected cases. Treatment would be surgical correction of coexisting anomalies and relocation of crossed ectopic testis. TESE procedure is utilized for the treatment of infertility.
Data Availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author Contributions
Contribution A. Vosough Taghi Dizaj: Designed, supervised the research, and revised the manuscript. M.A. Sadighi Gilani: Urologist, and the administrative supporter for collecting sample, F. Pahlavan: Drafting the manuscript, data collection, data analysis, and interpretation. A. Saadat Varnosfaderani: Data collection and revised the manuscript. All authors studied and approved the final manuscript.
Acknowledgments
The authors would like to thank the patient who participated in this study, also the Royan Institute, Tehran, Iran for their cooperation. No Artificial intelligence was used in this study.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Case Report |
Subject:
Reproductive Andrology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |