Fri, Apr 26, 2024
[Archive]
Volume 5, Issue 3 (7-2007)
IJRM 2007, 5(3): 61-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Allameh T, Mohammadizadeh F. Diagnostic value of hysteroscopy in abnormal uterine bleeding compared to pathology reports. IJRM 2007; 5 (3) :61-0
URL: http://ijrm.ir/article-1-68-en.html
URL: http://ijrm.ir/article-1-68-en.html
1- Department of Gynecology and Obstetrics, Isfahan University of Medical Sciences, Isfahan, Iran , t_allameh@med.mui.ac.ir
2- Department of Pathology, Isfahan University of Medical Sciences , Isfahan, Iran
2- Department of Pathology, Isfahan University of Medical Sciences , Isfahan, Iran
Full-Text [PDF 40 kb]
(672 Downloads)
| Abstract (HTML) (2206 Views)
Full-Text: (362 Views)
Introduction
Hysteroscopy is one of the newest diagnostic methods in gynecology with a relatively recent development. In this method, the whole uterine cavity is directly observed through hysteroscope. In the case of any pathologic lesion, biopsy is taken and treatment is carried out through hysteroscopy if needed (e.g. removal of submucosal myoma or endometrial polyp).
Hysteroscopy has been found to be a totally reliable method for the study of abnormal uterine bleeding (AUB) compared to histological tests (1).
This procedure has been generally accepted as the gold standard for evaluation of the uterine cavity. The most important benefit of hysteroscopy is its "see and treat" potential, which not only avoids multiple hospital visits, but also provides higher patient satisfaction. However to get the maximum benefit from this procedure, it is important to select patients properly and the investigation should be performed by skilled personnel to obtain optimal results so that patients are managed adequately and cost effectively (2).
General anesthesia is not necessary for diagnostic hysteroscopy, since the procedure can be performed by paracervical blocking or venous tranquilizers. This is why; it is counted as an appropriate outpatient method, economizing patient’s time and money. The patients who have contraindications for general anesthesia also benefit from this procedure.
Due to its high accuracy and patient acceptance, outpatient diagnostic hysteroscopy should become a first line investigation in postmenopausal patients with bleeding disorders (3). With high sensitivity and specificity of this method in diagnosis of uterine lesions, it can be used as an ideal diagnostic tool to assess the patients with AUB (4). Complications of hysteroscopy (vasovagal response, pain, hemorrhage and uterine perforation) have been reported in less than 2% of cases (5).
At present, hysteroscopy is not typically used as an initial diagnostic procedure in AUB because of its cost, invasiveness and need for a skilled operator (6).
The main goal of this study was defining the diagnostic value of hysteroscopy in evaluating uterine cavity in patients with AUB compared to pathologic reports.
Materials and methods
This was a descriptive analytic study conducted prospectively on patients in reproductive, perimenopausal or postmenopausal ages with complaint of AUB referring to Shahid Beheshti Hospital in Isfahan. The including criteria was: The patients in reproductive, perimenopausal, or postmenopausal ages who complain from AUB.
The excluding criteria were; virgin subjects, patients with contraindications for general anesthesia, pregnant or pregnancy suspected subjects, active gynecologic infections, known cases of endometrial cancer or malignant cervical lesions (6,7) .
With total number of 105 patients, the study was began in Dec 2001 and ended in Dec 2002.
The study and procedures were explained to the patients before entering the study, and written consent was obtained from women who participated in the study.
The patients with mentioned criteria were hospitalized and undergone hysteroscopy following general anesthesia. All of the procedures were carried out by one gynecologist. In the presence of any pathologic lesion, biopsy was taken and after removing the hysteroscope, routine dilatation and curettage were done. The reports were recorded. Both specimens from each patient were sent for pathologist in 10%formalin.
Pathologic study of hysteroscopic biopsies and curettage material were performed by one pathologist without awareness of hysteroscopic findings.
The hysteroscopy set specifications: The device used was Aesculap hysteroscope (AESCULAP AG & CO. KG company, Germany) 5mm continuous flow rigid. Expanding mediums were normal saline in mere diagnostic cases and sterile water in cases of electrosurgery.
All the data were registered in checklists including demographic characteristics, chief complaints, hysteroscopy findings and pathology results.
The data were coded and analyzed by SPSS-X and statistical indices were calculated.
Results
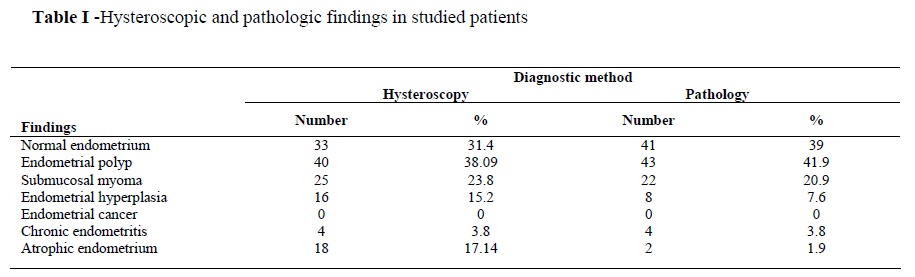
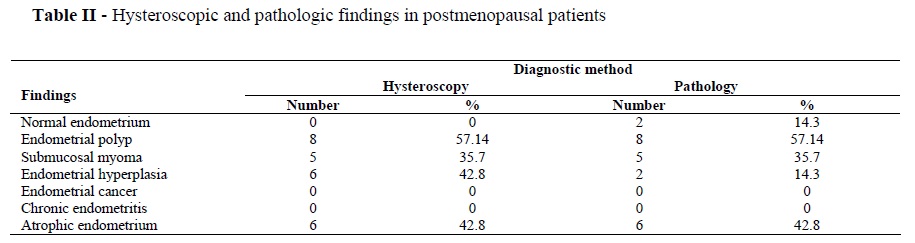
The subjects included 105 female patients aged between 21 to 61 years with mean age of 38.6 years and SD=10.8. Overall, 34.3% of patients were between 40-50 years old. The patients were classified in three age groups of child bearing age (<45 years), perimenopausal (45-50 years) and postmenopausal (>50 years). The patients’ complaints were menorrhagia in 22 cases (21%), menometrorrhagia in 69 cases (65.7%), and postmenopausal bleeding in 14 cases (13.3%). Hysteroscopy for patients with AUB showed sensitivity of 100%, specificity of 80.5%, positive predictive value (PPV) of 88.9% and negative predictive value (NPV) of 100%.
Sensitivity, specificity, PPV and NPV for endometrial polyp were 93%, 100%, 100% and 95.4%, respectively. These parameters were 100%, 96.4%, 88% and 100% respectively for submucosal myoma, and 25%, 89.7%, 12.5% and 93.3%, respectively for endometrial hyperplasia. There were 16 cases of endometrial hyperplasia according to hysteroscopic findings, but 8 cases of them were confirmed by pathology.
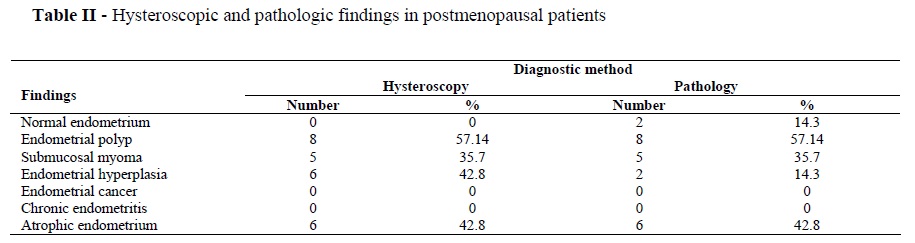
Hysteroscopic and pathologic findings of all
studied patients are shown in table I. Hysteroscopic and pathologic finding of postmenopausal patients are shown in table II.
Discussion
In our study, sensitivity, specificity, PPV and NPV of hysteroscopy in patients with AUB were 100%, 80.5%, 88.9% and 100%, respectively. Some studies have reported sensitivity of about 79% and specificity of 93%( 8).
In the study of Jakab et al (2001), the sensitivity of hysteroscopy in the diagnosis of intrauterine lesions was 97%( 9). Paschopoulos et al (2001) reported sensitivity and specificity of 92% and 95% for hysteroscopy in diagnosing intracavitary pathology in women with AUB (10).The research of Dueholm et al (2001) showed sensitivity and specificity of procedure as 84% and 88%, respectively (11). Bonnamy et al (2002) reported sensitivity and specificity of hysteroscopy as 78% and 97% in patients with AUB (12).
Kelekci et al (2005) found sensitivity of 87.5% and specificity of 100% for hysteroscopy in detecting intracavitary abnormalities (7).
As is seen, most of the studies have reported the sensitivity of hysteroscopy in diagnosing intrauterine lesions more than 80%, quite compatible with the results of this study. This finding proves hysteroscopy as a valid diagnostic method in AUB.
In our study, detection of endometrial polyp by hysteroscopy had sensitivity of 93%, specificity of 100%, PPV of 100% and NPV of 95.4%. Pasqualotto et al (2000) reported sensitivity of hysteroscopy for detection of endometrial polyp as 99%( 13), while Epstein et al (2001) reported it as 80%( 14). In the study of Jakab et al (2002), the sensitivity of hysteroscopy in detection of circumscribed intrauterine lesions was 100 %( 9).
In the study of Kelekci et al(2005) ,hysteroscopy revealed a sensitivity of 80%, a specificity of 80%, PPV of 100% and NPV of 93.9% for detecting endometrial polyps (7). Therefore, our study as well as other researches shows a high sensitivity of hysteroscopy in detection of endometrial polyp.
In our study, three cases of endometrial polyp were diagnosed as submucosal myoma by hysteroscopy, presumably because they were sessile polyps too hard to be distinguished from small myoma, something already mentioned by Dulholm et al (2001) in their study (11).
In this study, sensitivity, specificity, PPV and NPV of hysteroscopy in detection of submucosal myoma were 100%, 96.4%, 88%, and 100%, respectively. JaKab et al (2002) and Pasqualotto et al (2000) also reported the sensitivity of hysteroscopy for detection of submucosal myoma as 100 %( 9, 13).
In the study of Kelekci et al (2005), hysteroscopy had sensitivity, specificity, PPV and NPV of 100%, 100%, 100% and 100%, respectively in detecting submucosal mymoa (7).
Thus, hysteroscopy has a high diagnostic ability in detection of localized intracavitary uterine lesions such as polyp and myoma. It is far from expectation for this procedure to ignore these lesions, thus hysteroscopy relieves patients with these lesions from high cost and time waste resulting from additional interventions.
Hysteroscopy showed sensitivity, specificity, PPV and NPV of 25%, 89.7%, 12.5% and 93.3% respectively in detection of endometrial hyperplasia. There were some cases over diagnosed by hysteroscopy as endometrial hyperplasia, but no cases of hyperplasia were missed by this procedure.
No case of endometrial cancer was detected by hysteroscopy in our study, presumably because the highest frequency of endometrial carcinoma is among postmenopausal women with mean age of 61 years (15), while there were only 13.3% postmenopausal women in our study. In the study of Sousa et al (2001) on postmenopausal women with AUB, hysteroscopy revealed sensitivity of 88.9%, specificity of 98.3%, PPV of 88% and NPV of 98.3% in detection of endometrial carcinoma, presenting itself as a superior diagnostic procedure compared to ultrasonography (16).
Conclusion
The findings of this study show that hysteroscopy is an accurate diagnostic tool in evaluation of patients with AUB, especially when circumscribed intracavitary lesions are the underlying disorders leading to AUB. Determination of diagnostic value of hysteroscopy in detection of endometrial carcinoma needs further studies.
Hysteroscopy is one of the newest diagnostic methods in gynecology with a relatively recent development. In this method, the whole uterine cavity is directly observed through hysteroscope. In the case of any pathologic lesion, biopsy is taken and treatment is carried out through hysteroscopy if needed (e.g. removal of submucosal myoma or endometrial polyp).
Hysteroscopy has been found to be a totally reliable method for the study of abnormal uterine bleeding (AUB) compared to histological tests (1).
This procedure has been generally accepted as the gold standard for evaluation of the uterine cavity. The most important benefit of hysteroscopy is its "see and treat" potential, which not only avoids multiple hospital visits, but also provides higher patient satisfaction. However to get the maximum benefit from this procedure, it is important to select patients properly and the investigation should be performed by skilled personnel to obtain optimal results so that patients are managed adequately and cost effectively (2).
General anesthesia is not necessary for diagnostic hysteroscopy, since the procedure can be performed by paracervical blocking or venous tranquilizers. This is why; it is counted as an appropriate outpatient method, economizing patient’s time and money. The patients who have contraindications for general anesthesia also benefit from this procedure.
Due to its high accuracy and patient acceptance, outpatient diagnostic hysteroscopy should become a first line investigation in postmenopausal patients with bleeding disorders (3). With high sensitivity and specificity of this method in diagnosis of uterine lesions, it can be used as an ideal diagnostic tool to assess the patients with AUB (4). Complications of hysteroscopy (vasovagal response, pain, hemorrhage and uterine perforation) have been reported in less than 2% of cases (5).
At present, hysteroscopy is not typically used as an initial diagnostic procedure in AUB because of its cost, invasiveness and need for a skilled operator (6).
The main goal of this study was defining the diagnostic value of hysteroscopy in evaluating uterine cavity in patients with AUB compared to pathologic reports.
Materials and methods
This was a descriptive analytic study conducted prospectively on patients in reproductive, perimenopausal or postmenopausal ages with complaint of AUB referring to Shahid Beheshti Hospital in Isfahan. The including criteria was: The patients in reproductive, perimenopausal, or postmenopausal ages who complain from AUB.
The excluding criteria were; virgin subjects, patients with contraindications for general anesthesia, pregnant or pregnancy suspected subjects, active gynecologic infections, known cases of endometrial cancer or malignant cervical lesions (6,7) .
With total number of 105 patients, the study was began in Dec 2001 and ended in Dec 2002.
The study and procedures were explained to the patients before entering the study, and written consent was obtained from women who participated in the study.
The patients with mentioned criteria were hospitalized and undergone hysteroscopy following general anesthesia. All of the procedures were carried out by one gynecologist. In the presence of any pathologic lesion, biopsy was taken and after removing the hysteroscope, routine dilatation and curettage were done. The reports were recorded. Both specimens from each patient were sent for pathologist in 10%formalin.
Pathologic study of hysteroscopic biopsies and curettage material were performed by one pathologist without awareness of hysteroscopic findings.
The hysteroscopy set specifications: The device used was Aesculap hysteroscope (AESCULAP AG & CO. KG company, Germany) 5mm continuous flow rigid. Expanding mediums were normal saline in mere diagnostic cases and sterile water in cases of electrosurgery.
All the data were registered in checklists including demographic characteristics, chief complaints, hysteroscopy findings and pathology results.
The data were coded and analyzed by SPSS-X and statistical indices were calculated.
Results
The subjects included 105 female patients aged between 21 to 61 years with mean age of 38.6 years and SD=10.8. Overall, 34.3% of patients were between 40-50 years old. The patients were classified in three age groups of child bearing age (<45 years), perimenopausal (45-50 years) and postmenopausal (>50 years). The patients’ complaints were menorrhagia in 22 cases (21%), menometrorrhagia in 69 cases (65.7%), and postmenopausal bleeding in 14 cases (13.3%). Hysteroscopy for patients with AUB showed sensitivity of 100%, specificity of 80.5%, positive predictive value (PPV) of 88.9% and negative predictive value (NPV) of 100%.
Sensitivity, specificity, PPV and NPV for endometrial polyp were 93%, 100%, 100% and 95.4%, respectively. These parameters were 100%, 96.4%, 88% and 100% respectively for submucosal myoma, and 25%, 89.7%, 12.5% and 93.3%, respectively for endometrial hyperplasia. There were 16 cases of endometrial hyperplasia according to hysteroscopic findings, but 8 cases of them were confirmed by pathology.
Hysteroscopic and pathologic findings of all
studied patients are shown in table I. Hysteroscopic and pathologic finding of postmenopausal patients are shown in table II.
Discussion
In our study, sensitivity, specificity, PPV and NPV of hysteroscopy in patients with AUB were 100%, 80.5%, 88.9% and 100%, respectively. Some studies have reported sensitivity of about 79% and specificity of 93%( 8).
In the study of Jakab et al (2001), the sensitivity of hysteroscopy in the diagnosis of intrauterine lesions was 97%( 9). Paschopoulos et al (2001) reported sensitivity and specificity of 92% and 95% for hysteroscopy in diagnosing intracavitary pathology in women with AUB (10).The research of Dueholm et al (2001) showed sensitivity and specificity of procedure as 84% and 88%, respectively (11). Bonnamy et al (2002) reported sensitivity and specificity of hysteroscopy as 78% and 97% in patients with AUB (12).
Kelekci et al (2005) found sensitivity of 87.5% and specificity of 100% for hysteroscopy in detecting intracavitary abnormalities (7).
As is seen, most of the studies have reported the sensitivity of hysteroscopy in diagnosing intrauterine lesions more than 80%, quite compatible with the results of this study. This finding proves hysteroscopy as a valid diagnostic method in AUB.
In our study, detection of endometrial polyp by hysteroscopy had sensitivity of 93%, specificity of 100%, PPV of 100% and NPV of 95.4%. Pasqualotto et al (2000) reported sensitivity of hysteroscopy for detection of endometrial polyp as 99%( 13), while Epstein et al (2001) reported it as 80%( 14). In the study of Jakab et al (2002), the sensitivity of hysteroscopy in detection of circumscribed intrauterine lesions was 100 %( 9).
In the study of Kelekci et al(2005) ,hysteroscopy revealed a sensitivity of 80%, a specificity of 80%, PPV of 100% and NPV of 93.9% for detecting endometrial polyps (7). Therefore, our study as well as other researches shows a high sensitivity of hysteroscopy in detection of endometrial polyp.
In our study, three cases of endometrial polyp were diagnosed as submucosal myoma by hysteroscopy, presumably because they were sessile polyps too hard to be distinguished from small myoma, something already mentioned by Dulholm et al (2001) in their study (11).
In this study, sensitivity, specificity, PPV and NPV of hysteroscopy in detection of submucosal myoma were 100%, 96.4%, 88%, and 100%, respectively. JaKab et al (2002) and Pasqualotto et al (2000) also reported the sensitivity of hysteroscopy for detection of submucosal myoma as 100 %( 9, 13).
In the study of Kelekci et al (2005), hysteroscopy had sensitivity, specificity, PPV and NPV of 100%, 100%, 100% and 100%, respectively in detecting submucosal mymoa (7).
Thus, hysteroscopy has a high diagnostic ability in detection of localized intracavitary uterine lesions such as polyp and myoma. It is far from expectation for this procedure to ignore these lesions, thus hysteroscopy relieves patients with these lesions from high cost and time waste resulting from additional interventions.
Hysteroscopy showed sensitivity, specificity, PPV and NPV of 25%, 89.7%, 12.5% and 93.3% respectively in detection of endometrial hyperplasia. There were some cases over diagnosed by hysteroscopy as endometrial hyperplasia, but no cases of hyperplasia were missed by this procedure.
No case of endometrial cancer was detected by hysteroscopy in our study, presumably because the highest frequency of endometrial carcinoma is among postmenopausal women with mean age of 61 years (15), while there were only 13.3% postmenopausal women in our study. In the study of Sousa et al (2001) on postmenopausal women with AUB, hysteroscopy revealed sensitivity of 88.9%, specificity of 98.3%, PPV of 88% and NPV of 98.3% in detection of endometrial carcinoma, presenting itself as a superior diagnostic procedure compared to ultrasonography (16).
Conclusion
The findings of this study show that hysteroscopy is an accurate diagnostic tool in evaluation of patients with AUB, especially when circumscribed intracavitary lesions are the underlying disorders leading to AUB. Determination of diagnostic value of hysteroscopy in detection of endometrial carcinoma needs further studies.
Type of Study: Original Article |
References
1. Caserta D, Toro G, Porretta M, Mancini E, Moscarini M. Hysteroscopic vs histologic diagnosis: Study of 222 cases of abnormal uterine hemorrhage . Minerva Ginecol 1999; 51:169 -172.
2. Lalchandani S, Phillips K. Evaluation of endometrial cavity-investigation option. Rev Gynecol Prac 2003; 3:165-170. [DOI:10.1016/S1471-7697(03)00065-0]
3. Wieser F, Albrecht A, Kurz C, Wenzl R, Nagele F. Ambulatory hysteroscopy in evaluation of postmenopausal bleeding. Wien Klin Wochenschr 1999;111:289-293.
4. Malinova M. Ultrasonographic hysteroscopy, new approach for the investigation of the uterine cavity in women with postmenopausal bleeding. Akush Ginekol ( Sofiia ) 1999;38:36-38.
5. Lo KW, Yuen PM. The role of outpatient diagnostic hysteroscopy in identifying anatomic pathology and histo pathology in the endometrial cavity. J Am Assoc Gynecol Laparosc 2000; 7:381 -385. [DOI:10.1016/S1074-3804(05)60482-3]
6. Guido RS, Stovall DW. Hysteroscopy. Official reprint from Up To Date. 2006 Up to Date.
7. Kelekci S,Kaya E, Alan M, Alan Y, Bilge U, Mollamahmutoglu L. Comparison of transvaginal sonography , saline infusion sonography, and office hysteroscopy in reproductive-aged women with or without abnormal uterine bleeding. Fertil Steril 2005;84:682-686. [DOI:10.1016/j.fertnstert.2005.03.036]
8. Nichols DH, Clarke - Pearson DL. Gynecologic, obstetric, and related surgery. 2nd ed. St. Louis: Mosby; 2000:720 -750.
9. Jakab AJ , Ovari L , Juhasz B , Birinyi L , Bacsko G , Toth Z. Ultrasound diagnosis of focal intrauterine lesions. Orv Hetil 2002;143:1739 - 1743 .
10. Paschopoulos M, Lois ED, Alamanos Y, Kolipoulos G , Paraskevaidis E. Vaginoscopic hysteroscopy and transvaginal sonography in the evaluation of patients with abnormal uterine bleeding. J Am Assoc Gynecol Laparosc 2001; 8:506-510. [DOI:10.1016/S1074-3804(05)60612-3]
11. Dueholm M, Lundorf E, Hansen ES, Ledertoug S, Olesen F. Evaluation of the uterine cavity with magnetic resonance imaging , transvaginal sonography , hysterosonographic examination and diagnostic hysteroscopy. Fertil Steril 2001; 76:350-357 [DOI:10.1016/S0015-0282(01)01900-8]
12. Bonnamy L , Marret H , Perrotin F , Body G , Berger C , Lansac J . Sonohysterography : a prospective survey of results and complications in 81 patients . Eur J Obstet Gynecol Reprod Biol 2002; 102:42-47. [DOI:10.1016/S0301-2115(01)00567-X]
13. Pasqualotto EB, Margossian H , Price LL , Bradley LD . Accuracy of preoperative diagnostic tools and outcome of hysteroscopic management of menstrual dysfunction. J Am Assoc Gynecol Laparosc 2000; 7:201-209. [DOI:10.1016/S1074-3804(00)80041-9]
14. Epstein E, Ramirez A , Skoog L , Valentin L . Trans vaginal sonography , saline contrast sonohysterography and hysteroscopy for the investigation of women with postmenopausal bleeding and endometrium > 5 mm. Ultrasound Obstect Gynecol 2001;18 :157-162. [DOI:10.1046/j.1469-0705.2001.00472.x]
15. Rayan KJ ,Kistner RW. Kistner's gynecology and women's health.7th ed. St. Louis: Mosby;1999:121-142.
16. Sousa R , Silvestre M , Almeida e Sousa L , Falcao F , Dias I, Silva T , et al . Transvaginal ultrasonography and hysteroscopy in postmenopausal bleeding: a prospective study .Acta Obstet Gynecol Scand 2001; 80:856-562. [DOI:10.1034/j.1600-0412.2001.080009856.x]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |