Sat, Feb 21, 2026
[Archive]
Volume 22, Issue 10 (October 2024)
IJRM 2024, 22(10): 801-810 |
Back to browse issues page
Ethics code: IR.ACECR.REC.1398.002
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fazaeli H, Sheikholeslami A, Ebrahimi Z, Kalhor N, Naserpour L. Comparing intra-uterine injection of mononuclear cells and platelet-rich plasma on the pregnancy rate of women with recurrent implantation failure: An RCT. IJRM 2024; 22 (10) :801-810
URL: http://ijrm.ir/article-1-3366-en.html
URL: http://ijrm.ir/article-1-3366-en.html
1- Department of Cell Biology and Regenerative Medicine, Academic Center for Education, Culture, and Research (ACECR), Qom Branch, Qom, Iran.
2- Department of Reproductive Biology, Academic Center for Education, Culture, and Research (ACECR), Qom Branch, Qom, Iran.
3- Department of Reproductive Biology, Academic Center for Education, Culture, and Research (ACECR), Qom Branch, Qom, Iran. ,naserpour@acecr.ac.ir
2- Department of Reproductive Biology, Academic Center for Education, Culture, and Research (ACECR), Qom Branch, Qom, Iran.
3- Department of Reproductive Biology, Academic Center for Education, Culture, and Research (ACECR), Qom Branch, Qom, Iran. ,
Abstract: (1442 Views)
Background: Recurrent implantation failure (RIF) can be explained mainly by improper crosstalk between the embryo and endometrium. The T-helper1/T-helper2 profile balance influences effective embryo implantation. Endometrial immunomodulation via intrauterine injection of activated peripheral blood mononuclear cells (PBMCs) or autologous platelet-rich plasma (PRP) is a potentially efficient treatment option.
Objective: This study aims to examine the biochemical and clinical pregnancies resulting from the intrauterine administering of activated PBMCs and PRP in RIF women.
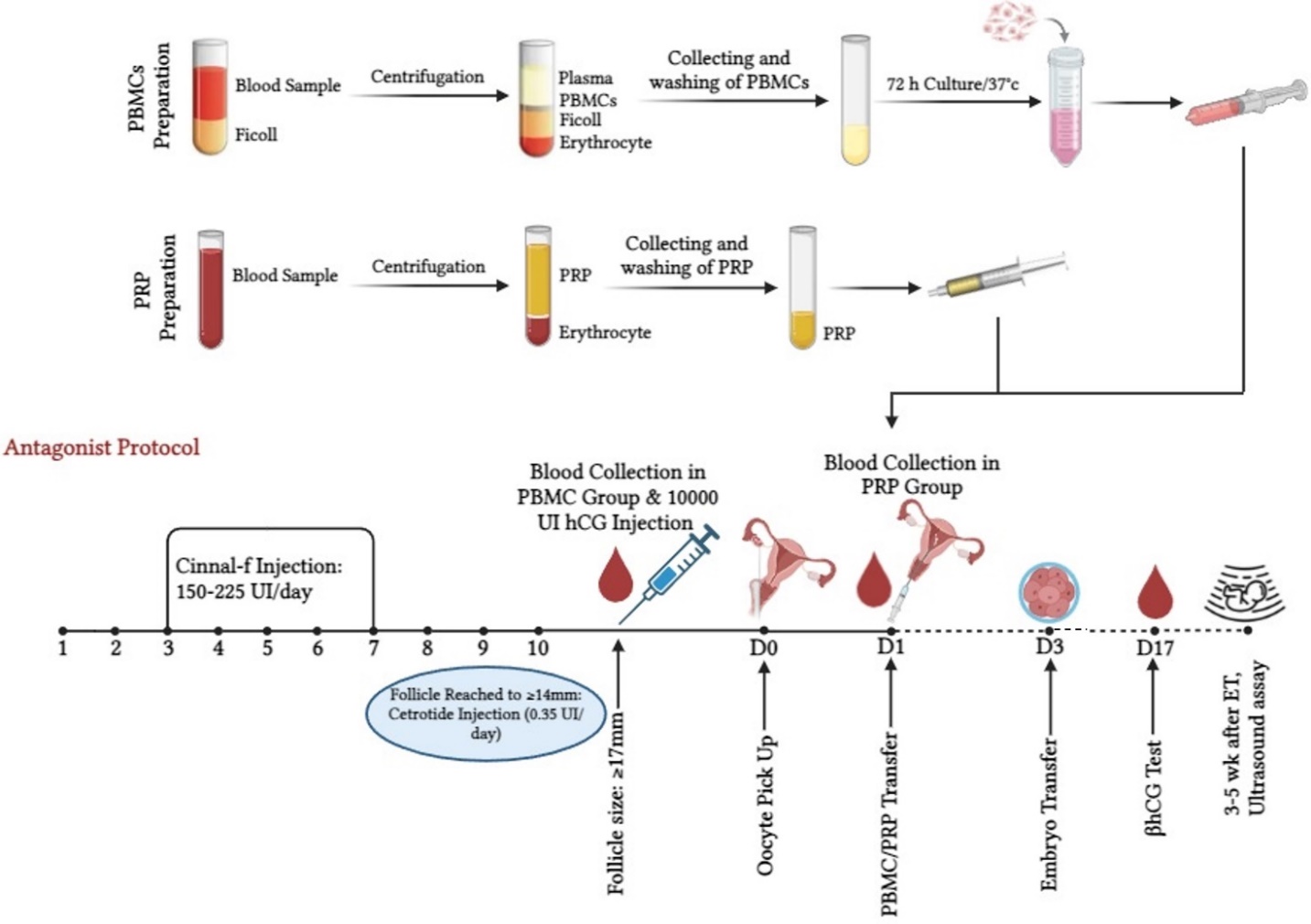
Materials and Methods: This randomized clinical trial study was done in the Rooya Infertility Treatment Center, Qom, Iran from November 2022 to April 2024. 96 women with at least 2 RIFs were randomized into control, PBMC, and PRP groups. Briefly, 3 ml of blood sample was collected and PBMCs were isolated using Ficoll separation solution, and cultured for 72 hr. PRP was separated from 10 ml of peripheral blood through centrifugation. 2 days before embryo transfer PBMCs or PRP were transferred into the endometrial cavity.
Results: Except for the duration of infertility, which was higher in the PBMC group, all other baseline characteristics were not statistically different. Moreover, a significantly higher rate of biochemical pregnancy was observed in the PRP (10/32) and PBMC (12/32) groups compared to the control (3/32) (p = 0.027), while the rate of clinical pregnancy was only significantly higher in the PBMC group (10/32) than in the control group (2/32) (p = 0.038).
Conclusion: Neither PBMC nor PRP interventions exhibited a substantial advantage over one another regarding biochemical and clinical pregnancy rates.
Objective: This study aims to examine the biochemical and clinical pregnancies resulting from the intrauterine administering of activated PBMCs and PRP in RIF women.
Materials and Methods: This randomized clinical trial study was done in the Rooya Infertility Treatment Center, Qom, Iran from November 2022 to April 2024. 96 women with at least 2 RIFs were randomized into control, PBMC, and PRP groups. Briefly, 3 ml of blood sample was collected and PBMCs were isolated using Ficoll separation solution, and cultured for 72 hr. PRP was separated from 10 ml of peripheral blood through centrifugation. 2 days before embryo transfer PBMCs or PRP were transferred into the endometrial cavity.
Results: Except for the duration of infertility, which was higher in the PBMC group, all other baseline characteristics were not statistically different. Moreover, a significantly higher rate of biochemical pregnancy was observed in the PRP (10/32) and PBMC (12/32) groups compared to the control (3/32) (p = 0.027), while the rate of clinical pregnancy was only significantly higher in the PBMC group (10/32) than in the control group (2/32) (p = 0.038).
Conclusion: Neither PBMC nor PRP interventions exhibited a substantial advantage over one another regarding biochemical and clinical pregnancy rates.
Registration ID in IRCT: IRCT20221010056132N1
Keywords: Peripheral blood mononuclear cells, Platelet-rich plasma, Recurrent implantation failure, Pregnancy.
Type of Study: Original Article |
Subject:
Assisted Reproductive Technologies
References
1. Farifteh Nobijari F, Arefi SS, Moini A, Taheripanah R, Fazeli E, Kharazi H, et al. Endometrium immunomodulation by intrauterine insemination administration of treated peripheral blood mononuclear cell prior frozen/thawed embryos in patients with repeated implantation failure. Zygote 2019; 27: 214-218. [DOI:10.1017/S0967199419000145] [PMID]
2. Benkhalifa M, Zayani Y, Bach V, Copin H, Feki M, Benkhalifa M, et al. Does the dysregulation of matrix metalloproteinases contribute to recurrent implantation failure? Expert Rev Proteomics 2018; 15: 311-323. [DOI:10.1080/14789450.2018.1464915] [PMID]
3. Busnelli A, Somigliana E, Cirillo F, Baggiani A, Levi-Setti PE. Efficacy of therapies and interventions for repeated embryo implantation failure: A systematic review and meta-analysis. Sci Rep 2021; 11: 1747. [DOI:10.1038/s41598-021-81439-6] [PMID] [PMCID]
4. Madkour A, Bouamoud N, Louanjli N, Kaarouch I, Copin H, Benkhalifa M, et al. Intrauterine insemination of cultured peripheral blood mononuclear cells prior to embryo transfer improves clinical outcome for patients with repeated implantation failures. Zygote 2016; 24: 58-69. [DOI:10.1017/S0967199414000719] [PMID]
5. Yoshioka S, Fujiwara H, Nakayama T, Kosaka K, Mori T, Fujii S. Intrauterine administration of autologous peripheral blood mononuclear cells promotes implantation rates in patients with repeated failure of IVF-embryo transfer. Hum Reprod 2006; 21: 3290-3294. [DOI:10.1093/humrep/del312] [PMID]
6. Piekarska K, Dratwa M, Radwan P, Radwan M, Bogunia-Kubik K, Nowak I. Pro- and anti-inflammatory cytokines and growth factors in patients undergoing in vitro fertilization procedure treated with prednisone. Front Immunol 2023; 14: 1250488. [DOI:10.3389/fimmu.2023.1250488] [PMID] [PMCID]
7. Andreescu M. The impact of the use of immunosuppressive treatment after an embryo transfer in increasing the rate of live birth. Front Med 2023; 10: 1167876. [DOI:10.3389/fmed.2023.1167876] [PMID] [PMCID]
8. Zhao Y, Zhang T, Guo X, Wong CK, Chen X, Chan YL, et al. Successful implantation is associated with a transient increase in serum pro-inflammatory cytokine profile followed by a switch to anti-inflammatory cytokine profile prior to confirmation of pregnancy. Fertil Steril 2021; 115: 1044-1053. [DOI:10.1016/j.fertnstert.2020.10.031] [PMID]
9. Lédée N, Petitbarat M, Chevrier L, Vitoux D, Vezmar K, Rahmati M, et al. The uterine immune profile may help women with repeated unexplained embryo implantation failure after in vitro fertilization. Am J Reprod Immunol 2016; 75: 388-401. [DOI:10.1111/aji.12483] [PMID] [PMCID]
10. Deshmukh H, Way SS. Immunological basis for recurrent fetal loss and pregnancy complications. Annu Rev Pathol 2019; 14: 185-210. [DOI:10.1146/annurev-pathmechdis-012418-012743] [PMID] [PMCID]
11. Liang P-Y, Diao L-H, Huang C-Y, Lian R-C, Chen X, Li G-G, et al. The pro-inflammatory and anti-inflammatory cytokine profile in peripheral blood of women with recurrent implantation failure. Reprod Biomed Online 2015; 31: 823-826. [DOI:10.1016/j.rbmo.2015.08.009] [PMID]
12. Bashiri A, Halper KI, Orvieto R. Recurrent implantation failure-update overview on etiology, diagnosis, treatment and future directions. Reprod Biol Endocrinol 2018; 16: 121. [DOI:10.1186/s12958-018-0414-2] [PMID] [PMCID]
13. Yu N, Zhang B, Xu M, Wang S, Liu R, Wu J, et al. Intrauterine administration of autologous peripheral blood mononuclear cells (PBMCs) activated by HCG improves the implantation and pregnancy rates in patients with repeated implantation failure: A prospective randomized study. Am J Reprod Immunol 2016; 76: 212-216. [DOI:10.1111/aji.12542] [PMID]
14. Chang Y, Li J, Chen Y, Wei L, Yang X, Shi Y, et al. Autologous platelet-rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med 2015; 8: 1286-1290.
15. Lee JW, Kwon OH, Kim TK, Cho YK, Choi KY, Chung HY, et al. Platelet-rich plasma: Quantitative assessment of growth factor levels and comparative analysis of activated and inactivated groups. Arch Plast Surg 2013; 40: 530-535. [DOI:10.5999/aps.2013.40.5.530] [PMID] [PMCID]
16. Makrigiannakis A, BenKhalifa M, Vrekoussis T, Mahjub S, Kalantaridou SN, Gurgan T. Repeated implantation failure: A new potential treatment option. Eur J Clin Invest 2015; 45: 380-384. [DOI:10.1111/eci.12417] [PMID]
17. Joao F, Ricaud G, Lamoureux J, Disdier M, Blais V, Adam C, et al. Intrauterine administration of activated peripheral blood mononuclear cells in intrauterine insemination: A prospective double-blind randomized clinical trial. J Obstet Gynaecol Can 2022; 44: 383-389. [DOI:10.1016/j.jogc.2021.11.010] [PMID]
18. Fan L, Sha M, Li W, Kang Q, Wu J, Chen S, et al. Intrauterine administration of peripheral blood mononuclear cells (PBMCs) improves embryo implantation in mice by regulating local Treg/Th17 cell balance. J Reprod Dev 2021; 67: 359-368. [DOI:10.1262/jrd.2021-006] [PMID] [PMCID]
19. Sakakibara M, Maeda Y, Nakamura K. Fetal loss due to Th1-skewed Th1/Th2 balance with increase (not decrease) of regulatory T cells in abortion-prone mouse model. J Toxicol Sci 2022; 47: 327-336. [DOI:10.2131/jts.47.327] [PMID]
20. Yu N, Yan W, Yin T, Wang Y, Guo Y, Zhou D, et al. HCG-activated human peripheral blood mononuclear cells (pbmc) promote trophoblast cell invasion. PLoS One 2015; 10: e0125589. [DOI:10.1371/journal.pone.0125589] [PMID] [PMCID]
21. Fujiwara H, Araki Y, Imakawa K, Saito S, Daikoku T, Shigeta M, et al. Dual positive regulation of embryo implantation by endocrine and immune systems-step-by-step maternal recognition of the developing embryo. Am J Reprod Immunol 2016; 75: 281-289. [DOI:10.1111/aji.12478] [PMID]
22. Xu Y, Hao C, Fang J, Liu X, Xue P, Miao R. Intrauterine perfusion of autologous platelet-rich plasma before frozen-thawed embryo transfer improves the clinical pregnancy rate of women with recurrent implantation failure. Front Med 2022; 9: 850002. [DOI:10.3389/fmed.2022.850002] [PMID] [PMCID]
23. Chang Y, Li J, Wei LN, Pang J, Chen J, Liang X. Autologous platelet-rich plasma infusion improves clinical pregnancy rate in frozen embryo transfer cycles for women with thin endometrium. Medicine 2019; 98: e14062. [DOI:10.1097/MD.0000000000014062] [PMID] [PMCID]
24. Tandulwadkar SR, Naralkar MV, Surana AD, Selvakarthick M, Kharat AH. Autologous intrauterine platelet-rich plasma instillation for suboptimal endometrium in frozen embryo transfer cycles: A pilot study. J Hum Reprod Sci 2017; 10: 208-212. [DOI:10.4103/jhrs.JHRS_28_17] [PMID] [PMCID]
25. Eftekhar M, Neghab N, Naghshineh E, Khani P. Can autologous platelet rich plasma expand endometrial thickness and improve pregnancy rate during frozen-thawed embryo transfer cycle? A randomized clinical trial. Taiwan J Obstet Gynecol 2018; 57: 810-813. [DOI:10.1016/j.tjog.2018.10.007] [PMID]
26. Coksuer H, Akdemir Y, Ulas Barut M. Improved in vitro fertilization success and pregnancy outcome with autologous platelet-rich plasma treatment in unexplained infertility patients that had repeated implantation failure history. Gynecol Endocrinol 2019; 35: 815-818. [DOI:10.1080/09513590.2019.1597344] [PMID]
27. Tehraninejad ES, Kashani NG, Hosseini A, Tarafdari A. Autologous platelet-rich plasma infusion does not improve pregnancy outcomes in frozen embryo transfer cycles in women with history of repeated implantation failure without thin endometrium. J Obstet Gynaecol Res 2021; 47: 147-151. [DOI:10.1111/jog.14445] [PMID]
28. Allahveisi A, Seyedoshohadaei F, Rezaei M, Bazrafshan N, Rahimi K. The effect of platelet-rich plasma on the achievement of pregnancy during frozen embryo transfer in women with a history of failed implantation. Heliyon 2020; 6: e03577. [DOI:10.1016/j.heliyon.2020.e03577] [PMID] [PMCID]
29. Qin Q, Chang H, Zhou S, Zhang S, Yuan D, Yu LL, et al. Intrauterine administration of peripheral blood mononuclear cells activated by human chorionic gonadotropin in patients with repeated implantation failure: A meta-analysis. J Reprod Immunol 2021; 145: 103323. [DOI:10.1016/j.jri.2021.103323] [PMID]
30. Yakin K, Oktem O, Urman B. Intrauterine administration of peripheral mononuclear cells in recurrent implantation failure: A systematic review and meta-analysis. Sci Rep 2019; 9: 3897. [DOI:10.1038/s41598-019-40521-w] [PMID] [PMCID]
31. Pourmoghadam Z, Soltani-Zangbar MS, Sheikhansari G, Azizi R, Eghbal-Fard Sh, Mohammadi H, et al. Intrauterine administration of autologous hCG- activated peripheral blood mononuclear cells improves pregnancy outcomes in patients with recurrent implantation failure; a double-blind, randomized control trial study. J Reprod Immunol 2020; 142: 103182. [DOI:10.1016/j.jri.2020.103182] [PMID]
32. Makrigiannakis A, Vrekoussis T, Makrygiannakis F, Ruso H, Kalantaridou SN, Gurgan T. Intrauterine CRH-treated PBMC in repeated implantation failure. Eur J Clin Invest 2019; 49: e13084. [DOI:10.1111/eci.13084] [PMID]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |