Sat, Feb 21, 2026
[Archive]
Volume 23, Issue 2 (February 2025)
IJRM 2025, 23(2): 171-184 |
Back to browse issues page
Ethics code: IR.TUMS.AEC.1401.001
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Gholami K, Asheghmadine E, Guitynavard F, Zareian Baghdadabad L, Taheri D, Zahmatkesh P, et al . An investigation of the therapeutic potential of the testicular tissue encapsulated in amnion membrane in mouse model: An experimental study. IJRM 2025; 23 (2) :171-184
URL: http://ijrm.ir/article-1-3400-en.html
URL: http://ijrm.ir/article-1-3400-en.html
Keykavoos Gholami1 

 , Elahe Asheghmadine2
, Elahe Asheghmadine2 

 , Fateme Guitynavard3
, Fateme Guitynavard3 

 , Leila Zareian Baghdadabad3
, Leila Zareian Baghdadabad3 

 , Diana Taheri4
, Diana Taheri4 

 , Parisa Zahmatkesh3
, Parisa Zahmatkesh3 

 , Leonardo Oliveira Reis5
, Leonardo Oliveira Reis5 

 , Seyed Mohammad Kazem Aghamir *6
, Seyed Mohammad Kazem Aghamir *6 




 , Elahe Asheghmadine2
, Elahe Asheghmadine2 

 , Fateme Guitynavard3
, Fateme Guitynavard3 

 , Leila Zareian Baghdadabad3
, Leila Zareian Baghdadabad3 

 , Diana Taheri4
, Diana Taheri4 

 , Parisa Zahmatkesh3
, Parisa Zahmatkesh3 

 , Leonardo Oliveira Reis5
, Leonardo Oliveira Reis5 

 , Seyed Mohammad Kazem Aghamir *6
, Seyed Mohammad Kazem Aghamir *6 


1- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran. 2. Department of Plastic & Reconstructive Surgery, Cedars-Sinai Medical Center, Los Angeles, CA, USA. & Department of Plastic & Reconstructive Surgery, Cedars-Sinai Medical Center, Los Angeles, CA, USA.
2- Students’ Scientific Research Center, Tehran University of Medical Sciences, Tehran, Iran.
3- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran.
4- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran. & Department of Pathology, Isfahan Kidney Disease Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
5- UroScience and Department of Surgery (Urology), School of Medical Sciences, University of Campinas, Unicamp, and Pontifical Catholic University of Campinas, PUC-Campinas, Campinas, São Paulo, Brazil.
6- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran. ,mkaghamir@tums.ac.ir
2- Students’ Scientific Research Center, Tehran University of Medical Sciences, Tehran, Iran.
3- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran.
4- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran. & Department of Pathology, Isfahan Kidney Disease Research Center, Isfahan University of Medical Sciences, Isfahan, Iran.
5- UroScience and Department of Surgery (Urology), School of Medical Sciences, University of Campinas, Unicamp, and Pontifical Catholic University of Campinas, PUC-Campinas, Campinas, São Paulo, Brazil.
6- Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran. ,
Abstract: (891 Views)
Background: Restoring fertility in male cancer individuals through testicular tissue transplantation faces challenges due to hypoxia-induced loss of spermatogonial stem cells (SSCs). Hydrogel encapsulation was explored to minimize hypoxic damage in testicular tissue transplantation. For this purpose, human amnion membrane (hAM)-derived hydrogel could be an alternative.
Objective: The potential of hAM-derived hydrogel to support testis tissue grafts was evaluated.
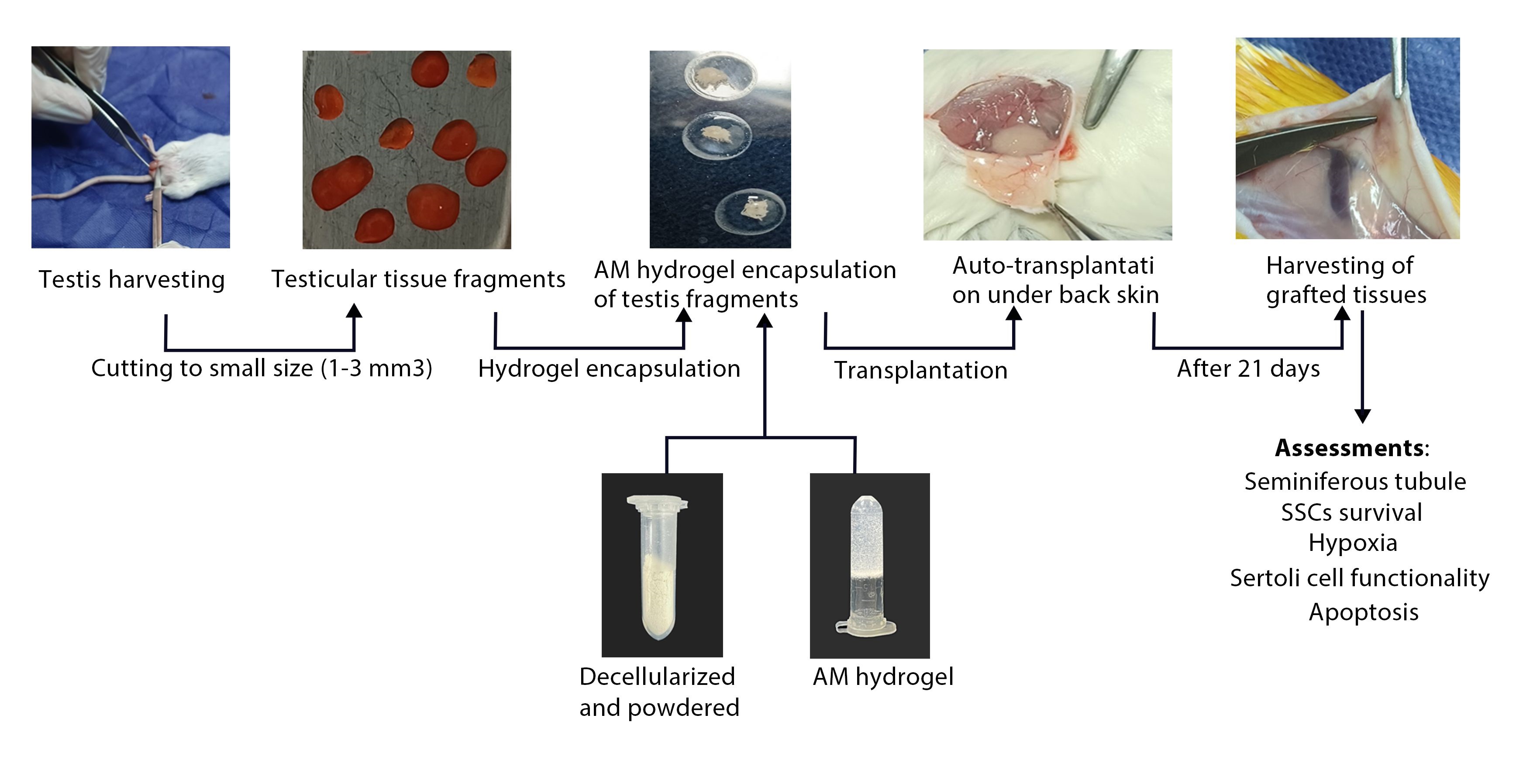
Materials and Methods: In this experimental study, testicular tissue samples (1-3 mm3) were obtained from 16 male NMRI mice (4-5 wk, 22 ± 2 gr). These tissue fragments were either encapsulated within a hydrogel derived from a hAM or left unencapsulated (control) prior to being autologously transplanted beneath the dorsal skin of mice subjected to hemilateral or bilateral orchiectomy. The grafted testicular tissues were histologically evaluated for key parameters, including the integrity of seminiferous tubules, survival of SSCs, Sertoli cell functionality, as well as hypoxia and apoptosis on day 21.
Results: No significant differences were observed between groups regarding ST integrity, number of SSCs, Sertoli cell functionality, or the rate of hypoxia-inducible factor 1-alpha and apoptosis (p ≤ 0.05).
Conclusion: In conclusion, this study demonstrated no effect of hAM hydrogel encapsulation on the outcomes of testicular tissue transplantation.
Objective: The potential of hAM-derived hydrogel to support testis tissue grafts was evaluated.
Materials and Methods: In this experimental study, testicular tissue samples (1-3 mm3) were obtained from 16 male NMRI mice (4-5 wk, 22 ± 2 gr). These tissue fragments were either encapsulated within a hydrogel derived from a hAM or left unencapsulated (control) prior to being autologously transplanted beneath the dorsal skin of mice subjected to hemilateral or bilateral orchiectomy. The grafted testicular tissues were histologically evaluated for key parameters, including the integrity of seminiferous tubules, survival of SSCs, Sertoli cell functionality, as well as hypoxia and apoptosis on day 21.
Results: No significant differences were observed between groups regarding ST integrity, number of SSCs, Sertoli cell functionality, or the rate of hypoxia-inducible factor 1-alpha and apoptosis (p ≤ 0.05).
Conclusion: In conclusion, this study demonstrated no effect of hAM hydrogel encapsulation on the outcomes of testicular tissue transplantation.
Type of Study: Original Article |
Subject:
Reproductive Urology
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |