Sun, Feb 22, 2026
[Archive]
Volume 23, Issue 5 (May 2025)
IJRM 2025, 23(5): 409-424 |
Back to browse issues page
Ethics code: IR.MAZUMS.IMAMHOSPITAL.REC.1402.125
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Safarloo F, Zamaniyan M, Nazar E, Samadaee Gelehkolaee K, Omid M, Peivandi S. Comparison of clinical pregnancy rates between hormone replacement therapy and modified natural cycle for endometrial preparation in frozen embryo transfer cycles: An RCT. IJRM 2025; 23 (5) :409-424
URL: http://ijrm.ir/article-1-3516-en.html
URL: http://ijrm.ir/article-1-3516-en.html
Farnaz Safarloo1 

 , Marzieh Zamaniyan2
, Marzieh Zamaniyan2 

 , Eisa Nazar3
, Eisa Nazar3 

 , Keshvar Samadaee Gelehkolaee4
, Keshvar Samadaee Gelehkolaee4 

 , Mahboubeh Omid4
, Mahboubeh Omid4 

 , Sepideh Peivandi *5
, Sepideh Peivandi *5 




 , Marzieh Zamaniyan2
, Marzieh Zamaniyan2 

 , Eisa Nazar3
, Eisa Nazar3 

 , Keshvar Samadaee Gelehkolaee4
, Keshvar Samadaee Gelehkolaee4 

 , Mahboubeh Omid4
, Mahboubeh Omid4 

 , Sepideh Peivandi *5
, Sepideh Peivandi *5 


1- Department of Obstetrics and Gynecology, Faculty of Medicine, Imam Khomeini Hospital, IVF Ward, Mazandaran University of Medical Sciences, Sari, Iran.
2- Department of Obstetrics and Gynecology, Faculty of Medicine, Sexual and Reproductive Health Research Center, Diabetes Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
3- Orthopedic Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
4- Department Of Reproductive Health and Midwifery, Faculty of Nursing and Midwifery, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
5- Department of Obstetrics and Gynecology, Faculty of Medicine, Sexual and Reproductive Health Research Center, Imam Khomeini Hospital, IVF Ward, Mazandaran University of Medical Sciences, Sari, Iran. ,speivandi@mazums.ac.ir; dr_peyvandi@yahoo.com
2- Department of Obstetrics and Gynecology, Faculty of Medicine, Sexual and Reproductive Health Research Center, Diabetes Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
3- Orthopedic Research Center, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
4- Department Of Reproductive Health and Midwifery, Faculty of Nursing and Midwifery, Imam Khomeini Hospital, Mazandaran University of Medical Sciences, Sari, Iran.
5- Department of Obstetrics and Gynecology, Faculty of Medicine, Sexual and Reproductive Health Research Center, Imam Khomeini Hospital, IVF Ward, Mazandaran University of Medical Sciences, Sari, Iran. ,
Abstract: (659 Views)
Background: Frozen-thawed embryo transfer (FET) during the endometrial receptivity window is important for implantation.
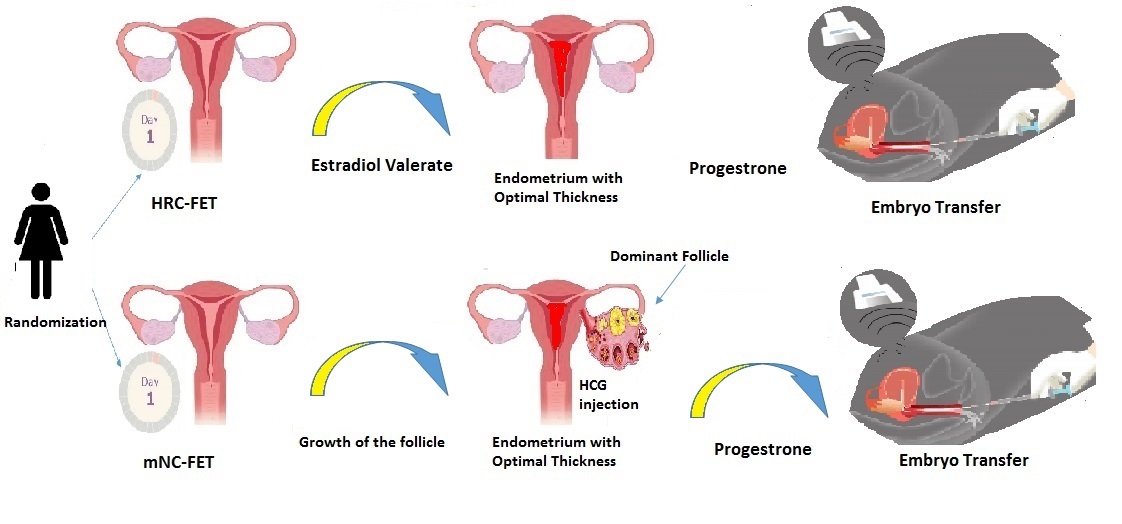
Objective: This study aims to compare the clinical pregnancy rate in 2 methods of endometrial preparation in FET using the hormone replacement cycle (HRC) and the modified natural cycle (mNC).
Materials and Methods: In this randomized clinical trial, 128 infertile women who visited the Imam Khomeini hospital infertility clinic, Sari, Iran between April and October 2024 were randomly assigned to 2 groups (n = 64/each): the mNC frozen embryo transfer group and the HRC group. In the mNC frozen embryo transfer group, ovulation was induced using human chorionic gonadotropin, and the timing of frozen embryo transfer was scheduled based on ovulation. The HRC group received estradiol valerate until the endometrial thickness reached 8 mm, then daily injections of progesterone were added and FET were performed.
Results: The participants had no significant differences in demographic characteristics. The primary outcome was clinical pregnancy rate with no significant difference between two groups (p = 0.282). No significant differences were observed between the mNC and HRC groups regarding the secondary outcome, which included human chorionic gonadotropin positive rate, chemical pregnancy rate, implantation rate, ongoing pregnancy rate, early miscarriage, ectopic pregnancy, twin pregnancy, and cycle cancellation rate. Significant differences were observed in the number of monitoring visits between the mNC frozen embryo transfer and HRC groups (p = 0.001).
Conclusion: Although the results indicate that the impact of both methods is similar, the fact that fewer visits are required in a natural cycle and there is also less need for hormones could make it preferable.
Objective: This study aims to compare the clinical pregnancy rate in 2 methods of endometrial preparation in FET using the hormone replacement cycle (HRC) and the modified natural cycle (mNC).
Materials and Methods: In this randomized clinical trial, 128 infertile women who visited the Imam Khomeini hospital infertility clinic, Sari, Iran between April and October 2024 were randomly assigned to 2 groups (n = 64/each): the mNC frozen embryo transfer group and the HRC group. In the mNC frozen embryo transfer group, ovulation was induced using human chorionic gonadotropin, and the timing of frozen embryo transfer was scheduled based on ovulation. The HRC group received estradiol valerate until the endometrial thickness reached 8 mm, then daily injections of progesterone were added and FET were performed.
Results: The participants had no significant differences in demographic characteristics. The primary outcome was clinical pregnancy rate with no significant difference between two groups (p = 0.282). No significant differences were observed between the mNC and HRC groups regarding the secondary outcome, which included human chorionic gonadotropin positive rate, chemical pregnancy rate, implantation rate, ongoing pregnancy rate, early miscarriage, ectopic pregnancy, twin pregnancy, and cycle cancellation rate. Significant differences were observed in the number of monitoring visits between the mNC frozen embryo transfer and HRC groups (p = 0.001).
Conclusion: Although the results indicate that the impact of both methods is similar, the fact that fewer visits are required in a natural cycle and there is also less need for hormones could make it preferable.
Keywords: Embryo transfer, Pregnancy rate, Vitrification, Hormone replacement therapy, Ovulation induction.
Type of Study: Original Article |
Subject:
Fertility & Infertility
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |