Sun, Feb 15, 2026
[Archive]
Volume 23, Issue 12 (December 2025)
IJRM 2025, 23(12): 995-1006 |
Back to browse issues page
Ethics code: IR.TBZMED.REC.1403.492
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Hamdi K, Khakpour S, Ghasemzadeh Darjani A, Farzadi L, Niknafs B, Navali N, et al . Comparison of frozen embryo transfer outcomes in hormonal vs. mild stimulation protocols in polycystic ovary syndrome women: A randomized controlled trial. IJRM 2025; 23 (12) :995-1006
URL: http://ijrm.ir/article-1-3612-en.html
URL: http://ijrm.ir/article-1-3612-en.html
Kobra Hamdi1 

 , Sahar Khakpour *2
, Sahar Khakpour *2 

 , Aliyeh Ghasemzadeh Darjani1
, Aliyeh Ghasemzadeh Darjani1 

 , Laya Farzadi1
, Laya Farzadi1 

 , Behrouz Niknafs3
, Behrouz Niknafs3 

 , Nazli Navali1
, Nazli Navali1 

 , Parvin Hakimi1
, Parvin Hakimi1 

 , Roghayeh Anvari Aliabad1
, Roghayeh Anvari Aliabad1 

 , Hamed Hajipour4
, Hamed Hajipour4 




 , Sahar Khakpour *2
, Sahar Khakpour *2 

 , Aliyeh Ghasemzadeh Darjani1
, Aliyeh Ghasemzadeh Darjani1 

 , Laya Farzadi1
, Laya Farzadi1 

 , Behrouz Niknafs3
, Behrouz Niknafs3 

 , Nazli Navali1
, Nazli Navali1 

 , Parvin Hakimi1
, Parvin Hakimi1 

 , Roghayeh Anvari Aliabad1
, Roghayeh Anvari Aliabad1 

 , Hamed Hajipour4
, Hamed Hajipour4 


1- Women's Reproductive Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Women's Reproductive Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. ,Skh55992@gmail.com; saharkhakpour@tbzmed.ac.ir
3- Department of Anatomical Sciences, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran.
4- School of Advanced Medical Sciences, Tabriz University of Medical Sciences, Tabriz, Iran.
2- Women's Reproductive Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. ,
3- Department of Anatomical Sciences, School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran.
4- School of Advanced Medical Sciences, Tabriz University of Medical Sciences, Tabriz, Iran.
Abstract: (34 Views)
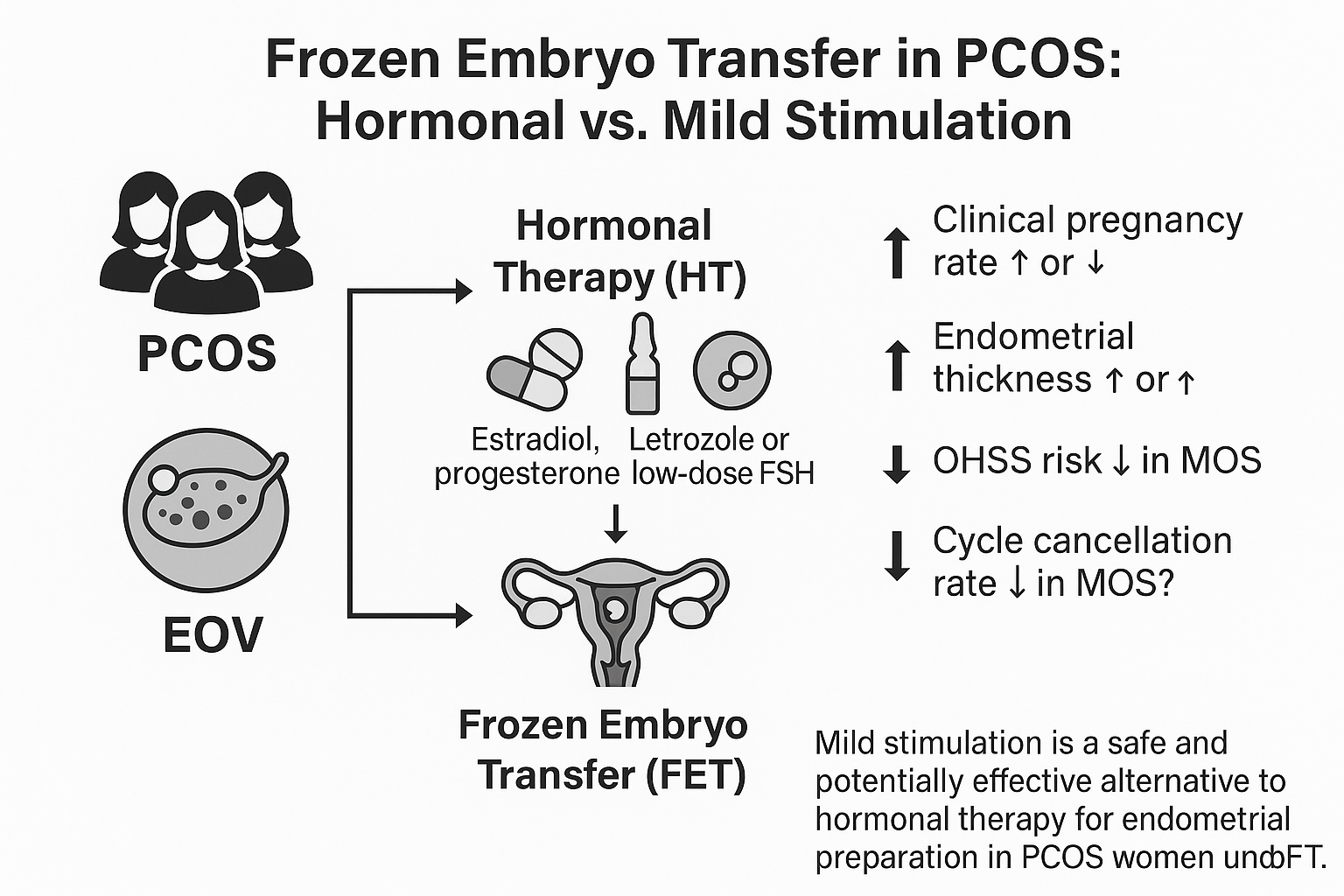
Background: Polycystic ovary syndrome (PCOS) is a leading cause of anovulatory infertility. In women undergoing frozen embryo transfer, the method of endometrial preparation (hormone replacement therapy [HRT] or mild ovarian stimulation [MOS]) can affect pregnancy outcomes. Letrozole‑based MOS protocols may improve endometrial receptivity and reduce miscarriage rates by upregulating key implantation markers leukemia inhibitory factor, dickkopf-related protein 1, leukemia inhibitory factor receptor, fibroblast growth factor 22, integrin alpha V beta 3.
Objective: This study aimed to compare the frozen embryo transfer outcomes in 2 endometrial preparation methods: HRT and MOS in infertile women with PCOS.
Materials and Methods: This double‑blind randomized trial included 100 infertile women with PCOS and frozen embryos who referred to Al‑Zahra hospital, Tabriz, Iran between October 2024 and 2025. Participants were assigned to HRT or MOS for endometrial preparation. In HRT, oral estradiol followed by injectable progesterone was used; in MOS, letrozole + follicle-stimulating hormone stimulation continued until follicle > 17 mm and endometrium ≥ 7.5 mm, then human chorionic gonadotropin was given. Cleavage‑stage transfer was performed in both groups, and pregnancy outcomes (chemical, clinical, and final) were compared.
Results: The number of transferred embryos (p = 0.771) and their quality (types 1 and 2) (p = 0.857) were similar between groups. The number of chemical pregnancies in the MOS group (25 cases) was non-significantly higher than in the HRT group (20 cases) (p = 0.078). However, the number of clinical pregnancies (p = 0.045) and the number of successful pregnancies (p = 0.049) were significantly higher in the MOS group compared to the HRT group.
Conclusion: This study showed that MOS achieved higher clinical and successful pregnancy rates than HRT in women with PCOS.
Objective: This study aimed to compare the frozen embryo transfer outcomes in 2 endometrial preparation methods: HRT and MOS in infertile women with PCOS.
Materials and Methods: This double‑blind randomized trial included 100 infertile women with PCOS and frozen embryos who referred to Al‑Zahra hospital, Tabriz, Iran between October 2024 and 2025. Participants were assigned to HRT or MOS for endometrial preparation. In HRT, oral estradiol followed by injectable progesterone was used; in MOS, letrozole + follicle-stimulating hormone stimulation continued until follicle > 17 mm and endometrium ≥ 7.5 mm, then human chorionic gonadotropin was given. Cleavage‑stage transfer was performed in both groups, and pregnancy outcomes (chemical, clinical, and final) were compared.
Results: The number of transferred embryos (p = 0.771) and their quality (types 1 and 2) (p = 0.857) were similar between groups. The number of chemical pregnancies in the MOS group (25 cases) was non-significantly higher than in the HRT group (20 cases) (p = 0.078). However, the number of clinical pregnancies (p = 0.045) and the number of successful pregnancies (p = 0.049) were significantly higher in the MOS group compared to the HRT group.
Conclusion: This study showed that MOS achieved higher clinical and successful pregnancy rates than HRT in women with PCOS.
Keywords: Polycystic ovary syndrome, Frozen embryo, Endometrium, Hormonal therapy, Mild ovarian stimulation protocol.
Type of Study: Original Article |
Subject:
Fertility & Infertility
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |