Sat, Dec 27, 2025
[Archive]
Volume 6, Issue 2 (7-2008)
IJRM 2008, 6(2): 45-0 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Taheripanah R, Hosseini M S, Hashemi M. Tubal patency after ultrasound guided local injection of KCL to tubal ectopic pregnancy with alive fetus. IJRM 2008; 6 (2) :45-0
URL: http://ijrm.ir/article-1-100-en.html
URL: http://ijrm.ir/article-1-100-en.html
1- Obstetrics and Gynecology Dept, IRHRC Center, Shahid Beheshti University, Tehran, Iran , Taheripanahf@yahoo.com
2- Obstetrics and Gynecology Dept, Imam Hossein Hospital, Shahid Beheshti university (M.C),Tehran, Iran
3- Pathology Department, Shahid Beheshti University (M.C), Tehran, Iran
2- Obstetrics and Gynecology Dept, Imam Hossein Hospital, Shahid Beheshti university (M.C),Tehran, Iran
3- Pathology Department, Shahid Beheshti University (M.C), Tehran, Iran
Full-Text [PDF 247 kb]
(1120 Downloads)
| Abstract (HTML) (3599 Views)
Full-Text: (554 Views)
Introduction
The incidence of ectopic pregnancy has been increasing in the last decades coincidental with significant advances in assisted reproductive technology (1, 2). On the other hand, ectopic pregnancy is diagnosed earlier due to more sensitive measurement of serum quantitative
b-HCG and high resolution transvaginal ultrasound (3).
Recently, advances in treatment and diagnosis, resulted for less invasive and conservative or non surgical treatment and saving the tubes for future pregnancy (4, 5). Methotrexate as a chemotherapic agent was used for medical therapy. It acts as trophoblastic growth inhibitor by inhibiting DNA synthesis. Methotrexate as a chemotherapic agent used for medical therapy. It acts as trophoblastic growth inhibitor by inhibiting DNA synthesis. Both systemic and local methotrexate has been useful in early un-ruptured diagnosed ectopic pregnancy (6, 7). The success rate of systemic methotrexate is about 90% (8) but it has some limitation in alive tubal ectopic pregnancy. Transvaginal ultrasound guided local injection of methotrexate is an alternative medical therapy for ectopic pregnancy that has been described in the last decade. It reduces the side effects of systemic methotrexate and increases the success rate especially in live and more gestational age of ectopic pregnancy. Methotrexate is contraindicated in heterotopic pregnancy due to teratogenic effects on fetus. So, we can use of potassium chloride or hypersmolar glucose (9) as a feticidal agent for heterotopic pregnancy (7, 10-11).
Ultrasound guided oocyte pick up and embryo reduction with local injection of KCL in the heart of fetus are the processes that can help the high multiple pregnancy and reduces the rate of major surgery complications. This approach reduces the morbidity and is associated with good fertility outcomes. In our hospital we use transvaginal ultrasound guided injection of KCL for embryo reduction in high order multiple pregnancies. In this case report we are discussing tubal patency and successful intrauterine pregnancy after conservative tubal ectopic pregnancy treatment with local injection of KCL to fetal heart in an infertile PCOD patient for showing the efficacy of this method for the cases that are contraindicated for medical therapy and methotrexate.
Case report
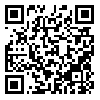
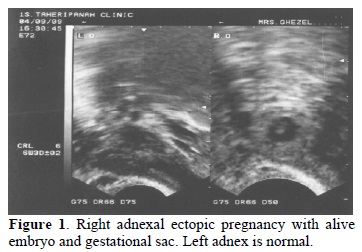
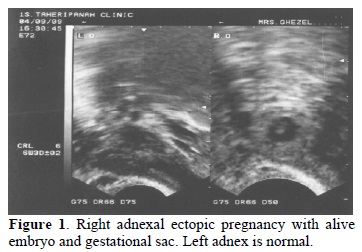
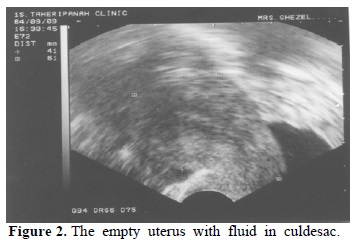
A 26 years old woman with history of 6 years primary infertility presented to our clinic for infertility treatment. Menstrual pattern was irregular and the patient had polycystic ovary syndrome according the 2003 Roterdam criteria (12). Semen analysis was within the normal range of WHO criteria (13). The patient has been received 6 cycles of clomiphene citrate as induction ovulation. Metformin was added to the induction ovulation regimens in three last cycles, but no pregnancy was occurred. Hystero-salpingography was performed on the 8th day of normal menstruation and without abnormal pattern under fluoroscopic observation using a water soluble medium. The HSG findings were normal uterus, open tubes without any hydrosalpinxes or filling defects. The patient was candidate for intrauterine insemination (IUI). Before IUI, she referred with lower right quadrant pain 2 months later after HSG. Patient had menstrual retardation and a positive B-hCG of 490Mu/ml on the 38th day LMP. Transvaginal ultrasound was carried out with 5 MHZ transvaginal probe (GE, a-100MP, USA). Ectopic pregnancy was confirmed by viewing a 4-5cm heterogenic mass in right adnexa. One gestational sac and alive 6 weeks +3 days of fetus with fetal heart was seen in it (Figure 1). The uterine cavity was empty and endometrial line was 14 millimeter. The ovaries were evaluated to rule out the other pathologies and heteroptopic pregnancy. There were some liquid in cul-de sac (Figure 2). The patient selected for local injection of KCL in gestational sac. The couple was counseled about the benefits and disadvantages of this conservative treatment. Patient had signed a written consent letter in which entire procedure and its complications were described.
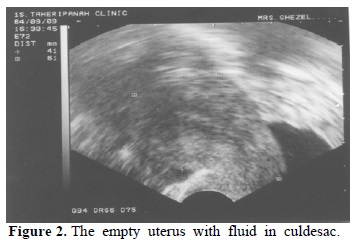
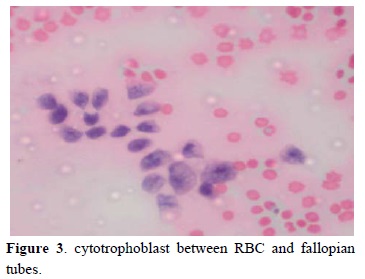
The baseline serum B-HCG on the day of procedure was 21,130 IU/ml and hemodynamic condition was stable. Under vaginal ultrasound guidance the syringe of 21 gauge needle of oocyte pick was entered to the gestational sac. At first a little fluid of gestational sac and wall was withdrawn and sent to pathology. Then 1 CC KCL (10%) was injected into the intacardiac cavity of the fetus until cardiac asystole was occurred after a short time. There was any vaginal bleeding and patients followed for several hours and discharged from hospital with good condition on that day. As follow up, quantitative serum B-hCG was obtained at 24 and 48 hours later and they were 14,340 and 12,000 IU/ml, respectively. Serial ultrasound examination was performed after 2 days for evaluation of adnexal mass and intra-abdominal hemorrhage. A collapsed gestational sac without cardiac activity revealed in the first ultrasound examination. Patient came to hospital one time by abdominal pain but no significant change was observed in CBC. Declining B-HCG was monitored as outpatient weekly intervals. Serum B-HCG declined gradually from 20,100 and was negative after 41 days. The pathology report of aspirated tissues confirmed the cytotrophbalst and tubal mucosa (Figure 3). Trophoblastic tissue established ectopic pregnancy. Periodic Ultrasound scanning was done due to gradually resorbtion of the adnexal mass.
After 2 normal menstrual cycles and normal pelvis in transvaginal ultrasound hysterosalpingography was done again. Both fallopian tubes were open and no hydrosalpinxes was observed in second HSG. There was no hydrosalpinx on ipsilateral tube. Induction ovulation and intrauterine insemination was done for patient in the next cycle according to clomiphene and gonadotropin protocol. Patient became pregnant and intrauterine pregnancy detected on the 5th weeks of pregnancy. Ongoing pregnancy continued and a normal 3450 gram male infant delivered by elective cesarean section at 39 weeks of gestation. There were no adhesions or sequels of ectopic pregnancy on the right side. The macroscopic view of the tubes were normal (Figure 4)

Discussion
The rate of ectopic pregnancy will be increased by increasing use of nowadays, IVF and induction ovulation regimens increased the ectopic pregnancy and high order multiple pregnancy. Fertility preservation is one of the most important aspects of ectopic pregnancy management. Nonsurgical and conservative treatment of ectopic pregnancy is one of the modern alternative treatments that it is able to reserve the fertility capacity of the patient and patent tubes free of peritubal adhesion (5).
Today, there are many alternatives and conservative treatments for un-ruptured ectopic pregnancy especially in rare places such as cervix, interstitial or cesarean scar (14-15). The routine use of ultrasound in obstetrics and gynecology and infertility treatment can be made conservative ectopic pregnancy treatments. Embryo reduction by ultrasound guided transabdominally and transvaginally injection of potassium chloride 10% into the fetal cardiac is a new modality of treatment in high order multiple pregnancy that is associated with good outcome (16). The advantages of this procedure are the elimination of radical surgery and reduce morbidity and fetal outcomes in high multiple pregnancy. Local injection of chemotherapeutic agents is a safe and proven modality that is especially indicated for pregnancies in which a laparoscopic approach is not ideal and systemic therapy either has failed or is not desired. Recently, this procedure has been doing for preserving the future fertility and intrauterine pregnancy in hetertopic ectopic pregnancy (17). Local injection may be increase successfully minimally invasive management of ectopic pregnancy with very high titer of B-hCG and cardiac activity if it will use combined with the systemic chemotherapic agents (18-19).
There are some papers about the success rate of local injection of drugs to gestational sac especially in rare location such as abdominal, cervical or heterotopic and is associated with desire prognosis. Although this minimally invasive approach is a good method of treatment but local injection requires experience in diagnostic and operative ultrasound (20). Golldstein in a review of the literature revealed that 55% of tubal heterotopic pregnancies treated by KCl injection required subsequent salpingectomy (21). It seems that non-tubal advanced ectopic pregnancies may be ideal for local therapy (22). In addition, the Patient should be informed about its side effects and has good compliance for follow up. Hemodynamic situation of the patient can be confirmed. Although, some evidences are present in this matter but there is no large study for this new method but spit article determined the usefulness of the local injection chemotherapeutic drugs and there are concerns about the advisability of this treatment. Because in heterotopic pregnancy, ongoing pregnancy may cause the persistence or even enlargement of remaining trophoblastic tissue and complicate the pregnancy with obstetrics hemorrhage (23).
As, we have been performing this procedure for embryo reduction in our center, we decided to use it for ectopic pregnancy termination in un-ruptured ectopic pregnancy.
Ujvari reported the saving the intrauterine pregnancy after embryo aspiration of cervical pregnancy and preserving fertility for future pregnancy (24). Frates described cases of successful intrathoracic kcl injection in cervical pregnancy (25).There are some evidences that this method can be useful for selective termination of heterotopic pregnancy and preserve the alive intrauterine fetus. There is no evidence that KCL injection induce electrolyte imbalance or any teratogen for the patient and the other fetuses. Although Benfila showed 91.7% tubal patency in interstitial pregnancy but no study was done to evaluate the subsequent tubal patency and successful spontaneous pregnancy (26). There was no significant difference in the tubal patency after systemic metotrexate, expectant management and surgical intervention but the ipsilateral tubal obstruction is more following the expectant management (27). Although contra-lateral obstruction after surgical intervention was similar with conservative treatment but no significant differences were observed. However, normal radiological finding in hysterosalpingography can not determine regarding tubal function, since disturbances in the tube may be a cause of ectopic pregnancy. We could establish the patency of the tube in our patient and ne sequels of adhesions in fallopian tubes and pelvis.
So, local KCL injection can be considered as a safe and alternative method in ectopic pregnancy patients that have contraindication for methotrexate due to alive fetus or other medical disorders such as hepatic diseases.
Therefore, ultrasound guidance of local KCL or methotrexate injection in fetus, intra-amniotic or intra-chorionic were able us to manage successfully ectopic pregnancies without surgical intervention and also preserves the fertility potential of the patients.
The incidence of ectopic pregnancy has been increasing in the last decades coincidental with significant advances in assisted reproductive technology (1, 2). On the other hand, ectopic pregnancy is diagnosed earlier due to more sensitive measurement of serum quantitative
b-HCG and high resolution transvaginal ultrasound (3).
Recently, advances in treatment and diagnosis, resulted for less invasive and conservative or non surgical treatment and saving the tubes for future pregnancy (4, 5). Methotrexate as a chemotherapic agent was used for medical therapy. It acts as trophoblastic growth inhibitor by inhibiting DNA synthesis. Methotrexate as a chemotherapic agent used for medical therapy. It acts as trophoblastic growth inhibitor by inhibiting DNA synthesis. Both systemic and local methotrexate has been useful in early un-ruptured diagnosed ectopic pregnancy (6, 7). The success rate of systemic methotrexate is about 90% (8) but it has some limitation in alive tubal ectopic pregnancy. Transvaginal ultrasound guided local injection of methotrexate is an alternative medical therapy for ectopic pregnancy that has been described in the last decade. It reduces the side effects of systemic methotrexate and increases the success rate especially in live and more gestational age of ectopic pregnancy. Methotrexate is contraindicated in heterotopic pregnancy due to teratogenic effects on fetus. So, we can use of potassium chloride or hypersmolar glucose (9) as a feticidal agent for heterotopic pregnancy (7, 10-11).
Ultrasound guided oocyte pick up and embryo reduction with local injection of KCL in the heart of fetus are the processes that can help the high multiple pregnancy and reduces the rate of major surgery complications. This approach reduces the morbidity and is associated with good fertility outcomes. In our hospital we use transvaginal ultrasound guided injection of KCL for embryo reduction in high order multiple pregnancies. In this case report we are discussing tubal patency and successful intrauterine pregnancy after conservative tubal ectopic pregnancy treatment with local injection of KCL to fetal heart in an infertile PCOD patient for showing the efficacy of this method for the cases that are contraindicated for medical therapy and methotrexate.
Case report
A 26 years old woman with history of 6 years primary infertility presented to our clinic for infertility treatment. Menstrual pattern was irregular and the patient had polycystic ovary syndrome according the 2003 Roterdam criteria (12). Semen analysis was within the normal range of WHO criteria (13). The patient has been received 6 cycles of clomiphene citrate as induction ovulation. Metformin was added to the induction ovulation regimens in three last cycles, but no pregnancy was occurred. Hystero-salpingography was performed on the 8th day of normal menstruation and without abnormal pattern under fluoroscopic observation using a water soluble medium. The HSG findings were normal uterus, open tubes without any hydrosalpinxes or filling defects. The patient was candidate for intrauterine insemination (IUI). Before IUI, she referred with lower right quadrant pain 2 months later after HSG. Patient had menstrual retardation and a positive B-hCG of 490Mu/ml on the 38th day LMP. Transvaginal ultrasound was carried out with 5 MHZ transvaginal probe (GE, a-100MP, USA). Ectopic pregnancy was confirmed by viewing a 4-5cm heterogenic mass in right adnexa. One gestational sac and alive 6 weeks +3 days of fetus with fetal heart was seen in it (Figure 1). The uterine cavity was empty and endometrial line was 14 millimeter. The ovaries were evaluated to rule out the other pathologies and heteroptopic pregnancy. There were some liquid in cul-de sac (Figure 2). The patient selected for local injection of KCL in gestational sac. The couple was counseled about the benefits and disadvantages of this conservative treatment. Patient had signed a written consent letter in which entire procedure and its complications were described.
The baseline serum B-HCG on the day of procedure was 21,130 IU/ml and hemodynamic condition was stable. Under vaginal ultrasound guidance the syringe of 21 gauge needle of oocyte pick was entered to the gestational sac. At first a little fluid of gestational sac and wall was withdrawn and sent to pathology. Then 1 CC KCL (10%) was injected into the intacardiac cavity of the fetus until cardiac asystole was occurred after a short time. There was any vaginal bleeding and patients followed for several hours and discharged from hospital with good condition on that day. As follow up, quantitative serum B-hCG was obtained at 24 and 48 hours later and they were 14,340 and 12,000 IU/ml, respectively. Serial ultrasound examination was performed after 2 days for evaluation of adnexal mass and intra-abdominal hemorrhage. A collapsed gestational sac without cardiac activity revealed in the first ultrasound examination. Patient came to hospital one time by abdominal pain but no significant change was observed in CBC. Declining B-HCG was monitored as outpatient weekly intervals. Serum B-HCG declined gradually from 20,100 and was negative after 41 days. The pathology report of aspirated tissues confirmed the cytotrophbalst and tubal mucosa (Figure 3). Trophoblastic tissue established ectopic pregnancy. Periodic Ultrasound scanning was done due to gradually resorbtion of the adnexal mass.
After 2 normal menstrual cycles and normal pelvis in transvaginal ultrasound hysterosalpingography was done again. Both fallopian tubes were open and no hydrosalpinxes was observed in second HSG. There was no hydrosalpinx on ipsilateral tube. Induction ovulation and intrauterine insemination was done for patient in the next cycle according to clomiphene and gonadotropin protocol. Patient became pregnant and intrauterine pregnancy detected on the 5th weeks of pregnancy. Ongoing pregnancy continued and a normal 3450 gram male infant delivered by elective cesarean section at 39 weeks of gestation. There were no adhesions or sequels of ectopic pregnancy on the right side. The macroscopic view of the tubes were normal (Figure 4)

Discussion
The rate of ectopic pregnancy will be increased by increasing use of nowadays, IVF and induction ovulation regimens increased the ectopic pregnancy and high order multiple pregnancy. Fertility preservation is one of the most important aspects of ectopic pregnancy management. Nonsurgical and conservative treatment of ectopic pregnancy is one of the modern alternative treatments that it is able to reserve the fertility capacity of the patient and patent tubes free of peritubal adhesion (5).
Today, there are many alternatives and conservative treatments for un-ruptured ectopic pregnancy especially in rare places such as cervix, interstitial or cesarean scar (14-15). The routine use of ultrasound in obstetrics and gynecology and infertility treatment can be made conservative ectopic pregnancy treatments. Embryo reduction by ultrasound guided transabdominally and transvaginally injection of potassium chloride 10% into the fetal cardiac is a new modality of treatment in high order multiple pregnancy that is associated with good outcome (16). The advantages of this procedure are the elimination of radical surgery and reduce morbidity and fetal outcomes in high multiple pregnancy. Local injection of chemotherapeutic agents is a safe and proven modality that is especially indicated for pregnancies in which a laparoscopic approach is not ideal and systemic therapy either has failed or is not desired. Recently, this procedure has been doing for preserving the future fertility and intrauterine pregnancy in hetertopic ectopic pregnancy (17). Local injection may be increase successfully minimally invasive management of ectopic pregnancy with very high titer of B-hCG and cardiac activity if it will use combined with the systemic chemotherapic agents (18-19).
There are some papers about the success rate of local injection of drugs to gestational sac especially in rare location such as abdominal, cervical or heterotopic and is associated with desire prognosis. Although this minimally invasive approach is a good method of treatment but local injection requires experience in diagnostic and operative ultrasound (20). Golldstein in a review of the literature revealed that 55% of tubal heterotopic pregnancies treated by KCl injection required subsequent salpingectomy (21). It seems that non-tubal advanced ectopic pregnancies may be ideal for local therapy (22). In addition, the Patient should be informed about its side effects and has good compliance for follow up. Hemodynamic situation of the patient can be confirmed. Although, some evidences are present in this matter but there is no large study for this new method but spit article determined the usefulness of the local injection chemotherapeutic drugs and there are concerns about the advisability of this treatment. Because in heterotopic pregnancy, ongoing pregnancy may cause the persistence or even enlargement of remaining trophoblastic tissue and complicate the pregnancy with obstetrics hemorrhage (23).
As, we have been performing this procedure for embryo reduction in our center, we decided to use it for ectopic pregnancy termination in un-ruptured ectopic pregnancy.
Ujvari reported the saving the intrauterine pregnancy after embryo aspiration of cervical pregnancy and preserving fertility for future pregnancy (24). Frates described cases of successful intrathoracic kcl injection in cervical pregnancy (25).There are some evidences that this method can be useful for selective termination of heterotopic pregnancy and preserve the alive intrauterine fetus. There is no evidence that KCL injection induce electrolyte imbalance or any teratogen for the patient and the other fetuses. Although Benfila showed 91.7% tubal patency in interstitial pregnancy but no study was done to evaluate the subsequent tubal patency and successful spontaneous pregnancy (26). There was no significant difference in the tubal patency after systemic metotrexate, expectant management and surgical intervention but the ipsilateral tubal obstruction is more following the expectant management (27). Although contra-lateral obstruction after surgical intervention was similar with conservative treatment but no significant differences were observed. However, normal radiological finding in hysterosalpingography can not determine regarding tubal function, since disturbances in the tube may be a cause of ectopic pregnancy. We could establish the patency of the tube in our patient and ne sequels of adhesions in fallopian tubes and pelvis.
So, local KCL injection can be considered as a safe and alternative method in ectopic pregnancy patients that have contraindication for methotrexate due to alive fetus or other medical disorders such as hepatic diseases.
Therefore, ultrasound guidance of local KCL or methotrexate injection in fetus, intra-amniotic or intra-chorionic were able us to manage successfully ectopic pregnancies without surgical intervention and also preserves the fertility potential of the patients.
Type of Study: Original Article |
References
1. Abusheikba N, Salha O, Brinssden P. Extrauterine pregnancy following assisted conception treatment. Hum Reprod Update 2000; 5: 80-82. [DOI:10.1093/humupd/6.1.80]
2. Ludwig M, Kaisi M, Bauer O, Diedrich K. Heterotopic pregnancy in a spontaneous cycle: do not forget about it. Eur J Obstet Gynecol Reprod Biol 199l; 87: 91-93. [DOI:10.1016/S0301-2115(99)00079-2]
3. Godin PA, Bassil S, Donnez J. An ectopic pregnancy developing in a previous caesarean section scar. Fertil Steril 1997; 67: 398-400. [DOI:10.1016/S0015-0282(97)81930-9]
4. Nawroth F, Foth D, Wilhelm L, Schmidt T, Warm M, Romer T.Conservative treatment of ectopic pregnancy in a caesarean section scar with methotrexate: a case report. Eur J Obstet Gynecol Reprod Biol 2001; 99:135-137. [DOI:10.1016/S0301-2115(01)00365-7]
5. Mukul LV, Teal SB. Current Management of Ectopic Pregnancy. Obstet Gynecol Clin N Am 2007; 4: 403-419. [DOI:10.1016/j.ogc.2007.07.001]
6. Stovall TG, Ling FW, Gray LA, Carson SA, Buster JE. Methotrexate treatment of unruptured ectopic pregnancy: a report of 100 cases. Obstet Gynecol 1991; 77: 749-753.
7. Fernandez H, Benifla JL, Lelaidier C, Baton C, Frydman R. Methotrexate treatment of ectopic pregnancy: 100 cases treated by primary transvaginal injection under sonographic control. Fertil Steril 1993; 59: 773-777. [DOI:10.1016/S0015-0282(16)55858-0]
8. Sperrof L, Fritz MA. Clinical Gynecologic endocrinology and infertility. 7th edition. Lippincott. 2005: 1275-1300
9. Roberts H, Kohlenber C, Lanzarone V, Murray H. Ectopic pregnancy in lower segment uterine scar. Aust NZ J Obstet Gynecol 1998; 38: 114-116. [DOI:10.1111/j.1479-828X.1998.tb02976.x]
10. Monteagudo A, Tarricone NJ, Timor-Tritsch IE, Lerner JP. Successful transvaginal ultrasound-guided puncture and injection of a cervical pregnancy in a patient with simultaneous intrauterine pregnancy and a history of a previous cervical pregnancy. Ultrasound Obstet. Gynecol 1996; 8: 381-386. [DOI:10.1046/j.1469-0705.1997.08060381.x]
11. Benifla JL, Fernandez H, Sebban E, Darai E, Frydman R, Madelenat P. Alternative to surgery of treatment of unruptured interstitial pregnancy: 15 cases of medical treatment. Eur J Obstet Gynecol Reprod Biol 1996; 70: 151-156. [DOI:10.1016/S0301-2115(95)02589-8]
12. Rotterdam. The Netherlands.Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome.Fertil Steril 2004; 81:19-25. [DOI:10.1016/j.fertnstert.2003.10.004]
13. World Health Organiztion, Laboratory, manual for examination of human sperm and Sperm-mucus interaction. 4th edition. Cambridge University press 1999.
14. Jeng CJ, Ko ML, Shen J. Transvaginal ultrasound-guided treatment of cervical pregnancy. Obstet Gynecol 2007; 109:1076-1082. [DOI:10.1097/01.AOG.0000262052.09350.52]
15. Salomon LJ, Fernandez H, Chauveaud A, Doumerc S, Frydman R .Successful management of a heterotopic Caesarean scar pregnancy: potassium chloride injection with preservation of the intrauterine gestation: case report. Hum Reprod 2003; 18:189-191. [DOI:10.1093/humrep/deg010]
16. Papiernik E, Grangé G, Zeitlin J. Should multifetal pregnancy reduction be used for prevention of preterm deliveries in triplet or higher order multiple pregnancies? J Perinat Med 1998; 26:365-370. [DOI:10.1515/jpme.1998.26.5.365]
17. .Ozgur K, Isikoglu M. Cornual heterotopic pregnancy: conservative treatment with transvaginal embryo reduction. Arch Gynecol Obstet 2005; 271(1):73-75. [DOI:10.1007/s00404-003-0587-5]
18. Verma U, Jacques E.Conservative management of live tubal pregnancies by ultrasound guided potassium chloride injection and systemic methotrexate treatment. J Clin Ultrasound 2005; 33: 460-463. [DOI:10.1002/jcu.20179]
19. Takashima M, Yamasaki M, Fujita I, Ohashi M, Matsuo H, Mochizuki M, et al. Enhanced magnetic resonance imaging in monitoring of conservative treatment of cervical pregnancy. J Obstet Gynaecol 1995; 21: 545-550. [DOI:10.1111/j.1447-0756.1995.tb00910.x]
20. Monteagudo A, Minior VK, Stephenson C, Monda S, Timor-Tritsch IE. Non-surgical management of live ectopic pregnancy with ultrasound -guided local injection:a case series.Ultrasound Obstet Gynecol 2005; 25: 282-288. [DOI:10.1002/uog.1822]
21. Goldstein JS, Ratts VS, Philpott T, Dahan MH. Risk of surgery after use of potassium chloride for treatment of tubal heterotopic pregnancy. Obstet Gynecol 2006; 107:506-508. [DOI:10.1097/01.AOG.0000175145.23512.5e]
22. Raughley MJ, Frishman GN. Local treatment of ectopic pregnancy. Semin Reprod Med 2007; 25:99-115. [DOI:10.1055/s-2007-970049]
23. Gyamfi C, Cohen S, Stone JL. Maternal complication of cervical heterotopic pregnancy after successful potassium chloride fetal reduction. Fertil Steril 2004; 82:940-943. [DOI:10.1016/j.fertnstert.2004.03.044]
24. Ujvari E, Krizsa F, Sebestyen A, Varbiro S, Paulin F. Successful management of intrauterine twin and concomitant cervical pregnancy: a case report. Fetal Diagn Ther 2006; 21:181-184. [DOI:10.1159/000089300]
25. Frates MC,Benson cb, Doubilet PM. Cervical ectopic pregnancy :results of conservative treatment. Radiology 1994; 191:773. [DOI:10.1148/radiology.191.3.8184062]
26. Benifla JL, Fernandez H, Sebban E, Darai E, Frydman R, Madelenat P. Alternative to surgery of treatment of unruptured interstitial pregnancy: 15 cases of medical treatment. Eur J Obstet Gynecol Reprod Biol 1996: 27; 70:151-156. [DOI:10.1016/S0301-2115(95)02589-8]
27. Ghazeeri GS, Phillips OP, Emerson DS, Kutteh WH, Ke RW. Live birth after treatment of a heterotopic cornual pregnancy with fetal intrathoracic KCI. A case report. J Reprod Med 2002; 47:1038-1040.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |