Thu, Feb 19, 2026
[Archive]
Volume 21, Issue 1 (January 2023)
IJRM 2023, 21(1): 53-60 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aliani F, Haghshenas Z, Vosough Dizaj A, Arabipoor A, Vesali S, Ashrafi M. Birth prevalence of genital anomalies among males conceived by intracytoplasmic sperm injection cycles: A cross-sectional study. IJRM 2023; 21 (1) :53-60
URL: http://ijrm.ir/article-1-2295-en.html
URL: http://ijrm.ir/article-1-2295-en.html
Fatemeh Aliani1 

 , Zahra Haghshenas1
, Zahra Haghshenas1 

 , Ahmad Vosough Dizaj2
, Ahmad Vosough Dizaj2 

 , Arezoo Arabipoor3
, Arezoo Arabipoor3 

 , Samira Vesali4
, Samira Vesali4 

 , Mahnaz Ashrafi *5
, Mahnaz Ashrafi *5 




 , Zahra Haghshenas1
, Zahra Haghshenas1 

 , Ahmad Vosough Dizaj2
, Ahmad Vosough Dizaj2 

 , Arezoo Arabipoor3
, Arezoo Arabipoor3 

 , Samira Vesali4
, Samira Vesali4 

 , Mahnaz Ashrafi *5
, Mahnaz Ashrafi *5 


1- Department of Pediatrics, Faculty of Medicine, Tehran University of Medical Sciences, Tehran, Iran.
2- Department of Reproductive Imaging, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
3- Department of Endocrinology and Female Infertility, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
4- Reproductive Epidemiology Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
5- Department of Endocrinology and Female Infertility, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran. Shahid Akbarabadi Clinical Research Development Unit (ShACRDU), Iran University of Medical Science (IUMS), Tehran, Iran. ,dr.mahnaz.ashrafi@gmail.com
2- Department of Reproductive Imaging, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
3- Department of Endocrinology and Female Infertility, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
4- Reproductive Epidemiology Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran.
5- Department of Endocrinology and Female Infertility, Reproductive Biomedicine Research Center, Royan Institute for Reproductive Biomedicine, ACECR, Tehran, Iran. Shahid Akbarabadi Clinical Research Development Unit (ShACRDU), Iran University of Medical Science (IUMS), Tehran, Iran. ,
Keywords: Cryptorchidism, Hypospadias, Microinjections, Prevalence, Reproductive techniques, Urogenital abnormalities.
Full-Text [PDF 275 kb]
(1389 Downloads)
| Abstract (HTML) (1812 Views)
1. Introduction
During the past 4 decades, assisted reproductive technology (ART) has been used as a standard worldwide medical practice to achieve pregnancy. ART is responsible for an estimated 1-5.9% of conceptions in some developed countries (1). In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) are the 2 main ART modalities. Because sperm and oocytes are manipulated outside the body, there are concerns regarding embryos derived from these invasive procedures (2). The findings of several studies and meta-analyses indicate that ART is associated with an increased risk of congenital anomalies (1-5). Results of previous studies have suggested an association between ART and some specific cardiac birth defects (6, 7), as well as some noncardiac defects such as cleft lip with or without cleft palate (8); hypospadias (9, 10), neural tube defects (11), esophageal, anorectal (8, 12), genitourinary defects (13), and large intestinal atresias (12). However, the magnitude of these associations and the spectrum of the involved defects remains unknown (14).
Presumed reasons to explain the higher risk of congenital malformations (CM) in ART infants include underlying subfertility, medications for ovulation induction, micromanipulation in ICSI and/or IVF, as well as increase in multiple gestations and prematurity (14). More CM have been observed in ICSI as a more invasive treatment method in cases where sperm could not pass through the natural route and physiologic deletion of abnormal sperms does not occur (oligospermia) (15). Similar interventions applied in IVF include the gonadotropin stimulator, oocyte aspiration, and culture media, which likely raise the incidence of CM (15). Some studies have investigated whether there is a higher risk of CM in offspring conceived by ICSI than IVF. However, they reported controversial results (9, 15-17). It was hypothesized that congenital genitourinary malformations, such as hypospadias, are more frequent after ICSI than after IVF. Moreover, they stated that there is a lack of robust data due to the rarity of these conditions (9). Hence, it was concluded that the increased prevalence of congenital genitourinary malformations was observed in singletons born after ART; however, more studies are warranted for confirmation (17). Only one study in Iran evaluated congenital anomalies and could not find a significant relationship between the type of infertility treatments and CM; however, the rate of CM after the ICSI cycles (11.7%) was slightly higher than after IVF cycles (5.9%) (15).
The developmental effect of ART on infants remains an important subject that needs further monitoring and investigation. This cross-sectional study with the retrospective design was done to evaluate the prevalence rate of congenital anomalies, particularly male genital malformations, in offspring conceived by ICSI at Royan Institute.
2. Materials and Methods
This cross-sectional study was performed at Royan Institute, Tehran, Iran from April 2013-December 2015. After registering the ICSI cycles in Hakim's software system at Royan Institute, data regarding pregnancies were investigated, and all live births were monitored and followed retrospectively. The ICSI cycles and embryo transfer procedure were performed with standard protocols at Royan Institute. We collected the data regarding the cause of infertility and type of embryo transfer from participants’ records. The characteristics of newborns were also collected and recorded from the follow-up clinic. Gestational age was determined as 14 days before oocyte pick-up until delivery. To exclude outliers, only children with gestational ages between 22 and 44 wk and birth weight between 400 and 7000 gr were included. Preterm birth was considered as delivery before 37 completed weeks of gestation. Low-birth weight (LBW) was defined as 2500 gr and very LBW as 1500 gr (18).
All children were assessed at birth by neonatologists and the premature infants were reevaluated at the expected date of delivery. The diagnosis of the genital anomaly was determined on the basis of the clinical examination at the expected date of delivery. Sonography was performed if the anomaly was not diagnosed by a physical exam. A diagnosis of hypospadias was made as a failure of fusion of the urethra was observed, and the urethral meatus was ectopically located. Cryptorchidism could not be diagnosed if the testis was in the inguinal canal or not palpable. Testis in a high scrotal position was not considered to be cryptorchidism (19). Micropenis was described as a penis 2.5 standard deviations (SD) smaller than the mean for the child's age and race. It was diagnosed by observing a stretched penis length of less than 1.9 centimeters at birth. Testicular regression syndrome or vanishing testis is reported to be due to the subsequent atrophy and disappearance in the fetal life of an initially normal testis, and its diagnosis is confirmed by surgery (20). Epispadias was defined by observing the opening of the urethra in the back of the penis (19).
2.1. Ethical considerations
The study was approved by the Institutional Review Boards and the Ethical Committees of Royan Institute, Tehran, Iran (Code: IR.ACECR.ROYAN.REC.1397.207). The patients' file information has been used while maintaining the confidentiality of names, and oral consent has been obtained from all participants.
2.2. Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences 20.0 (SPSS; SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to evaluate the normality of continuous variables. Normally distributed continuous variables are presented as mean (SD). Comparison of means for dichotomous variables was performed by the independent sample t test, and the Chi-square test was used to examine the relationship between categorical variables. A p-value < 0.05 was considered to be statistically significant.
3. Results
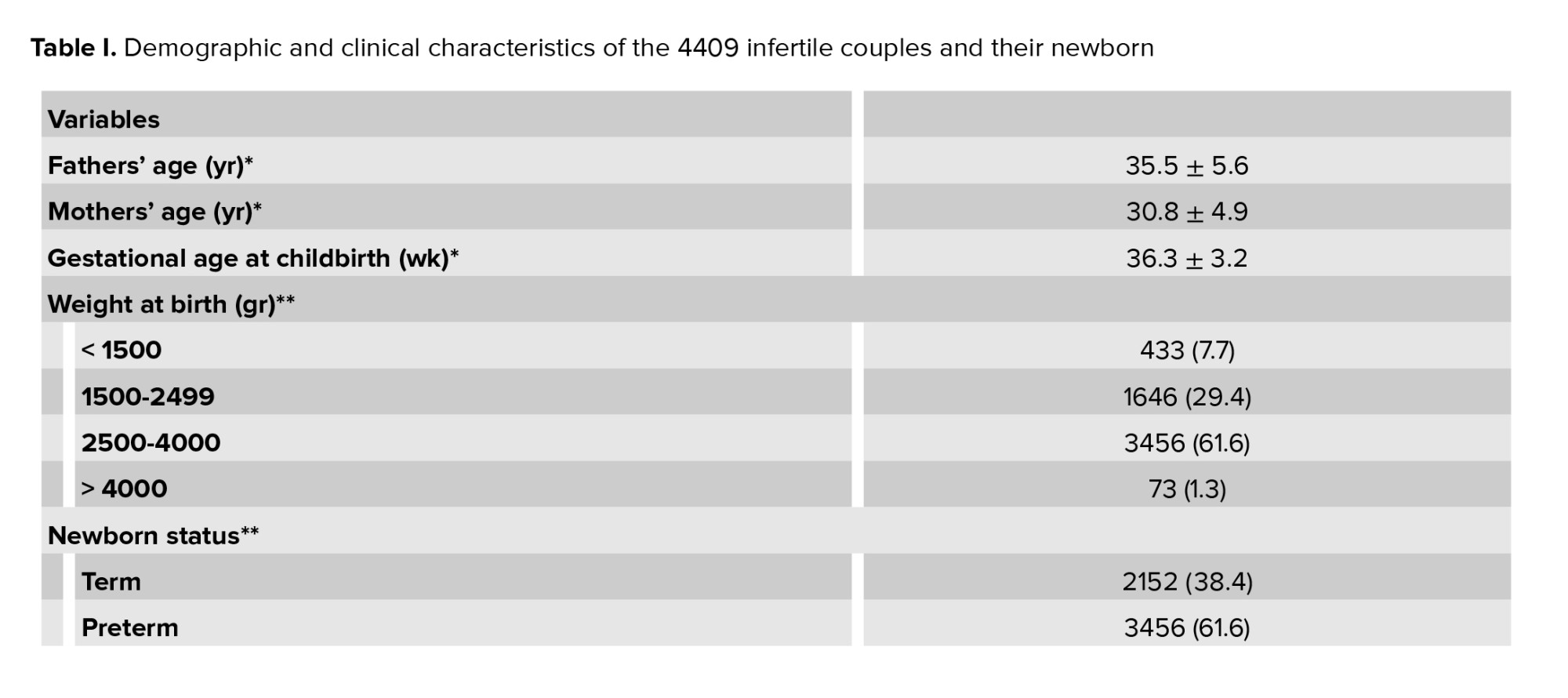
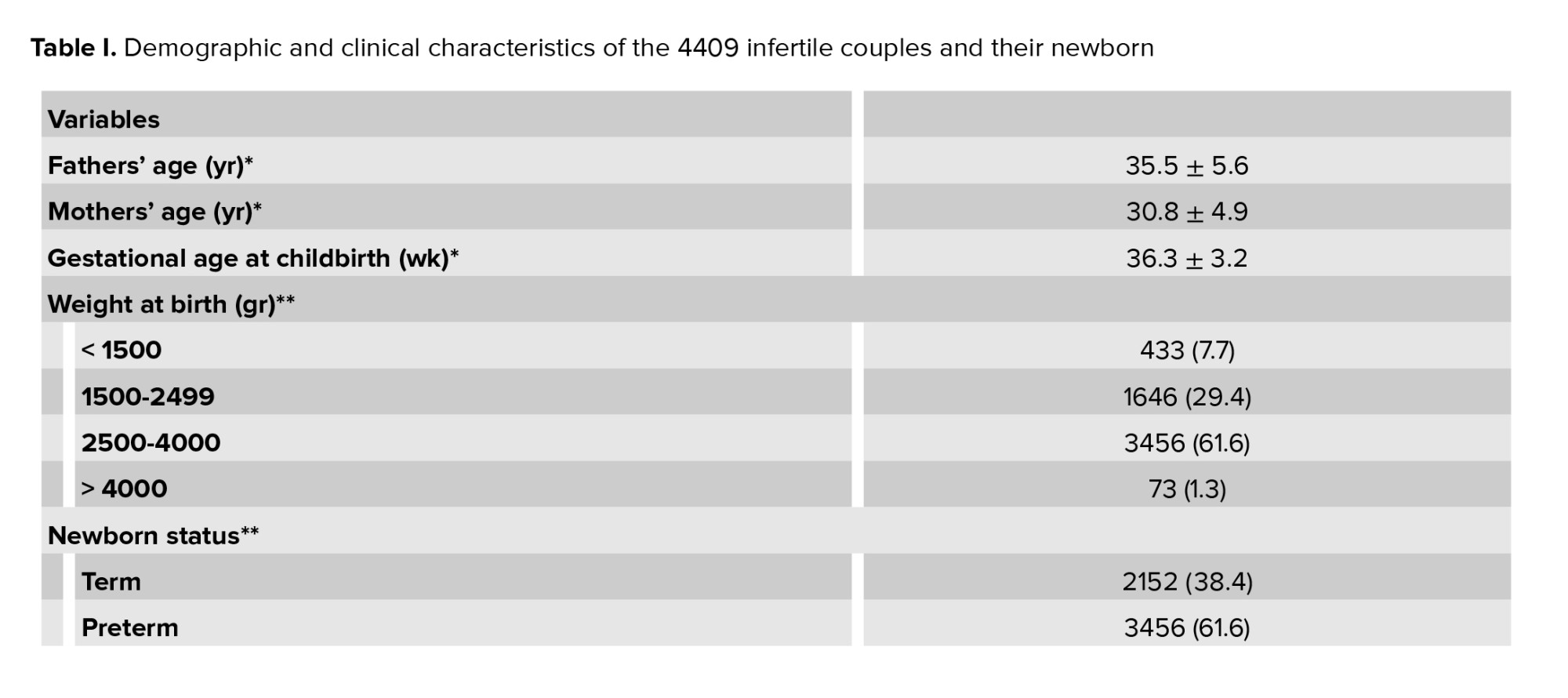
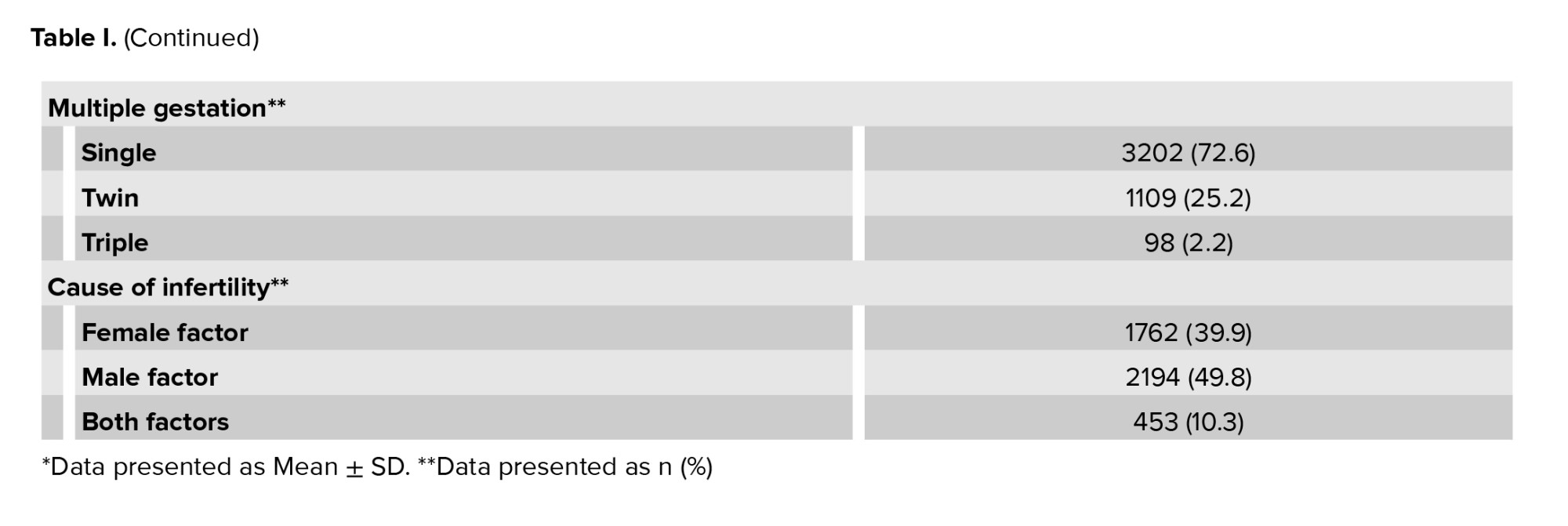
In this study, 4409 infertile couples with successful pregnancies after ICSI cycles were investigated to examine the male urogenital anomalies in their newborns. The mean age of fathers and mothers was 35.58 ± 5.64 yr and 30.86 ± 4.92 yr. Out of 4409 pregnancies, 3202 pregnancies (72.6%) were single, 1109 pregnancies (25.2%) twin, and 98 pregnancies (2.2%) triple. In total, the all-out number of live births were 5608. Of the 4409 couples studied, 1762 couples (39.9%) had female infertility, 2194 couples (49.8%) had male infertility, and 453 couples (10.3%) had both male and female infertility factors. The mean gestational age at delivery was 36.3 ± 3.2 wk. Of 5608 live births, 2152 (38.4%) were preterm and 3456 (61.6%) had normal weight. Of 5608 live births, 2614 newborns were male (46.61%), and the remaining (2994 newborns) were female. The demographic and clinical characteristics of the participating couples are shown in table I.
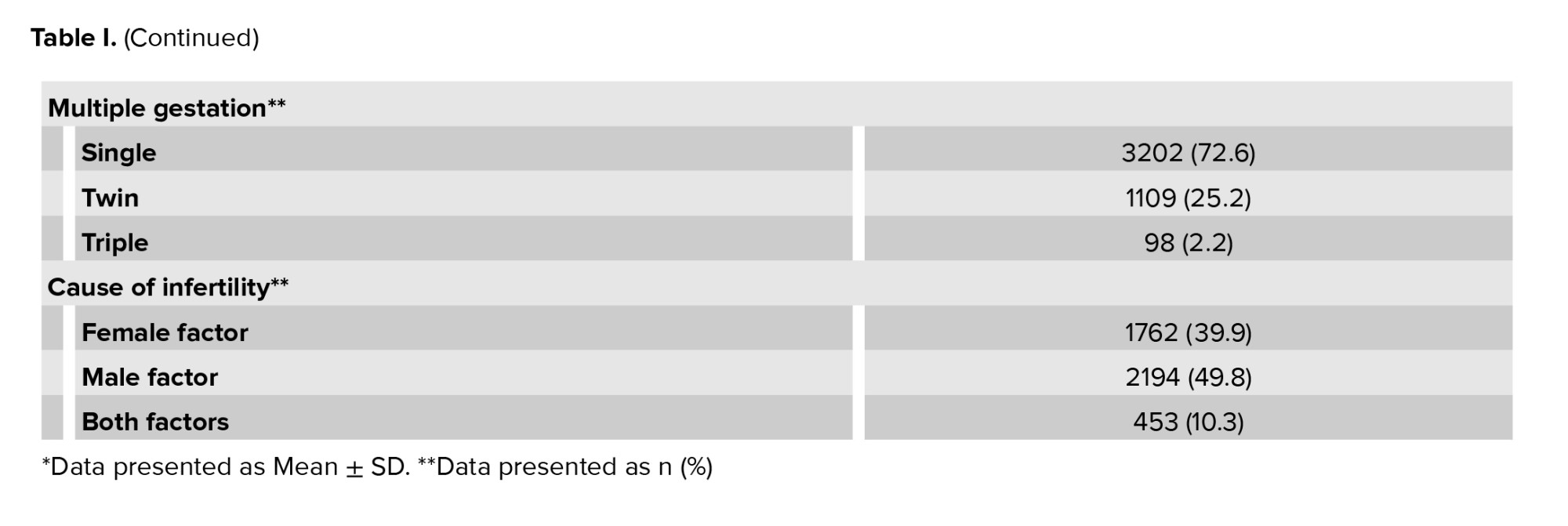
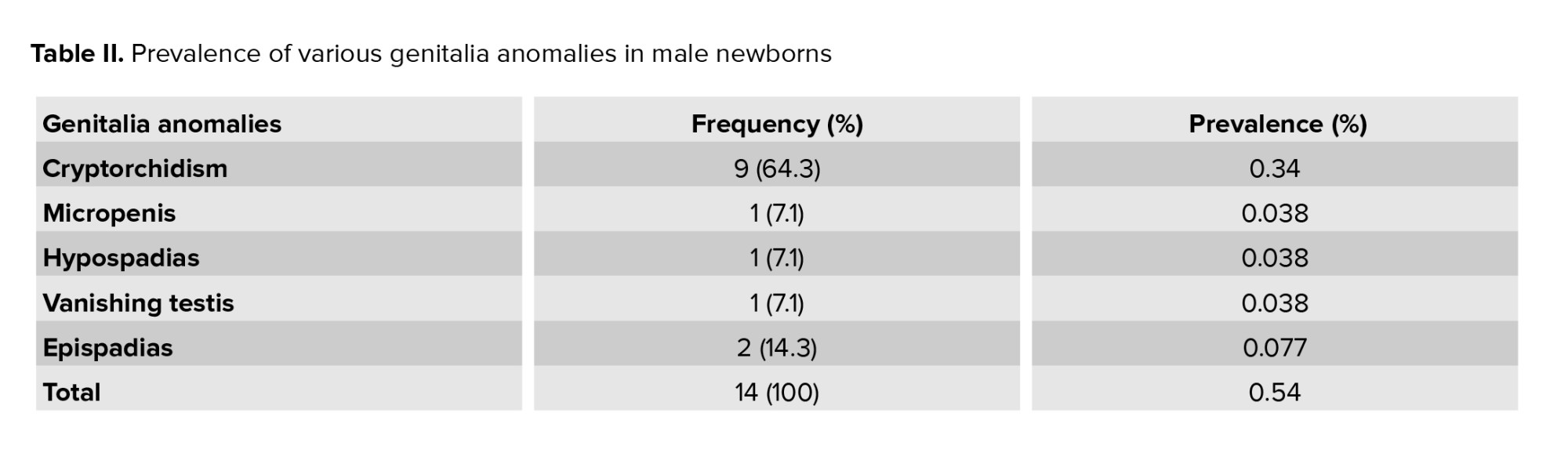
Out of 2614 male newborns, only 14 (0.54%) had urogenital anomalies. As seen in table II, the highest prevalence of genitalia anomalies were related to cryptorchidism [9 (0.34%)]. The lowest prevalence of genitalia anomalies were related to hypospadias, micropenis, and vanishing testis [1 (0.038%)].
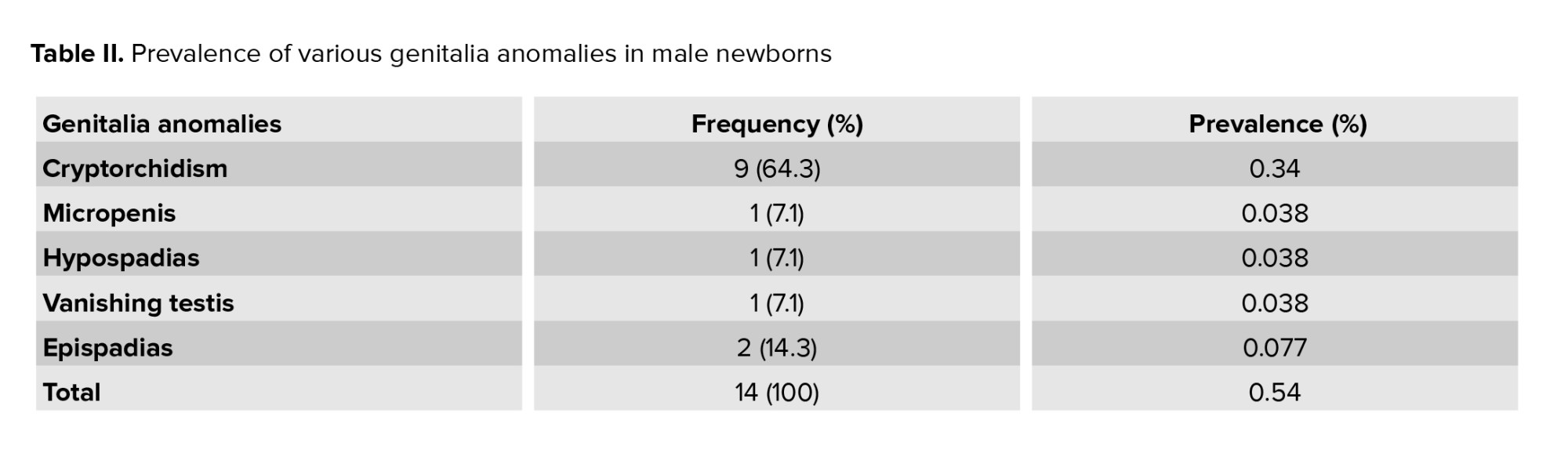
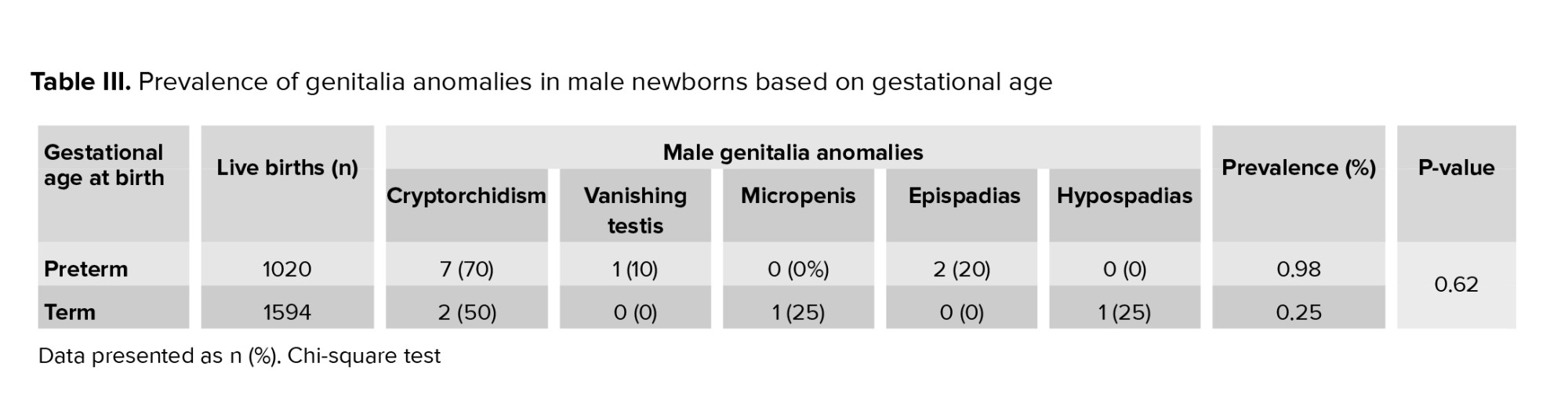
Table III shows the prevalence of genitalia anomalies based on gestational age in male newborns. The highest prevalence of genitalia anomalies was related to preterm (< 37 wk) newborns (0.98%). The most common anomaly was cryptorchidism (7 cases from 10 anomalies). The prevalence of genitalia anomalies in male term newborns (> 37 wk) was 0.25%. The total prevalence of genitalia anomalies by gestational age in male newborns was 0.54%. The Chi-square test showed that the relationship between the prevalence of male genitalia anomalies and the gestational age was not statistically significant (p = 0.62).
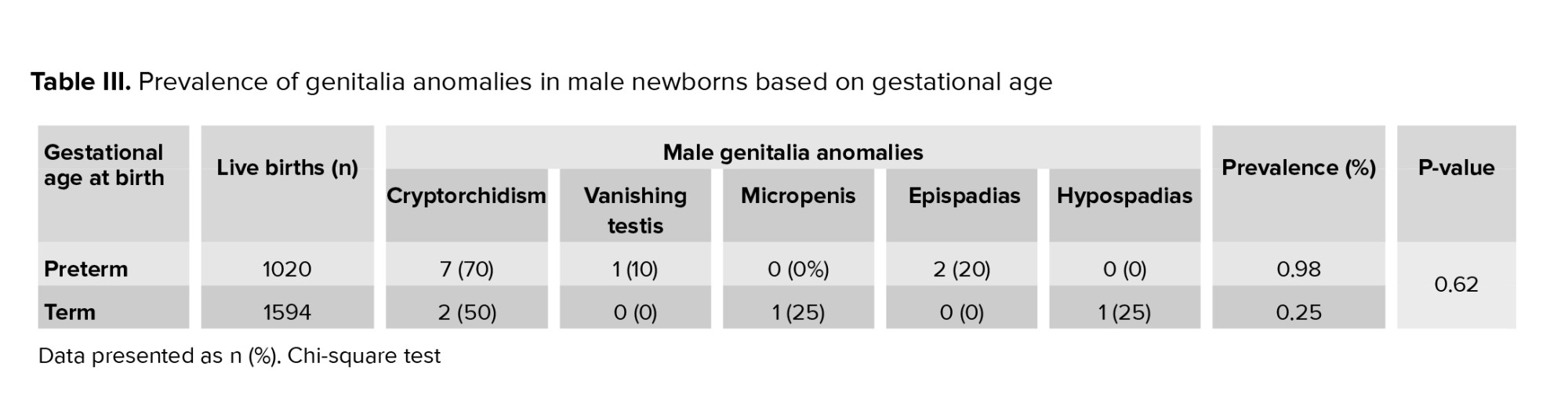
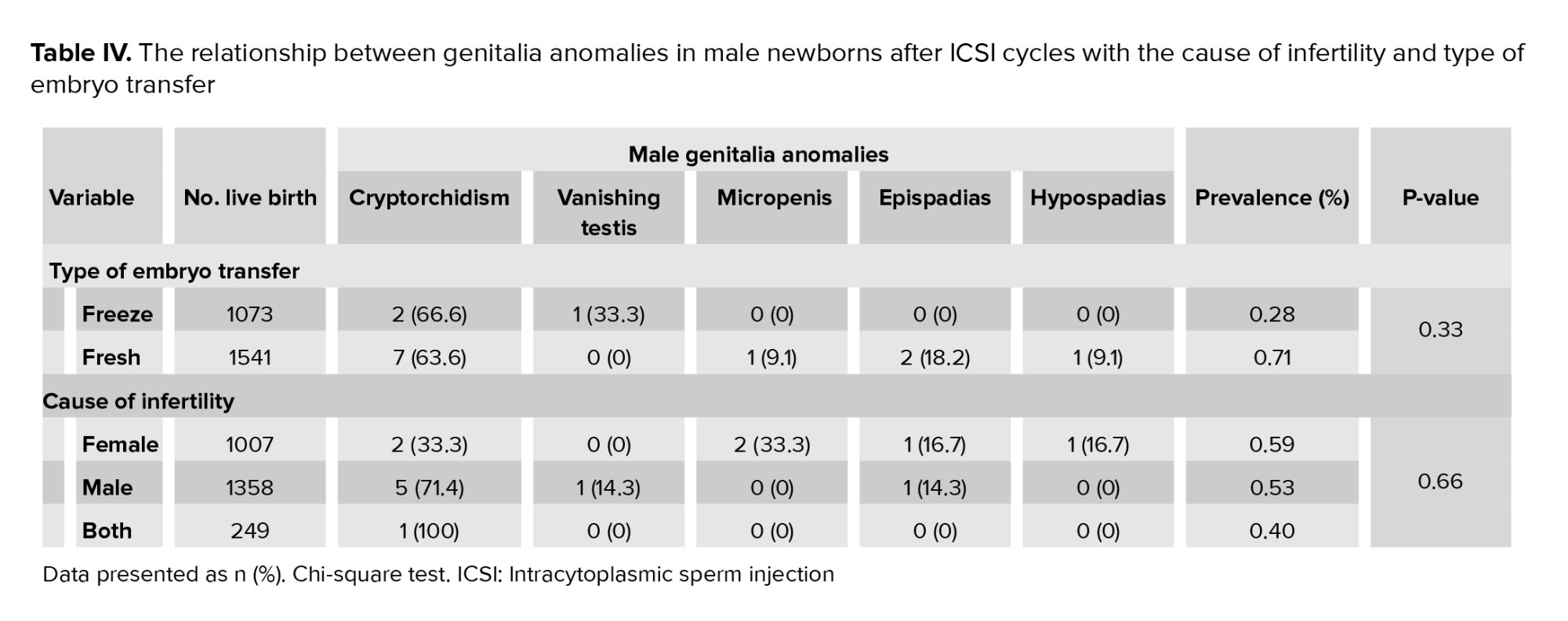
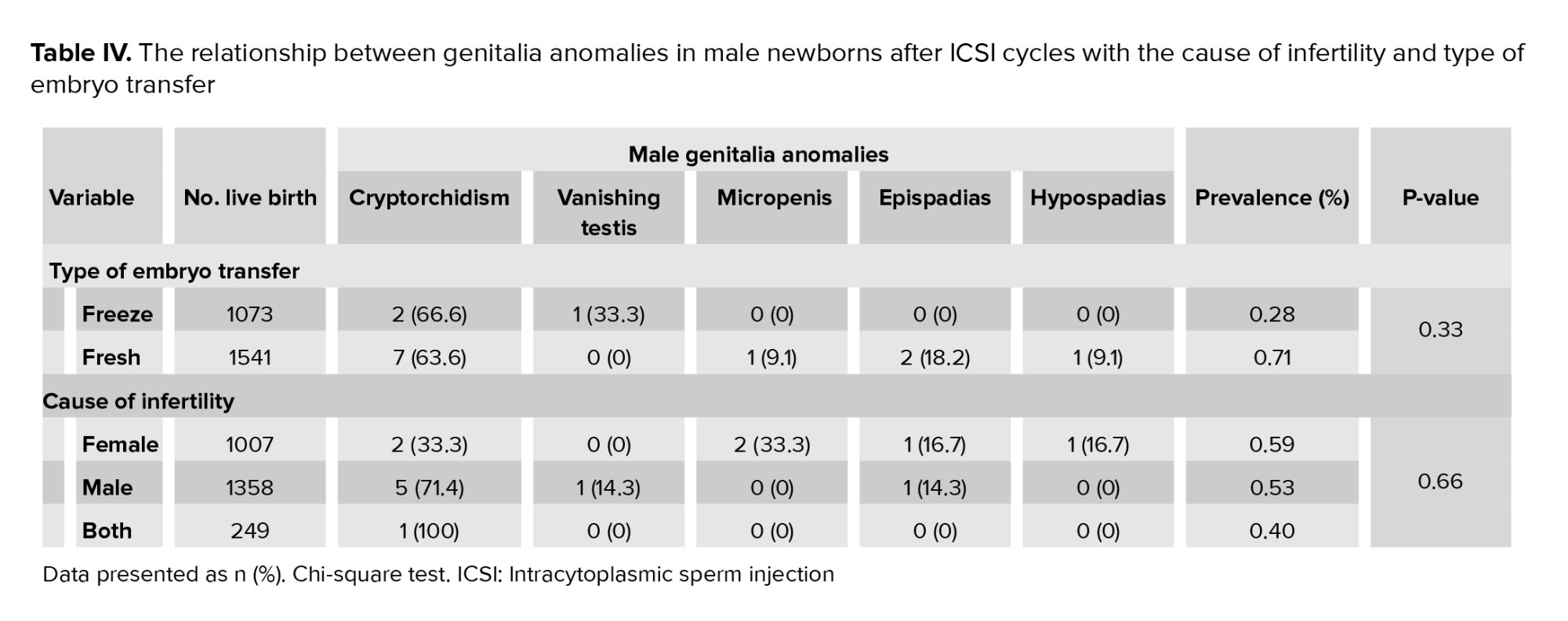
Table IV shows the relationship between the cause of infertility and the type of embryo transfer and male genital anomalies. With fresh embryo transfer, the prevalence of genital anomalies was 0.71%. The Chi-square test showed that the relationship between the prevalence of genitalia anomalies and the type of embryo transfer was not statistically significant (p = 0.33). The Chi-square test demonstrated that the relationship between the prevalence of male genitalia anomalies and the causes of infertility was not statistically significant (p = 0.66). Out of 1582 male infants, with male infertility caused by their father, only 351 were diagnosed with azoospermia. In the following, out of 14 infants with male genitalia anomalies, 6 infants had a history of mild or moderate male infertility without an azoospermia diagnosis or surgery for sperm retrieval in their father (Table IV). As a result, no significant link was discovered between azoospermia diagnosis and male genital anomalies in newborns following ICSI cycles.
4. Discussion
Epidemiological research on the distribution of various male genitalia malformation in children conceived by ART was the first fundamental step in the current study. In many parts of the world, extensive studies have been performed. Recently, in a meta-analysis study, a significant association between congenital abnormalities and ART cycles which imposes a tremendous burden on global health was reported (2). Despite these extensive studies, there is limited research on male and female genitalia malformation in Iran due to the lack of integrated electronic information of individuals’ medical records. We chose to study genitalia anomalies because the genitalia system is the target of most hormonal drugs used in treatment cycles. In addition, the underlying causes of infertility are maternal and/or paternal reproductive system disorders.
In the present study, various genitalia anomalies had the following prevalences: cryptorchidism (0.34%), hypospadias (0.038%), micropenis (0.038%), vanishing testis (0.038%), and epispadias (0.077%). Due to our limitations, these children were almost entirely examined by pediatricians at the hospital's birth center. The information collected was obtained from the parents via telephone and by assessment of medical records.
In the current study, the prevalence of cryptorchidism was 0.16% (9 out of 5608 live births) and 0.34% in boys. The prevalence of this disease was 0.2% in preterm neonates and 0.09% in term infants, which is approximately 20 times higher in premature infants and is consistent with the physiopathology description of this disease. The prevalence of cryptorchidism was 4.5% in live births from natural pregnancies, approximately 30% in premature infants, and 3.4% in term newborns. The difference in the prevalence of these 2 categories is that the normal time of testicular decline is between 28 and 32 wk of gestation. Although the cause of the testicle decline and its main mechanism is still unknown, it is undoubtedly affected by 2 hormonal changes, androgens and Müllerian-inhibiting substance (21). In another study in Yazd, the prevalence of cryptorchidism in preterm and mature infants was reported as 29.5% and 3.27%, respectively (22). Mozafari Kermani and colleagues (15) studied the children who resulted from IVF or ICSI and reported a 0.5% prevalence of cryptorchidism. Similarly, a systematic review and meta-analysis determined that the prevalence of cryptorchidism in children born by ICSI was 0.53%, and concluded that there was no significant difference compared to the general population regarding this congenital anomaly (9). We found similar results with previous studies; however, a recent meta-analysis in China concluded that ART was correlated with an increased risk of congenital urinary tract malformation in offspring, especially cryptorchidism (1.83 times more) (17).
The prevalence of hypospadias was reported in 3-5 cases in 1000 natural live births (0.3-0.5%). The prevalence of hypospadias in Asia was reported to be 69 in 10,000 (0.69%) (23). Other research estimated the incidence of hypospadias as 0.38% in those born by ICSI, which did not significantly increase in the general population (9). In agreement with previous studies, the prevalence of hypospadias in the present study was 0.017%, one in 5608 cases of total births and 0.038% in male births. The average birth weight in the present study was 2890.3 gr, and the rates of LBW and premature infants were 34.4% and 61.4%, respectively. It seems that the cryptorchidism and hypospadias in children conceived by ART are due to LBW, and prematurity and male factor infertility do not correlate with an increase in the prevalence of these diseases in neonates. However, in a recent mate-analysis research reported that ART was correlated with an increased risk of hypospadias in offspring (1.87 times more) (17).
The prevalence of epispadias at birth for the whole spectrum is reported at 1 in 10,000, which ranges from 1 in 30,000 (0.003%) for classical bladder exstrophy to 1 in 200,000 for exstrophy of the cloaca, with an overall more significant proportion of affected males (24). However, in the current study, the prevalence of this anomaly was 0.035% in total live births and 0.077% in males. Compared to the mentioned prevalence, the rate of epispadias in live births after ICSI was 10 times more than reported previously in live births from natural conception. Unfortunately, there is no accurate epidemiologic study on the prevalence of this congenital anomaly in natural live births in Iran to compare. However, these reports may indicate the need for further studies on the association of ART and this anomaly and examine other types of extrophy in these children. This finding was consistent with the results of Zwink and colleagues who suggested that ART treatments such as IVF and ICSI are associated with an increased risk of the exstrophy-epispadias complex. However, it is unclear whether they are caused by ART therapy per se or based on the infertility etiology or parents' characteristics (25).
In our study, the incidence of micropenis was 0.017%. Elsewhere, in northeastern Brazil incidence of micropenis (18 cases among 2710 newborns) was reported as 0.66% (26). Unfortunately, this prevalence is not available in the natural live births in Iran for comparison and further discussion.
The only strength of this study is the first report of the prevalence of male genitalia malformations after ICSI cycles in Iran. However, this study has some limitations that should be mentioned. One limitation was that in our institute, the treatment cycles were defined as IVF/ICSI cycles and ICSI cycles. Since in the IVF/ICSI cycles, it was not determined whether the fetus was the result of IVF or ICSI procedure, and the IVF cycle alone is not a routine at Royan Institute; however a non-ICSI group for comparison was not available. In addition, it was not possible to collect the clinical characteristics and information of babies from natural pregnancies for the researchers. Therefore, we compared our results with the prevalence of these anomalies in natural pregnancies reported in the published scientific articles.
5. Conclusion
The results of the study indicated that the prevalence of each male urogenital anomalies including cryptorchidism, hypospadias, micropenis, and vanishing after the ICSI cycle was rare and less than 0.5%, and almost similar to those in infants from natural pregnancies which reported in Iranian scientific literature; however, we had no control group for better comparison. Therefore, a prospective study with a control group should confirm the present results.
Acknowledgments
We would like to thank all of the participants and the coworkers at Royan Institute, Tehran, Iran, especially Mrs. Reihani and Mrs. Zolfaghary for their assistance in this study. There was no financial support and no conflict of interest to declare.
Conflict of Interest
There are no conflict of interest to declare.
Full-Text: (342 Views)
1. Introduction
During the past 4 decades, assisted reproductive technology (ART) has been used as a standard worldwide medical practice to achieve pregnancy. ART is responsible for an estimated 1-5.9% of conceptions in some developed countries (1). In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) are the 2 main ART modalities. Because sperm and oocytes are manipulated outside the body, there are concerns regarding embryos derived from these invasive procedures (2). The findings of several studies and meta-analyses indicate that ART is associated with an increased risk of congenital anomalies (1-5). Results of previous studies have suggested an association between ART and some specific cardiac birth defects (6, 7), as well as some noncardiac defects such as cleft lip with or without cleft palate (8); hypospadias (9, 10), neural tube defects (11), esophageal, anorectal (8, 12), genitourinary defects (13), and large intestinal atresias (12). However, the magnitude of these associations and the spectrum of the involved defects remains unknown (14).
Presumed reasons to explain the higher risk of congenital malformations (CM) in ART infants include underlying subfertility, medications for ovulation induction, micromanipulation in ICSI and/or IVF, as well as increase in multiple gestations and prematurity (14). More CM have been observed in ICSI as a more invasive treatment method in cases where sperm could not pass through the natural route and physiologic deletion of abnormal sperms does not occur (oligospermia) (15). Similar interventions applied in IVF include the gonadotropin stimulator, oocyte aspiration, and culture media, which likely raise the incidence of CM (15). Some studies have investigated whether there is a higher risk of CM in offspring conceived by ICSI than IVF. However, they reported controversial results (9, 15-17). It was hypothesized that congenital genitourinary malformations, such as hypospadias, are more frequent after ICSI than after IVF. Moreover, they stated that there is a lack of robust data due to the rarity of these conditions (9). Hence, it was concluded that the increased prevalence of congenital genitourinary malformations was observed in singletons born after ART; however, more studies are warranted for confirmation (17). Only one study in Iran evaluated congenital anomalies and could not find a significant relationship between the type of infertility treatments and CM; however, the rate of CM after the ICSI cycles (11.7%) was slightly higher than after IVF cycles (5.9%) (15).
The developmental effect of ART on infants remains an important subject that needs further monitoring and investigation. This cross-sectional study with the retrospective design was done to evaluate the prevalence rate of congenital anomalies, particularly male genital malformations, in offspring conceived by ICSI at Royan Institute.
2. Materials and Methods
This cross-sectional study was performed at Royan Institute, Tehran, Iran from April 2013-December 2015. After registering the ICSI cycles in Hakim's software system at Royan Institute, data regarding pregnancies were investigated, and all live births were monitored and followed retrospectively. The ICSI cycles and embryo transfer procedure were performed with standard protocols at Royan Institute. We collected the data regarding the cause of infertility and type of embryo transfer from participants’ records. The characteristics of newborns were also collected and recorded from the follow-up clinic. Gestational age was determined as 14 days before oocyte pick-up until delivery. To exclude outliers, only children with gestational ages between 22 and 44 wk and birth weight between 400 and 7000 gr were included. Preterm birth was considered as delivery before 37 completed weeks of gestation. Low-birth weight (LBW) was defined as 2500 gr and very LBW as 1500 gr (18).
All children were assessed at birth by neonatologists and the premature infants were reevaluated at the expected date of delivery. The diagnosis of the genital anomaly was determined on the basis of the clinical examination at the expected date of delivery. Sonography was performed if the anomaly was not diagnosed by a physical exam. A diagnosis of hypospadias was made as a failure of fusion of the urethra was observed, and the urethral meatus was ectopically located. Cryptorchidism could not be diagnosed if the testis was in the inguinal canal or not palpable. Testis in a high scrotal position was not considered to be cryptorchidism (19). Micropenis was described as a penis 2.5 standard deviations (SD) smaller than the mean for the child's age and race. It was diagnosed by observing a stretched penis length of less than 1.9 centimeters at birth. Testicular regression syndrome or vanishing testis is reported to be due to the subsequent atrophy and disappearance in the fetal life of an initially normal testis, and its diagnosis is confirmed by surgery (20). Epispadias was defined by observing the opening of the urethra in the back of the penis (19).
2.1. Ethical considerations
The study was approved by the Institutional Review Boards and the Ethical Committees of Royan Institute, Tehran, Iran (Code: IR.ACECR.ROYAN.REC.1397.207). The patients' file information has been used while maintaining the confidentiality of names, and oral consent has been obtained from all participants.
2.2. Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences 20.0 (SPSS; SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to evaluate the normality of continuous variables. Normally distributed continuous variables are presented as mean (SD). Comparison of means for dichotomous variables was performed by the independent sample t test, and the Chi-square test was used to examine the relationship between categorical variables. A p-value < 0.05 was considered to be statistically significant.
3. Results
In this study, 4409 infertile couples with successful pregnancies after ICSI cycles were investigated to examine the male urogenital anomalies in their newborns. The mean age of fathers and mothers was 35.58 ± 5.64 yr and 30.86 ± 4.92 yr. Out of 4409 pregnancies, 3202 pregnancies (72.6%) were single, 1109 pregnancies (25.2%) twin, and 98 pregnancies (2.2%) triple. In total, the all-out number of live births were 5608. Of the 4409 couples studied, 1762 couples (39.9%) had female infertility, 2194 couples (49.8%) had male infertility, and 453 couples (10.3%) had both male and female infertility factors. The mean gestational age at delivery was 36.3 ± 3.2 wk. Of 5608 live births, 2152 (38.4%) were preterm and 3456 (61.6%) had normal weight. Of 5608 live births, 2614 newborns were male (46.61%), and the remaining (2994 newborns) were female. The demographic and clinical characteristics of the participating couples are shown in table I.
Out of 2614 male newborns, only 14 (0.54%) had urogenital anomalies. As seen in table II, the highest prevalence of genitalia anomalies were related to cryptorchidism [9 (0.34%)]. The lowest prevalence of genitalia anomalies were related to hypospadias, micropenis, and vanishing testis [1 (0.038%)].
Table III shows the prevalence of genitalia anomalies based on gestational age in male newborns. The highest prevalence of genitalia anomalies was related to preterm (< 37 wk) newborns (0.98%). The most common anomaly was cryptorchidism (7 cases from 10 anomalies). The prevalence of genitalia anomalies in male term newborns (> 37 wk) was 0.25%. The total prevalence of genitalia anomalies by gestational age in male newborns was 0.54%. The Chi-square test showed that the relationship between the prevalence of male genitalia anomalies and the gestational age was not statistically significant (p = 0.62).
Table IV shows the relationship between the cause of infertility and the type of embryo transfer and male genital anomalies. With fresh embryo transfer, the prevalence of genital anomalies was 0.71%. The Chi-square test showed that the relationship between the prevalence of genitalia anomalies and the type of embryo transfer was not statistically significant (p = 0.33). The Chi-square test demonstrated that the relationship between the prevalence of male genitalia anomalies and the causes of infertility was not statistically significant (p = 0.66). Out of 1582 male infants, with male infertility caused by their father, only 351 were diagnosed with azoospermia. In the following, out of 14 infants with male genitalia anomalies, 6 infants had a history of mild or moderate male infertility without an azoospermia diagnosis or surgery for sperm retrieval in their father (Table IV). As a result, no significant link was discovered between azoospermia diagnosis and male genital anomalies in newborns following ICSI cycles.
4. Discussion
Epidemiological research on the distribution of various male genitalia malformation in children conceived by ART was the first fundamental step in the current study. In many parts of the world, extensive studies have been performed. Recently, in a meta-analysis study, a significant association between congenital abnormalities and ART cycles which imposes a tremendous burden on global health was reported (2). Despite these extensive studies, there is limited research on male and female genitalia malformation in Iran due to the lack of integrated electronic information of individuals’ medical records. We chose to study genitalia anomalies because the genitalia system is the target of most hormonal drugs used in treatment cycles. In addition, the underlying causes of infertility are maternal and/or paternal reproductive system disorders.
In the present study, various genitalia anomalies had the following prevalences: cryptorchidism (0.34%), hypospadias (0.038%), micropenis (0.038%), vanishing testis (0.038%), and epispadias (0.077%). Due to our limitations, these children were almost entirely examined by pediatricians at the hospital's birth center. The information collected was obtained from the parents via telephone and by assessment of medical records.
In the current study, the prevalence of cryptorchidism was 0.16% (9 out of 5608 live births) and 0.34% in boys. The prevalence of this disease was 0.2% in preterm neonates and 0.09% in term infants, which is approximately 20 times higher in premature infants and is consistent with the physiopathology description of this disease. The prevalence of cryptorchidism was 4.5% in live births from natural pregnancies, approximately 30% in premature infants, and 3.4% in term newborns. The difference in the prevalence of these 2 categories is that the normal time of testicular decline is between 28 and 32 wk of gestation. Although the cause of the testicle decline and its main mechanism is still unknown, it is undoubtedly affected by 2 hormonal changes, androgens and Müllerian-inhibiting substance (21). In another study in Yazd, the prevalence of cryptorchidism in preterm and mature infants was reported as 29.5% and 3.27%, respectively (22). Mozafari Kermani and colleagues (15) studied the children who resulted from IVF or ICSI and reported a 0.5% prevalence of cryptorchidism. Similarly, a systematic review and meta-analysis determined that the prevalence of cryptorchidism in children born by ICSI was 0.53%, and concluded that there was no significant difference compared to the general population regarding this congenital anomaly (9). We found similar results with previous studies; however, a recent meta-analysis in China concluded that ART was correlated with an increased risk of congenital urinary tract malformation in offspring, especially cryptorchidism (1.83 times more) (17).
The prevalence of hypospadias was reported in 3-5 cases in 1000 natural live births (0.3-0.5%). The prevalence of hypospadias in Asia was reported to be 69 in 10,000 (0.69%) (23). Other research estimated the incidence of hypospadias as 0.38% in those born by ICSI, which did not significantly increase in the general population (9). In agreement with previous studies, the prevalence of hypospadias in the present study was 0.017%, one in 5608 cases of total births and 0.038% in male births. The average birth weight in the present study was 2890.3 gr, and the rates of LBW and premature infants were 34.4% and 61.4%, respectively. It seems that the cryptorchidism and hypospadias in children conceived by ART are due to LBW, and prematurity and male factor infertility do not correlate with an increase in the prevalence of these diseases in neonates. However, in a recent mate-analysis research reported that ART was correlated with an increased risk of hypospadias in offspring (1.87 times more) (17).
The prevalence of epispadias at birth for the whole spectrum is reported at 1 in 10,000, which ranges from 1 in 30,000 (0.003%) for classical bladder exstrophy to 1 in 200,000 for exstrophy of the cloaca, with an overall more significant proportion of affected males (24). However, in the current study, the prevalence of this anomaly was 0.035% in total live births and 0.077% in males. Compared to the mentioned prevalence, the rate of epispadias in live births after ICSI was 10 times more than reported previously in live births from natural conception. Unfortunately, there is no accurate epidemiologic study on the prevalence of this congenital anomaly in natural live births in Iran to compare. However, these reports may indicate the need for further studies on the association of ART and this anomaly and examine other types of extrophy in these children. This finding was consistent with the results of Zwink and colleagues who suggested that ART treatments such as IVF and ICSI are associated with an increased risk of the exstrophy-epispadias complex. However, it is unclear whether they are caused by ART therapy per se or based on the infertility etiology or parents' characteristics (25).
In our study, the incidence of micropenis was 0.017%. Elsewhere, in northeastern Brazil incidence of micropenis (18 cases among 2710 newborns) was reported as 0.66% (26). Unfortunately, this prevalence is not available in the natural live births in Iran for comparison and further discussion.
The only strength of this study is the first report of the prevalence of male genitalia malformations after ICSI cycles in Iran. However, this study has some limitations that should be mentioned. One limitation was that in our institute, the treatment cycles were defined as IVF/ICSI cycles and ICSI cycles. Since in the IVF/ICSI cycles, it was not determined whether the fetus was the result of IVF or ICSI procedure, and the IVF cycle alone is not a routine at Royan Institute; however a non-ICSI group for comparison was not available. In addition, it was not possible to collect the clinical characteristics and information of babies from natural pregnancies for the researchers. Therefore, we compared our results with the prevalence of these anomalies in natural pregnancies reported in the published scientific articles.
5. Conclusion
The results of the study indicated that the prevalence of each male urogenital anomalies including cryptorchidism, hypospadias, micropenis, and vanishing after the ICSI cycle was rare and less than 0.5%, and almost similar to those in infants from natural pregnancies which reported in Iranian scientific literature; however, we had no control group for better comparison. Therefore, a prospective study with a control group should confirm the present results.
Acknowledgments
We would like to thank all of the participants and the coworkers at Royan Institute, Tehran, Iran, especially Mrs. Reihani and Mrs. Zolfaghary for their assistance in this study. There was no financial support and no conflict of interest to declare.
Conflict of Interest
There are no conflict of interest to declare.
Type of Study: Original Article |
Subject:
Assisted Reproductive Technologies
References
1. Qin J, Sheng X, Wang H, Liang D, Tan H, Xia J. Assisted reproductive technology and risk of congenital malformations: A meta-analysis based on cohort studies. Arch Gynecol Obstet 2015; 292: 777-798. [DOI:10.1007/s00404-015-3707-0]
2. Chen L, Yang T, Zheng Z, Yu H, Wang H, Qin J. Birth prevalence of congenital malformations in singleton pregnancies resulting from in vitro fertilization/intracytoplasmic sperm injection worldwide: A systematic review and meta-analysis. Arch Gynecol Obstet 2018; 297: 1115-1130. [DOI:10.1007/s00404-018-4712-x]
3. Wen J, Jiang J, Ding C, Dai J, Liu Y, Xia Y, et al. Birth defects in children conceived by in vitro fertilization and intracytoplasmic sperm injection: A meta-analysis. Fertil Steril 2012; 97: 1331-1337. [DOI:10.1016/j.fertnstert.2012.02.053]
4. Hansen M, Kurinczuk JJ, Milne E, de Klerk N, Bower C. Assisted reproductive technology and birth defects: A systematic review and meta-analysis. Hum Reprod Update 2013; 19: 330-353. [DOI:10.1093/humupd/dmt006]
5. Yin L, Hang F, Gu L-J, Xu B, Ma D, Zhu G-J. Analysis of birth defects among children 3 years after conception through assisted reproductive technology in China. Birth Defects Res A Clin Mol Teratol 2013; 97: 744-749. [DOI:10.1002/bdra.23116]
6. Giorgione V, Parazzini F, Fesslova V, Cipriani S, Candiani M, Inversetti A, et al. Congenital heart defects in IVF/ICSI pregnancy: Systematic review and meta-analysis. Ultrasound Obstet Gynecol 2018; 51: 33-42. [DOI:10.1002/uog.18932]
7. Tararbit K, Lelong N, Houyel L, Bonnet D, Goffinet F, Khoshnood B, et al. Assessing the role of multiple pregnancies in the association between tetralogy of Fallot and assisted reproductive techniques: A path-analysis approach. Orphanet J Rare Dis 2014; 9: 1750-1752. [DOI:10.1186/1750-1172-9-27]
8. Reefhuis J, Honein MA, Schieve LA, Correa A, Hobbs CA, Rasmussen SA. Assisted reproductive technology and major structural birth defects in the United States. Hum Reprod 2009; 24: 360-366. [DOI:10.1093/humrep/den387]
9. Massaro PA, MacLellan DL, Anderson PA, Romao RLP. Does intracytoplasmic sperm injection pose an increased risk of genitourinary congenital malformations in offspring compared to in vitro fertilization? A systematic review and meta-analysis. J Urol 2015; 193: 1837-1842. [DOI:10.1016/j.juro.2014.10.113]
10. Bang JK, Lyu SW, Choi J, Lee DR, Yoon TK, Song S-H. Does infertility treatment increase male reproductive tract disorder? Urology 2013; 81: 644-648. [DOI:10.1016/j.urology.2012.12.003]
11. Benedum CM, Yazdy MM, Parker SE, Mitchell AA, Werler MM. Association of clomiphene and assisted reproductive technologies with the risk of neural tube defects. Am J Epidemiol 2016; 183: 977-987. [DOI:10.1093/aje/kwv322]
12. Boulet SL, Kirby RS, Reefhuis J, Zhang Y, Sunderam S, Cohen B, et al. Assisted reproductive technology and birth defects among liveborn infants in Florida, Massachusetts, and Michigan, 2000-2010. JAMA Pediatr 2016; 170: e154934. [DOI:10.1001/jamapediatrics.2015.4934]
13. Luke B, Brown MB, Wantman E, Forestieri NE, Browne ML, Fisher SC, et al. The risk of birth defects with conception by ART. Hum Reprod 2021; 36: 116-129. [DOI:10.1093/humrep/deaa272]
14. Liberman RF, Getz KD, Heinke D, Luke B, Stern JE, Declercq ER, et al. Assisted reproductive technology and birth defects: Effects of subfertility and multiple births. Birth Defects Res 2017; 109: 1144-1153. [DOI:10.1002/bdr2.1055]
15. Mozafari Kermani R, Nedaeifard L, Nateghi MR, Shahzadeh Fazeli A, Ahmadi E, Osia MA, et al. Congenital anomalies in infants conceived by assisted reproductive techniques. Arch Iran Med 2012; 15: 228-231.
16. Fedder J, Loft A, Parner ET, Rasmussen S, Pinborg A. Neonatal outcome and congenital malformations in children born after ICSI with testicular or epididymal sperm: A controlled national cohort study. Hum Reprod 2013; 28: 230-240. [DOI:10.1093/humrep/des377]
17. Zhang Z, Liu X, Wei C, Luo J, Shi Y, Lin T, et al. Assisted reproductive technologies and the risk of congenital urogenital tract malformations: A systematic review and meta-analysis. J Pediatr Urol 2021; 17: 9-20. [DOI:10.1016/j.jpurol.2020.11.005]
18. Cunningham G, Leveno KJ, Bloom SL, Spong CY, Dashe JS. Williams obstetrics. 24th Ed. USA: Mcgraw-hill; 2014.
19. Shepard CL, Gayheart DT, Joseph DB. Male genitourinary system. in: Tubbs RS, Shoja MM, Loukas M. Bergman's comprehensive encyclopedia of human anatomic variation. USA: Wiley Online Library; 2016. [DOI:10.1002/9781118430309.ch115]
20. Nataraja RM, Yeap E, Healy CJ, Nandhra IS, Murphy FL, Hutson JM, et al. Presence of viable germ cells in testicular regression syndrome remnants: Is routine excision indicated? A systematic review. Pediatr Surg Int 2018; 34: 353-361. [DOI:10.1007/s00383-017-4206-0]
21. Singh R, Singh K. Male infertility: Understanding, causes and treatment. Singapore: Springer; 2017. [DOI:10.1007/978-981-10-4017-7]
22. Amooei A, Kargar S. Prevalence and pathological features of cryptorchidism among Iranian children in Yazd province, central Iran. Int J Pediatr 2018; 6: 7615-7621.
23. Delnord M, Blondel B, Zeitlin J. What contributes to disparities in the preterm birth rate in European countries? Curr Opin Obstet Gynecol 2015; 27: 133-142. [DOI:10.1097/GCO.0000000000000156]
24. Ebert AK, Zwink N, Reutter HM, Jenetzky E. A prevalence estimation of exstrophy and epispadias in Germany from public health insurance data. Front Pediatr 2021; 9: 648414. [DOI:10.3389/fped.2021.648414]
25. Zwink N, Jenetzky E, Hirsch K, Reifferscheid P, Schmiedeke E, Schmidt D, et al. Assisted reproductive techniques and risk of exstrophy-epispadias complex: A German case-control study. J Urol 2013; 189: 1524-1529. [DOI:10.1016/j.juro.2012.11.108]
26. Gaspari L, Sampaio DR, Paris F, Audran F, Orsini M, Neto JB, et al. High prevalence of micropenis in 2710 male newborns from an intensive‐use pesticide area of Northeastern Brazil. Int J Androl 2012; 35: 253-264. [DOI:10.1111/j.1365-2605.2011.01241.x]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





