Tue, Feb 24, 2026
[Archive]
Volume 23, Issue 8 (August 2025)
IJRM 2025, 23(8): 637-646 |
Back to browse issues page
Ethics code: IR.SSU.AEC.1401.011
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fotoohi-Ardakani G, Ghasemi N, Hassanpour Dehnavi A, Dadbinpour A, Lotfi M. Impact of platelet-rich plasma at different concentrations on genes of apoptotic pathway and differentiation of stem cells in cyclophosphamide-induced ovarian failure in a mouse model: An experimental study. IJRM 2025; 23 (8) :637-646
URL: http://ijrm.ir/article-1-3577-en.html
URL: http://ijrm.ir/article-1-3577-en.html
Gholamreza Fotoohi-Ardakani1 

 , Nasrin Ghasemi2
, Nasrin Ghasemi2 

 , Azam Hassanpour Dehnavi3
, Azam Hassanpour Dehnavi3 

 , Ali Dadbinpour4
, Ali Dadbinpour4 

 , Marzieh Lotfi *5
, Marzieh Lotfi *5 




 , Nasrin Ghasemi2
, Nasrin Ghasemi2 

 , Azam Hassanpour Dehnavi3
, Azam Hassanpour Dehnavi3 

 , Ali Dadbinpour4
, Ali Dadbinpour4 

 , Marzieh Lotfi *5
, Marzieh Lotfi *5 


1- Department of Molecular Medicine, School of Advanced Technologies in Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2- Abortion Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Department of Anatomical Sciences, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Department of Medical Genetics, Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. & Genetics and Environmental Hazards Research Center, Abarkouh School of Medical Sciences, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
5- Department of Molecular Medicine, Abortion Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,M.lotfi@ssu.ac.ir
2- Abortion Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3- Department of Anatomical Sciences, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4- Department of Medical Genetics, Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. & Genetics and Environmental Hazards Research Center, Abarkouh School of Medical Sciences, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
5- Department of Molecular Medicine, Abortion Research Center, Yazd Reproductive Sciences Institute, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. ,
Full-Text [PDF 1986 kb]
(575 Downloads)
| Abstract (HTML) (573 Views)
Full-Text: (77 Views)
1. Introduction
Premature ovarian failure (POF) affects 1% of women in the general population. POF is a medical condition that affects women under the age of 40 who experience hormonal imbalances and decreased fertility (1, 2). The condition is characterized by a decrease in estrogen levels and an increase in gonadotropin levels. POF etiology is multifactorial, encompassing chromosomal and genetic abnormalities, autoimmune disorders, infection, surgery, radiation, and chemotherapy (3).
Alkylating drugs for cancer treatment, such as cyclophosphamide (CTX), have detrimental effects on the female reproductive system and decrease ovarian function. CTX primary actions include the suppression of DNA synthesis and function, as well as the DNA damage and production. By inhibiting angiogenesis and inducing apoptosis, CTX has been shown to reduce the number of primitive follicles, oocytes, and granulosa cells on eggs, thereby causing ovarian atrophy (4, 5).
Hormone and stem cell therapy, and most recently, platelet-rich plasma (PRP) are current therapeutic methods for POF. PRP is composed of growth factors including vascular endothelial growth factor, transforming growth factor beta, hepatocyte growth factor, insulin-like growth factor-1, growth differentiation factor-9, bone morphogenetic protein 15, and epidermal growth factor found in the person's own blood. It can stimulate tissue regeneration at the cellular level because of its high concentration of growth factors (6, 7). PRP has been shown to promote and expedite alopecia, wound healing, scar repair, skeletal muscle, and skin regeneration (6).
Many studies suggest that PRP components promote ovarian follicle survival and growth (8, 9). Finally, PRP shows promise as a novel therapy to rejuvenate failing ovarian tissue and improve outcomes for women with POF (10).
However, because this procedure is still in the early stages of study, understanding the parameters that can enhance the PRP's impact on ovarian tissue cells proliferation is crucial (11). Also, considering that the platelet density varies in various studies in ovarian rejuvenation, finding the optimal platelet density is very important for increasing the efficiency of platelets (12, 13).
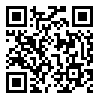
This study aims to find the optimal concentration of PRP in ovarian function and to identify the mechanism of PRP effect in ovarian tissue repair through evaluating the expression of apoptosis genes B-cell lymphoma 2 (BCL-2) and Bcl-2–associated X protein (BAX) and octamer-binding transcription factor 4 (OCT4), efficient in ovarian stem cell differentiation in a mouse model of POF caused by CTX.
2. Materials and Methods
2.1. Animals
This study was conducted at the Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. In this experimental study, female Syrian mice (8-10 wk old, 25-30 gr) were used. Mice were kept in a cage with temperature control, a 12-hr light/dark cycle, and free access to water and food ad libitum. Mice randomly divided into 5 groups (n = 6/each).
Premature ovarian failure (POF) affects 1% of women in the general population. POF is a medical condition that affects women under the age of 40 who experience hormonal imbalances and decreased fertility (1, 2). The condition is characterized by a decrease in estrogen levels and an increase in gonadotropin levels. POF etiology is multifactorial, encompassing chromosomal and genetic abnormalities, autoimmune disorders, infection, surgery, radiation, and chemotherapy (3).
Alkylating drugs for cancer treatment, such as cyclophosphamide (CTX), have detrimental effects on the female reproductive system and decrease ovarian function. CTX primary actions include the suppression of DNA synthesis and function, as well as the DNA damage and production. By inhibiting angiogenesis and inducing apoptosis, CTX has been shown to reduce the number of primitive follicles, oocytes, and granulosa cells on eggs, thereby causing ovarian atrophy (4, 5).
Hormone and stem cell therapy, and most recently, platelet-rich plasma (PRP) are current therapeutic methods for POF. PRP is composed of growth factors including vascular endothelial growth factor, transforming growth factor beta, hepatocyte growth factor, insulin-like growth factor-1, growth differentiation factor-9, bone morphogenetic protein 15, and epidermal growth factor found in the person's own blood. It can stimulate tissue regeneration at the cellular level because of its high concentration of growth factors (6, 7). PRP has been shown to promote and expedite alopecia, wound healing, scar repair, skeletal muscle, and skin regeneration (6).
Many studies suggest that PRP components promote ovarian follicle survival and growth (8, 9). Finally, PRP shows promise as a novel therapy to rejuvenate failing ovarian tissue and improve outcomes for women with POF (10).
However, because this procedure is still in the early stages of study, understanding the parameters that can enhance the PRP's impact on ovarian tissue cells proliferation is crucial (11). Also, considering that the platelet density varies in various studies in ovarian rejuvenation, finding the optimal platelet density is very important for increasing the efficiency of platelets (12, 13).
This study aims to find the optimal concentration of PRP in ovarian function and to identify the mechanism of PRP effect in ovarian tissue repair through evaluating the expression of apoptosis genes B-cell lymphoma 2 (BCL-2) and Bcl-2–associated X protein (BAX) and octamer-binding transcription factor 4 (OCT4), efficient in ovarian stem cell differentiation in a mouse model of POF caused by CTX.
2. Materials and Methods
2.1. Animals
This study was conducted at the Faculty of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. In this experimental study, female Syrian mice (8-10 wk old, 25-30 gr) were used. Mice were kept in a cage with temperature control, a 12-hr light/dark cycle, and free access to water and food ad libitum. Mice randomly divided into 5 groups (n = 6/each).
- Normal control
- POF + phosphate buffered saline (PBS)
- POF + PRP 0.25 ml/kg (X)
- POF + PRP 0.5 ml/kg (2X)
- POF + PRP 1 ml/kg (4X)
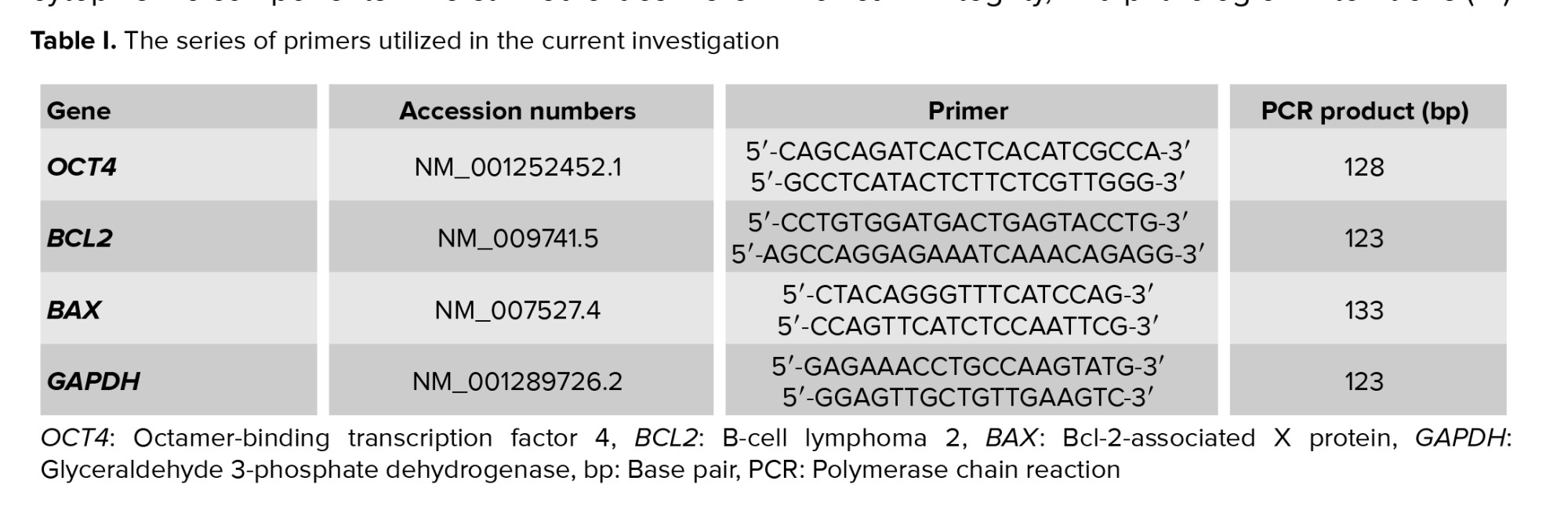
The POF model was established by administering a 50 mg/kg loading dose of CTX via intraperitoneal (IP) injection to female mice, followed by 15 consecutive days of the same dosage (14). PRP was injected into infertile mice on day 21st after model creation. 3 doses of PRP were selected to determine which dose of PRP was more effective in POF mice.
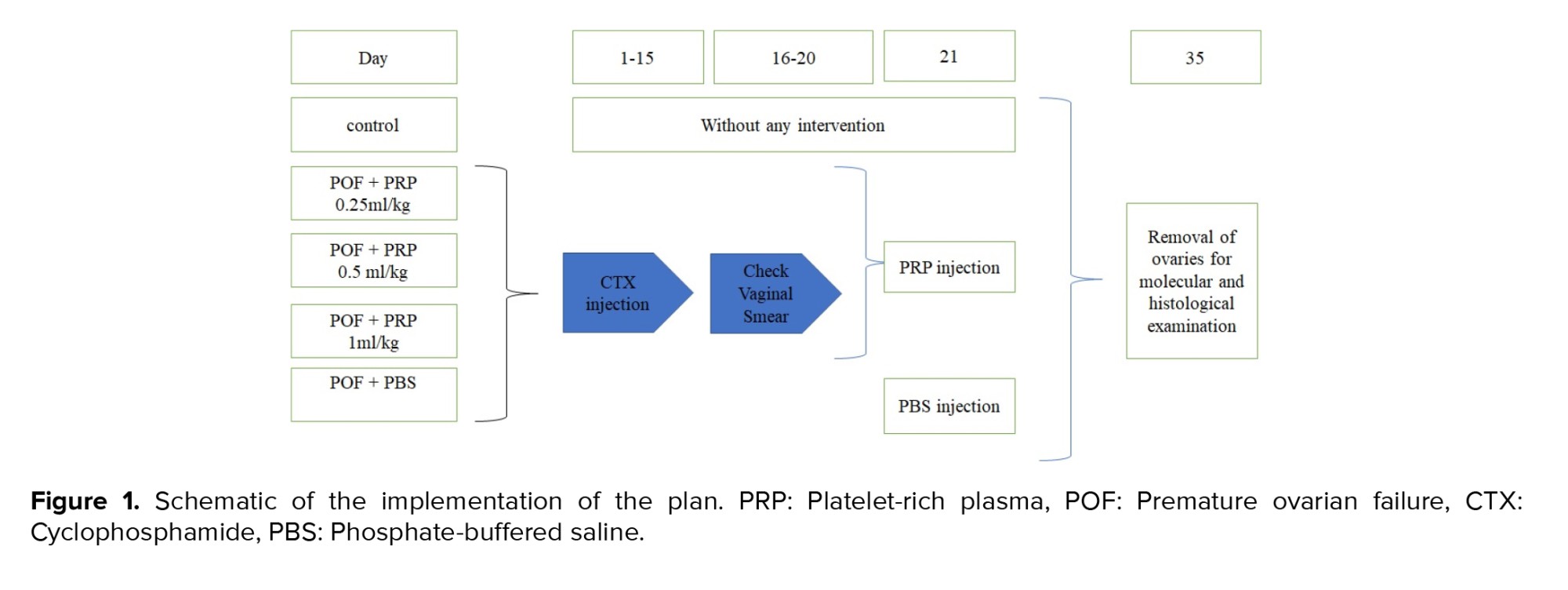
The normal control received no injection; the POF + PBS group received only PBS injection (150 μL); the POF + PRP X group received PRP 0.25 ml/kg; the POF + PRP 2X group received PRP 0.5 ml/kg; and the POF + PRP 4X group received PRP 1 ml/kg (Figure 1). IP injection was performed on both of the ovaries.
On the 35th day, mice were administered IP with 50 mg of ketamine and 7 mg/kg Xylazine and were anesthetized. After removal of the ovaries, the right ovary was placed in formalin for histological examination, and the left ovary was placed in RNAlater (Yekta Tajhiz, Iran) and stored at -80°C.
2.2. PRP preparation
PRP is produced by 2 centrifugation steps. Blood sample from the hearts of male mice was collected into tubes containing the anticoagulant sodium citrate. The supernatant was centrifuged at 1800 g for 8 min, then transferred to a separate tube and centrifuged again at 1000 g for 10 min. The upper layer of poor PRP was discarded, and platelet count in PRP was performed using the Sysmax device kx21.
2.3. Model proof
To investigate the establishment of a POF model in mice following CTX injection, vaginal smears were collected and analyzed over a period of 7 consecutive days to monitor estrous cycle patterns.
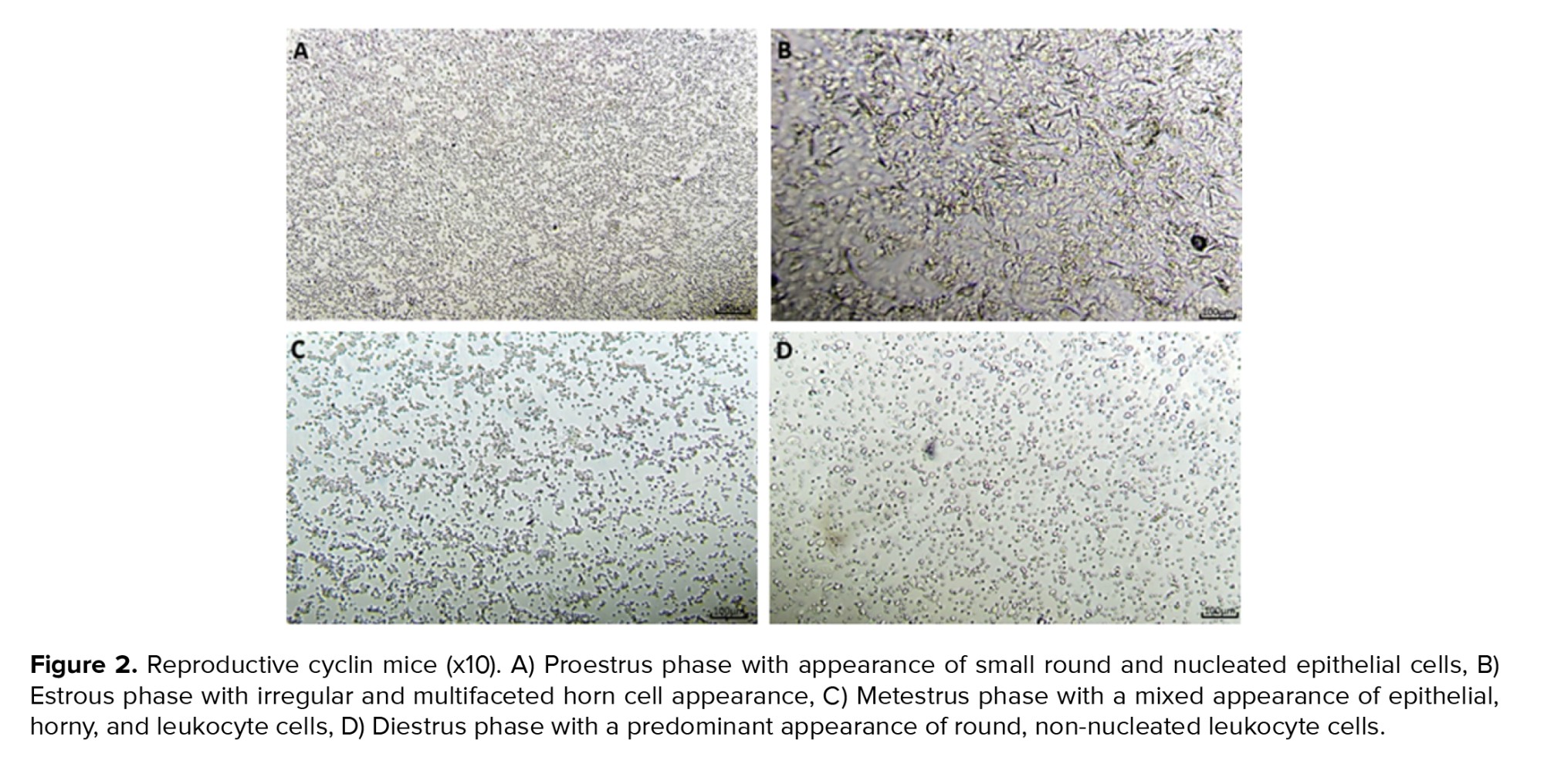
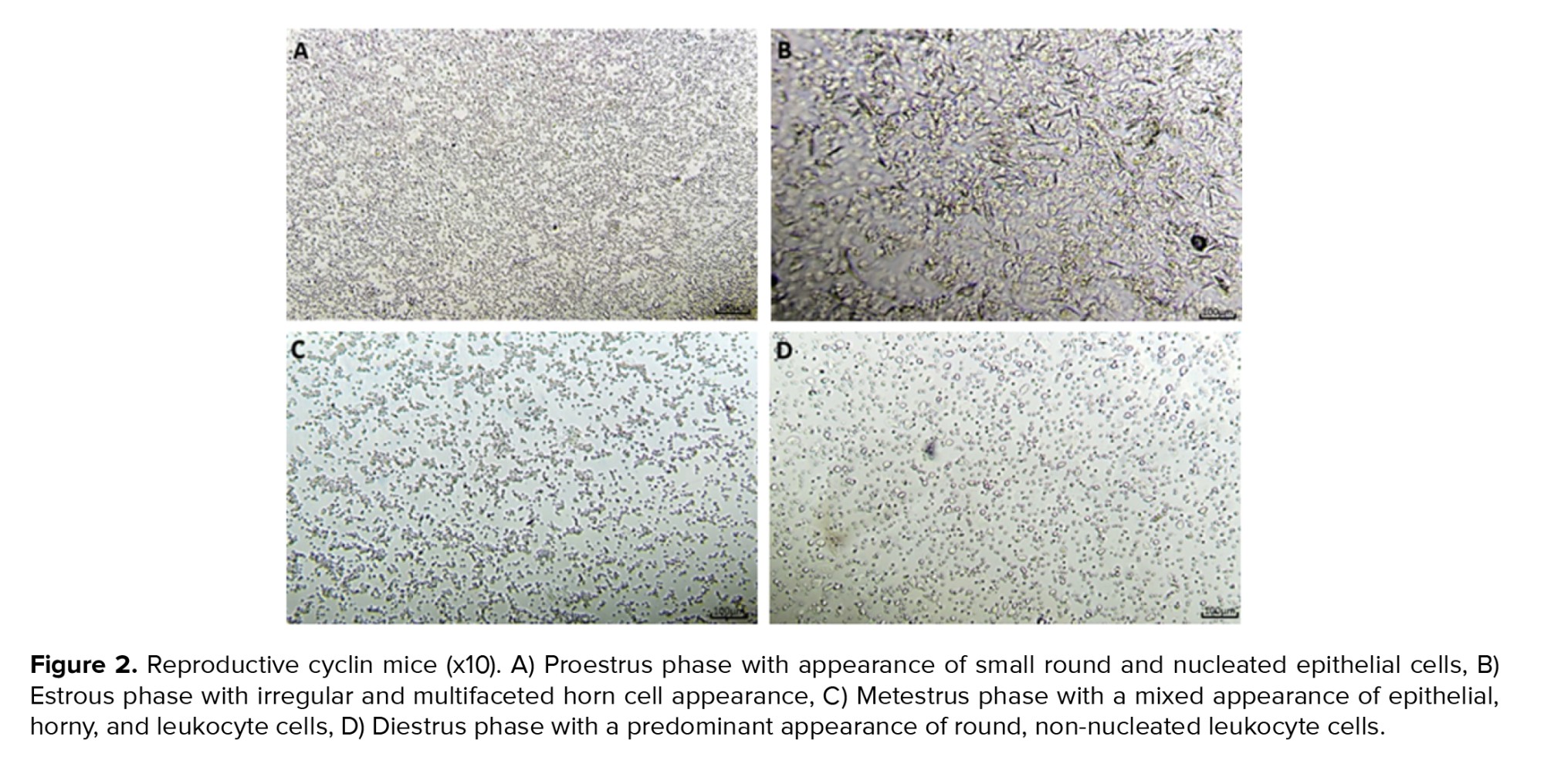
Detailed examination of vaginal smear samples revealed distinct differences between the control and POF groups. In the control group, estrous cycles were observed to be regular, occurring rhythmically every 4-5 days and consisting of 4 distinct, continuous, and sequential phases: proestrus, estrus, metestrus, and diestrus (Figure 2). In contrast, mice in the POF groups exhibited marked irregularities in their estrous cycles throughout the experimental period. The estrous cycles in these groups were disordered and nonrhythmic. These findings underscore the efficacy of CTX injection as a reliable method for inducing POF in mice, as demonstrated by the consistent disruption of normal estrous cyclicity. The interruption of estrous cycles demonstrates that the POF model has been successfully created in mice (Figure 2D).
2.4. Quantitative real-time polymerase chain reaction (PCR)
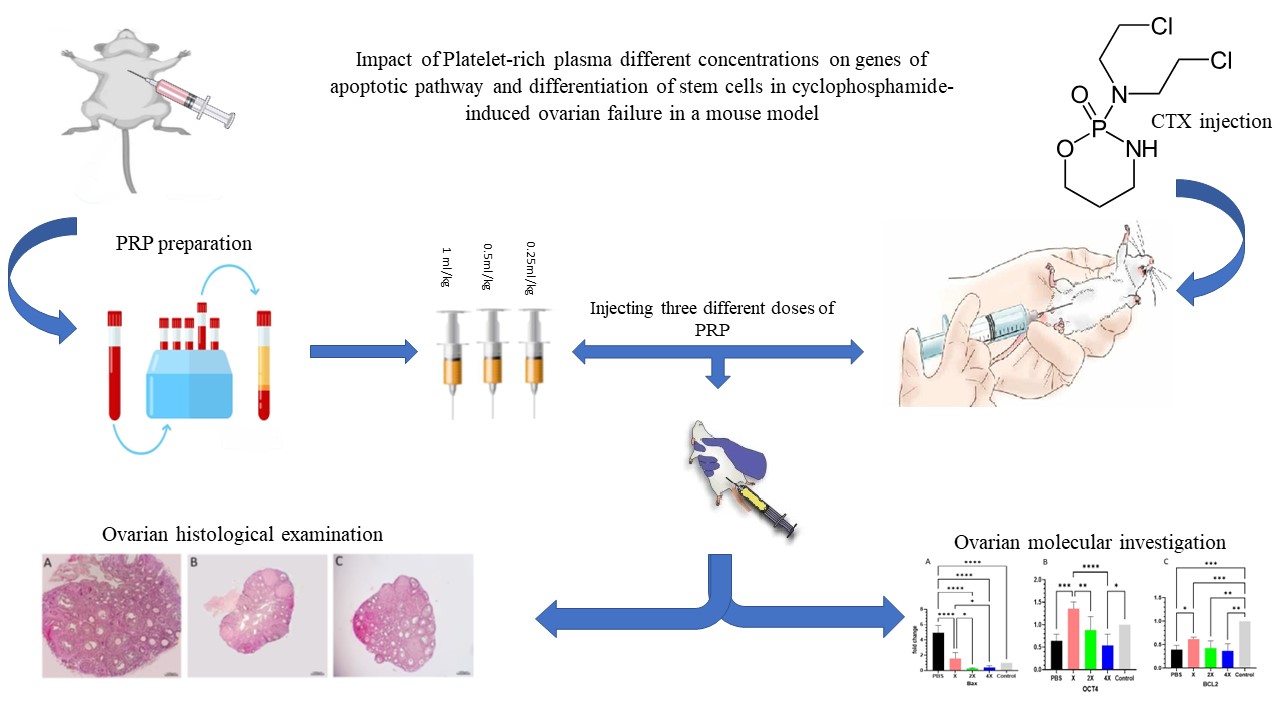
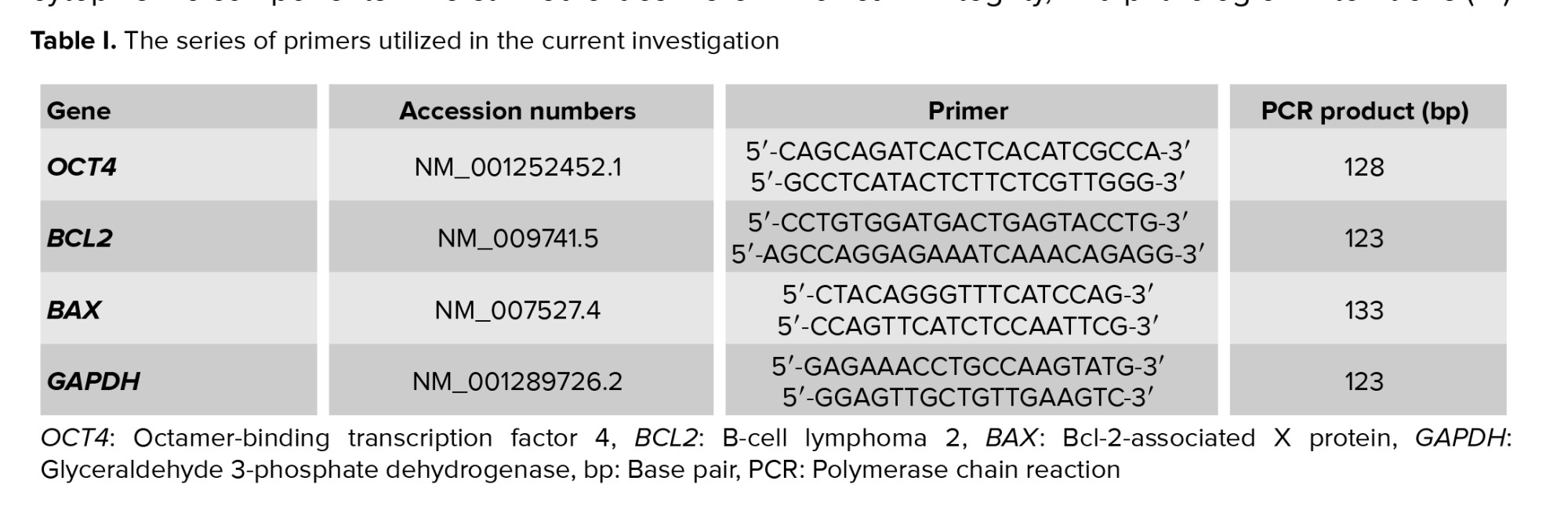
RNA extraction kit (Parstous Co., Iran) was used to extract total RNA from ovarian tissue, and cDNA was subsequently synthesized with another kit from the same manufacturer. Gene expression analysis was performed through SYBR Green-based real-time PCR (Ampliqon, Denmark) using the StepOne™ system (Applied Biosystems, USA). Primers were designed using Primer3 software, as detailed in table I, and their efficiency was validated. To normalize gene expression levels, the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) gene was used as a housekeeping reference. The relative expression of target genes was calculated using the 2-ΔΔCT method.
2.5. Histopathological examination
Following 24 hr of fixation in 10% buffered formalin, ovarian tissues were preserved in a pH-stabilized solution to prevent degradation. After adequate fixation, samples were carefully embedded in paraffin blocks, providing essential structural support for precise sectioning. Thin serial sections, each 4 µm thick, were prepared using a microtome, ensuring uniformity for histological evaluation. To facilitate microscopic examination of cellular architecture, sections underwent standard hematoxylin and eosin (H&E) staining, enhancing contrast between nuclear and cytoplasmic components. The stained slides were then analyzed using light microscopy, allowing detailed assessment of ovarian morphology, follicular integrity, and pathological alterations (15).
2.6. Ethical Considerations
Every experiment was authorized by the Ethics Committee of the Shahid Sadoughi University of Medical Sciences in Yazd, Iran (Code: IR.SSU.AEC.1401.011). All experiments were performed in accordance with the ARRIVE guidelines.
2.7. Statistical Analysis
The data collected in this study included both numerical and categorical variables. Numerical data are presented as the mean ± standard deviation, while categorical data are presented as frequencies and percentages. To assess the normality of the numerical data, the Kolmogorov-Smirnov test was used. For variables that did not have a normal distribution, the Mann-Whitney U test was used to compare groups. A one-way ANOVA was used to compare means between multiple groups. Statistical significance was determined using p-value (p < 0.05). Statistical analyses were performed using GraphPad Prism 9.0 and SPSS 25.0 for Windows.
3. Results
3.1. POF mouse model
We successfully developed a POF mouse model via IP injection of CTX. Following injection, experimental mice exhibited an irregular estrous cycle characterized by prolonged estrus and proestrus phases, and less frequent metestrus and diestrus phases, compared to pre-injection cycles (Figure 2).
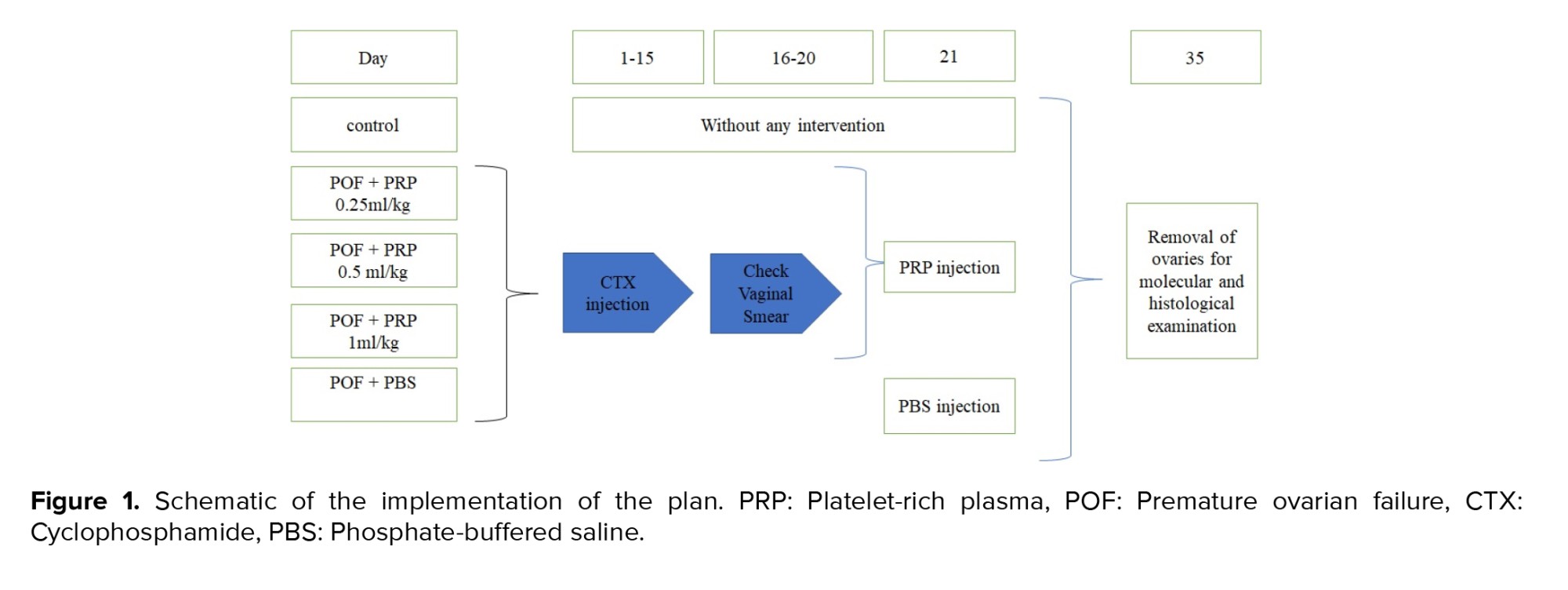
3.2. Ovarian histology
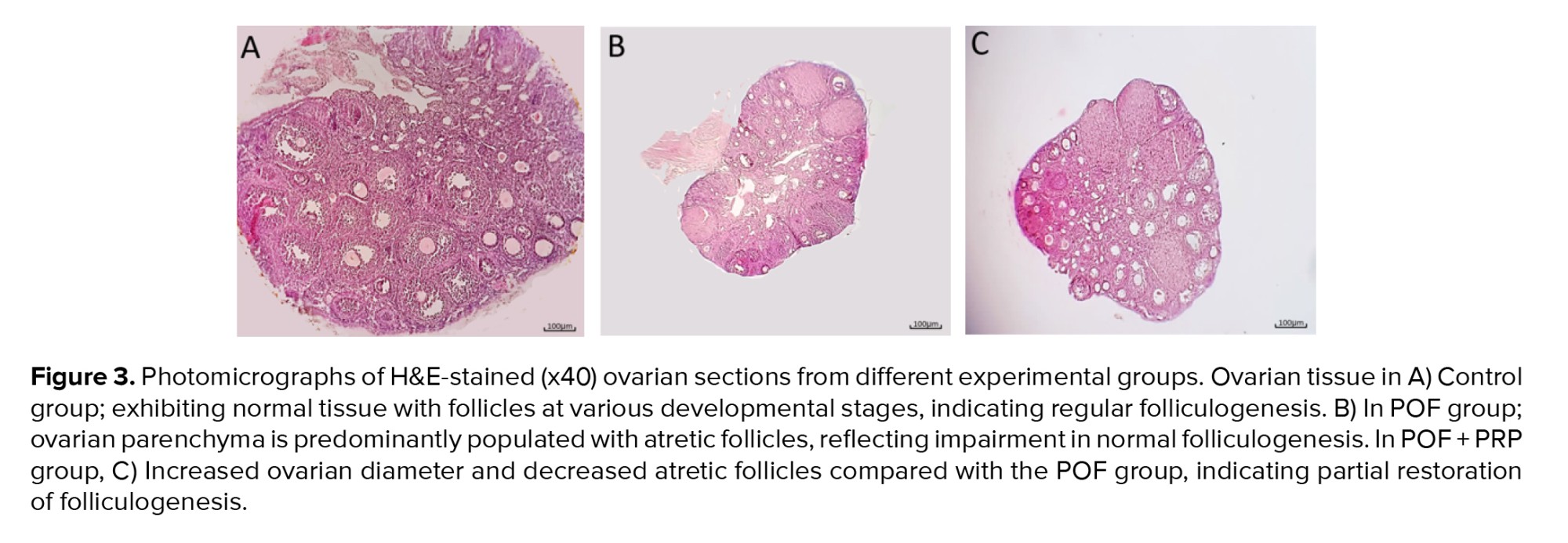
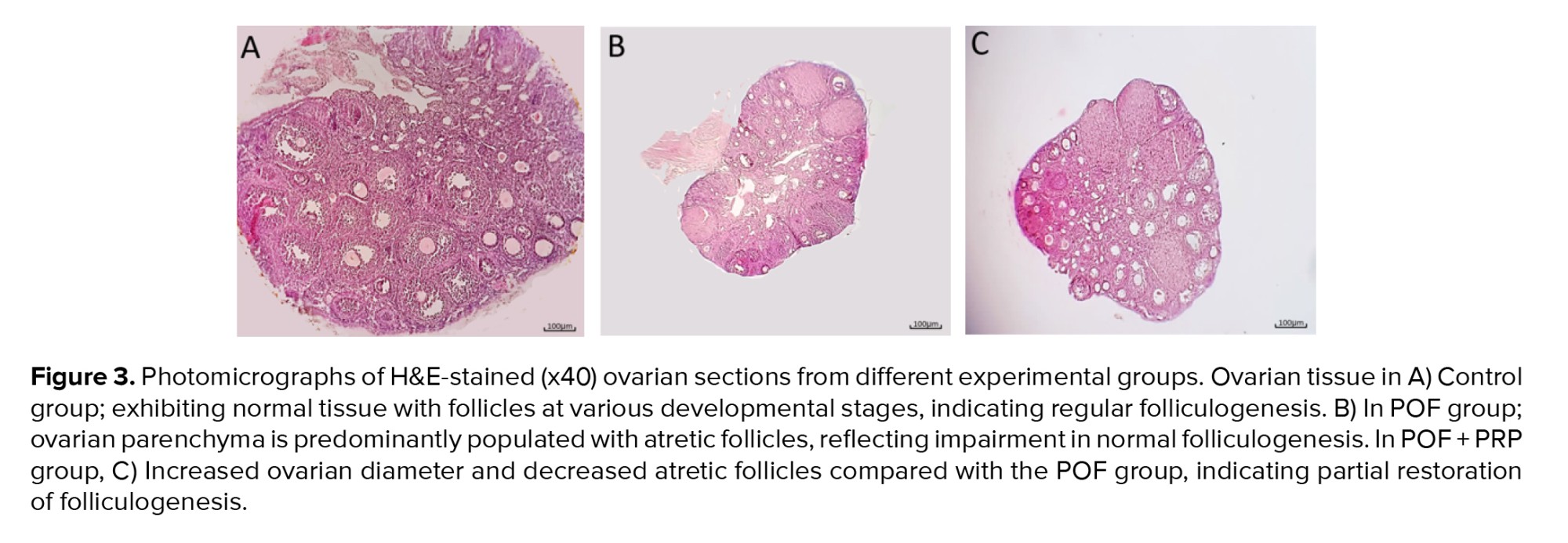
Ovarian histological examination revealed distinct differences between the experimental groups. In the control group (Figure 3A), the normal ovarian structure was preserved, with active and natural folliculogenesis observed throughout the tissue. The follicles at various stages of development, including primordial, primary, secondary, and antral follicles, were evident, confirming normal ovarian function.
In contrast, the POF + PBS group’s (Figure 3B) histopathological evaluation demonstrated disrupted ovarian morphology characterized by extensive follicular atresia and a significant decrease in healthy follicular structures. Folliculogenesis was largely arrested, consistent with the pathological features of POF.
The treatment groups receiving PRP exhibited dose-dependent improvements in ovarian morphology and function. In the POF + PRP 0.25 ml/kg group, only mild recovery was observed, with limited follicular activation and persistent atretic follicles.
The POF + PRP 0.5 ml/kg group showed moderate restoration of ovarian histology, as evidenced by a decrease in the number of atretic follicles and partial resumption of folliculogenesis.
The POF + PRP 1 ml/kg group (Figure 3C) exhibited the most substantial histological recovery, with ovarian tissue morphology closely resembling that of the control group. A significant increase in the number of healthy, developing follicles was observed across various stages, along with a marked reduction in follicular atresia. These findings suggest a pronounced therapeutic effect of PRP at higher dosages in ameliorating ovarian damage and promoting follicular regeneration.
3.3. RNA quality control
A NanoDrop spectrophotometer was utilized to assess the purity of the RNA, and the A260/A280 and A260/A230 ratios were utilized to identify various impurities. A260/A280 ratios ranging from 1.8-2.0 were considered pure RNA. A260/A280 ratios more than or less than 1.8 showed DNA or protein contamination. The acceptable range of A260/A230 ratio was 1.8-2.2.
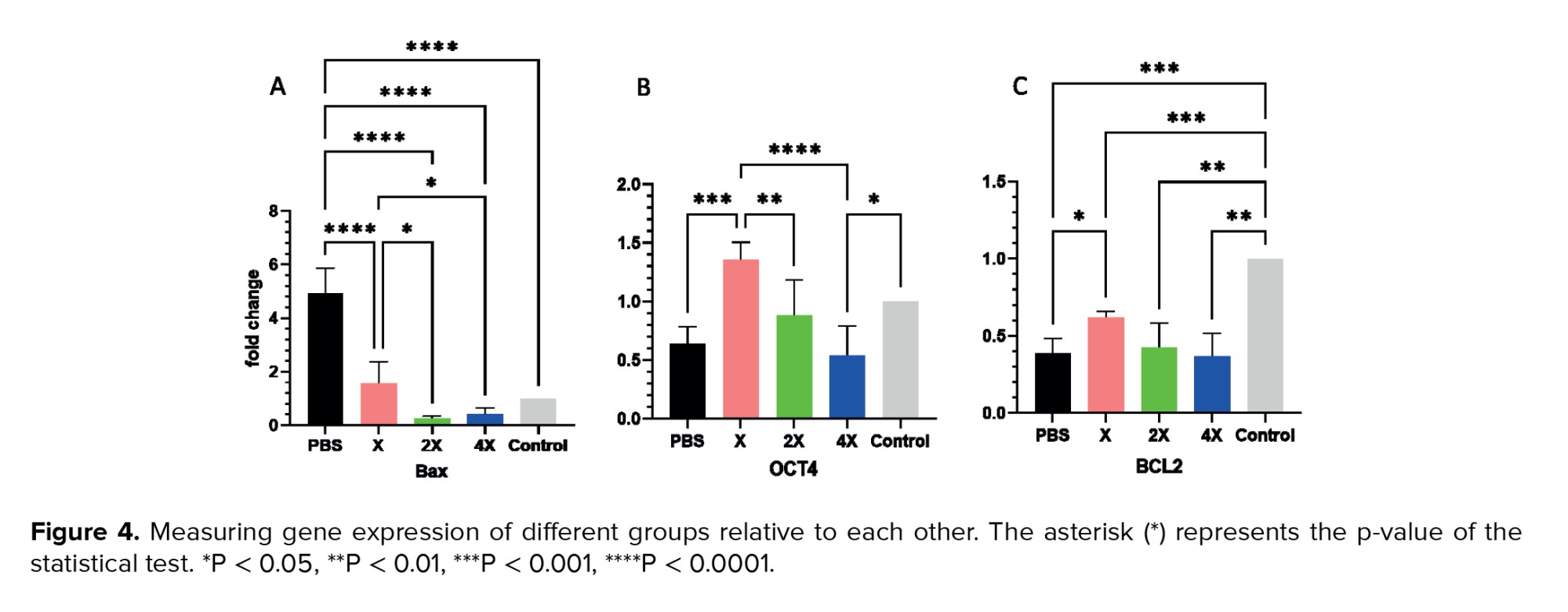
3.4. Expression level of OCT4, B-cell lymphoma 2 (BCL2), and BAX
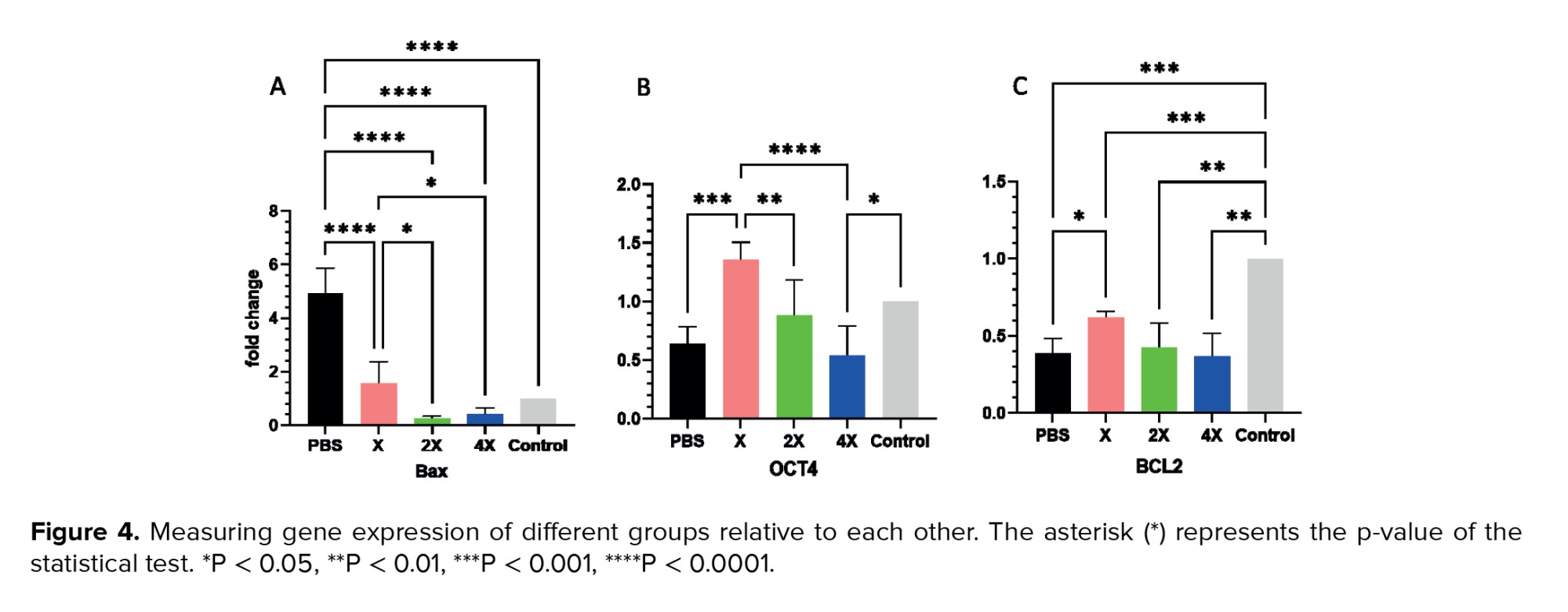
The expression levels of genes, including OCT4, BCL2, and BAX, were analyzed in all groups. In comparison to the PBS group, the BAX gene expression level was considerably lower in the PRP group overall (p < 0.0001) (Figure 4A). OCT4 gene expression in the PRP group X was significantly different from the PBS group (p < 0.001) (Figure 4B). Moreover, there was a significant increase in BCL2 gene expression in the PRP group X compared to the PBS group (p < 0.05) (Figure 4C).
4. Discussion
Folliculogenesis arrest or ovarian follicle depletion is common in women under 40 (16, 17). POF can result from various factors, such as stress and chemotherapy drugs (17). CTX and busulfan are commonly used chemotherapeutic drugs in the POF animal model (18). PRP ovarian injections may regenerate and improve ovarian function by releasing growth factors, potentially benefiting ovarian failure. A lot of research has been done on the effects of PRP on POF patients (10, 19, 20). The current study attempted to examine the protective impact of 3 PRP dosages against the destructive effect of CTX on ovarian tissue and possible pathways that caused the improvement of the ovary by examining the expression of proapoptotic and antiapoptotic genes and investigating the differentiation gene.
Platelet concentration directly correlates with the growth factors they release to tissues (21, 22). The concentration of 1,000,000 platelets in a 5 mL volume of plasma has been shown to promote bone and soft-tissue healing; as a result, this definition is frequently used to describe therapeutic PRP (23). PRP can stimulate ovarian function by 2 pathways: inhibition of apoptosis or stimulation of germ cells in ovary (24, 25). The pro-apoptotic BCL2 gene expression levels were considerably lower in the current investigation, and anti-apoptotic gene BAX was significantly increased, which indicates high apoptosis in the ovary in the POF group (Figure 4A, C). Additionally, it was shown that the POF mice treated with CTX had a considerably smaller number of primary, secondary, and antral follicles than the control group (Figure 3A, B).
A study showed decreased primary, secondary, and antral follicles in POF mice compared with controls based on histopathological analysis. POF + PRP group increased the number of primary and antral follicles significantly in comparison to the POF group, which is consistent with our study (26).
Developing alternative therapies is key to restoring ovarian function. Platelets and growth factors are abundant in PRP, which is isolated from peripheral blood (10). The results of experiments on POF rats have shown that PRP promotes presinusoidal follicle development (27). However, the fundamental mechanism remains unknown. In the present study, the expression level of pro-apoptotic BCL2 genes in the PRP X group showed a significant increase compared to the PBS group, indicating the effect of PRP in increasing anti-apoptotic gene expression and improving ovarian function, while in the 2X and 4X groups, no statistically significant difference was observed (Figure 4C).
It can be concluded that lower concentrations of PRP have a greater effect on increasing anti-apoptotic gene expression. Yuan et al. made a significant observation that the combination of G-CSF-mobilized peripheral blood mononuclear cells (PBMCs) with PRP resulted in the restoration of ovarian function in rats that were subjected to chemotherapy-induced POF through the use of CTX. This combination therapy worked by effectively activating the estrous cycle, which is a critical component of reproductive health, alongside restoring the levels of essential sex hormones that are vital for normal ovarian function. Furthermore, the treatment led to the generation of preantral follicles, which are important for the ovarian reserve, following the administration of CTX. This finding underscores the potential of using PBMCs and PRP as a therapeutic strategy to counteract the adverse effects of chemotherapy on ovarian health. The mobilized PBMC/PRP combination outperformed PBMCs and PRP alone. The mobilized PBMC/PRP combination greatly decreased granulosa cell mortality by lowering pro-apoptotic BAX and increasing anti-apoptotic BCL-2 genes (28).
A study showed that treatment of human granulosa cells with PRP significantly reduced apoptosis and increased cell viability compared to untreated cells. Real-time PCR analysis showed that PRP reduced the apoptosis factors P27 and caspase 3, while increasing the survival and proliferation-promoting genes BCL-2, phosphoinositide 3-kinase, and K-RAS (29).
In our study, the results were identical to prior studies, which caused a decrease in BAX and an increase in BCL2 genes (Figure 4A, C). Examining the expression of the pro-apoptotic BAX gene showed that the control group had a significant difference from the PBS group, that is, it caused an increase in apoptotic genes in PBS group (Figure 4A). BAX gene showed a significant reduction in the gene expression in all the groups that were treated with PRP, indicating that PRP has reduced apoptosis (Figure 4A). In the inter-group comparison, we have a significant difference between the X group, the 4X and 2X groups, this means that the increase in the number of platelets caused a much greater decrease in expression in the apoptotic BAX gene (Figure 4A).
It can be concluded that the higher platelet concentration can cause a decrease in apoptosis rate, which is related to the presence of more growth factors in platelet alpha granules. No significant difference was observed between the 2X and 4X groups, which shows that platelet density can have an inhibitory effect on the apoptosis process. El Bakly et al. used an experimental rat model of premature ovarian insufficiency established by a high-galactose diet to examine the therapeutic potential of PRP. 2 dosages (0.25 and 0.5 ml/kg) of PRP were examined to see which was more protective against toxicity. Because it produced better hormonal results, the 0.2 ml PRP volume was chosen once weekly. PRP therapy increased p70S6k and MCL-1 expression levels compared to the untreated galactose group, suggesting that apoptosis was inactive and the mammalian target of rapamycin growth signaling pathway was active (1). In our study, the findings were consistent with earlier research, which caused a decrease in apoptosis in the group receiving PRP. Comparable to our work's outcome, we had different gene expression results by changing the concentration of PRP.
Considering that in investigating the effect of platelets in the process of tissue regeneration and reconstruction, the mechanism is not fully known, and this point is still unclear whether platelets stimulate tissue regeneration by inhibiting apoptosis or by activating stem cells located in tissues that cause tissue regeneration and reconstruction. In this study, the effect of platelet density on the expression of the OCT4 gene that stimulates stem cells was investigated.
In many studies for the detection of ovarian function in POF model, the expression levels OCT4 gene was evaluated (18). OCT4 is a stem cell-specific marker gene that is a member of the transcription factors' POU domain family (30). In examining the OCT4 gene, a significant difference was observed between the X and 2X groups with the PBS group, but 4X group does not show a significant difference in OCT4 gene expression (Figure 4B). This shows that with the increase in platelet concentration, the stimulation of stem cells for growth and differentiation has increased. However, this increase in density can affect the stimulation of stem cells to an extent that at the concentration of 4X, no noticeable difference was observed in the expression of the OCT4 gene compared to the PBS group (Figure 4B). Figure 4B shows that X group concentration has a significant difference from the PBS group, which indicates that in lower concentrations, PRP can lead to the activation of stem cells. Jiang et al. used a mouse model of POF generated by CTX/busulfan to assess the protective effects of resveratrol (RES). In the meantime, the RES group showed an increase in OCT4 expression, suggesting that RES considerably and partially aided in the growth of germinal stem cells in the POF model (18).
5. Conclusion
It is worth mentioning that more studies should be done on this work and the work should be done on a larger scale. And if the result is acceptable, it should be done in the form of a case report on humans, keeping in mind the ethical considerations. Hoping that one day POF patients can be treated using PRP, which is a simple method, and there is no need for complicated treatments. Considering that in this study, the number of investigated genes from each pathway was one number, it is suggested to select more genes from each pathway for a more detailed investigation of the effect of platelet density and to identify the effective molecular pathway in ovarian tissue regeneration, and the number of mice in each group should be increased to get a more definite result.
Data Availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author Contributions
Gh. Fotoohi-Ardakani and M. Lotfi designed the study and conducted the research. M. Lotfi, and N. Ghasemi monitored, evaluated, and analyzed the result of the study. Further, Gh. Fotoohi-Ardakani, A. Dadbinpour, and A. Hassanpour Dehnavi reviewed the article. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
This article has been extracted from Ph.D. Thesis Gholamreza Fotoohi-Ardakani in Molecular Medicine, School of Advanced Technologies in Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. This study was supported by a grant from the Department of the School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran (grant number: 13399). This article does not use artificial intelligence in any way.
Conflict of Interest
The authors declare that there is no conflict of interest.
The normal control received no injection; the POF + PBS group received only PBS injection (150 μL); the POF + PRP X group received PRP 0.25 ml/kg; the POF + PRP 2X group received PRP 0.5 ml/kg; and the POF + PRP 4X group received PRP 1 ml/kg (Figure 1). IP injection was performed on both of the ovaries.
On the 35th day, mice were administered IP with 50 mg of ketamine and 7 mg/kg Xylazine and were anesthetized. After removal of the ovaries, the right ovary was placed in formalin for histological examination, and the left ovary was placed in RNAlater (Yekta Tajhiz, Iran) and stored at -80°C.
2.2. PRP preparation
PRP is produced by 2 centrifugation steps. Blood sample from the hearts of male mice was collected into tubes containing the anticoagulant sodium citrate. The supernatant was centrifuged at 1800 g for 8 min, then transferred to a separate tube and centrifuged again at 1000 g for 10 min. The upper layer of poor PRP was discarded, and platelet count in PRP was performed using the Sysmax device kx21.
2.3. Model proof
To investigate the establishment of a POF model in mice following CTX injection, vaginal smears were collected and analyzed over a period of 7 consecutive days to monitor estrous cycle patterns.
Detailed examination of vaginal smear samples revealed distinct differences between the control and POF groups. In the control group, estrous cycles were observed to be regular, occurring rhythmically every 4-5 days and consisting of 4 distinct, continuous, and sequential phases: proestrus, estrus, metestrus, and diestrus (Figure 2). In contrast, mice in the POF groups exhibited marked irregularities in their estrous cycles throughout the experimental period. The estrous cycles in these groups were disordered and nonrhythmic. These findings underscore the efficacy of CTX injection as a reliable method for inducing POF in mice, as demonstrated by the consistent disruption of normal estrous cyclicity. The interruption of estrous cycles demonstrates that the POF model has been successfully created in mice (Figure 2D).
2.4. Quantitative real-time polymerase chain reaction (PCR)
RNA extraction kit (Parstous Co., Iran) was used to extract total RNA from ovarian tissue, and cDNA was subsequently synthesized with another kit from the same manufacturer. Gene expression analysis was performed through SYBR Green-based real-time PCR (Ampliqon, Denmark) using the StepOne™ system (Applied Biosystems, USA). Primers were designed using Primer3 software, as detailed in table I, and their efficiency was validated. To normalize gene expression levels, the glyceraldehyde-3-phosphate dehydrogenase (GAPDH) gene was used as a housekeeping reference. The relative expression of target genes was calculated using the 2-ΔΔCT method.
2.5. Histopathological examination
Following 24 hr of fixation in 10% buffered formalin, ovarian tissues were preserved in a pH-stabilized solution to prevent degradation. After adequate fixation, samples were carefully embedded in paraffin blocks, providing essential structural support for precise sectioning. Thin serial sections, each 4 µm thick, were prepared using a microtome, ensuring uniformity for histological evaluation. To facilitate microscopic examination of cellular architecture, sections underwent standard hematoxylin and eosin (H&E) staining, enhancing contrast between nuclear and cytoplasmic components. The stained slides were then analyzed using light microscopy, allowing detailed assessment of ovarian morphology, follicular integrity, and pathological alterations (15).
2.6. Ethical Considerations
Every experiment was authorized by the Ethics Committee of the Shahid Sadoughi University of Medical Sciences in Yazd, Iran (Code: IR.SSU.AEC.1401.011). All experiments were performed in accordance with the ARRIVE guidelines.
2.7. Statistical Analysis
The data collected in this study included both numerical and categorical variables. Numerical data are presented as the mean ± standard deviation, while categorical data are presented as frequencies and percentages. To assess the normality of the numerical data, the Kolmogorov-Smirnov test was used. For variables that did not have a normal distribution, the Mann-Whitney U test was used to compare groups. A one-way ANOVA was used to compare means between multiple groups. Statistical significance was determined using p-value (p < 0.05). Statistical analyses were performed using GraphPad Prism 9.0 and SPSS 25.0 for Windows.
3. Results
3.1. POF mouse model
We successfully developed a POF mouse model via IP injection of CTX. Following injection, experimental mice exhibited an irregular estrous cycle characterized by prolonged estrus and proestrus phases, and less frequent metestrus and diestrus phases, compared to pre-injection cycles (Figure 2).
3.2. Ovarian histology
Ovarian histological examination revealed distinct differences between the experimental groups. In the control group (Figure 3A), the normal ovarian structure was preserved, with active and natural folliculogenesis observed throughout the tissue. The follicles at various stages of development, including primordial, primary, secondary, and antral follicles, were evident, confirming normal ovarian function.
In contrast, the POF + PBS group’s (Figure 3B) histopathological evaluation demonstrated disrupted ovarian morphology characterized by extensive follicular atresia and a significant decrease in healthy follicular structures. Folliculogenesis was largely arrested, consistent with the pathological features of POF.
The treatment groups receiving PRP exhibited dose-dependent improvements in ovarian morphology and function. In the POF + PRP 0.25 ml/kg group, only mild recovery was observed, with limited follicular activation and persistent atretic follicles.
The POF + PRP 0.5 ml/kg group showed moderate restoration of ovarian histology, as evidenced by a decrease in the number of atretic follicles and partial resumption of folliculogenesis.
The POF + PRP 1 ml/kg group (Figure 3C) exhibited the most substantial histological recovery, with ovarian tissue morphology closely resembling that of the control group. A significant increase in the number of healthy, developing follicles was observed across various stages, along with a marked reduction in follicular atresia. These findings suggest a pronounced therapeutic effect of PRP at higher dosages in ameliorating ovarian damage and promoting follicular regeneration.
3.3. RNA quality control
A NanoDrop spectrophotometer was utilized to assess the purity of the RNA, and the A260/A280 and A260/A230 ratios were utilized to identify various impurities. A260/A280 ratios ranging from 1.8-2.0 were considered pure RNA. A260/A280 ratios more than or less than 1.8 showed DNA or protein contamination. The acceptable range of A260/A230 ratio was 1.8-2.2.
3.4. Expression level of OCT4, B-cell lymphoma 2 (BCL2), and BAX
The expression levels of genes, including OCT4, BCL2, and BAX, were analyzed in all groups. In comparison to the PBS group, the BAX gene expression level was considerably lower in the PRP group overall (p < 0.0001) (Figure 4A). OCT4 gene expression in the PRP group X was significantly different from the PBS group (p < 0.001) (Figure 4B). Moreover, there was a significant increase in BCL2 gene expression in the PRP group X compared to the PBS group (p < 0.05) (Figure 4C).
4. Discussion
Folliculogenesis arrest or ovarian follicle depletion is common in women under 40 (16, 17). POF can result from various factors, such as stress and chemotherapy drugs (17). CTX and busulfan are commonly used chemotherapeutic drugs in the POF animal model (18). PRP ovarian injections may regenerate and improve ovarian function by releasing growth factors, potentially benefiting ovarian failure. A lot of research has been done on the effects of PRP on POF patients (10, 19, 20). The current study attempted to examine the protective impact of 3 PRP dosages against the destructive effect of CTX on ovarian tissue and possible pathways that caused the improvement of the ovary by examining the expression of proapoptotic and antiapoptotic genes and investigating the differentiation gene.
Platelet concentration directly correlates with the growth factors they release to tissues (21, 22). The concentration of 1,000,000 platelets in a 5 mL volume of plasma has been shown to promote bone and soft-tissue healing; as a result, this definition is frequently used to describe therapeutic PRP (23). PRP can stimulate ovarian function by 2 pathways: inhibition of apoptosis or stimulation of germ cells in ovary (24, 25). The pro-apoptotic BCL2 gene expression levels were considerably lower in the current investigation, and anti-apoptotic gene BAX was significantly increased, which indicates high apoptosis in the ovary in the POF group (Figure 4A, C). Additionally, it was shown that the POF mice treated with CTX had a considerably smaller number of primary, secondary, and antral follicles than the control group (Figure 3A, B).
A study showed decreased primary, secondary, and antral follicles in POF mice compared with controls based on histopathological analysis. POF + PRP group increased the number of primary and antral follicles significantly in comparison to the POF group, which is consistent with our study (26).
Developing alternative therapies is key to restoring ovarian function. Platelets and growth factors are abundant in PRP, which is isolated from peripheral blood (10). The results of experiments on POF rats have shown that PRP promotes presinusoidal follicle development (27). However, the fundamental mechanism remains unknown. In the present study, the expression level of pro-apoptotic BCL2 genes in the PRP X group showed a significant increase compared to the PBS group, indicating the effect of PRP in increasing anti-apoptotic gene expression and improving ovarian function, while in the 2X and 4X groups, no statistically significant difference was observed (Figure 4C).
It can be concluded that lower concentrations of PRP have a greater effect on increasing anti-apoptotic gene expression. Yuan et al. made a significant observation that the combination of G-CSF-mobilized peripheral blood mononuclear cells (PBMCs) with PRP resulted in the restoration of ovarian function in rats that were subjected to chemotherapy-induced POF through the use of CTX. This combination therapy worked by effectively activating the estrous cycle, which is a critical component of reproductive health, alongside restoring the levels of essential sex hormones that are vital for normal ovarian function. Furthermore, the treatment led to the generation of preantral follicles, which are important for the ovarian reserve, following the administration of CTX. This finding underscores the potential of using PBMCs and PRP as a therapeutic strategy to counteract the adverse effects of chemotherapy on ovarian health. The mobilized PBMC/PRP combination outperformed PBMCs and PRP alone. The mobilized PBMC/PRP combination greatly decreased granulosa cell mortality by lowering pro-apoptotic BAX and increasing anti-apoptotic BCL-2 genes (28).
A study showed that treatment of human granulosa cells with PRP significantly reduced apoptosis and increased cell viability compared to untreated cells. Real-time PCR analysis showed that PRP reduced the apoptosis factors P27 and caspase 3, while increasing the survival and proliferation-promoting genes BCL-2, phosphoinositide 3-kinase, and K-RAS (29).
In our study, the results were identical to prior studies, which caused a decrease in BAX and an increase in BCL2 genes (Figure 4A, C). Examining the expression of the pro-apoptotic BAX gene showed that the control group had a significant difference from the PBS group, that is, it caused an increase in apoptotic genes in PBS group (Figure 4A). BAX gene showed a significant reduction in the gene expression in all the groups that were treated with PRP, indicating that PRP has reduced apoptosis (Figure 4A). In the inter-group comparison, we have a significant difference between the X group, the 4X and 2X groups, this means that the increase in the number of platelets caused a much greater decrease in expression in the apoptotic BAX gene (Figure 4A).
It can be concluded that the higher platelet concentration can cause a decrease in apoptosis rate, which is related to the presence of more growth factors in platelet alpha granules. No significant difference was observed between the 2X and 4X groups, which shows that platelet density can have an inhibitory effect on the apoptosis process. El Bakly et al. used an experimental rat model of premature ovarian insufficiency established by a high-galactose diet to examine the therapeutic potential of PRP. 2 dosages (0.25 and 0.5 ml/kg) of PRP were examined to see which was more protective against toxicity. Because it produced better hormonal results, the 0.2 ml PRP volume was chosen once weekly. PRP therapy increased p70S6k and MCL-1 expression levels compared to the untreated galactose group, suggesting that apoptosis was inactive and the mammalian target of rapamycin growth signaling pathway was active (1). In our study, the findings were consistent with earlier research, which caused a decrease in apoptosis in the group receiving PRP. Comparable to our work's outcome, we had different gene expression results by changing the concentration of PRP.
Considering that in investigating the effect of platelets in the process of tissue regeneration and reconstruction, the mechanism is not fully known, and this point is still unclear whether platelets stimulate tissue regeneration by inhibiting apoptosis or by activating stem cells located in tissues that cause tissue regeneration and reconstruction. In this study, the effect of platelet density on the expression of the OCT4 gene that stimulates stem cells was investigated.
In many studies for the detection of ovarian function in POF model, the expression levels OCT4 gene was evaluated (18). OCT4 is a stem cell-specific marker gene that is a member of the transcription factors' POU domain family (30). In examining the OCT4 gene, a significant difference was observed between the X and 2X groups with the PBS group, but 4X group does not show a significant difference in OCT4 gene expression (Figure 4B). This shows that with the increase in platelet concentration, the stimulation of stem cells for growth and differentiation has increased. However, this increase in density can affect the stimulation of stem cells to an extent that at the concentration of 4X, no noticeable difference was observed in the expression of the OCT4 gene compared to the PBS group (Figure 4B). Figure 4B shows that X group concentration has a significant difference from the PBS group, which indicates that in lower concentrations, PRP can lead to the activation of stem cells. Jiang et al. used a mouse model of POF generated by CTX/busulfan to assess the protective effects of resveratrol (RES). In the meantime, the RES group showed an increase in OCT4 expression, suggesting that RES considerably and partially aided in the growth of germinal stem cells in the POF model (18).
5. Conclusion
It is worth mentioning that more studies should be done on this work and the work should be done on a larger scale. And if the result is acceptable, it should be done in the form of a case report on humans, keeping in mind the ethical considerations. Hoping that one day POF patients can be treated using PRP, which is a simple method, and there is no need for complicated treatments. Considering that in this study, the number of investigated genes from each pathway was one number, it is suggested to select more genes from each pathway for a more detailed investigation of the effect of platelet density and to identify the effective molecular pathway in ovarian tissue regeneration, and the number of mice in each group should be increased to get a more definite result.
Data Availability
Data supporting the findings of this study are available upon reasonable request from the corresponding author.
Author Contributions
Gh. Fotoohi-Ardakani and M. Lotfi designed the study and conducted the research. M. Lotfi, and N. Ghasemi monitored, evaluated, and analyzed the result of the study. Further, Gh. Fotoohi-Ardakani, A. Dadbinpour, and A. Hassanpour Dehnavi reviewed the article. All authors approved the final manuscript and take responsibility for the integrity of the data.
Acknowledgments
This article has been extracted from Ph.D. Thesis Gholamreza Fotoohi-Ardakani in Molecular Medicine, School of Advanced Technologies in Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. This study was supported by a grant from the Department of the School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran (grant number: 13399). This article does not use artificial intelligence in any way.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Original Article |
Subject:
Cellular and Molecular Biology of Reproduction
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |